Abstract
In India, men who have sex with men (MSM) and truck drivers are high-risk groups that often do not access HIV testing due to stigma and high mobility. This study evaluated a field testing package (FTP) that identified HIV positive participants through video pre-test counseling, OraQuick oral fluid HIV testing, and telephonic post-test counseling and then connected them to government facilities. 598 MSM and truck drivers participated in the FTP and completed surveys covering sociodemographics, HIV testing history, risk behaviors, and opinions on the FTP. Those who had previously been tested preferred traditional methods to video counseling. MSM and truck drivers equally preferred video counseling, although MSM who had been previously tested preferred traditional methods. Nearly all participants preferred oral testing. Rates of counseling completion and linkage to government centers were low, with one third of newly identified positives completing follow-up. With increased public-private coordination, this FTP could identify many hard-to-reach preliminary positive individuals and connect them to government testing and care.
KEY WORDS/PHRASES: Men who have sex with men (MSM), truck drivers, oral fluid HIV testing, India, telephonic counseling
INTRODUCTION
An estimated 2.4 million people in India are currently living with HIV (Joint United Nations Programme on HIV/AIDS, 2008). Most of these individuals are members of subpopulations that are experiencing concentrated HIV epidemics and require targeted HIV prevention efforts (Bachani & Sogarwal, 2010). The cornerstone of India’s HIV prevention effort is its network of effective Integrated Counselling and Testing Centres (ICTC) (National AIDS Control Organization, 2007b), which has historically struggled to reach marginalized subpopulations (Chandrasekaran et al., 2006). There are few approved HIV testing facilities beyond government ICTCs, as non-governmental organization (NGO) efforts such as the Bill and Melinda Gates Foundation’s Avahan initiative have historically tended to focus on HIV prevention efforts that do not include HIV testing services (Bill & Melinda Gates Foundation, 2011; National AIDS Control Organization, 2007c).
By better partnering with NGOs to connect high-risk individuals to testing, ICTCs could further increase their efficiency and ensure that their services are readily available to marginalized populations. ICTCs would benefit from NGO partners’ familiarity with marginalized populations, which would help them locate preliminary positive individuals and connect them to testing and care at government ICTCs. We developed a field testing package (FTP) intervention designed to galvanize this type of public-private coordination, with the goal of increasing testing among two Indian high-risk male populations that face barriers to accessing ICTCs: men who have sex with men (MSM) and truck-drivers (Chandrasekaran, et al., 2006; U.S. President’s Emergency Plan for AIDS Relief, Center for Disease Control-Global AIDS Program, the University of Chicago, & SHARE-India, 2007)
Previous research focused on MSM in India has shown that they are a particularly high-risk and stigmatized population (Asthana & Oostvogels, 2001; Chakrapani, Newman, & Shunmugam, 2008; Dandona et al., 2005; Go et al., 2004; Hemmige et al., 2011; Schneider et al., 2011a; Setia, Sivasubramanian, Anand, Row-Kavi, & Jerajani, 2010). Despite the recent decriminalization of homosexuality in India (Naz Foundation v. NCT of Delhi, 2009), substantial barriers to HIV testing remain for Indian MSM, including a perceived history of poor treatment in clinics as well as a variety of structural barriers (U.S. President’s Emergency Plan for AIDS Relief, et al., 2007). For example, strict identity card requirements may result in nearly half of all patients being denied care, with MSM being among the hardest hit groups due to their marginalization from mainstream society (The Times of India, 2010). Such structural barriers in combination with the history of stigmatization can make MSM unwilling or unable to utilize government testing and treatment centers.
Truck drivers face a distinct, yet equally troubling set of barriers to HIV testing. For example, government testing centers are often located in areas where long-haul trucks are not permitted, making it challenging for this group to access the centers. Furthermore, many ICTCs require that clients have their blood drawn in the morning and wait until the afternoon for test results, which is often impossible for drivers given high-pressure pick-up and delivery deadlines (Cornman, Schmiege, Bryan, Benziger, & Fisher, 2007; Schneider et al., 2010a; Schneider et al., 2009). Previously, leaders of the truck driver community known as Ustaads could have helped drivers negotiate such obstacles, but they are increasingly becoming less relevant in the face of a perceived decrease in pay and respect for the profession (Sethi, 2008). Several attempts have been made by the National AIDS Control Organisation (NACO) to implement mobile HIV testing units for this population, however such programs are sporadic and would be unable to reach the approximately 5–6 million truck-drivers working in India today (Bill & Melinda Gates Foundation, 2008; National AIDS Control Organization & National Institute of Medical Sciences, 2006). ICTCs are moderatelyeffective at bringing HIV testing to the general population of India, and through cooperation with complementary NGO services it could become easier for them to reach more marginalized populations.
In 2007, a conference was held in the state of Andhra Pradesh by a group of stakeholders that included the U.S. President’s Emergency Plan for AIDS Relief/Center for Disease Control-Global AIDS Program (PEPFAR/CDC-GAP), the University of Chicago, and SHARE-India (U.S. President’s Emergency Plan for AIDS Relief, et al., 2007). Andhra Pradesh was chosen as the conference location because it has an HIV prevalence that is three and a half times the national average and the largest HIV infected population in the country (International Institute for Population Sciences, 2007). The goal of the conference was to use discussions between officials, health providers, community based organizations (CBOs), corporate partners, and community stakeholders to develop a unified strategy for decreasing barriers to HIV prevention and testing services for high-risk men. Since previous HIV prevention interventions aimed at high-risk men had typically not involved HIV testing, participants concluded that novel HIV testing approaches (Gutierrez, McPherson, Fakoya, Matheou, & Bertozzi, 2010; Kumar, Dandona, Schneider, Ramesh, & Dandona, 2009) should be developed to specifically target these high-risk groups.
Tailored testing programs for high-risk males and mobile populations have been effectively used in past studies (Alemagno, Stephens, Stephens, Shaffer-King, & White, 2009; Centers for Disease Control and Prevention, 2007; Chen et al., 2010; Erausquin et al., 2009; Guy et al., 2009; Schulden et al., 2008; Seña, Hammer, Wilson, Zeveloff, & Gamble, 2010; Spielberg et al., 2003; Spielberg et al., 2005; Tsu, Burm, Gilhooly, & Sells, 2002) and could help connect such groups in India to government HIV care. For this intervention, an FTP was designed to meet the needs of high-risk men in India by combining three strategies that have been utilized successfully in other settings: 1) video pre-test counseling; 2) oral fluid testing; and 3) telephonic post-test counseling (McKinstry, Goldbaum, & Meischke, 2007; Merchant et al., 2007; Spielberg, et al., 2005).
Video pre-test counseling, the first FTP component, has several documented benefits, including ensuring that standardized messages are delivered, allowing the counselor to focus on answering client questions rather than delivering basic information, and increasing client satisfaction (Calderon et al., 2007; Papa et al., 2008). A well-designed pre-test counseling video can efficiently communicate important information to clients who achieve similar levels of comprehension to those participating in traditional face-to-face pre-test counseling (Merchant, et al., 2007). Video based media is very popular in India (The National Readership Studies Council, 2006) and the increasing popularity of laptops and touchpads could also enhance participants’ interest in the process. Pre-test videos are particularly effective in high-risk populations since they can be culturally tailored to the unique circumstances of each distinct group (e.g., actors/scenarios that are relevant) and they may have the added benefit of making the patient feel more anonymous in a sensitive setting.
