Abstract
Background
Many hospitalized adults cannot reposition themselves in their beds. Therefore, they are regularly turned by their nurses, primarily to prevent pressure ulcer formation. Previous research indicates that turning is painful and that patients are rarely pre-medicated with analgesics. Non-pharmacologic interventions may be used to help with this painful procedure. However, no published research was found on the use of non-pharmacologic interventions for turning of hospitalized patients.
Objectives
1) to describe patient pain characteristics during turning and their association with patient demographic and clinical characteristics; 2) to determine the frequency of use of various non-pharmacologic interventions for hospitalized adult patients undergoing the painful procedure of turning; and 3) to identify factors that predict the use of specific non-pharmacologic interventions for pain associated with turning.
Methods
Hospitalized adult patients who experienced turning, the nurses caring for them, and others who were present at the time of turning were asked if they used various non-pharmacologic interventions to manage pain during the turning.
Results
Of 1395 patients, 92.5% received at least one non-pharmacologic intervention. Most frequently used were calming voice (65.7%), information (60.6%), and deep breathing (37.9%). Critical care patients were more likely to receive a calming voice (OR= 1.66, p<.01); receive information (OR=1.62, p<.001); and use deep breathing (OR= 1.36, p<.05) than those who were not critical care patients. Those reporting higher pain were consistently more likely to receive each of the three interventions (OR=1.01, p<.05 for all 3).
Conclusions
Non-pharmacologic interventions are used frequently during a turning procedure. The specific interventions used most often are ones that can be initiated spontaneously. These data suggest that patients, nurses, and family members respond to patients’ turning-related pain by using non-pharmacologic interventions.
Introduction
Hospitalized patients experience painful procedures on a regular basis. Yet, little is known about the pain associated with common procedures in acute and critical care settings. While data are limited, turning has been identified as a painful procedure for acute and critically ill patients (Bahar, Rosen, & Vickers, 1985; Lamb, 1979; Morrison et al., 1998; Puntillo et al., 2001; Stanik-Hutt, Soeken, Belcher, Fontaine, & Gift, 2001; Young, Siffleet, Nikoletti, & Shaw, 2006). Recently, Young et al. (2006) demonstrated that, among sedated, unconscious intensive care unit (ICU) patients, 73% had increased pain behaviors during repositioning. The odds of an increase in pain behaviors after turning was 25 times greater than after eye care, which was believed to be a non-painful intervention (p<.0001).
To investigate the painfulness related to turning and other procedures, the American Association of Critical Care Nurses (AACN) conducted the Thunder II ® study. Previous reports from this study demonstrated that perceptions of procedural pain varied by procedure and that turning was the most painful of the six procedures studied (i.e., tracheal suctioning, wound drain removal, wound care, central line insertion, femoral sheath removal, and turning) (Puntillo et al, 2001). The mean pain intensity during turning was 4.93 ± 3.1 [(on a 0 to 10 numeric rating scale (NRS)], and only 14% of patients were pre-medicated with opioids for the turn (Puntillo et al., 2002). Given the fact that turning is painful and that patients rarely receive pre-medication with an analgesic, it may be that non-pharmacologic interventions are used to decrease pain. Since no research data exist about the use of non-pharmacologic interventions for the turning procedure, the use of non-pharmacologic interventions that may reduce pain and distress during procedures was examined as part of the Thunder II ® study. In addition, since demographic characteristics such as gender and ethnicity are known to influence pain (Chen, Woods, Wilkie, & Puntillo, 2005; Im et al., 2007), these factors were examined in relationship to the use of non-pharmacologic interventions during turning. Finally, the study investigators believed that it was important to consider clinical characteristics such as level of care, diagnosis, use of opioid pre-medication as well as characteristics of the turning procedure itself that might influence the patient’s pain.
Therefore, the purposes of this report from the Thunder II® study are to: 1) describe patient pain characteristics during turning and their association with patient demographic and clinical characteristics; 2) determine the frequency of use of various non-pharmacologic interventions for hospitalized adult patients undergoing the painful procedure of turning; and 3) identify factors that predict the use of specific non-pharmacologic interventions for pain associated with turning.
The conceptual framework of this study is the multidimensionality of procedural pain as described in Puntillo et al (2001). Procedural pain is conceptualized as an unpleasant sensory and emotional experience that arises from potential or actual tissue damage while patients are undergoing procedures. The multidimensionality includes sensory-discriminative, motivational-affective, and cognitive-evaluative factors that can influence a patient’s pain experience. Several other factors can influence the pain experience during a procedure, including the patient’s age, gender, ethnicity, analgesic therapies, and environmental factors. This report emphasizes environmental factors, specifically the use of non-pharmacologic interventions by others in the patient’s environment during the procedure.
