Abstract
Objectives
Few health literacy instruments are available to clinicians to help understand the implications of patient difficulty understanding health information. Those that do exist are lengthy and would not be conducive to use in a busy clinical setting. Long-term dental and medical outcomes may improve if health care providers can identify individuals with low health literacy levels who may benefit from tailored communication, yet few instruments are available for clinical use. The purpose of this study is to introduce a brief 20-item screener for limited dental/medical health literacy among adult dental patients.
Methods
Two-hundred adult patients seeking treatment at a dental clinic in a large medical complex completed a health literacy screening instrument and survey. Steps in the development of the 20-item instrument are described. Comparison of the 20-item dental/medical instrument with other health literacy measures are calculated using mean health literacy scores, tests of reliability and readability, and correlation coefficients.
Results
Scores on the brief 20-item measure varied significantly by race, education level, language use, needing help with medical/health materials forms. Those with lower dental/medical health literacy, as measured by the REALMD-20 were less likely to receive regular follow-up care than those with higher literacy.
Conclusions
The REALMD-20 is a quick screening instrument that can be used by clinicians to detect limited dental/medical health literacy among adult patients seeking treatment in dental/medical clinic settings.
Keywords: health literacy, oral health literacy, measurement, REALM-D, screening tool, dental
Introduction
Inability to understand health information can be a profound disadvantage to patients and their families when asked to make informed decisions about an array of treatment choices (1). In 2010, health literacy, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” was incorporated into The Patient Protection and Affordable Care Act (P.L. 111–148), reinforcing the importance of health literacy to the ability to affect positive health outcomes. Low health literacy is associated with differences in health care utilization (e.g., more emergency services and fewer preventive services), mistakes with medication dosages, and interpreting health messages (2,3).
Patients and their families manage diseases that cross multiple health fields, requiring a cross-disciplinary vocabulary and ability to navigate complex health systems for answers to problems that relate to their oral health (4,5). In dental clinics associated with teaching hospitals or health centers, patients often enter the system in need of a variety of services, and move from one specialty to another communicating across multiple health providers. For example, patients undergoing radiation or chemotherapy to treat cancer often must manage serious complications to their oral health as a result of these therapies (6). The dynamic relationship between periodontal disease and diabetes is also well documented (7), requiring patients to successfully communicate with both medical and dental providers. Long-term dental and medical outcomes may improve if clinicians can quickly identify individuals who need low literacy disease-specific material or other tailored communication (8,9).
Over the last decade, advances in the conceptualization of health literacy have resulted in a broad array of measurement tools that capture the full spectrum of skills ranging from reading comprehension to numeracy, however, for the purpose of this study, we are focusing on those that assess ability to read and pronounce health care-related words only. These measures use as a starting point the original Rapid Estimate of Adult Literacy in Medicine (REALM) that measured ability to read and pronounce medical words correctly (10). In 2003, this measure was shortened to create a brief 11-item version (11). Using the original REALM instrument as the methodological basis for instrument development, several oral health literacy assessment tools were developed, including the 33-item Rapid Estimate of Adult Literacy in Dentistry (REALD-33) (12–14); and the 99-item REALD-99 (15). As the fields of dentistry and medicine become more interconnected, the 84-item REALM-D was developed (16) as a tool that screens for a patient’s ability to read both medical and dental terminology. Creating a cross-disciplinary tool reflects findings that support the link between the medical and oral health care systems that the public is now recognizing. The purpose of this study is to conduct a secondary analysis to introduce a brief 20-item screener to determine limited dental/medical health literacy among adult dental patients.