Oral testing, the second FTP component, is a promising method for increasing testing rates among hard-to-reach populations in India such as truck drivers and MSM. This method is minimally invasive, pain-free, fast, and can be used in non-clinical settings (Chen, et al., 2010; Pant Pai et al., 2007). Increased rates of testing have been shown among high-risk men when oral testing was offered in settings outside of India (Chen, et al., 2010; Spielberg, et al., 2005). In India, oral testing has not yet been used in non-clinical settings and it has not been used in populations at high-risk for HIV such as truck drivers or MSM. Studies of oral testing in clients seeking hospital care in India demonstrate that they prefer oral testing over other blood sample collection methods, in part due to the reduction in pain and anxiety with oral swabs (Pant Pai, 2007; Pant Pai et al., 2008; Pant Pai, et al., 2007). Oral testing benefits marginalized groups because it does not require laboratory equipment, making it ideal for mobile clinics that bring HIV testing directly to hard-to-reach individuals. Using these field sites, NGOs could identify preliminary positive clients and then refer them to existing government ICTCs. In addition, oral testing allows patients to receive their preliminary results much faster than traditional techniques, significantly increasing the chances of completing follow-up (Liang et al., 2005). In this way, field-based HIV testing could reduce the timing and location based barriers to HIV testing that were reported by truck drivers during the 2007 conference (U.S. President’s Emergency Plan for AIDS Relief, et al., 2007).
Telephonic post-test counseling, the third FTP component, could make it easier for mobile populations to access their results by eliminating the need for clients to make multiple trips to the testing site as is necessary with traditional counseling. In other mobile populations internationally, studies have shown that clients who are offered telephonic follow-up are significantly more likely to receive their results and post-test counseling than those who are only offered face-to-face notification (Hutchinson, Branson, Kim, & Farnham, 2006; McKinstry, et al., 2007; Schluter et al., 1996; Tsu, et al., 2002). Even with increased use of point-of-care rapid testing, providing test results at the time of testing is often not feasible due to the need for confirmatory testing which can take several days. Telephonic counseling, which will allow participants to communicate with counselors more easily, could increase the frequency with which these high-risk, mobile clients receive their results and additional follow-up counseling if it is necessary. To the best of our knowledge, telephonic post-test counseling methods have not been studied in India.
It is challenging for non-mobile government ICTCs to reach MSM and truck drivers, due to their marginalization and mobility. As illustrated by the stakeholders conference, these groups face many barriers to testing, ranging from MSM fears of stigmatization in government clinics to inaccessibility of clinics for highly mobile truck drivers (U.S. President’s Emergency Plan for AIDS Relief, et al., 2007). This study addressed the barriers to HIV testing at government centers by implementing a novel FTP that draws upon three components used successfully in other settings: video pre-test counseling, oral testing and telephonic post-test counseling (Chen, et al., 2010; Merchant, et al., 2007; Spielberg, et al., 2005; Tsu, et al., 2002). The FTP was designed to be convenient and sensitive to the needs of high-risk men and was tailored specifically to truck drivers and MSM. The response the two groups to the FTP was compared in order to determine whether the it could be generalized or whether the protocol needs to be tailored more extensively to each group, The primary goal of the study was to determine the feasibility and acceptability of implementing the FTP in field settings in order to connect high-risk, hard-to-reach clients to government ICTCs for further confirmatory testing and treatment. In order to meet this goal, we focused on three specific research questions: 1) How satisfied were MSM and truck drivers with novel HIV testing and counseling methods? 2) What is the association between satisfaction with the methods and previous HIV testing experience or risk group? 3) What were the completion rates of each component of the FTP and which other participant characteristics were associated with completion? These questions allowed us to determine the feasibility and acceptability of the FTP, focusing on whether risk group, HIV testing experience, or demographic variation had an impact on participant satisfaction with and completion of the protocol. This information is vital for tailoring future FTPs to participant characteristics.
METHODS
Participants and setting
The study recruited 300 MSM and 300 truck drivers from field sites in Andhra Pradesh, India in 2009. Truck drivers were recruited from parking lots in Hyderabad and the coastal city of Vizag. These lots are areas where drivers rest between trips for 2–4 days at a time. In Hyderabad, drivers were recruited from lots associated with Gati Corporation, while in Vizag they were recruited from lots owned by the Vizag Lorry Operators Welfare Association. MSM were recruited from cruising areas, which are public venues such as bus stations, parks, and waterfront walkways where paid and unpaid sexual encounters occur and drop-in centers, which are small private offices where MSM CBOs organize and provide social services (e.g. counseling) to the community. All MSM recruitment took place in the sister cities of Hyderabad and Secunderabad, at sites associated with Darpan, an MSM community based organization.
Eligible participants identified as men, were between the ages of 18 and 60, and either reported anal intercourse with a man in the last 12 months or were primarily employed as truck drivers who had been driving a truck at least for the last 3 months. Additionally, to be eligible, participants were required to speak Hindi or Telugu and have reliable telephone access (cell phone or landline). Identification cards were not checked, participants were free to give any name. We tested all men who met these criteria and were interested, including those who believed they had previously tested positive. Participants were approached from a convenience sample, as was the practice of the concurrently run government Andhra Pradesh State AIDS Control Society prevention programs (National AIDS Control Organization, 2007d). At study field sites, research assistants would determine whether candidate participants met the study eligibility criteria, then collect written informed consent, perform the interview, and provide HIV testing services (Figure 1). Following informed consent, study participants completed video pre-test counseling, oral fluid collection, dry blood spot collection (for confirmatory testing), and a formal survey. Within two days they were contacted by phone for post-test counseling.
Figure 1.
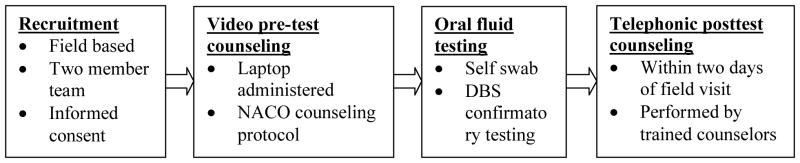
Field testing package (FTP) procedural flow
Video pre-test counseling development and implementation
Two pre-test counseling videos were developed and tailored to either MSM or truck drivers. The videos explained what HIV is, transmission facts, how to prevent getting infected, the importance of being tested, options for HIV testing, and follow up for positive or negative test results. Additionally, oral fluid sampling technique was depicted in the videos. The script was developed first in English, then translated from English to Hindi and Telugu and back-translated into English to check for accuracy. For each video, members of the target group helped to choose actors who would appeal to program participants. The video was filmed by a professional crew and the actors filmed Hindi and Telugu versions. The video depicted a pre-test counseling dialog between a counselor and an MSM or truck driver, and covered all NACO recommended pre-test counseling content for government HIV testing counselors (National AIDS Control Organization, 2007c). The full content is available by request from the lead author. The video was played on a laptop at field locations, with headphones provided if necessary. Participants had the opportunity to ask the research assistant questions about HIV or the oral sampling procedure and a 24 hour phone counselor was available for additional information or counseling support. This technique ensured that all participants received standardized pre-test counseling information through the video, while allowing the counselors to focus on responding to participants’ unique questions and concerns.