Materials and Methods
Study Sample
A convenience sample of 169 hospitals agreed to participate in the Thunder II ® study. As described previously (Puntillo et al, 2001), each hospital had a site coordinator who was a nurse with research experience and/or research support. The protection of human subjects in research was confirmed at each of the individual sites. The sample was obtained by convenience at participating institutions. Selected procedures included turning, central venous catheter insertion, wound drain removal, non-burn wound care, tracheal suctioning, and femoral sheath removal. Patients were included if they were experiencing the selected procedure as part of normal care and were determined by their nurse to be awake, alert, oriented, and medically stable enough to respond to questions; ≥ 18 yrs of age; able to understand and communicate; and able to hear and see. Patients were excluded if they were receiving neuromuscular blocking medications or had a disease process or injury that impaired sensory transmission proximal to the procedure site such as a peripheral neuropathy. This report focuses on the subset of patients who underwent the turning procedure.
Procedures and Measures
Data on pain intensity were collected during the turn. Pain intensity was measured using a 0 (no pain) to 10 (worst possible pain) numeric rating scale (NRS). Construct and criterion validity as well as reliability of NRS scales are well established (Jensen, 1989). Additional procedure-related and patient demographic and clinical data, including analgesics administered within one hour prior to and during the procedure, were obtained from the patient's chart.
Immediately after the procedure, patients, their nurse, and others present during the procedure (such as family members) were asked what non-pharmacologic interventions, if any, they used during the procedure. Participants were asked to select all that applied from the following list: distraction; progressive relaxation; ice; heat; guided imagery; gentle touch/hand holding; acupressure; massage; presence of family/friends; music; information; hypnosis; deep breathing; therapeutic touch; calming voice; pillow splinting; humor; TENS; unknown; other (to be specified). These non-pharmacologic interventions were chosen by the project team through consensus as representing interventions that have been used to treat pain in other patient populations.
Study Variables and Data Analysis
Affirmative responses by patients, nurses, or others present about the use of non-pharmacologic interventions for turning were aggregated. A negative response indicated that neither the patient, nurse, nor others present noted that they used that intervention for the turn. This aggregation was done because, for the purposes of this exploratory study, the investigators wanted to simply identify all non-pharmacologic interventions regardless of the initiator.
Statistical Package for the Social Sciences (SPSS) version 11.0 was used for all analyses. Descriptive statistics were used to generate information about patient demographic and clinical characteristics as well as frequency of use of each non-pharmacologic intervention. Chi square statistics, t-tests, and one-way Analysis of Variance (ANOVA) tests were used to explore univariate associations between the most frequently used non-pharmacologic interventions for turning and demographic and clinical characteristics. All the assumptions of the t-test and ANOVA were met. Then, three multivariate logistic regression models were constructed to examine demographic and clinical predictors of the three most frequently used non-pharmacologic interventions for turning. The dependent variable was the specific non-pharmacologic intervention. The independent variables were the clinical and demographic characteristics including age, gender, ethnicity, care level, diagnosis, turn method, patient assistance, use of a draw sheet, pain intensity, and opioid pre-medication. Age and pain intensity scores were entered as continuous variables, and the other variables were entered as categorical variables. Simultaneous entry of variables was used, and a p-value of <0.05 was considered statistically significant.
Results
Sample
This report focuses on one specific turn for each of the 1395 adult patients in the Thunder II study ® who were turned. Table 1 reports the demographic and clinical characteristics of these patients. Patients were predominantly white (86.3%) and male (55.3%), with a mean age of 63.5 ± 3.1 years. The majority of patients (65.9%) were in a critical care unit; 21.9% were on a specialty floor; and 12.2% were on “other” units. Most patients had a primary diagnosis that was surgical (70.4%). Most patients were turned using a drawsheet (53.6%), and most patients (69.4%) assisted with the turn. Only 12% of the patients were pre-medicated for the turn with an opioid analgesic.
Table 1.
