Abstract
We report a case of transient osteoporosis of the hip (TOH) in a 59-year-old man including the clinical presentation, diagnostic studies, management and clinical progress. TOH is a rare self-limiting condition that typically affects middle-aged men or, less frequently, women in the third trimester of pregnancy. Affected individuals present clinically with acute hip pain, limping gait, and limited ranges of hip motion. TOH may begin spontaneously or after a minor trauma. Radiographs are typically unremarkable but MR imaging studies yield findings consistent with bone marrow edema. TOH is referred to as regional migratory osteoporosis if it travels to other joints or the contralateral hip. TOH often resembles osteonecrosis but the two conditions must be differentiated due to different prognoses and management approaches. The term TOH is often used interchangeably and synonymously with transient bone marrow edema.
Keywords: osteoporosis, hip, transient
Abstract
Nous rapportons le cas d’une ostéoporose transitoire de la hanche (OTH) d’un homme de 59 ans avec une présentation clinique, des études diagnostiques, la gestion et les progrès cliniques. L’OTH est une maladie à résolution spontanée rare qui atteint généralement les hommes d’un certain âge ou, moins fréquemment, les femmes lors du troisième trimestre de la grossesse. Les personnes touchées présentent des douleurs aiguës de la hanche, marchent en boitant, et ont une amplitude des mouvements de la hanche limités. L’OTH peut se déclencher spontanément ou après un traumatisme mineur. Les radiographies sont généralement ordinaires mais les études menées sur l’IRM fournissent des résultats compatibles avec un œdème de la moelle osseuse. L’OTH est qualifié d’ostéoporose migratoire régionale si elle se déplace vers d’autres articulations ou vers la hanche controlatérale. L’OTH ressemble à l’ostéonécrose mais les deux conditions doivent être différenciées en raison de pronostics et d’approches de gestion différentes. Le terme OTH est souvent synonyme d’œdème de la moelle osseuse transitoire, et ces deux termes sont souvent employés de manière interchangeable.
Keywords: ostéoporose, hanche, transitoire
Introduction
Transient osteoporosis of the hip (TOH) is a rare self-limiting condition that typically affects middle-aged men or, less commonly, women in the third trimester of pregnancy. These individuals present without a history of major trauma but usually developed an acute onset of hip pain accompanied by decreased ranges of motion, and a limping gait.1–6 Radiographs of TOH are frequently unremarkable, but may display diffuse osteopenia of the femoral head and neck. The affected area appears “warm” on bone scans; however, this test is seldom used due to its low specificity for TOH.1 Computed tomography findings include reduced bone density of the affected area and loss of thickness with continuity of vertical primary compressive trabeculae.2 Magnetic resonance (MR) imaging yields findings consistent with bone marrow edema – low signal intensity of bone marrow on T1-weighted sequences and high signal intensity of bone marrow on fluid-sensitive (T2-weighted and fat-suppressed) sequences.3 The edema affects the subchondral bone of the femoral head and can extend toward the neck and intertrochanteric region. Unlike osteonecrosis, TOH does not result in collapse, fragmentation, or remodeling of the cortical bone of the femoral head nor does it progress to arthritis.1
Cases of TOH have been reported with and without the co-existent presence of subchondral stress fractures of the femoral head.1–4 The susceptibility to stress fractures may be partly due to diminished bone density secondary to increased osteoclastic activity.3 There has been debate within the literature whether TOH is a consequence of a stress fracture or vice versa, since not every patient with TOH also has subchondral stress fractures.3,4
Although the specific risk factors for TOH are poorly understood, it is generally agreed that they differ from the risk factors associated with osteonecrosis.1,3–7 For example, it is postulated that there may be a relationship between TOH and reflex sympathetic dystrophy, also known as complex regional pain syndrome (CRPS).3,5,6 The two conditions share similar signs and symptoms of pain, edema, and inflammatory soft tissue changes, however, the hypersensitivity, vasomotor dysfunction, temperature and skin changes typically observed in CRPS are not characteristic of transient osteoporosis.3,5 A small retrospective study6 (n=17) reported that physicians had a higher incidence of TOH compared to osteonecrosis or transient bone marrow edema syndrome and postulated that this may be due to long hours of standing.