HIV testing implementation
Oral fluid was self-collected using the OraQuick oral fluid collection device (OraQuick ADVANCE® HIV-1/2, OraSure, USA) according to manufacturer’s instructions. This rapid test detects both HIV-1 and HIV-2 without distinguishing between the two. Because of the lack of confidentiality in most field settings, it was decided that oral fluid test results would not be provided to study participants in the field, but would be given by phone within two days. In addition, dry blood spots (DBS) were collected using a validated finger prick method with a safety lancet and prepared on Whatman No. 3 paper according to procedures utilized previously (Schneider et al., 2010b). Confirmatory testing was conducted according to NACO guidelines (National AIDS Control Organization, 2007a, 2007c, 2007d) with three consecutive ELISAs. DBS were processed with the following kits utilized: Vironostika HIV Uni-Form Ag/Ab, bioMerieux, France; Vidas HIV Duo Ultra; bioMerieux, France; and HIV Tridot; J. Mitra, New Delhi, India (Dandona, Lakshmi, Sudha, Kumar, & Dandona, 2006; Lakshmi, Sudha, Bhanurekha, & Dandona, 2007; Lakshmi et al., 2009). When results from oral and DBS testing were discordant, qualitative PCR (Amplicor 1.5; Roche Molecular Diagnostics, Branchburg, USA) was performed. Each study participant was assigned an identifying code, to which preliminary oral and confirmatory DBS test results were linked.
Survey
Survey items were adapted from previous HIV prevention surveys in this setting and population (Dandona, et al., 2005; Dandona, et al., 2006; Schneider, et al., 2010b). Sociodemographic information included age, education, marital status, income, and neighborhood or town of residence. Sexual behavior/sexual partner history included number of male and female sex partners, MSM identity, and condom use with last partner. HIV testing history included questions about the time, location, and cost of previous HIV tests, as well as facilitators and barriers to testing. Study participants were asked about their satisfaction with the video pre-test counseling and oral testing methods, and how they compared to traditional ICTC methods. The surveys were confidentially administered orally at the site of testing by one of 6 trained research assistants each of whom had at least 5 years experience working with these communities.
Telephonic post-test counseling
Study participants who had provided phone numbers were called within 2 days of testing by trained counselors. Those individuals who did not provide a number were instructed to call the counselor or come into the PEPFAR/CDC-GAP affiliated clinic to receive their results and post-test counseling. Telephonic post-test counseling content was conducted according to NACO guidelines (National AIDS Control Organization, 2007a, 2007c, 2007d). At the time of testing, a unique question and answer was created for each participant to ensure that counselors could properly identify the study participants when they called. For example, a question could be “what color shirt were you wearing on the day of the interview?” Once the participant’s identity was confirmed, the counselor provided post-test counseling and preliminary oral fluid test results. Preliminary positive study participants were referred to government ICTCs for confirmatory HIV testing, CD4+ lymphocyte testing, and appropriate treatment if necessary. They were given the contact information for the ICTC location that was most convenient for them. If dry blood spot test results subsequently contradicted oral fluid test results, participants were contacted by counselors (0.51% of cases), and referred once again to a government ICTC. If the counselor was not able to get in touch with the participant when they called, the reason for failure was recorded and three total attempts were made.
Data analysis
Descriptive characteristics of MSM and truck drivers were examined using bivariate analyses. All continuous outcomes were categorized, allowing the statistical significance of the groups to be tested by Fisher’s exact or the chi-square test. These tests were also used for comparisons of MSM and truck drivers as well as HIV seropositive vs. seronegative participants. The logistic regression analysis with an enter method was used to verify potential factors influencing participants opinions on which pre-test counseling method was better and their rates of phone counseling completion. The logistic regression included all variables that were significant in bivariate analysis at p<0.05. The model included age, education, marital status, income, whether they had been previously tested, risk group, and the interaction between risk group and previous testing. Two sided p-values< 0.05 were accepted as statistically significant. All statistical analyses were performed using PASW (Predictive Analytics SoftWare) statistics version 18.0 (IBM Corp., Somers, NY, USA).
Ethics statement
Procedures and protocols were approved by institutional review boards at the University of Chicago and SHARE-India. All study participants provided written informed consent at enrollment. This study conformed to the Declaration of Helsinki.
RESULTS
Participant characteristics
A total of 298 MSM and 300 truck drivers participated in the study, and all study participants completed HIV testing. Through a convenience sampling method, an estimated 62% of MSM and 89% of truck-drivers who were approached by study staff agreed to participate. Nearly half of study participants (48.3%) were under 25 years of age (Table 1). Truck drivers were less likely to have higher education, with 5.0% of truck drivers completing more than high school vs. 26.2% of MSM (p<0.001). The majority of truck drivers (53.7%) and 34.2% of MSM were married (p<0.001).
Table 1.
Characteristics of truck drivers and men who have sex with men completing an HIV Field Testing Package in Southern India (n=598).
| All Participants N (%) | Truck Drivers (n=300) N (%)‡ | MSM (n=298) N (%)§ | P-value | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Age | 0.21 | |||
| ≤25 | 288 (48.3) | 150 (50) | 138 (46.6) | |
| 26–35 | 203 (34.1) | 94 (31.3) | 109 (36.8) | |
| 36–45 | 84 (14.1) | 48 (16.0) | 36 (12.2) | |
| >45 | 21 (3.5) | 8 (2.7) | 13 (4.4) | |
| Education | < 0.001 | |||
| None or primary | 202 (34.0) | 117 (39.0) | 85 (28.9) | |
| Some high school | 300 (50.5) | 168 (56.0) | 132 (44.9) | |
| More than high school | 92 (15.5) | 15 (5.0) | 77 (26.2) | |
| Marital status | < 0.001 | |||
| Unmarried* | 333 (56.0) | 139 (46.3) | 194 (65.8) | |
| Married | 262 (44.0) | 161 (53.7) | 101 (34.2) | |
| Monthly Income (INR($US)) | ||||
| ≤3000 ($75) | 175 (29.4) | 97 (32.3) | 78 (26.4) | 0.17 |
| 3001–5000 ($75–125) | 198 (33.3) | 101 (33.7) | 97 (32.9) | |
| >5000 (>$125) | 222 (37.3) | 102 (34.0) | 120 (40.7) | |
| Risk factors | ||||
| Ever had sex with a woman | 363 (61.1) | 237 (79.0) | 126 (42.9) | < 0.001 |
| Used a condom at last sex | 120 (33.6) | 90 (38.3) | 30 (24.6) | 0.006 |
| Number of female sex partners in last 3 months | ||||