Demographic and clinical characteristics of the sample (N=1395)
| Age | Mean = 63.5 years | Range = 18–97 | |
|---|---|---|---|
| N | % | ||
| Gender | Female | 592 | 44.7% |
| Male | 803 | 55.3% | |
| Ethnicity | |||
| White | 1204 | 86.3% | |
| African American | 98 | 7.1% | |
| Other | 77 | 5.6% | |
| Level of care | |||
| Critical care | 907 | 65.9% | |
| Specialty floor | 302 | 21.9% | |
| Other | 167 | 12.2% | |
| Primary diagnosis | |||
| Medical | 332 | 24.2% | |
| Surgical | 965 | 70.4% | |
| Trauma/Burn/Other | 74 | 5.4% | |
| Turning method | |||
| Hands | 518 | 43.6% | |
| Drawsheet | 637 | 53.6% | |
| Other | 34 | 2.8% | |
| Patient assist with turn | |||
| Assisted | 927 | 69.4% | |
| Did not assist | 409 | 30.6% | |
| Opioid premedication | |||
| Yes | 168 | 12.0% | |
| No | 1227 | 88.0% | |
Pain intensity reports
The mean pain intensity score at the time of the turn was 4.9 ± 3.1. As shown in Table 2, except for ethnicity, significant differences were found in mean pain intensity scores for a variety of demographic and clinical characteristics. Specifically, females, specialty floor patients, surgical and trauma or burn patients reported significantly higher levels of pain during the turn. Those who were turned with a drawsheet, those who did not assist with the turn, and those who were pre-medicated reported more pain.
Table 2.
Differences in mean pain intensity score during turning according to demographic and clinical characteristics (N=1395)
| Mean | (Standard Deviation) |
Statistics | ||
|---|---|---|---|---|
| Overall | 4.9 | (3.1) | ||
| Age | ||||
| 18–40 | 6.0 | (2.8) | F=22.2*** | |
| 41–60 | 5.5 | (3.0) | ||
| 61+ | 4.5 | (3.1) | ||
| Gender | ||||
| Male | 4.7 | (3.0) | t=3.9*** | |
| Female | 5.2 | (3.2) | ||
| Ethnicity | ||||
| African American | 4.9 | (3.4) | F=.01 | |
| White | 4.9 | (3.1) | ||
| Other | 4.9 | (3.0) | ||
| Level of care | ||||
| Critical Care | 4.7 | (3.1) | t=3.9*** | |
| Specialty floor/other | 5.4 | (3.0) | ||
| Diagnosis | ||||
| Medical | 3.8 | (3.4) | F=34.6*** | |
| Surgical | 5.2 | (2.8) | ||
| Trauma/burn/other | 6.1 | (3.1) | ||
| Turn procedure | ||||
| Drawsheet | 5.2 | (3.1) | t=3.0*** | |
| Hands/other | 4.7 | (3.0) | ||
| Patient assist with turn? | ||||
| Assisted | 4.8 | (3.0) | t=2.8*** | |
| Did not assist | 5.3 | (3.2) | ||
| Opioid pre-medication | ||||
| Pre-medicated | 6.4 | (2.8) | t=−6.5*** | |
| Not pre-medicated | 4.7 | (3.1) | ||
NRS = numeric rating scale
p<.001
Frequency of non-pharmacologic interventions
Table 3 reports the frequency of specific non-pharmacologic interventions used during turning. The most frequently reported interventions included calming voice, information, deep breathing, gentle touch/hand holding, distraction, pillow splinting, and humor. Somewhat less frequently used were massage, presence of family/friends, therapeutic touch, progressive relaxation, ice, and “other”. Infrequently used interventions were music, heat, guided imagery, TENS, acupressure, and hypnosis.
Table 3.
Frequency of non-pharmacologic interventions used during turning (N=1395)
| Percent | N | |
|---|---|---|
| Calming voice | 65.7% | 917 |
| Information | 60.6% | 845 |
| Deep breathing | 37.9% | 528 |
| Gentle touch/hand holding | 36.6% | 510 |
| Distraction | 34.2% | 474 |
| Pillow splinting | 34.0% | 473 |
| Humor | 25.9% | 361 |
| Massage | 15.4% | 215 |
| Presence of family/friends | 13.7% | 191 |
| Therapeutic touch | 10.1% | 141 |
| Progressive relaxation | 8.1% | 113 |
| Other | 4.7% | 65 |
| Ice | 2.3% | 32 |
| Music | 1.9% | 27 |
| Heat | 1.4% | 20 |
| Guided imagery | 0.9% | 13 |
| TENS | 0.7% | 10 |
| Acupressure | 0.2% | 3 |
| Hypnosis | 0.0% | 0 |
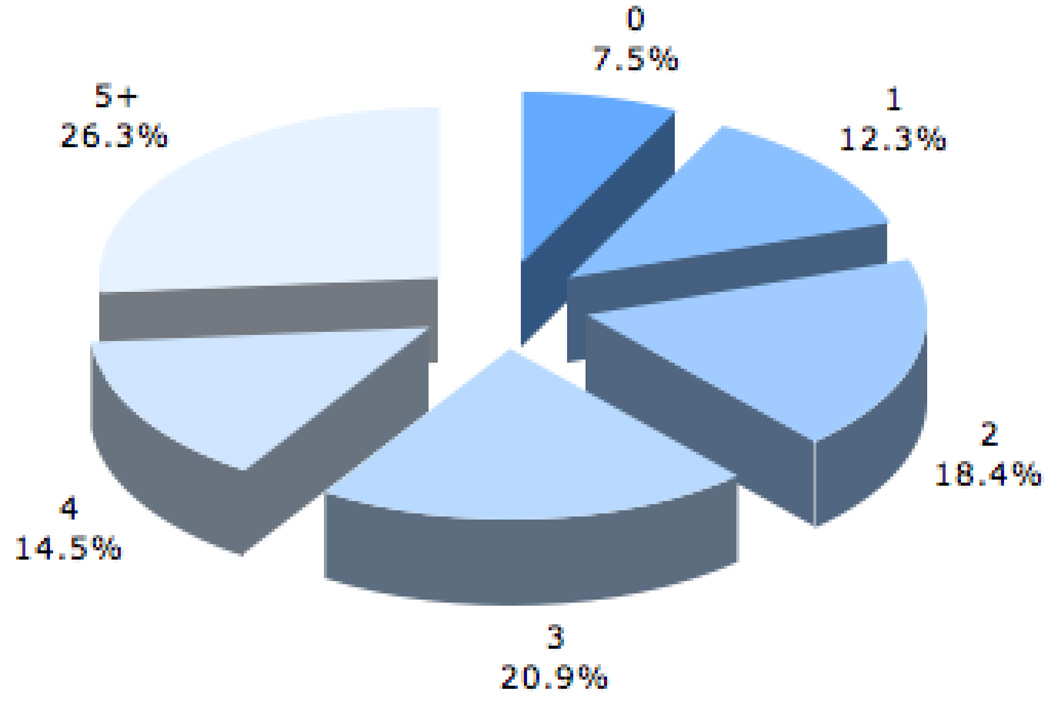
Figure 1 presents the total number of all non-pharmacologic interventions used during one particular turn. The vast majority of patients (92.5%) had at least one non-pharmacologic intervention, while over a quarter of patients (26.3%) had five or more interventions.
