Abstract
Time sensitive acute stroke treatments and the growing shortage of vascular neurologists compound to create a gap in the delivery of care to meet the American Stroke Association guidelines in underserviced regions. Audio/video consultation (telemedicine), which has been evolving since the late 1990’s, is a putative solution. While telemedicine can serve as a valuable facilitative tool, the telestroke consultation is only one piece of a complex collaboration between hub and spoke environments and clinical personnel. The growing use of telemedicine in stroke offers more opportunities for all nurses to participate in the continuum of cerebrovascular disease care. A review of this collaboration will include but will not be limited to: algorithms of the acute stroke evaluation, hub and spoke staff meetings, stroke education for spoke staff, and patient follow-up post acute treatment. Our team’s telemedicine experience, utilizing research, education, and clinical practice, will be described.
Keywords: stroke, telemedicine, nursing, nurse practitioners, and physician-nurse relations
Stroke and acute treatment disparities
In America stroke has an incidence of 750,000 per year and is the third most common cause of death.1,2 Since 1996, when the US Food and Drug Administration approved tissue plasminogen activator (tPA), which remains the only recognized medical treatment for acute ischemic stroke, there has been a growing public knowledge of stroke and its acute treatment. Unfortunately, the commensurate growth in vascular neurology providers and systems of care has lagged. This discrepancy matters when the acute stroke patient has been transported into the emergency department (ED) and the ED physician has neither a vascular neurologist nor a general neurologist to call upon for assistance. There are two glaring disparities present: firstly, a vascular neurology provider shortage and secondly the rural—urban disparity. Vascular neurologists are in short supply with approximately 704 certified with the American Board of Psychiatry and Neurology;3 with approximately 64 accredited programs with 67 filled in the 2009–2010 academic year.4 ED physicians generally lack the experience necessary for solo stroke thrombolysis care. They may be reluctant to make a decision for the administration of tPA, without neurology support, but timely transfer to a primary stroke center is not a viable option in many rural settings.5–7 The tPA administration for stroke in academic centers and in organized urban stroke systems of care is demonstrated to be 17.2% to 23.4%.8–10 However, in the rural communities tPA administration for stroke is generally low at 2% to 4%.11–13 Telemedicine becomes a feasible solution to bridge the demonstrable gap in delivery for acute stroke care.
Stroke Telemedicine Defined
The evolution of telemedicine has moved from telephone to audiovisual. There are different telemedicine facilitated systems of care. For the purpose of this article, the system that will be discussed is a hub and spoke network. The hub is the urban primary stroke center, from where vascular neurologists make remote connections via the internet to the different spoke ED sites that are situated in rural community hospitals.14 The American Telemedicine Association defines telemedicine as “the use of medical information exchanged from one site to another via electronic communications to improve patients’ health status. Closely associated with telemedicine is the term “telehealth,” which is often used to encompass a broader definition of remote healthcare that does not always involve clinical services. Videoconferencing, transmission of still images, e-health including patient portals, remote monitoring of vital signs, continuing medical education and nursing call centers are all considered part of telemedicine and telehealth”.15 Telemedicine for the purpose of this article is real time audiovisual (AV) communication that is accomplished by a camera system in a remote ED. In the 2009 American Heart Association/American Stroke Association issued a scientific statement reviewing the evidence for the use of telemedicine within stroke systems of care.16
Nursing roles
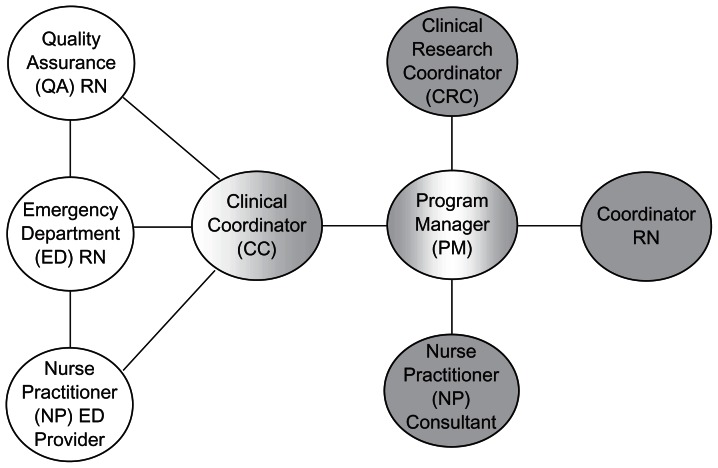
The growing use of telemedicine offers more opportunities for all nurses to participate in the continuum of stroke care. This article will address nursing roles that were identified within the Stroke Telemedicine for Arizona Rural Residents (STARR) network. The roles that will be discussed include: program manager (PM) at hub, clinical coordinator at hub, clinical research coordinator (CRC) at hub, nurse practitioner (NP) at hub, NP at spoke, coordinator at spoke, quality assurance (QA) RN at spoke, and emergency department (ED) registered nurse (RN) at spoke. Each nursing role has an important function that allows a telemedicine network to succeed. These roles need not be assigned to separate individuals at hub or spoke. Depending on the size of the network or volume at a spoke site, these roles can easily be blended. A diagram illustrating the flow and relationships of these roles is depicted in Figure 1.