| ≤1 | 257 (72.2) | 176 (74.6) | 81 (67.5) | 0.005 |
| 2 | 48 (13.5) | 36 (15.3) | 12 (10.0) | |
| >2 | 51 (14.3) | 24 (10.2) | 27 (22.5) | |
| Ever had sex with a man | 297 (50.2) | 3 (1.0) | 294 (100.0) | -- |
| Used a condom last sex | 216 (74.2) | -- | 216 (74.2) | -- |
| Number of male sex partners in the last week | -- | |||
| ≤2 | 97 (33.2) | -- | 97 (33.2) | |
| 3–5 | 108 (37.0) | -- | 108 (37.0) | |
| >5 | 87 (29.8) | -- | 87 (29.8) | |
| Alcohol before sex | -- | |||
| Usually | 41 (8.7) | 13 (7.3) | 28 (9.7) | 0.004 |
| Sometimes | 264 (56.3) | 118 (65.9) | 146 (50.3) | |
| Never | 164 (35.0) | 48 (26.8) | 116 (40.0) | |
| HIV Testing | ||||
| Ever tested | < 0.001 | |||
| Yes | 259 (43.3) | 84 (28.0) | 175 (58.7) | |
| No | 339 (56.7) | 216 (72.0) | 123 (41.3) | |
| Previous HIV test | ||||
| Within the past month | 60 (23.3) | 30 (36.1) | 30 (17.1) | 0.003 |
| Within the past six months | 79 (30.6) | 17 (20.5) | 62 (35.4) | |
| Within the past year | 48 (18.6) | 17 (20.5) | 31 (17.7) | |
| More than a year ago | 71 (27.4) | 19 (22.9) | 52 (29.5) | |
| Test location | ||||
| Private clinic/hospital | 77 (30.0) | 55 (66.3) | 22 (12.6) | < 0.001 |
| ICTC/government facility | 128 (49.8) | 10 (12.0) | 118 (67.8) | |
| NGO facility/study site | 45 (17.5) | 18 (21.7) | 27 (15.5) | |
| More than one location | 7 (2.7) | 0 (0.0) | 7 (4.0) | |
| Why tested | < 0.001 | |||
| Voluntary | 180 (71.4) | 46 (59.7) | 134 (76.6) | |
| Friend’s advice | 19 (7.5) | 3 (3.9) | 16 (9.1) | |
| Doctor’s advice | 34 (13.5) | 14 (18.2) | 20 (11.4) | |
| Other | 19 (7.5) | 14 (18.2) | 5 (2.9) | |
| Results collected | 0.001 | |||
| Yes | 225 (87.2) | 63 (75.9) | 162 (92.6) | |
| No | 33 (12.8) | 20 (24.1) | 13 (7.4) | |
| Results status | ||||
| Positive | 10 (4.4) | 1 (1.6) | 9 (5.6) | 0.363 |
| Negative | 211 (93.4) | 67 (95.3) | 150 (92.6) | |
| Indeterminate† | 5 (2.2) | 2 (3.1) | 3 (1.9) | |
Includes unmarried, separated, divorced, and widowed
Includes indeterminate, do not know, and refused to answer
Data missing for truck drivers: 2 for condom with women, 1 for number of women, 121 for alcohol before sex, 1 for last HIV test time, 1 for test location, 7 for why tested, 1 for results collected, 14 for results status
Data missing for MSM: 2 for age, 4 for education, 3 for marital status, 3 for income, 4 for ever had sex with a woman, 2 for condom with a woman, 4 for number of women, 4 for ever had sex with a man, 3 for condom with a man, 2 for number of men, 8 for alcohol before sex, 1 for test location, 13 for results status. Two men were excluded from the analysis as they were found to not meet eligibility criteria.
HIV testing history and test results
Previous HIV testing was reported among 83 (27.7%) truck drivers and 175 (58.7%) MSM; 55 (66.3%) of the previously tested truck drivers reported testing at a private facility and 118 (67.8%) of the MSM reported testing at a government ICTC. Truck drivers were less likely to previously receive their results compared to MSM; 63 (75.9%) vs. 162 (92.6%) respectively (p<0.001). HIV prevalence was 1.3% for truck-drivers and 26.1% for MSM. Of all participants testing positive, 79 individuals (93.7%) were HIV positive unaware; they had either tested negative previously or this was their first test. These new positives included 72 (24.7%) MSM and 3 (1.0%) truck drivers. OraQuick sensitivity was 98.7% (95% CI: 92.3–99.9) and specificity was 99.6% (95% CI 98.4–99.9) when compared to the 3 ELISA confirmatory tests.
FTP preferences and follow-up
Video pre-test counseling was completed by 484 (80.9%) participants. Bivariate analysis showed that nearly all of those who completed video counseling (98.8%) rated it as good or very good; however 277 (57.7%) rated face-to-face counseling as a better method (Table 2). Truck drivers were more likely than MSM to rate the video counseling as better than or as good as face-to-face pre-test counseling (OR: 0.29, 95% CI: 0.20–0.43), while those who had received HIV testing previously tended to prefer face-to-face counseling to video (OR: 0.61, 95% CI: 0.42–0.88). Oral testing was deemed to be comfortable or very comfortable by 576 (97,5%) participants, while 581 (98.6%) said they were likely or very likely to recommend it to a friend. While 486 participants were able to give phone numbers to the counselors, 349 (58.4%) completed telephonic post-test counseling (Table 3), with those previously tested more likely to complete it (OR: 1.66, 95% CI: 1.19–2.31). This included 44 of those who were receiving their first diagnosis (59.5%). Participants who had tested negative at their last HIV test were also more likely to receive their results compared to those who had tested positive (OR: 4.67, 95% CI: 1.18–18.51). The most common reason why telephonic post-test counseling could not be completed was that the participant’s phone was switched off; this was the case for 46.9% of these participants. Those who had never been tested before were more likely to have their phones switched off compared to those who had been previously tested (OR: 2.83, 95% CI 1.21 to 6.62). Furthermore, of the 349 who completed telephonic post-test counseling, 335 (99.7%) participants rated the phone counseling as good or very good. Fifteen (33.3%) of those who tested positive for the first time during this study had a confirmed visit to an ICTC following receipt of their results. Of those with CD4 counts available at 3 months, the mean CD4 count was 451 cells/mm3 (range: 175–640).
Table 2.
Satisfaction with Field Testing Package components by risk group and HIV testing history (n=598).
| MSM N (%) | Truck Drivers N (%) | OR for MSM vs. Truck Drivers‡ (95% CI) | Previously Tested N (%) | Never Tested N (%) | OR for Previously tested vs. never tested‡ (95% CI) | |
|---|---|---|---|---|---|---|
| Video pre-test counseling | ||||||
| Video rated as good or very good | 230 (97.5) | 248 (100.0) | -- | 202 (99.0) | 276 (98.6) | 1.46 (0.27–8.07) |
| Best method is video or methods are equal | 64 (27.5) | 139 (56.3) | 0.29 (0.20–0.43)* | 71(35.3) | 132 (47.3) | 0.61 (0.42–0.88)† |
| Oral Test | ||||||
| Comfortable | 288 (98.3) | 288 (96.6) | 2.00 (0.68–5.92) | 249 (97.3) | 327 (97.6) | 0.87 (0.31–2.43) |
| Advantages§ | ||||||
| Good, nice, new or interesting | 23 (7.9) | 45 (15.3) | 0.03 (0.02–0.07)* | 18 (7.2) | 50 (15.0) | 0.26 (0.14–0.48)* |
| No blood/pain or comfortable | 14 (4.8) | 25 (8.5) | 0.04 (0.02–0.09) * | 16 (6.4) | 23 (6.9) | 0.50 (0.25–1.01) |
| Easy, quick, or flexible | 38 (13.1) | 86 (29.3) | 0.03 (0.02–0.06) * | 48 (19.1) | 76 (22.8) | 0.46 (0.29–0.72)† |
| Multiple answers | 36 (12.4) | 126 (42.9) | 0.02 (0.01–0.04)* | 58 (23.1) | 104 (31.2) | 0.40 (0.26–0.62)* |
| Recommend to a friend | ||||||
| Very likely/likely | 286 (97.9) | 295 (99.3) | 0.32 (0.07–1.61) | 251 (98.8) | 330 (98.5) | 1.27 (0.30–5.35) |
| Rating of telephonic counseling | ||||||
| Good or very good | 172 (100.0) | 163 (99.4) | -- | 163 (99.4) | 172 (100.0) | -- |
p<0.001
p<0.05
Reference group: no advantages listed
Table 3.