Figure 1.
Number of non-pharmacologic interventions used during one turn (N=1395)
The three most frequently performed non-pharmacologic interventions were calming voice (65.7%), receiving information (60.6%), and deep breathing (37.9%). Table 4 presents the differences in use of each of these three interventions according to patients’ demographics and clinical characteristics. Use of calming voice differed according to whether the patient was in a critical care unit. Patients in critical care units were more likely to receive a calming voice. Those who were turned with the use of a drawsheet and those who reported a higher pain intensity more frequently received a calming voice. Those who were in a critical care unit, who did not assist the health care provider during the turn, who had higher pain intensity, or who were non-medical patients received information significantly more frequently. Use of deep breathing was the only non-pharmacologic intervention that was influenced by age. Those patients who used deep breathing were younger than those who did not. Deep breathing was used more frequently by those who reported a higher pain intensity score; were in a critical care unit; who had a surgical versus trauma or burn diagnosis; and were pre-medicated with opioids.
Table 4.
Differences in demographic and clinical characteristics for each of the three most frequently used non=pharmacologic interventions (N=1395)
| Calming Voice | Information | Deep Breathing | ||
|---|---|---|---|---|
| Gender | ||||
| Male | 62.9% | 63.6% * | 39.2% | |
| Female | 67.4% | 55.7% | 35.8% | |
| Ethnicity | ||||
| White | 66.6% | 62.4% * | 38.9% | |
| African-American | 68.8% | 55.3% | 30.8% | |
| Other | 53.3% | 45.2% | 38.1% | |
| Care level | ||||
| Critical care | 68.2% * | 65.2% ** | 40.5% ** | |
| Specialty floor/ other |
60.6% | 51.3% | 32.8% | |
| Diagnosis | ||||
| Medical | 62.5% | 47.9% ** | 18.8% ** | |
| Surgical | 66.3% | 64.3% | 44.5% | |
| Trauma/burn/other | 76.8% | 75.0% | 38.7% | |
| Turn method | ||||
| Hands | 58.5% ** | 56.7% ** | 39.0% | |
| Drawsheet | 71.2% | 66.0% | 38.5% | |
| Other | 54.8% | 35.5% | 32.5% | |
| Patient assist | ||||
| Assisted | 64.5% | 57.4% ** | 37.0% | |
| Did not assist | 70.1% | 68.0% | 41.8% | |
| Opioid premed | ||||
| Premedicated | 70.7% | 67.3% | 57.6% ** | |
| Not premedicated | 65.0% | 59.7% | 32.5% | |
| Calming Voice | Information | Deep Breathing | ||||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| Mean NRS pain (during turn) |
5.3 | 4.4** | 5.2 | 4.6** | 5.6 | 4.6** |
| Mean age (years) | 63.7 | 63.1 | 63.6 | 63.3 | 61.1 | 65.0** |
Chi-square tests for categorical variables and t-tests for continuous variables
p<.01,
p<.001
Predictors of the three most frequently performed non-pharmacologic interventions
Separate multivariate logistic regression models were constructed for calming voice, deep breathing, and information (Table 5). Since all demographic and clinical variables had significant univariate associations with at least one of the three top non-pharmacologic interventions, all demographic and clinical predictors were included in each model. Age did not predict use of any of the three non-pharmacologic interventions studied. Gender was predictive of use of a calm voice; female patients were 1.3 times more likely than male patients to receive a calming voice (odds ratio= 0.74, 95% CI 0.56–0.98). Ethnicity was predictive, since white patients were 1.7 times more likely than patients of other ethnicities to receive a calming voice (odds ratio=1.74, 95% CI 1.01–3.02) and 1.9 times more likely than patients of other ethnicities to receive information (odds ratio=1.87, 95% CI 1.07–3.25). Those patients in critical care were more likely to receive each of these non-pharmacologic interventions than were those on a specialty floor (for calm voice: odds ratio=1.66, 95% CI 1.23–2.23; for information: odds ratio=1.62, 95% CI 1.21–2.16; and for deep breathing: odds ratio=1.36, 95% CI=1.01–1.84).