Figure 1.
Flow chart illustrating RN roles and relationships.
The spoke is demonstrated in white and the hub in grey. Please note that the PM leads the initiative facilitating the needs of the hub and spoke, while supporting the CC of the spoke directly. The CC is the liaison and the point person at the spoke.
Program manager
The PM is the individual designated to set up new spoke sites. The PM is usually the first to establish contact and set the agenda for the program in the new spoke site. The nurse PM organizes site visits, invites the requisite people to the table for initial meetings,17 and creates a network of individuals at the spoke that will carry through this partnership. Once the decision to collaborate has been made between spoke and hub, contractual agreements are strongly recommended to formalize the agreement.17
Thereafter the PM will maintain communication as the liaison between spoke and hub for day to day Stroke telemedicine nursing operations and ongoing logistics. These communications can be facilitated in many ways, for example, newsletters, spoke staff meetings, emails, and telephone calls. Monthly newsletters can communicate updates including statistics of the number of stroke alerts activated, number of tPA administrations, duration of door to needle time intervals, to increase awareness of workflow and need for improvement. This is an effective venue for introducing new consultants from the hub side and congratulate staff at the spoke sites for successful work.18,19 All sites are included as recipients of the newsletter to promote networking and collegiality. Attending spoke staff meetings utilizing the camera system allows questions and answers, updating, and creates a level of confidence when utilizing the technology to activate the stroke alert system. Adding weekly emails and touching base by telephone also create seamless communication. The staff at the spoke sites affirm that the hub staff become an extension of their ED. The PM leads the program by working through multiple levels of the spoke organization and the hub’s team to create a successful network.20
Hub clinical coordinator
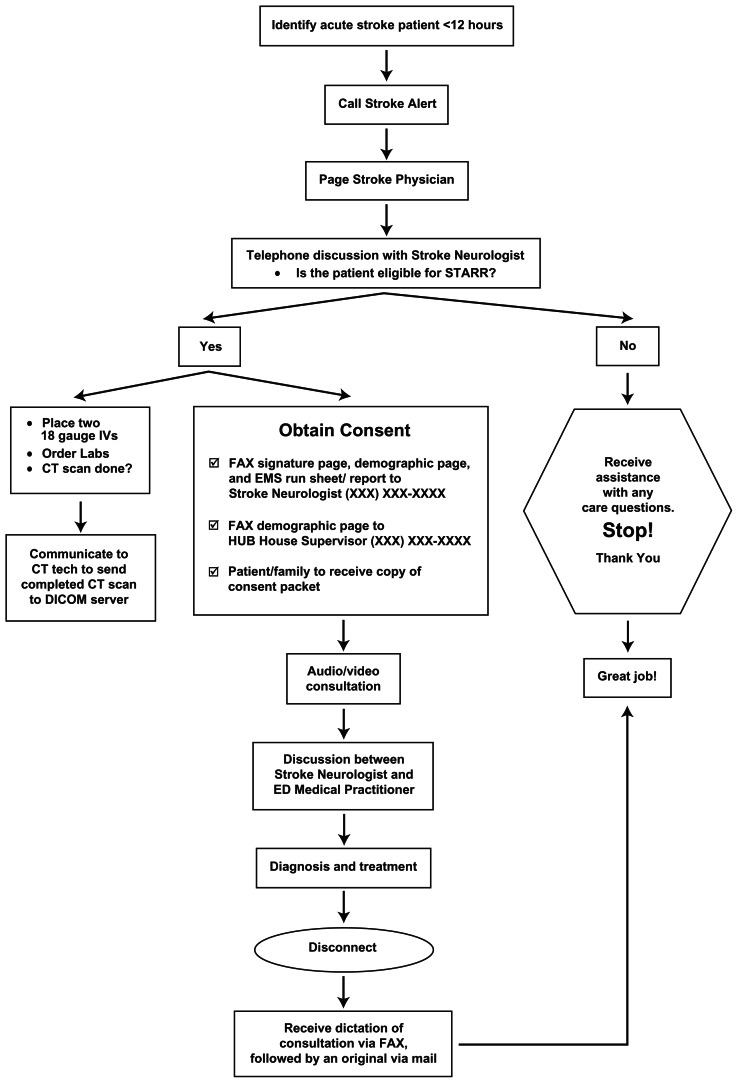
This position is a role that can be incorporated with the PM role in a smaller network. In a larger network a separate position may be called for due to workload. This is a role that can lead the clinical development at the spoke sites.21 The clinical coordinator creates and drives a simple stroke alert algorithm for the hub and spoke so expectations from both sites are clear and the consultation runs as smoothly as if the consultant were physically in the spoke ED.
The spoke algorithm should be concise and easy to follow, Figure 2. These algorithms are placed at the ED secretary desk and physician work areas. Some spokes have placed a copy in the stroke alert packets, so each RN can anticipate the plan of care their patient will receive.
Figure 2.
STARR algorithm.