Telephonic post-test counseling for MSM and truck drivers (n=598) and by HIV serostatus (n=586).*
| Truck drivers N (%) | MSM N (%) | OR for MSM vs. Truck Driver (95% CI) | Previously tested N (%) | Never tested N (%) | OR for Previously tested vs. Never tested (95% CI) | |
|---|---|---|---|---|---|---|
| Phone counseling completed | 167 (55.7) | 182 (61.1) | 1.25 (0.90–1.73) | 169 (65.3) | 180 (53.1) | 1.66 (1.19–2.31) † |
| Reason not completed (on last attempt) § | ||||||
| Switched off | 64 (50.0) | 11 (34.4) | 0.88 (0.34–2.29) | 11 (28.2) | 64 (52.9) | 0.35 (0.15–0.83) † |
| Person not available/Number busy/rejected/no answer | 18 (14.1) | 12 (37.5) | 3.41 (1.23–9.47) † | 10 (25.6) | 20 (16.5) | 1.03 (0.40–2.65) |
| Confirmed visit to government center|| | 0 (0.0) | 18 (10.2) | -- | 12 (7.2) | 6 (3.4) | 2.19 (0.80–5.99) |
| CD4 count | ||||||
| ≤350 | 0 (0.0) | 4 (26.7) | -- | 3 (30.0) | 1 (20.0) | -- |
| 351–550 | 0 (0.0) | 6 (40.0) | -- | 3 (30.0) | 3 (60.0) | -- |
| >550 | 0 (0.0) | 5 (33.3) | -- | 4 (40.0) | 1 (20.0) | -- |
Excludes participants with equivocal results
p<0.05
Reference group: wrong number/disconnected. Number missing out of those who did not complete counseling: 5 truck drivers, 84 MSM, 51 previously tested, 39 never tested.
Number missing out of those who did complete counseling: 1 truck driver, 5 MSM, 2 previously tested, 4 never tested
Number missing out of those who had confirmed visits to government centers: 3 MSM, 3 positives, 2 previously tested, 5 never tested
In logistic regression analysis, a previous HIV test was associated with preference for video pre-test counseling or rating it as equal to face-to-face counseling, as well as with completing telephonic post-test counseling (Table 4). There was a significant interaction between male risk group and previous HIV testing, such that the odds of preferring video counseling or both video and face-to-face counseling was significantly lower for MSM who had a previous HIV test than those who had not been tested (OR: 0.11, 95% CI: 0.04–0.26). There was also evidence that participants with higher education, including greater than high school, were more likely to have completed telephonic post-test counseling (OR: 2.35, 95% CI: 1.33–4.16).
Table 4.
Relationship between participant characteristics, pre-test counseling methods and completion of post-test telephonic counseling*
| Best pre-test counseling method is video or both† (n=478) OR (95% CI) | Phone Counseling Completed (n=594) OR (95% CI) | |
|---|---|---|
| Age | ||
| ≤25 | 1.00 (ref) | 1.00 (ref) |
| 26–35 | 1.04 (0.64–1.70) | 1.01 (0.67–1.53) |
| 36–45 | 1.15 (0.58–2.26) | 0.94 (0.53–1.65) |
| >45 | 0.82 (0.28–2.41) | 0.73 (0.28–1.88) |
| Education | ||
| None or primary | 1.00 (ref) | 1.00 (ref) |
| Some high school | 1.20 (0.77–1.85) | 1.55 (1.07–2.24)§ |
| More than high school | 1.03 (0.51–2.05) | 2.35 (1.33–4.16)§ |
| Marital status | ||
| Unmarried | 1.00 (ref) | 1.00 (ref) |
| Married | 1.07 (0.67–1.70) | 1.34 (0.90–2.0) |
| Income | ||
| ≤ 3000 | 1.00 (ref) | 1.00 (ref) |
| 3001–5000 | 0.95 (0.58–1.58) | 1.55 (1.01–2.38)§ |
| > 5000 | 0.83 (0.49–1.39) | 1.33 (0.86–2.04) |
| Previous HIV test | ||
| No | 1.00 (ref) | 1.00(ref) |
| Yes | 2.95 (1.53–5.69)§ | 2.04 (1.19–3.50)§ |
| Group | ||
| Truck driver | 1.00 (ref) | 1.00 (ref) |
| MSM | 0.74 (0.44–1.26) | 1.16 (0.73–1.87) |
| Previous HIV test by Group | ||
| Previous HIV tested MSM | 0.11 (0.04–0.26)|| | 0.68 (0.33–1.41) |
Logistic regression model includes the following variables: age, education, marital status, income, whether they had been previously tested, risk group, and the interaction between risk group and previous testing
Includes those who rated video pre-test counseling as better than face-to-face and those who rated the two methods as equally good.
p<0.05
p<0.001
DISCUSSION
This study evaluated whether a novel field testing package (FTP) that combined three HIV testing and counseling methods would be a feasible and acceptable way to increasing HIV testing and receipt of results among high-risk Indian men. Our results confirm that men reached through this intervention were at high-risk for HIV, yet many of them were not utilizing government testing facilities. Less than half of participants had ever been tested for HIV and of these, half had chosen to do so outside of government centers. ICTCs are reaching many MSM and truck drivers, but it is important to connect the remaining high risk men to ICTCs through more targeted outreach that will bridge the gap between ICTC services and more hesitant high risk men. Additionally, more than 90% of those who tested positive were HIV positive unaware, which indicates that the high-risk men who are not being reached by existing programs have a high seroprevalence and it is therefore important to develop testing programming that targets these individuals. Truck-drivers were disproportionately under-tested with less than one-third ever having been tested prior to our study. Overall, these figures indicate that, despite their high seroprevalence, many Indian MSM and truck drivers are not being reached by traditional counseling and testing methods.
The three components of the FTP were found to be highly acceptable among participants. First, participants were overall very enthusiastic about oral rapid testing, describing it as painless, simple and fast. Those who were hesitant to undergo testing tended to be uncomfortable with the need for confirmatory blood spot testing rather than the oral test itself. In the future we envision rapid testing being implemented as a preliminary test with on-site confirmatory testing being replaced by patient referral to government ICTCs for confirmatory testing. Thus painless and convenient oral rapid tests should make high-risk men significantly more willing to undergo testing.