Table 5.
Multivariate logistic regression of demographic and clinical predictors for each of the three most frequently performed non-pharmacologic interventions during turning (N=1395)
| Calming voice | Information | Deep breathing | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio |
95% Confidence Interval |
Odds Ratio |
95% Confidence Interval |
Odds Ratio |
95% Confidence Interval |
||
| Age | 1.00 | 0.99–1.01 | 1.01 | 0.99–1.01 | 0.99 | 0.98–1.00 | |
| Male gender | 0.74 * | 0.56–0.98 | 1.23 | 0.93–1.62 | 1.01 | 0.76–1.34 | |
| Ethnicity | |||||||
| African-American | 1.68 | 0.81–3.50 | 1.27 | 0.61–2.64 | 1.21 | 0.55–2.66 | |
| White | 1.74 * | 1.01–3.02 | 1.87 * | 1.07–3.25 | 1.43 | 0.79–2.62 | |
| Critical care | 1.66 ** | 1.23–2.23 | 1.62 *** | 1.21–2.16 | 1.36 * | 1.01–1.84 | |
| Diagnosis | |||||||
| Surgical | 1.02 | 0.73–1.42 | 1.73 *** | 1.25–2.38 | 2.33 *** | 1.62–3.34 | |
| Trauma/burn/other | 1.70 | 0.82–3.53 | 4.12 *** | 1.97–8.63 | 1.56 | 0.78–3.11 | |
|
Turned with drawsheet |
1.63 *** | 1.23–2.14 | 1.53 ** | 1.17–2.02 | 0.90 | 0.68–1.19 | |
|
Patient assisted with turn |
1.01 | 0.74–1.37 | 0.86 | 0.64–1.17 | 0.85 | 0.64–1.16 | |
|
Pain intensity during turn |
1.01 *** | 1.01–1.02 | 1.01 * | 1.001–1.009 | 1.01 * | 1.001–1.010 | |
| Opioid pre-medication | 1.05 | 0.68–1.61 | 1.11 | 0.73–1.69 | 1.58 * | 1.06–2.36 | |
p<.05,
p<.01,
p<.001
reference categories: ethnicity: “other”
level of care/critical care: “specialty floor, other”
diagnosis: “medical”
turning method: “turned with hands/other”
Primary diagnosis predicted the use of non-pharmacologic interventions. Surgical patients were more likely than medical patients to receive information (odds ratio=1.73, 95% CI 1.25–2.38) and deep breathing (odds ratio=2.33, 95% CI 1.62–3.34) interventions. Patients who reported a higher pain intensity score were more likely to receive each of these non-pharmacologic interventions (for calming voice: odds ratio=1.01, 95% CI 1.01–1.02; for information: odds ratio=1.01, 95% CI 1.001–1.009; and for deep breathing: odds ratio=1.01, 95% CI=1.001–1.010). For example, this means that the odds of using a calming voice was 1.01 times more likely for each one point increase in the 10 point NRS.
Discussion
The results of this study provide important new insights into the use of non-pharmacologic interventions in the hospital setting for adult patients who are being turned. Of note, non-pharmacologic interventions were used more frequently than opioid pre-medication. The non-pharmacologic interventions most frequently employed were calming voice, receiving information, and deep breathing. In addition, for these interventions, clinical characteristics (such as the patient’s diagnosis and level of care) as well as some demographic characteristics were associated with the use of non-pharmacologic interventions.