Methods
A secondary analysis of data collected from a sample of 200 adult patients seeking treatment for the first time from an Oral Diagnosis Clinic at a School of Dentistry in the United States between January 2005 and June 2006 were used for this study. In the original study, participants were screened by the clinic coordinator based on information from their completed intake form for inclusion in the study. Criteria included being at least 18 years of age, without cognitive, vision, or hearing impairment, and having at least limited understanding of English. Each eligible participant was given a letter describing the study and inviting them to participate, including information on receiving $5.00 after completing the initial survey and another $5.00 after completing a follow-up survey. Each of the 200 study participants was given a laminated copy of the 84-item REALM-D by the interviewer and asked to read each word aloud (16). The protocol for administration and scoring of the original instrument was retained and used for scoring the REALM-D. If the subject could not read a word, he/she was instructed to say “blank” and move to the next word. Interviewers were trained by the co-investigator on how to administer and score the REALM-D instrument. Words pronounced correctly received a score by the interviewer of 1 and mispronounced or not attempted words received a score of 0. Paper copies of a 48-item health beliefs and attitudes survey were also administered to the study subject. Categories of questions included patient health education assessment (UCLA clinic survey), health values, beliefs and attitudes, and health locus of control.
Item reduction process to create a 20-item measure
With the goal of creating a brief dental/medical health literacy screener that would demonstrate acceptable psychometric properties, 20 terms were selected from the 84-item REALM-D instrument in a two-step process. In the initial step, 18 dental terms from the REALMD that were correctly pronounced by all participants were entered into a principle component factor analysis using a varimax rotation method. Three factors emerged from this analysis. Given the simplicity of the five items that loaded on the first factor (teeth, pain, tongue, brushing, and toothache), they were dropped from further analysis. Two other terms (root-canal and bacteria) had very low factor loadings on any of the three factors and were also dropped from further analysis, leaving 11 dental terms.
The second step was to re-run the factor analysis using a varimax rotation method, with the remaining 11 dental terms (anesthetic, abscess, amalgam, caries, calculus, dentures, gingivitis, extraction, insurance, hygiene, and periodontitis) and adding the 8 REALM-R medical terms (fatigue, directed, jaundice, allergic, constipation, anemia, colitis, osteoporosis), plus depression (11). Two factors emerged, explaining 45 percent of the total variance of the 20-item list with 7.14 and 1.77 eigenvalues (see Table 1). The first factor consists of 10 less difficult items (abscess, dentures, hygiene, insurance, extraction, fatigue, directed, allergic, constipation, and depression) with 5 dental terms and 5 medical/mental health terms. The second factor consists of the 10 more difficult to pronounce items (calculus, gingivitis, anesthetic, periodontitis, caries, amalgam, jaundice, colitis, anemia, and osteoporosis) with 6 dental and 4 medical terms.
Table 1.
REALMD-20 terms
| REALMD-20 | |
|---|---|
| List 1 | List 2 |
| Abscess | Extraction |
| Denture | Anemia |
| Hygiene | Caries |
| Insurance | Jaundice |
| Calculus | Anesthetic |
| Fatigue | Periodontitis |
| Depression | Colitis |
| Allergic | Amalgam |
| Directed | Gingivitis |
| Constipation | Osteoporosis |
We compared the reliability of the REALMD-20 to the longer REALM and REALMD measures using Cronbach’s alpha. We tested for convergent and predictive validity using Spearman’s correlations as well as Mann-Whitney U and Kruskal-Wallis non-parametric tests. For convergent validity, the 20-item measure was correlated with other health literacy measures, including two single-item health literacy indicators (17); How often do you have someone help you read hospital materials?; and How confident are you filling out medical forms by yourself? These two variables were dichotomized to show those who always feel confident (n = 134) and those who never need help with reading hospital material (n = 140). All statistical tests were conducted using SPSS version 18 (18).
Results
The sample of 200 patients ranged in age from 19 to 89 with a mean age of 49 years and 55 percent were male. Study participants come from a variety of socio-demographic and ethnic groups, reporting their racial/ethnic makeup to be largely Caucasian (58 percent), Hispanic (19 percent), African American (11 percent), Asian/Pacific Islander (9 percent), American Indian (2 percent), and 2 percent reporting the “other” category. Twenty-eight percent of the study sample completed less than or equal to 12 years of education, and 20 percent reported that English was not their main language.