Second, video counseling was rated as good or very good by nearly all participants. Logistic regression analysis of specific groups, however, demonstrated that those who had been previously tested were less likely to prefer video counseling than those who had not been tested, while truck-drivers and MSM were equally likely to prefer video counseling. Within MSM, those who had been previously tested were particularly likely to prefer traditional face-to-face pre-test counseling to video counseling. It is possible that those who had not been tested preferred video counseling more than those who had been previously tested because they had not felt comfortable enough with face-to-face counseling at an ICTC to get tested, thus they welcomed the more anonymous video counseling method. The previously tested men who tended to prefer face-to-face counseling may have been more outgoing and comfortable talking about the testing process with a counselor. Pre-test counseling has variable acceptability among different high-risk male sub-populations and requires further work to better understand why such differences exist. Although acceptability of video counseling was high in this study, feasibility was limited. While nearly all participants rated the video counseling as good, and many found the new technology exciting, it was only fully implemented among 81.9% of participants due to a delay in video production, issues with privacy and security at the field testing sites and limited laptop battery life in the field. In the future, counseling and testing could occur in a private space near the recruitment sites where the equipment would be more secure, participants would have more privacy, a reliable power source would be available, and the video would be easier to hear. Optional group viewing of the pre-test counseling video could also speed up the testing process, and be followed by individual sessions with counselors in which any questions could be addressed. These changes to protocol would not only make video pre-test counseling more feasible, it might also decrease the numbers of participants who prefer face-to-face counseling.
This was the first study in India where participants were provided with HIV test results telephonically. Telephonic post-test counseling was very well received by the participants who completed it; however rates of completion were fairly low at 54.8%. Those who reported previous HIV testing were more likely to complete post-test counseling, perhaps because they were more engaged in their healthcare and therefore worked to receive their results. However, those who had previously received a positive HIV test result were less likely to obtain their results than those who had tested negative, perhaps because they already believed that they had HIV and therefore did not need their results. Our rate of completed phone counseling is lower than in other studies of telephonic post-test counseling (McKinstry, et al., 2007; Tsu, et al., 2002), which can be attributed to three major factors. First, our unique field site recruitment strategy meant that the majority of our patients were not seeking testing and therefore were likely less independently motivated to receive results than those who self-initiate testing by presenting to non-mobile testing centers. Second, cell phones are still an emerging technology in India, with most plans being “prepaid”. More than one sixth of participants were not able to provide a number at which they could be reliably reached, and instead had to agree to contact the counselors themselves. Furthermore, in populations of lower economic strata, pre-paid phone plans may lead to phones being off or not in service due to inability to pay, which makes it hard to contact even those participants who do have their own phones. This socioeconomic association with phone function is supported by the fact that individuals with lower incomes and less education tended to be less likely to receive their results. Third, low phone counseling rates may have been caused by participants screening their calls for unrecognized numbers. Although our rates of post-test counseling are lower than those in other telephonic post-test counseling studies, they are comparable to other field-based studies with MSM in the United States (Prachand & Skaathun, 2008). Further studies could directly compare face-to-face and telephonic post-test counseling in such field settings, while more extensive partnerships with NGOs and CBOs that work with study participants could help increase receipt of results. In the future, field settings with increased privacy could have trained counselors give rapid test results in person onsite as soon as results are available, thereby decreasing loss to follow up.
One of the primary goals of the FTP was to identify men who tested positive with the preliminary oral test in order to connect them to government counseling and testing centers. We were only able to confirm that one third of those who tested positive for the first time had followed up at an ICTC, due to our inability to confirm the visits with the ICTCs and the short duration of the study. In the future, field based rapid testing programs could improve follow up by working more closely with the ICTCs to confidentially share information about follow up visits. Currently several CBOs are able to refer clients to government ICTCs and receive written confirmation of whether the referral was completed, so such information sharing is feasible. Of those positive individuals who did have a confirmed visit, the mean CD4 count was 451, which suggests that, for those who followed up, the disease had not progressed and was still above the local threshold for initiating treatment. Therefore the study successfully identified individuals who did not know they were seropositive and did so early enough in their disease course to allow effective treatment. Our study had five important limitations. First, we used a convenience sample, and reasons for non-participation were not collected. However, in line with other work with these same populations in the field, the predominant reason for non participation would likely be individuals claiming to be “too busy”(Hemmige, et al., 2011; Schneider, et al., 2010a; Schneider, et al., 2011a; Schneider et al., 2011b). Second, the majority of responses to questions about acceptability were strongly positive, limiting comparisons across participant characteristics. Such levels of acceptability were comparable to other studies where acceptability was measured for components of the FTP, such as studies of oral testing in northern India (Pant Pai, et al., 2007). This may be due to social desirability bias, and differences in response to survey items between international settings require further investigation. Third, we were unable to determine whether many of those who tested preliminary positive did in fact follow-up at a government center. Strong partnerships with government care centers may not completely remedy this situation as clients may follow-up with care at a non-partnering government center, use a different name, or seek care in the private sector. Efforts by the government to provide a unique identifier and track HIV infected patients may help stakeholders understand the flow of patients from field-based HIV testing programs to follow up care. In the future, willing participants with government identification cards could consent to be enrolled in this system to track follow-up, however this would not be required to participate in the FTP. Fourth, rates of completed phone counseling and follow up to ICTCs were low. In the future, more readily available cell phone technology and more cooperation between ICTCs and NGOs may make follow-up less challenging. Fifth, aggregate analyses could not entirely explain the differences in preferences and follow-up between different subgroups. Sub-analyses within different groups were, however, performed and components of FTP were tailored to specific cultural and situational factors affecting both populations (e.g., pre-test video counseling). The reasons for these differences must be further investigated.
In summary, this study demonstrates that a field test package including video pre-test counseling, oral rapid testing, and telephonic post-test counseling was quite acceptable among high-risk South Indian men. Implementation gaps in the form of limited completion of video pre-test counseling, telephonic post-test counseling, and unknown linkage to care rates must be addressed before the FTP can be implemented on a wider scale. Less than half of the high-risk men tested in this study reported a previous HIV test, and of those testing positive, more than 90% were HIV positive unaware. In combination with recent changes to Indian law that decriminalized homosexuality, and efforts to provide testing at mandatory driver licensing centers, the FTP, could help erode many of the structural barriers to HIV testing and treatment for high-risk Indian men. Further program implementation could include testing and counseling in private locations near field recruitment sites, collaboration with local NGOs and clinics to ensure post-test counseling, and cooperation with government ICTCs to ensure that HIV infected persons are connected to treatment.
Acknowledgments
We would like to thank our partners including Darpan, Suraksha and the Gati Corporation. We would also like to thank all of the study participants for their participation and for OraSure for providing test kits.
Footnotes
This work was presented in part as an oral presentation at the 18th International AIDS Conference, Vienna Austria, 18–23 July 2010 and was supported in part by the American Foundation for AIDS Research (amFAR), the National Institutes of Health (KL2RR025000).
References
- Alemagno SA, Stephens RC, Stephens P, Shaffer-King P, White P. Brief motivational intervention to reduce HIV risk and to increase HIV testing among offenders under community supervision. J Correct Health Care. 2009;15(3):210–221. doi: 10.1177/1078345809333398. [DOI] [PubMed] [Google Scholar]
- Asthana S, Oostvogels R. The social construction of male ‘homosexuality’ in India: implications for HIV transmission and prevention. Soc Sci Med. 2001;52(5):707–721. doi: 10.1016/s0277-9536(00)00167-2. [DOI] [PubMed] [Google Scholar]
- Bachani D, Sogarwal R. National Response to HIV/AIDS in India. Indian Journal of Community Medicine. 2010;35(4):469–472. doi: 10.4103/0970-0218.74341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bill & Melinda Gates Foundation. Off the Beaten Track: Avahan’s Experience in the Business of Prevention among India’s Long-Distance Truckers. 2008 Retrieved August 12, 2011, from http://www.gatesfoundation.org/avahan/Documents/Avahan_OffTheBeatenTrack.pdf.