Most notably, non-pharmacologic interventions were used frequently, with 93% of patients receiving at least one and 26% receiving five or more. While no data were found in the literature on frequency of non-pharmacologic interventions for procedural pain, the limited data that exist on their use for acute pain suggest that these techniques are not used frequently (Carroll et al., 1999; Manias, Bucknall, & Botti, 2005). However, the Thunder II ® study differed from these studies by including a very comprehensive list of non-pharmacologic interventions, which might partially explain this discrepancy. In addition, non-pharmacologic interventions may be used more frequently for procedural pain than for acute pain. One reason for their increased use with procedures may be that a nurse is present for the procedure and is likely to initiate or coach the patient to use a non-pharmacologic intervention, such as deep breathing, during procedures. Another possible explanation is that procedures, especially turning, occur during brief, discrete and relatively predictable blocks of time, which could facilitate their use.
Of concern is our finding that few patients were pre-medicated with analgesics. Since turning usually requires a second person, making the exact timing unpredictable, nurses may sometimes have insufficient opportunity to prepare for pre-medication. Thus, when patients experienced pain during turning, they and their caregivers may have attempted to control the pain using other methods. The non-use of medications is clearly problematic, given the amount of pain experienced by these patients who were turned. Nursing vigilance and attention to the importance of pre-medication whenever possible may help to decrease pain associated with this ubiquitous procedure. Furthermore, the combined use of pharmacologic and non-pharmacologic interventions during a turning procedure may provide the optimal approach to pain management and warrants further study.
The most frequently used interventions during turning included calming voice, information, deep breathing, gentle touch hand holding, distraction, pillow splinting, and humor. In general, these techniques are easy to implement and did not require equipment or specific training. In contrast, the methods that require equipment and/or training, such as TENS, music, and guided imagery were not used frequently. These results are not unexpected given the busy nature of acute and critical care settings.
Overall, the non-pharmacologic interventions previously studied for efficacy do not fully correspond to those that were most frequently used in this study. For example, the largest body of research is on the use of music for procedural pain (Bally, Campbell, Chesnick, & Tranmer, 2003; Broscious, 1999; Cepeda, Carr, Lau, & Alvarez, 2006; Chan et al., 2006; Kwekkeboom, 2003). However, only 1.9% of our sample used music. Calming voice, gentle touch, pillow splinting, and humor were four out of the six most frequently used interventions, yet no data were found regarding their effectiveness for procedural pain. While this study did not examine the effectiveness of these interventions for pain, the identification of and predictors of their use provides foundational information for future studies.
Of the most frequently used interventions in our study, only information and deep breathing were evaluated in two previous studies. Lang and colleagues (2005) examined the relationship between pain intensity and information about painful sensations, such as “sharp” or “stinging”, patients might feel during interventional radiological procedures. Interestingly, patients who were told to expect pain or noxious stimuli reported higher procedural pain intensity scores than those patients who were not told what to expect. In the second study, Puntillo and colleagues (2004) examined the addition of sensory information to a pharmacologic analgesic intervention for chest tube removal. Sensory information was that which described the specific sensation to be expected such as aching, sharp, or stinging. No differences were found in pain intensity and distress between patients who received sensory information with an analgesic compared to those who received only an analgesic. Findings from these two studies suggest that information may not alleviate procedural pain.
Two studies assessed the effectiveness of deep breathing on procedural pain. In the first, Friesner and colleagues (2006) found that patients who performed deep breathing exercises (i.e., inhaling through nose and exhaling slowly through pursed lips) and received opioids had a significant decrease in pain intensity scores during chest tube removal compared to patients who received only opioids. In a second randomized clinical trial (Lang et al., 2000), patients undergoing percutaneous vascular and renal procedures randomized to a self-hypnosis group (i.e., instructed to close their eyes, breath deeply, and concentrate on a sensation of floating) (n=82) reported a constant level of procedural pain. This is in comparison to increases in pain in patients in attention control (n=80) or standard care groups (n=79). This finding suggests that a hypnosis intervention which includes deep breathing may help to diminish this type of procedural pain. Because the hypnotic intervention included eye closing and concentration on a sensation of floating, it is not possible to determine the independent contribution of deep breathing. Yet, both of these studies provide some evidence that deep breathing may help to alleviate procedural pain.
Regarding the efficacy of the most frequently used non-pharmacologic interventions in our study, the evidence is mixed. No data are available on the effectiveness of a calming voice; information may have no effect or a detrimental effect on pain; and deep breathing may help to alleviate pain. All of these data focus on procedures other than turning. Given the paucity of research, it is unclear that the information obtained about one procedure is generalizable to another. Randomized controlled trials are needed to elucidate the efficacy of different non-pharmacologic interventions, with subsequent development of evidence-based guidelines.