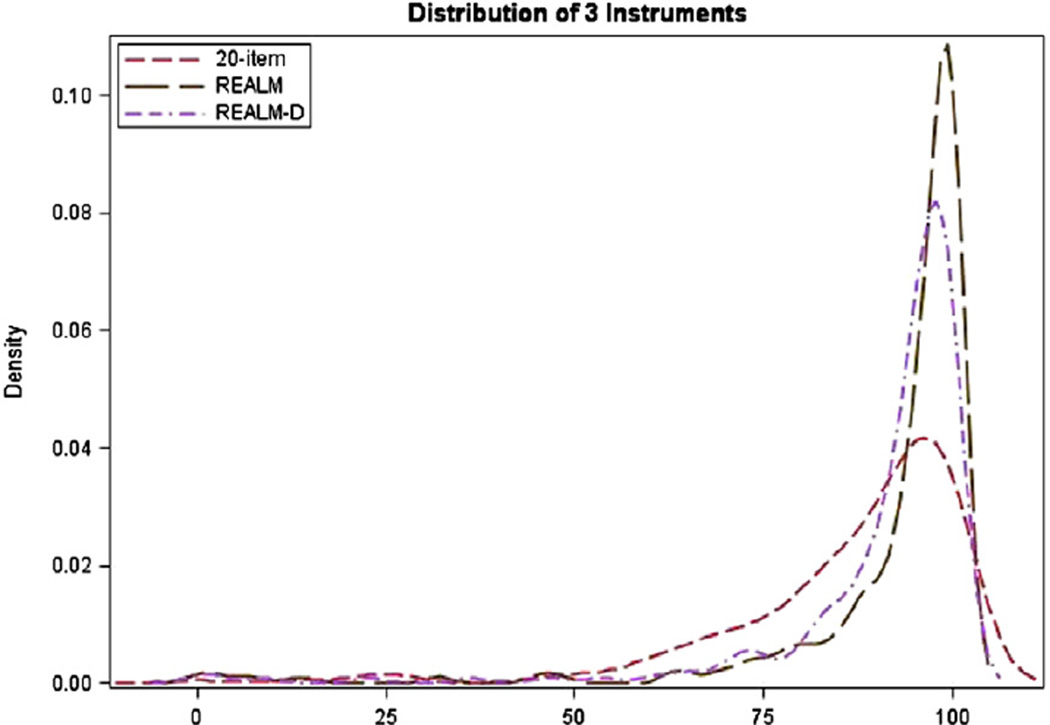
A comparison of the 20-item instrument to three related measures was made using a variety of analyses. An illustrative comparison of mean scores and the distribution of the scales is shown in Figure 1, where the REALMD-20 instrument approximates the most normal distribution of all three measures in that it has a lower skewness (−2.32) than both the REALM (−4.01) and REALM-D (−3.84). Potential scores on the 20-item instrument (REALMD-20) ranged from 0 to 20 with a mean of 17.2 (Table 2). A mean score of 62.6 is reported for the original 66-item REALM and 78.7 for the 84-item REALM-D. Using the same algorithm created for the original REALM (10) to determine grade, 8 participants scored at 3rd grade or below (range 0–5), 15 participants scored at the 4th–6th grade level (range 6–13), 85 participants scored at the 7th to 8th grade level (range 14–18), and 95 participants scored at the high school or more education level (range 19–20).
Figure 1.
Distribution of REALM, REALMD, and REALMD-20 instruments.
Table 2.
Distribution, Reliability and Readability of Health Literacy Measures on Sample of 200 Subjects
| REALMD-20 (20-item) |
Original REALM (66-item) |
REALM-D (84-item) |
|
|---|---|---|---|
| Range | 0–20 | 22–66 | 26–84 |
| Mean (SD) | 17.28 (3.25) | 62.62 (6.95) | 78.71 (8.88) |
| Median | 18.00 | 65.00 | 81.00 |
| Skewness | −2.32 | −4.01 | −3.84 |
| Cronbach alpha | 0.86 | 0.95 | 0.96 |
| Grade equivalent | % (n) | % (n) | % (n) |
| 3rd and below | 2.5 (5) | 0 | 0 |
| 4th to 6th grade | 7.5 (15) | 3.5 (7) | 3.0 (6) |
| 7th to 8th grade | 42.5 (85) | 12.0 (24) | 15.5 (31) |
| High school | 47.5 (95) | 84.5 (169) | 81.5 (163) |
| Estimated time to administer | 2–3 minutes | 3–5 minutes | 5–7 minutes |
The shorter REALMD-20 instrument represents comparatively the same reliability (alpha = 0.86) as the longer REALM and REALM-D measures (alphas = 0.95 and 0.96, respectively) when the number of items is considered. The Cronbach alpha values of 0.95 and 0.96 for the REALM and REALM-D are exactly the ones the Spearman-Brown prophecy index predicts would result for the REALMD-20 if the number of items were increased from 20 to 66 and 84, respectively. In other words the only reason the REALM and REALMD-84 have higher values is because they have 3.3 and 4.2 times more items.