TOH may eventually migrate to other joints, especially the contralateral hip, a condition referred to as regional migratory osteoporosis (RMO).5 The signs and symptoms of RMO are identical to TOH and both eventually resolve without treatment, suggesting that these are variations of the same or a similar condition.8
TOH is also similar to a condition termed transient bone marrow edema (TBME) syndrome. Within the literature, authors may either use the terms interchangeably3 or choose to differentiate the two conditions. According to some authors5,7, TBME syndrome should be reserved for cases where radiographs do not show osteopenic changes of the femoral head and neck, whereas the term TOH is typically reserved for cases where radiographs do demonstrate osteopenia. Aside from this minor distinction the clinical presentation and MR findings of TBME syndrome and TOH are equivalent.5
Case History
A 59-year-old male presented to a chiropractic clinic with a chief complaint of acute left hip pain after building a dock. The pain began two to three days after the building project during which he repeatedly carried 16-foot long, two inch by six inch planks of lumber on his left hip down a steep incline to the beach. The pain was a constant ache with sharp, stabbing pain when moving from sitting to standing and after prolonged walking, sitting or lying supine. Following prolonged standing or walking, the severity of the patient’s pain prevented him from lying in a neutral left hip, knee extended posture. In order to avoid pain he would assume a supine lying position of 45° hip and knee flexion. At night he would frequently wake up to “walk off the pain”.
Physical Examination
Upon examination, the patient had difficultly arising from sitting and ambulated with an antalgic gait and limp favoring his left hip. His left groin and hip region were tender to palpation and demonstrated painful limitation of passive ranges of internal rotation, external rotation, flexion, and extension. Log roll, FABER Patrick, and FADIR (hip impingement) tests were all exquisitely painful with soft end feel restriction associated with muscular guarding rather than with a hard end feel restriction suggestive of joint pathology. Ober test and Trendelenberg tests were negative (refer to Table 1 for a summary of the relevant orthopedic examinations). Conventional AP (Figure 1A) and frog-leg lateral (Figure 1B) radiographs of the left hip were interpreted as normal.
Table 1.
Relevant Orthopedic Examinations14
| Orthopedic Exam | Description | Interpretation |
|---|---|---|
| Log Roll | Patient is supine, the examiner places both hands on the patient’s mid-thigh and passively externally rotates each hip maximally. | Test is positive for intra-articular pathology if greater external rotation is noted on the affected side. |
| FABER Patrick | Patient is supine, the examiner flexes, abducts, and externally rotates the affected hip so that the ipsilateral ankle is placed just proximal to the unaffected knee. While stabilizing the anterior superior iliac spine, the affected leg is lowered toward the table. | Test is positive for intra-articular hip pain if the maneuver reproduces the patient’s symptoms. |
| FADIR Hip Impingement | Patient is supine, the examiner flexes the hip and knee to 90°, then adducts and internally rotates the affected hip in the flexed position. | Test is positive for intra-articular hip pathology if the patient’s symptoms are reproduced. |
| Ober’s test | Patient is side-lying with the affected side up, the examiner flexes the patient’s knee to 90° and abducts and extends the hip. The examiner allows gravity to adduct the hip as much as possible. | Test is positive if the hip is unable to adduct to the neutral position. Positive test is indicative of iliotibial band pathology. |
| Trendelenberg | Patient is standing and lifts one foot off the ground. | Test is positive if the non-stance hip drops. Positive test is indicative of gluteus medius weakness on the stance side. |
Figure 1.
Anteroposterior (A) and frog-leg lateral (B) radiographs reveal normal bone density, trabeculae and only minor hip joint space narrowing.