This study explored demographic and clinical characteristics that, when studied within the context of other factors, influenced whether or not a patient got the interventions of calming voice, deep breathing, and information. The logistic regression analyses indicated that, in general, clinical factors did affect non-pharmacologic intervention use, while only some demographic factors did. Of demographic variables, age was not predictive. This suggests that, while age is inversely related to level of reported pain, age was not associated with the use of non-pharmacologic interventions for turning. Of the clinical characteristics, a critical care setting and pain intensity during turn were consistently associated with increased likelihood that a patient would receive each of the three non-pharmacologic interventions. Perhaps the finding related to setting can be explained by increased nursing experience and better nurse-patient ratios in ICUs. A critical care nurse is often more experienced and cares for fewer patients. Thus, the critical care nurse may be able to allocate more time for the turn and be more comfortable and skilled in using multiple interventions. The level of a patient’s pain intensity may be related to non-pharmacologic intervention use; nurses who know that a patient is having pain during the procedure may be aware of a patient’s pain during turning and respond with non-pharmacologic interventions that are immediately available. Similarly, when patients experience procedural pain during a turn, they themselves might initiate an intervention such as deep breathing.
While this study does present new findings, it has limitations. Since data were collapsed across patients’, nurses’, and others’ responses, we do not know for sure who initiated the non-pharmacologic interventions and whether one provider is more successful that another in using these interventions. Yet, we believed that identity of performer was less important than capturing the overall use of non-pharmacologic interventions in this exploratory study. Due to the observational design of the study, we cannot evaluate the effectiveness of the various non-pharmacologic interventions that were used for turning. The finding that pain was positively associated with use of a non-pharmacologic intervention evidenced this limitation. Another limitation is that, instead of random sampling, a convenience sample was recruited. This could contribute to selection bias and limit the generalizability of the findings. However, the sample was very large, with multiple units in many hospitals.
While the large sample size based on multiple sites strengthens generalizability, it can lead to statistical overpowering and the finding of significant results that are due to chance. However, some of the key findings, such as frequency of use of non-pharmacologic interventions, were purely descriptive and not influenced by statistical power. For the univariate and logistic regression analyses, most significant findings met a more rigorous level of significance (p<.01 or p<.001). Another potential limitation of the sample is that it was not very ethnically diverse: it was predominantly white (86.3%), with a small group of African – American patients (7.1%). This ethnic distribution limits applicability of findings to Asian, Latino, or other ethnically diverse patient populations. Future studies should incorporate sampling interventions to ensure a more ethnically diverse sample.
Conclusions
This study found that non-pharmacologic interventions were used frequently for turning. The specific interventions used most often included calming voice, information, and deep breathing, ones that can be initiated spontaneously and without specific equipment or training. These data suggest that patients, nurses, and family members may be aware of patients’ pain during turning and respond to their increased pain by using non-pharmacologic interventions available in that situation, such as calm voice and deep breathing, Randomized controlled trials are needed that examine the effectiveness of non-pharmacologic interventions for procedural pain, especially considering that some are frequently used in clinical practice.
Acknowledgments
Work was performed at University of California, San Francisco, School of Nursing. Grant support-
1) American Association of Critical Care Nurses
2) University of California, San Francisco, Pathways to Clinical and Translational Research Fellowship, Spring 2007
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bonnie Faigeles, Nurse Practitioner, Department of Neurosciences, Kaiser-Permanente Medical Center, Redwood City, CA.
Jill Howie-Esquivel, Assistant Professor, Acute Care Nurse Practitioner Program, University of California, San Francisco.
Christine Miaskowski, Professor and Associate Dean for Academic Affairs, Department of Physiological Nursing, University of California, San Francisco.
Julie Stanik - Hutt, Associate Professor, Johns Hopkins University School of Nursing And Nurse Practitioner, Halsted 5 Cardiology NP Service, Johns Hopkins Hospital.
Carol Thompson, Professor Critical and Acute Care Nursing, University Tennessee Health Science Center, Memphis, TN.
Cheri White, Trauma Program Director, Sutter Roseville Medical Center, Roseville, CA.
Lorie Rietman Wild, Chief Nursing Officer and Senior Associate Administrator, Patient Care Services, Assistant Dean, University of Washington School of Nursing, University of Washington Medical Center.
Kathleen Puntillo, Professor Emeritus and Research Scientist, Department of Physiological Nursing, University of California, San Francisco.