The higher alphas are strictly a product of the high number of items in the measures and not a reflection of the quality of the items.
As shown in a correlation matrix using Spearman correlation coefficients for all health literacy measures (Table 3), the REALMD-20 was highly correlated with coefficients ranging from rs = 0.90 to rs = 0.93. Correlations between instruments and two single-item indicators were weakly, but significantly correlated with positive correlations between rs = 0.25 and rs = 0.32 (P < 0.001) for confident filling out medical forms, and negative correlations between rs = −0.25 and rs = −0.34 (P < 0.001) for needing help reading hospital material.
Table 3.
Correlation of Health Literacy Measures on Sample of 200 Subjects
| REALMD-20 (20-item) |
REALM (original 66-item) |
REALM-D (84-item) |
Confident filling out forms |
Need help reading hospital material |
|
|---|---|---|---|---|---|
| REALMD-20 (20-item) | – | ||||
| Original REALM (original 66-item) | 0.894** | – | |||
| REALM-D (84-item) | 0.931** | 0.991** | – | ||
| Always confident filling out medical forms | 0.321** | 0.299** | 0.317** | – | |
| Never need help reading hospital material | −0.286** | −0.336** | −0.325** | −0.247** | – |
Health literacy measures are not normally distributed, hence non-parametric tests (Mann-Whitney and Kruskal-Wallis) were used.
P ≥ 0.05,
P ≤ 0.001.
A comparison of mean oral health literacy scores by patient characteristics and single-item literacy indicators is shown in Table 4. The REALMD-20 score varied significantly with study participants who were non-white, reported that English was not their main language, needed help with hospital materials, and were less confident filling out medical forms.
Table 4.
Comparison of Mean Health Literacy Scores by Patient Characteristics of 200 Subjects
| n | REALMD-20 (20-item) |
Original REALM (66-item) |
REALM-D (84-item) |
|
|---|---|---|---|---|
| Race** | ||||
| White | 115 | 17.97 | 64.02 | 80.54 |
| Non-white | 85 | 16.35 | 60.72 | 76.24 |
| P = 0.001 | P = 0.003 | P = 0.002 | ||
| Education** | ||||
| ≤HS | 55 | 16.05 | 60.29 | 75.6 |
| College | 115 | 17.54 | 63.29 | 79.5 |
| Post college | 30 | 18.53 | 64.30 | 81.2 |
| P = 0.001 | P = 0.011 | P = 0.005 | ||
| English main language** | ||||
| Yes | 160 | 17.70 | 63.66 | 80.00 |
| No | 40 | 15.60 | 58.45 | 73.35 |
| P = 0.002 | P = 0.003 | P = 0.002 | ||
| Never need help with hospital materials** | ||||
| No | 140 | 17.71 | 63.58 | 79.92 |
| Yes | 60 | 16.28 | 60.37 | 75.88 |
| P = 0.016 | P = 0.015 | P = 0.015 | ||
| Always confident filling out medical forms** | ||||
| Yes | 134 | 17.78 | 63.63 | 79.98 |
| No | 66 | 16.27 | 60.76 | 76.14 |
| P = 0.004 | P = 0.012 | P = 0.012 | ||
Health literacy measures are not normally distributed, hence nonparametric tests (Mann-Whitney and Kruskal-Wallis) were used.
P < .001.