Initial Diagnosis and Management
The initial clinical impression was of an acute capsular lesion of the hip. The patient’s primary care clinician prescribed analgesic and non-steroidal anti-inflammatory medication for six weeks which provided only minimal relief. A brief three visit course of conservative physical therapy triggered acute exacerbations of pain lasting 48 to 72 hours following each therapy session and was therefore discontinued. Despite the patient’s optimistic expectation of a gradual self-resolution of the complaint, at six weeks post-injury his pain and disability appeared to be increasing. As a result, the patient was referred for MR imaging with intra-articular gadolinium (MR arthrogram) to assess the hip joint and intra-articular structures.
MR Imaging and Final Diagnosis
MR imaging was ordered to rule out internal derangement or osseous pathology (i.e. labral tear, osteoarthrosis or osteonecrosis respectively). The MR images revealed extensive edema within the medullary bone of the head and neck of the left femur with an associated joint effusion. No findings suggestive of avascular necrosis, labral tear or intra-articular lesion were identified. Further T1-weighted MR images were obtained after intravenous injection of gadolinium, revealing minor signal enhancement of the femoral head. The radiologist’s report concluded that these findings were most consistent with transient osteoporosis of the hip (Figure 2A).
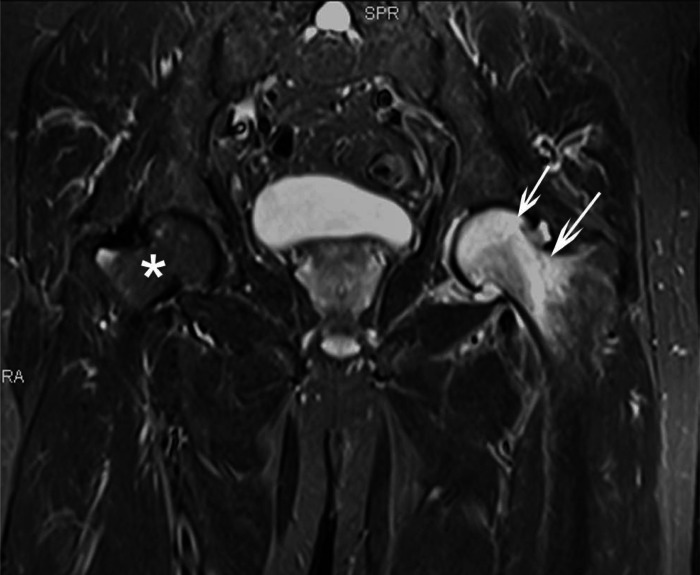
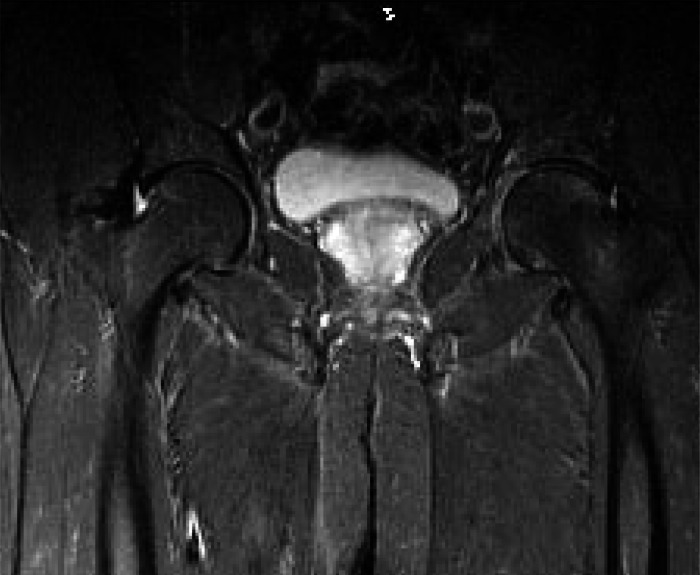
Figure 2.