- Bill & Melinda Gates Foundation. Meeting the Challenge. 2011 Retrieved February 9, 2011, from http://www.gatesfoundation.org/avahan/Pages/meeting-the-challenge.aspx.
- Calderon Y, Haughey M, Leider J, Bijur PE, Gennis P, Bauman LJ. Increasing willingness to be tested for human immunodeficiency virus in the emergency department during off-hour tours: a randomized trial. Sex Transm Dis. 2007;34(12):1025–1029. doi: 10.1097/OLQ.0b013e31814b96bb. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Rapid HIV testing among racial/ethnic minority men at gay pride events--nine U.S. cities, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56(24):602–604. [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M. Secondary HIV prevention among kothi-identified MSM in Chennai, India. Cult Health Sex. 2008;10(4):313–327. doi: 10.1080/13691050701816714. [DOI] [PubMed] [Google Scholar]
- Chandrasekaran P, Dallabetta G, Loo V, Rao S, Gayle H, Alexander A. Containing HIV/AIDS in India: the unfinished agenda. The Lancet Infectious Diseases. 2006;6(8):508–521. doi: 10.1016/S1473-3099(06)70551-5. [DOI] [PubMed] [Google Scholar]
- Chen MY, Bilardi JE, Lee D, Cummings R, Bush M, Fairley CK. Australian men who have sex with men prefer rapid oral HIV testing over conventional blood testing for HIV. Int J STD AIDS. 2010;21(6):428–430. doi: 10.1258/ijsa.2010.009552. [DOI] [PubMed] [Google Scholar]
- Cornman DH, Schmiege SJ, Bryan A, Benziger TJ, Fisher JD. An information-motivation-behavioral skills (IMB) model-based HIV prevention intervention for truck drivers in India. Soc Sci Med. 2007;64(8):1572–1584. doi: 10.1016/j.socscimed.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandona L, Dandona R, Gutierrez JP, Kumar GA, McPherson S, Bertozzi SM, et al. Sex behaviour of men who have sex with men and risk of HIV in Andhra Pradesh, India. AIDS. 2005;19(6):611–619. doi: 10.1097/01.aids.0000163938.01188.e4. [DOI] [PubMed] [Google Scholar]
- Dandona L, Lakshmi V, Sudha T, Kumar GA, Dandona R. A population-based study of human immunodeficiency virus in south India reveals major differences from sentinel surveillance-based estimates. BMC Medicine. 2006;4(1):31. doi: 10.1186/1741-7015-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erausquin JT, Duan N, Grusky O, Swanson AN, Kerrone D, Rudy ET. Increasing the reach of HIV testing to young Latino MSM: results of a pilot study integrating outreach and services. J Health Care Poor Underserved. 2009;20(3):756–765. doi: 10.1353/hpu.0.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go VF, Srikrishnan AK, Sivaram S, Murugavel GK, Galai N, Johnson SC, et al. High HIV prevalence and risk behaviors in men who have sex with men in Chennai, India. J Acquir Immune Defic Syndr. 2004;35(3):314–319. doi: 10.1097/00126334-200403010-00014. [DOI] [PubMed] [Google Scholar]
- Gutierrez JP, McPherson S, Fakoya A, Matheou A, Bertozzi SM. Community-based prevention leads to an increase in condom use and a reduction in sexually transmitted infections (STIs) among men who have sex with men (MSM) and female sex workers (FSW): the Frontiers Prevention Project (FPP) evaluation results. BMC Public Health. 2010;10:497. doi: 10.1186/1471-2458-10-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy R, Goller J, Leslie D, Thorpe R, Grierson J, Batrouney C, et al. No increase in HIV or sexually transmissible infection testing following a social marketing campaign among men who have sex with men. J Epidemiol Community Health. 2009;63(5):391–396. doi: 10.1136/jech.2008.077099. [DOI] [PubMed] [Google Scholar]
- Hemmige V, Snyder H, Liao C, Mayer K, Lakshmi V, Gandham SR, et al. Sex Position, Marital Status, and HIV Risk Among Indian Men Who Have Sex with Men: Clues to Optimizing Prevention Approaches. AIDS Patient Care STDS. 2011 doi: 10.1089/apc.2011.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson AB, Branson BM, Kim A, Farnham PG. A meta-analysis of the effectiveness of alternative HIV counseling and testing methods to increase knowledge of HIV status. AIDS. 2006;20(12):1597–1604. doi: 10.1097/01.aids.0000238405.93249.16. [DOI] [PubMed] [Google Scholar]
- International Institute for Population Sciences. National Family Health Survey, India. 2007;1 Ch. 12. Retrieved August 8, 2011, from http://www.nfhsindia.org/NFHS-3%20Data/VOL-1/Chapter%2012%20-%20HIV%20Prevalence%20(422K).pdf. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Estimated number of people living with HIV by country. 2008 Retrieved August 24, 2011, from http://data.unaids.org/pub/GlobalReport/2008/20080818_gr08_plwh_1990_2007_en.xls.
- Kumar SG, Dandona R, Schneider JA, Ramesh YK, Dandona L. Outputs and cost of HIV prevention programmes for truck drivers in Andhra Pradesh, India. BMC Health Serv Res. 2009;9:82. doi: 10.1186/1472-6963-9-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakshmi V, Sudha T, Bhanurekha M, Dandona L. Evaluation of the Murex HIV Ag/Ab Combination assay when used with dried blood spots. Clin Microbiol Infect. 2007;13(11):1134–1136. doi: 10.1111/j.1469-0691.2007.01809.x. [DOI] [PubMed] [Google Scholar]
- Lakshmi V, Sudha T, Dandona R, Teja VD, Kumar GA, Dandona L. Application of human immunodeficiency virus type 1 BED enzyme immunoassay on dried blood spots in India. J Med Microbiol. 2009;58(Pt 3):312–317. doi: 10.1099/jmm.0.005249-0. [DOI] [PubMed] [Google Scholar]
- Liang TS, Erbelding E, Jacob CA, Wicker H, Christmyer C, Brunson S, et al. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDS. 2005;19(4):253–257. doi: 10.1089/apc.2005.19.253. [DOI] [PubMed] [Google Scholar]
- McKinstry LA, Goldbaum GM, Meischke HW. Telephone notification of HIV test results: impact in King County, Washington. Sex Transm Dis. 2007;34(10):796–800. doi: 10.1097/01.olq.0000261726.56859.5a. [DOI] [PubMed] [Google Scholar]
- Merchant RC, Gee EM, Clark MA, Mayer KH, Seage GR, 3rd, Degruttola VG. Comparison of patient comprehension of rapid HIV pre-test fundamentals by information delivery format in an emergency department setting. BMC Public Health. 2007;7:238. doi: 10.1186/1471-2458-7-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDS Control Organization. Guidelines on HIV Testing. 2007a Retrieved August 12, 2011, from http://www.nacoonline.org/Quick_Links/Publication/Blood_Safety__Lab_Services/Operational__Technical_guidelines_and_policies/Guidelines_for_HIV_test/
- National AIDS Control Organization. Integrated Counselling and Testing Centre. 2007b Retrieved August 8, 2011, from http://nacoonline.org/National_AIDS_Control_Program/Services_for_Prevention/Integrated_Counselling_and_Testing__ICT/
- National AIDS Control Organization. Operational Guidelines for Integrated Counselling and Testing Centres. 2007c Retrieved August 8, 2011, from http://nacoonline.org/upload/Final%20Publications/Operational%20Guidelines%20for%20Integrated%20Counseling%20and%20Testing%20Centres.pdf.