Discussion
In order to be widely used in clinical settings, screening for low health literacy must be accomplished in an efficient manner that will benefit the care delivery system. Patients seeking health care often have complicated health problems that have both oral and medical problems and are seen by multiple health care professionals. One of the benefits of the REALMD-20 is that it uses terms that are applicable to a variety of medical fields. Short instruments that capture limited medical/dental health literacy can be useful to clinicians working in multidisciplinary settings, or sharing electronic records, where multiple providers can utilize the same instrument.
Results of this study show that a short instrument such as the REALMD-20 is a quick screening instrument that can be used to detect limited dental/medical health literacy among adult patients seeking treatment in dental or medical clinic settings in under 3 minutes. Compared to other medical or dental literacy measures, this instrument captures both domains of health in a short period of time. Many of the more comprehensive health literacy measures such as the ToFHLiD and OHLI are reported to take approximately 20 minutes and we purposely chose not to compare the 20-item screener to these more comprehensive measures. Of the measures that use the original REALM and focus on reading ability only, the REALMD-D proves to be a valuable measure for a clinical setting as it captures both medical and dental terms in a short period of time.
The reliability of a measure that is responsive to the number of items and the Cronbach alpha of the 20-item is appropriately lower (alpha = 0.86) than the longer measure. This suggests that too few items might compromise instrument reliability, however too many items produces redundancy, as evident by extremely high alpha scores for the original, more lengthy measures. A shorter instrument consisting of a comparatively greater number of difficult terms to pronounce ensures that providers will more readily recognize a health literacy issue, and adapt an appropriate communication strategy accordingly.
Limitations of this study relate to the narrow focus of the screening instrument and the characteristics of the study participant. Secondary data analysis was from a non-random recruitment of relatively well educated clinic patients who were able to read words written in English, under-representing a segment of our clinic population most at risk for low health literacy, at least in English. Despite this selection bias, 20 percent of the sample reported English as not their primary language (ESL), representative of the demographics of the UCLA Dental Clinic, which serves an extremely diverse urban population. Clinicians serving patients identified as having a primary language other than English may want to focus more on comprehension rather than pronunciation. However this screening instrument does not measure word comprehension, making it difficult to determine, for those who report English as not their main language, if they are mispronouncing words they know and understand. We know from previous work with this data (16) that there was an interaction between race, education, and English as a second language, Those who report less than or equal to 12 years of education, and being non-white were more likely to have English as a second language. One approach is to focus on linguistically and culturally appropriate communication techniques for all patient-provider interactions which may help serve those whose primary language is not English and have difficulty with pronunciation rather than knowledge of health terms.
As suggested by Baker (19), health literacy is a complicated construct, consisting of an individual’s capacity to communicate as well as system demands, requiring more comprehensive assessments of the full range of literacy skills. Gong and colleagues (20) who have done extensive work with word recognition instruments as well as functional oral health literacy measures, suggest that while using a version of the REALM-D to screen for low dental literacy is a good first step, consideration of functional literacy in terms of reading comprehension and numerical ability will more fully capture deficits in health literacy that may influence oral health outcomes. While we recognize that health literacy is more than just reading ability (21), this type of screening tool may be most useful in helping clinic staff decide on appropriate communication for informed consent or delivery of patient education material. However, as with the original instrument it was designed from, it is strictly a screening tool to identify inadequate medical and dental word recognition and does not assess a patient’s ability to fully understand the meaning of medical or dental terms.
As clinic populations become increasingly socio-demographically and culturally diverse, a quick and efficient screen for dental/medical health literacy that can be utilized by multiple health providers is a good first step in identifying patients who may require more tailored health communication. The ability for dental and medical clinicians to quickly assess what has been termed an “invisible barrier” to better oral health outcomes (22) has the potential to improve both the patient and provider’s ability to maintain oral health and manage disease.