A) Initial coronal fluid–sensitive (STIR) MR image obtained 3 months after initial onset of pain reveals hyper-intense bone marrow signal within the left femoral head and neck (arrows) consistent with the bone marrow edema associated with transient osteoporosis. A joint effusion is also present. The right femoral head and neck exhibit normal bone marrow signal. (*)
B) Follow up coronal fluid–sensitive (STIR) MR image obtained 3 months after the initial MR study reveals complete resolution of the abnormal bone marrow signal within the left femoral head and neck as well as resolution of the initial joint effusion. The right femoral head and neck exhibit normal bone marrow signal.
The cornerstone of management involved education of the patient to the benign, self-limiting nature of the condition. This included a cautionary warning regarding the heightened risk for fracture of the femoral neck secondary to transient osteoporosis and the risk of migration of the condition to the contralateral hip. Pain reduction strategies included utilization of analgesics on an as-needed basis and the adoption of hip sparing postures and activities to decrease loading.
The radiologist requested follow-up MR imaging to confirm that the edema had resolved satisfactorily, to exclude the presence of subchondral stress fracture, and to ensure that the contralateral femoral head and neck remained normal. MR imaging obtained four months post-diagnosis demonstrated complete resolution of the findings of bone marrow edema and joint effusion. There was no evidence of contralateral hip involvement or complications such as fracture (Figure 2B). The patient reported a full resolution of his symptoms at the follow-up appointment just prior to his second MRI. Regular and moderate manual labor provoked no symptomatic flair or recurrence.
Discussion
TOH is a self-limiting condition which develops spontaneously or may be triggered by minor trauma and is characterized clinically by acute hip pain, limping gait, and limited range of motion.1,3 It is three times as likely to affect males5 who are typically between the ages of 32 and 551. A subset less frequently affected by TOH are women in the third trimester of pregnancy.1,2,5 Most cases of TOH are spontaneous3,5 while others occur following minor trauma1,6 such as a “groin pull” or a slip. It is thought that minor trauma may cause a transient ischemic period which triggers an episode of TOH.6 In the current case it can be postulated that the repetitive compressive loading of the left hip may have been sufficient trauma to result in transient ischemia which progressed to TOH.
Conventional radiographic studies are generally insensitive to TOH and contribute little value to the diagnosis.1,3 The radiographs in the current case were unremarkable, exhibiting no degenerative (osteoarthritic) changes of either hip, despite the patient’s age of 59 years. Some cases of TOH report diffuse osteopenia of the femoral head and neck, however, this finding may not be detected radiographically until up to eight weeks post-injury.1–5 Our patient underwent radiographic examination within four weeks of the onset of acute hip pain, perhaps explaining the absence of osteopenia on his images.
MR imaging findings of bone marrow edema are the diagnostic hallmark of TOH – low signal intensity of bone marrow on T1-weighted images and high signal on STIR and fat saturated T2-weighted, fluid sensitive sequences.3 Hip joint effusion (seen in this study) is a consistent finding in many cases of TOH.1,3,5 Although not present in the current case, another finding frequently associated with TOH is a subchondral stress fracture.3,4 The absence of subchondral stress fractures in some cases may suggest that TOH is a cause rather than a consequence of such fractures.
TOH often presents clinically in a pattern similar to early stage osteonecrosis.1,3,7 Osteonecrosis is an irreversible condition that can be categorized as primary or secondary.3 Secondary osteonecrosis is caused by an ischemic lesion and is associated with trauma, alcoholism, corticosteroid use, and hematological disorders. Primary (or spontaneous) osteonecrosis is idiopathic and therefore not associated with the aforementioned risk factors.3 Early osteonecrosis of the femoral head will display the radiographic signs of subchondral sclerosis of the rim of the femoral head which is known as the crescent or half-moon sign.3,9 MR imaging of early osteonecrosis typically reveals a low signal intensity serpentine band surrounding a normal appearing epiphyseal area on T1 weighted images; while advanced cases reveal epiphyseal collapse, subchrondral fractures, and subchondral cysts.9
TOH spontaneously resolves within a four to nine month period with conservative treatment which focuses on hip sparing activities and postures which decrease loading on the hip joint.4 Surgical decompression is occasionally performed to shorten the healing period but is unnecessary.3 Ringe et al10 found that administering an intravenous dose (four mg initial dose with an optional second two mg dose at three months) of ibandronate, a potent nitrogen-containing bisphosphonate, decreased visual analogue pain scales by an average of 94.3% with a decrease of at least 75% in all patients (N=12). Furthermore, the bone mineral density between the affected and unaffected femoral neck regions (N=7) decreased from 10.1 to 2.6% at the six month follow-up. TOH does not result in osteoarthritic changes to the bone or joint1 and does not progress to osteonecrosis3. It is therefore imperative that TOH be differentiated from osteonecrosis in the early stages as the prognosis and treatment of these two conditions differs substantially (refer to Table 2 for differential diagnoses).1
Table 2.