REFERENCES
- Bahar M, Rosen M, Vickers MD. Self-administered nalbuphine, morphine and pethidine. Comparison, by intravenous route, following cholecystectomy. Anaesthesia. 1985;40(6):529–532. [PubMed] [Google Scholar]
- Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of patient-controlled music therapy during coronary angiography on procedural pain and anxiety distress syndrome. Critical Care Nurse. 2003;23(2):50–58. [PubMed] [Google Scholar]
- Broscious SK. Music: an intervention for pain during chest tube removal after open heart surgery. American Journal of Critical Care. 1999;8(6):410–415. [PubMed] [Google Scholar]
- Carroll KC, Atkins PJ, Herold GR, Mlcek CA, Shively M, Clopton P, et al. Pain assessment and management in critically ill postoperative and trauma patients: a multisite study. American Journal of Critical Care. 1999;8(2):105–117. [PubMed] [Google Scholar]
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Systematic Review. 2006;(2) doi: 10.1002/14651858.CD004843.pub2. CD004843. [DOI] [PubMed] [Google Scholar]
- Chan MF, Wong OC, Chan HL, Fong MC, Lai SY, Lo CW, et al. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions. Journal of Advances in Nursing. 2006;53(6):669–679. doi: 10.1111/j.1365-2648.2006.03773.x. [DOI] [PubMed] [Google Scholar]
- Chen W, Woods SL, Wilkie DJ, Puntillo KA. Gender differences in symptom experiences of patients with acute coronary syndromes. Journal of Pain and Symptom Management. 2005;30(6):553–562. doi: 10.1016/j.jpainsymman.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Friesner SA, Curry DM, Moddeman GR. Comparison of two pain-management strategies during chest tube removal: Relaxation exercise with opioids and opioids alone. Heart and Lung. 2006;35(4):269–276. doi: 10.1016/j.hrtlng.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Im EO, Chee W, Guevara E, Liu Y, Lim HJ, Tsai HM, et al. Gender and ethnic differences in cancer pain experience: A multiethnic survey in the United States. Nursing Research. 2007;56(5):296–306. doi: 10.1097/01.NNR.0000289502.45284.b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP, Karoly P, O’Riordan EF, Bland F, Burns RS. The subjective experience of acute pain: an assessment of the utility of 10 indices. Clinical Journal of Pain. 1989;5:153–159. doi: 10.1097/00002508-198906000-00005. [DOI] [PubMed] [Google Scholar]
- Kwekkeboom KL. Music versus distraction for procedural pain and anxiety in patients with cancer. Oncology Nursing Forum. 2003;30(3):433–440. doi: 10.1188/03.ONF.433-440. [DOI] [PubMed] [Google Scholar]
- Lamb K. Effect of positioning of postoperative fractured-hip patients as related to comfort. Nursing Research. 1979;28(5):291–294. [PubMed] [Google Scholar]
- Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet. 2000;355(9214):1486–1490. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]
- Lang EV, Hatsiopoulou O, Koch T, Berbaum K, Lutgendorf S, Kettenmann E, et al. Can words hurt? Patient-provider interactions during invasive procedures. Pain. 2005;114(1–2):303–309. doi: 10.1016/j.pain.2004.12.028. [DOI] [PubMed] [Google Scholar]
- Manias E, Bucknall T, Botti M. Nurses' strategies for managing pain in the postoperative setting. Pain Management Nursing. 2005;6(1):18–29. doi: 10.1016/j.pmn.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Morrison RS, Ahronheim JC, Morrison GR, Darling E, Baskin SA, Morris J, et al. Pain and discomfort associated with common hospital procedures and experiences. Journal of Pain and Symptom Management. 1998;15(2):91–101. [PubMed] [Google Scholar]
- Puntillo K, Ley SJ. Appropriately timed analgesics control pain due to chest tube removal. American Journal of Critical Care. 2004;13(4):292–301. [PubMed] [Google Scholar]
- Puntillo KA, Wild LR, Morris AB, Stanik-Hutt J, Thompson CL, White C. Practices and predictors of analgesic interventions for adults undergoing painful procedures. American Journal of Critical Care. 2002;11(5):415–429. [PubMed] [Google Scholar]
- Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, et al. Patients' perceptions and responses to procedural pain: Results from Thunder Project II. American Journal of Critical Care. 2001;10(4):238–251. [PubMed] [Google Scholar]
- Stanik-Hutt JA, Soeken KL, Belcher AE, Fontaine DK, Gift AG. Pain experiences of traumatically injured patients in a critical care setting. American Journal of Critical Care. 2001;10(4):252–259. [PubMed] [Google Scholar]
- Young J, Siffleet J, Nikoletti S, Shaw T. Use of a Behavioural Pain Scale to assess pain in ventilated, unconscious and/or sedated patients. Intensive Critical Care Nursing. 2006;22(1):32–39. doi: 10.1016/j.iccn.2005.04.004. [DOI] [PubMed] [Google Scholar]