References
- 1.Atchison KA, Black E, Leathers R, Belin TR, Abrego M, Gironda MW, Wong D, Shetty V, DerMartirosian C. A qualitative report of patient problems and post-operative instructions. J Oral Maxillofac Surg. 2005;63:449–456. doi: 10.1016/j.joms.2004.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gazmararian J, Williams MV, Peal J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 3.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 4.Kirsch I, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the findings of the National Adult Literacy Survey. Washington, DC: National Center for Education Statustics, U.S. Department of Education; 1993. [Google Scholar]
- 5.Rudd R, Renzulli D, Pereira A, Daltroy L. Literacy demands in health care settings: the patient perspective. In: Schwartzberg JG, VanGeest J, Wang C, editors. Understanding health literacy. Chicago (IL): American Medical Association; 2005. pp. 69–84. [Google Scholar]
- 6.Walsh LJ. Clinical assessment and management of the oral environment in the oncology patient. Aust Dent J. 2010;55:66–77. doi: 10.1111/j.1834-7819.2010.01201.x. [DOI] [PubMed] [Google Scholar]
- 7.Mealey BL. Periodontal disease and diabetes, a two-way street. J Am Dent Assoc. 2006;137(2 Suppl):26S–31S. doi: 10.14219/jada.archive.2006.0404. [DOI] [PubMed] [Google Scholar]
- 8.Mejia GC, Weintraub JA, Cheng NF, Grossman W, Han PZ, Phipps KR, Gansky SA. Language and literacy relate to lack of children’s dental sealant use. Community Dent Oral Epidemiol. 2011;39:318–324. doi: 10.1111/j.1600-0528.2010.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller E, Lee JY, DeWalt DA, Vann WF., Jr Impact of caregiver literacy on children’s oral health outcomes. Pediatrics. 2010;126:107–114. doi: 10.1542/peds.2009-2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis TC, Crouch M, Long S. Rapid estimate of adult literacy in medicine. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 11.Bass PF, 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18:1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JY, Rozier RG, Daniel Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30-A brief communication. J Public Health Dent. 2007;67:94–98. doi: 10.1111/j.1752-7325.2007.00021.x. [DOI] [PubMed] [Google Scholar]
- 13.Stucky BD, Lee JY, Lee SY, Rozier RG. Development of the two-stage rapid estimate of adult literacy in dentistry. Community Dent Oral Epidemiol. 2011;39:474–480. doi: 10.1111/j.1600-0528.2011.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones MJ, Lee JY, Rozier RG. Oral health literacy among adult patients seeking dental care. J Am Dent Assoc. 2007;138:1199–1208. doi: 10.14219/jada.archive.2007.0344. [DOI] [PubMed] [Google Scholar]
- 15.Richman JA, Lee JY, Rozier G, Gong DA, Pahel BT, Vann WF. Evaluation of a word recognition instrument to test health literacy in dentistry: the REALD-99. J Public Health Dent. 2006;67:99–204. doi: 10.1111/j.1752-7325.2007.00022.x. [DOI] [PubMed] [Google Scholar]
- 16.Atchison KA, Gironda MW, Messadi D, Der-Martirosian C. Screening for oral health literacy in an urban dental clinic. J Public Health Dent. 2010;70:269–758. doi: 10.1111/j.1752-7325.2010.00181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 18.SPSS, Inc. PASW Statistics for Windows, Version 18.0. Chicago (IL): SPSS Inc.; 2009. Released. [Google Scholar]
- 19.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gong DA, Lee JY, Rozier RG, Pahel BT, Richman JA, Vann WF. Development and testing of the Test of Functional Health Literacy in Dentistry (TOFHLiD) J Public Health Dent. 2007;67:105–112. doi: 10.1111/j.1752-7325.2007.00023.x. [DOI] [PubMed] [Google Scholar]
- 21.Schonlau M, Martin L, Haas A, Derose KP, Rudd R. Patients’ literacy skills: more than just reading ability. J Health Commun. 2011;16:1046–1054. doi: 10.1080/10810730.2011.571345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A report of a workgroup sponsored by the National Institute of Dental and Craniofacial Research, National Institute of Health, U.S. Public Health Service, Department of Health and Human Services. J Public Health Dent. 2005;63:174–182. doi: 10.1111/j.1752-7325.2005.tb02808.x. [DOI] [PubMed] [Google Scholar]