| Transient Osteoporosis | Osteonecrosis | Stress Fracture | |
|---|---|---|---|
| Signs, Symptoms, and Physical Exam | Acute onset of hip pain Limping gait Decreased ROM |
Acute onset of hip pain Limping gait Decreased ROM |
Acute onset of hip pain Limping gait Decreased ROM |
| Etiology | Unknown Possible association with CRPS |
Ischemic trauma Risk factors: fracture, steroid use, alcohol, etc |
Mechanical trauma Fatigue (healthy bone) Risk factors: overuse, repetitive running Stress (weak bone) Risk factors: osteoporosis |
| Imaging Findings | Bone edema Joint effusion ± Stress fracture |
Bone edema Subchondral collapse Subchondral cysts ± Subchondral fracture Osteoarthritic changes XR: cresent sign MR: low intensity serpentine band surrounding normal tissue on T1 |
Bone edema XR: fracture line MR: low intensity line on T1 |
| Progression | Spontaneous resolution Possible migration |
Irreversible | Reversible Possible progression to osteonecrosis |
| Treatment | No weight bearing activities Nonsteroidal anti-inflammatory drugs (NSAIDs) Analgesics Corticosteroids Possible ibandronate |
Surgery | No weight bearing activities Possible surgery |
The most common treatment options for osteonecrosis are rotational osteotomy, core decompression, and free vascularized fibular grafting.11 Outcomes are affected by the patient’s age, etiology, stage of osteonecrosis, size, and location of the necrotic lesion. Conservative treatment (e.g. partial weight bearing) of early stage osteonecrosis has been proven ineffective in 80 to 90% of patients.11 Osteotomies attempt to realign the femoral articulating surface to reduce the weight-bearing zone of the necrotic area. Hasegawa et al12 reported five and ten year transtrochanteric rotational osteotomy survival rates without failure as 71% and 61%, respectively. Core decompression is an alternative treatment option that is one of the least invasive surgical procedures to manage osteonecrosis. Malizos et al11 reported further surgical intervention was necessary in 16%, 37%, and 71% after core decompression of osteonecrosis stages I, II, and III, respectively. Decompression procedures have higher success rates with segmental lesions prior to articular collapse. Free vascularized fibular grafting is a procedure that has a survival of 61%–96% at mid-term (4–7 years) follow-up.13 Yoo et al13 followed 110 patients (124 hips) who underwent vascularized fibular grafting for a minimum of 10 years. The average Harris hip score improved from 72 to 88 while 13 patients (13 hips) failed treatment and had to undergo total hip arthroplasty. The ultimate purpose of osteotomies, decompression procedures, and grafts is to prevent or delay total hip arthroplasty.10
Conclusion
TOH should be considered in the differential diagnosis of middle-aged males presenting with acute hip pain, limping gait, and limited ranges of hip motion. Early radiographic findings of TOH are usually unremarkable, but may show diffuse osteopenia of the femoral head and neck beyond six to eight weeks post-onset of pain. Symptom progression following treatment may require advanced imaging to differentiate TOH from other conditions such as osteonecrosis. TOH differs from osteonecrosis in its risk factors; its absence of radiographic findings of subchondral or focal lesions; and its self-limiting resolution with conservative management.