- National AIDS Control Organization. Targeted Interventions Under NACP III: Operational Guidelines. 2007d Retrieved August 12, 2011, from http://nacoonline.org/Quick_Links/Publication/NGO__Targeted_Interventions/Operational__Technical_guidelines_and_policies/
- National AIDS Control Organization, & National Institute of Medical Sciences. Technical Report: India HIV Estimates 2006. 2006 Retrieved August 23, 2011, from http://www.nacoonline.org/upload/NACO%20PDF/Technical%20Report%20on%20HIV%20Estimation%202006.pdf.
- Naz Foundation v. NCT of Delhi, Delhi High Court (2009).
- OraSure Technologies, I. OraQuick ADVANCE® Rapid HIV-1/2 Antibody Test [Package Insert] Bethlehem, PA: 2007. [Google Scholar]
- Pant Pai N. Rapid oral fluid-based point-of-care HIV testing: applicability in developing countries. Indian J Med Res. 2007;126(3):171–173. [PubMed] [Google Scholar]
- Pant Pai N, Barick R, Tulsky JP, Shivkumar PV, Cohan D, Kalantri S, et al. Impact of round-the-clock, rapid oral fluid HIV testing of women in labor in rural India. PLoS Med. 2008;5(5):e92. doi: 10.1371/journal.pmed.0050092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant Pai N, Joshi R, Dogra S, Taksande B, Kalantri SP, Pai M, et al. Evaluation of diagnostic accuracy, feasibility and client preference for rapid oral fluid-based diagnosis of HIV infection in rural India. PLoS One. 2007;2(4):e367. doi: 10.1371/journal.pone.0000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papa L, Seaberg DC, Rees E, Ferguson K, Stair R, Goldfeder B, et al. Does a waiting room video about what to expect during an emergency department visit improve patient satisfaction? CJEM. 2008;10(4):347–354. doi: 10.1017/s1481803500010356. [DOI] [PubMed] [Google Scholar]
- Prachand N, Skaathun B. HIV Prevalence and Unrecognized Infection among Men Who Have Sex with Men in Chicago. 2008 Retrieved August 12, 2011, from http://www.cityofchicago.org/content/dam/city/depts/cdph/statistics_and_reports/MSM2008NHBSsldSet.pdf.
- Schluter WW, Judson FN, Baro’n AE, McGill WL, Marine WM, Douglas JM., Jr Usefulness of human immunodeficiency virus post-test counseling by telephone for low-risk clients of an urban sexually transmitted diseases clinic. Sex Transm Dis. 1996;23(3):190–197. doi: 10.1097/00007435-199605000-00006. [DOI] [PubMed] [Google Scholar]
- Schneider JA, Dandona R, Pasupneti S, Lakshmi V, Liao C, Yeldandi V, et al. Initial commitment to pre-exposure prophylaxis and circumcision for HIV prevention amongst Indian truck drivers. PLoS One. 2010a;5(7):e11922. doi: 10.1371/journal.pone.0011922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Dude A, Dinaker M, Kumar V, Laumann E, Holloway-Beth A, et al. General hygiene, sexual risk behaviour and HIV prevalence in truck drivers from Andhra Pradesh, South India: implications for prevention interventions. Int J STD AIDS. 2009;20:39–45. doi: 10.1258/ijsa.2008.008163. [DOI] [PubMed] [Google Scholar]
- Schneider JA, Kapur A, Schumm P, Laumann E, Rani S, Oruganti G. A novel men who have sex with men (MSM) digital communication network analytic approach: cell phone assisted network detection and identification (CANDID). Paper presented at the 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention; Rome. 2011a. [Google Scholar]
- Schneider JA, Lakshmi V, Dandona R, Kumar GA, Sudha T, Dandona L. Population-based seroprevalence of HSV-2 and syphilis in Andhra Pradesh state of India. BMC Infect Dis. 2010b;10:59. doi: 10.1186/1471-2334-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Michaels S, Gandham SR, McFadden R, Liao C, Yeldandi VV, et al. A Protective Effect of Circumcision Among Receptive Male Sex Partners of Indian Men Who Have Sex with Men. AIDS Behav. 2011b doi: 10.1007/s10461-011-9982-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulden JD, Song B, Barros A, Mares-DelGrasso A, Martin CW, Ramirez R, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep. 2008;123(Suppl 3):101–114. doi: 10.1177/00333549081230S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seña AC, Hammer JP, Wilson K, Zeveloff A, Gamble J. Feasibility and acceptability of door-to-door rapid HIV testing among latino immigrants and their HIV risk factors in North Carolina. AIDS Patient Care STDS. 2010;24(3):165–173. doi: 10.1089/apc.2009.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi A. The Last of the Ustaads. In: Akhavi N, editor. AIDS: Untold Stories from India. New Delhi: Random House India; 2008. pp. 287–309. [Google Scholar]
- Setia MS, Sivasubramanian M, Anand V, Row-Kavi A, Jerajani HR. Married men who have sex with men: the bridge to HIV prevention in Mumbai, India. Int J Public Health. 2010;55(6):687–691. doi: 10.1007/s00038-010-0173-0. [DOI] [PubMed] [Google Scholar]
- Spielberg F, Branson BM, Goldbaum GM, Lockhart D, Kurth A, Celum CL, et al. Overcoming barriers to HIV testing: preferences for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr. 2003;32(3):318–327. doi: 10.1097/00126334-200303010-00012. [DOI] [PubMed] [Google Scholar]
- Spielberg F, Branson BM, Goldbaum GM, Lockhart D, Kurth A, Rossini A, et al. Choosing HIV Counseling and Testing Strategies for Outreach Settings: A Randomized Trial. J Acquir Immune Defic Syndr. 2005;38(3):348–355. [PubMed] [Google Scholar]
- The National Readership Studies Council. NRS 2006 – Key Findings. 2006 Retrieved March 30, 2011, from http://www.hindu.com/nic/nrs.htm.
- The Times of India. Transgenders sans ‘ID proof’ turned away from hospitals. 2010. Retrieved August 14, 2011, from Transgenders sans ‘ID proof’ turned away from hospitals. [Google Scholar]
- Tsu RC, Burm ML, Gilhooly JA, Sells CW. Telephone vs. face-to-face notification of HIV results in high-risk youth. J Adolesc Health. 2002;30(3):154–160. doi: 10.1016/s1054-139x(01)00340-8. [DOI] [PubMed] [Google Scholar]
- U.S. President’s Emergency Plan for AIDS Relief, Center for Disease Control-Global AIDS Program, the University of Chicago, & SHARE-India. Mainstreaming the Public Health Response to HIV in Andhra Pradesh. 2007 from http://www.sharefoundations.org.