Acknowledgments
The authors thank Chris Herrington for assistance with the reproductions
Footnotes
Disclaimers: No disclaimers or conflicts of interest.
Sources of Support: No sources of financial support.
References
- 1.Balakrishman A, Schemitsch EH, Pearce D, McKee MD. Distinguishing transient osteoporosis of the hip from avascular necrosis. Can J Surg. 2003;46(3):187–192. [PMC free article] [PubMed] [Google Scholar]
- 2.Kim YL, Nam KW, Yoo JJ, Hong SH, Kim HJ. CT evidence for subchondral trabecular injury of the femoral head in transient osteoporosis of the hip: a case report. J Korean Med Sci. 2010;25:192–5. doi: 10.3346/jkms.2010.25.1.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandez-Canton G. From bone marrow edema to osteonecrosis. New Concepts. Reumatol Clin. 2009;5(5):223–7. doi: 10.1016/j.reuma.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Ergun T, Lakadamyali H. The relationship between MRI findings and duration of symptoms in transient osteoporosis of the hip. Acta Orthop Traumatol Turc. 2008;42(1):10–5. doi: 10.3944/aott.2008.010. [DOI] [PubMed] [Google Scholar]
- 5.Hayes CW, Conway WF, Daniel WW. MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome, or osteonecrosis. Radiographics. 1993;13:1001–11. doi: 10.1148/radiographics.13.5.8210586. [DOI] [PubMed] [Google Scholar]
- 6.Hadidy AM, Al Ryalat NT, Hadidi ST, Tarawneh ES, Hadidi MT, Samara OA, Abu-Labn DM, Al-Rousan LM, Hiyasat DA, Hamamy HA. Male transient hip osteoporosis: are physicians at a higher risk? Arch Osteoporos. 2009;4:41–45. doi: 10.1007/s11657-009-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YM, Oh HC, Kim HJ. The pattern of bone marrow oedema on MRI in osteonecrosis of the femoral head. J Bone Joint Surg (Br) 2000;82-B:837–41. doi: 10.1302/0301-620x.82b6.10740. [DOI] [PubMed] [Google Scholar]
- 8.Swoopes F, Mazzini N, Centonze M, Fancellu G. It is true that regional migratory osteoporosis has a full remission? A follow-up after 14 years: a case report. Euro J Phys Rehabil Med. 2011;47:1–2. [PubMed] [Google Scholar]
- 9.Vande Berg BE, Malghem JJ, Labaisse MA, Noel HM, Maldague BE. MR imaging of avascular necrosis and transient marrow edema of the femoral head. Radiographics. 1993;13:501–20. doi: 10.1148/radiographics.13.3.8316660. [DOI] [PubMed] [Google Scholar]
- 10.Ringe JD, Dorst A, Faber H. Effective and rapid treatment of painful localized transient osteoporosis (bone marrow edema) with intravenous ibandronate. Osteoporos Int. 2005;16:2063–8. doi: 10.1007/s00198-005-2001-6. [DOI] [PubMed] [Google Scholar]
- 11.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: Etiology, imaging, and treatment. Eur J Radiol. 2007;63:16–28. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa Y, Sakano S, Iwase T, Iwasada S, Torii S, Iwata H. Pedicle bone grafting versus transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Bone Joint Surg [Br] 2003;85-B:191–8. doi: 10.1302/0301-620x.85b2.13190. [DOI] [PubMed] [Google Scholar]
- 13.Yoo MC, Kim K, Hahn CS, Parvizi J. Long-term followup of vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2008;466(5):1133–1140. doi: 10.1007/s11999-008-0204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cleland JA, Koppenhaver S. Netter’s Orthopaedic Clinical Examination: An Evidence-Based Approach. 2nd ed. Philadelphia: Saunders; 2011. pp. 267–75. [Google Scholar]
- 15.Souza TA. Differential Diagnosis and Management for the Chiropractor: Protocols and Algorithms. 4th ed. Sudbury, Massachusetts: Jones and Bartlett Publishers; 2009. pp. 353–56. [Google Scholar]