The hub clinical coordinator will develop, facilitate and present the spoke site education. The education is heavily front loaded for a spoke site start up. This typically involves the ED and intensive care unit RN’s, and ED physicians. Concepts that are discussed include: understanding the expectations during each component of the algorithm, acute stroke care in the ED, the continuum of care from ED to ICU, to an acute medical floor, and finally preparing the patient for rehabilitation.22 Emergency medical staff (EMS) education is also an important component. EMS personnel become familiar with stroke assessment and how the telemedicine program can assist their community.8 Some spoke sites were evaluating approximately 10 stroke patients per year prior to telemedicine participation and are now seeing double or triple this volume. Patients are no longer being routinely diverted, by EMS, from their remote communities to the metropolitan primary stroke centers.
Yearly education should be considered to capture any staff turn over and review or update existing staff. This also offers an opportunity for feedback regarding what is going well and where improvement can be made.
Hub clinical research coordinator
The American Heart Association and American Stroke Association have issued a new policy statement for implementation of telemedicine in stroke.17 It specifically outlines the necessity to have on-going research within telestroke practice. We continue to have questions with this new consultative practice modality. A CRC can assist with writing and implementing consent forms, organizing and retrieving data, and depositing into a repository. The ability to scrutinize monthly statistics pertaining to time windows and patterns of improvement or regression is valuable to the hub and spoke network. This prospective research will assist in implementing change to improve patient care. Utilizing research improves patient care and therefore improves patients’ lives.23
Telemedicine is still a relatively novel healthcare delivery system in the stroke field. This opens a whole new arena in nursing research. There are many questions that should be addressed pertaining to outcomes and quality research. For example: Does the telestroke patient who is able to stay in their own community have improved measurable outcome compared to the stroke patient that has to leave their community for the same care? Is the acute hospitalization and rehabilitation shorter when the patient is able to stay in their own community? Similar questions have been focused on in the telemedic pilot project for integrative stroke care (TEMPiS) study in Germany.24 Also, one could propose the concept of studying experimental stroke treatment in telemedicine networks by screening, consenting, randomizing, treating, and even following all research subjects via telemedicine. This would allow more opportunity for enrollment into stroke trials with an enlarged catchment area within a telestroke network.25 The hub could act as the governing Institutional Review Board to assist smaller centers to become involved in ongoing stroke trials.14
Hub nurse practitioner vascular neurology consult
There is a plethora of documentation in the literature of NP’s working within sub-specialties and the positive impact they have in patient care.26 Some organizations are creating their own fellowships for midlevel provider to anticipate staffing sub-specialties. Neurovascular Education and Training in Stroke Management and Acute Reperfusion Therapy (NET SMART) a neurology vascular fellowship for advanced practice nurses (APN) prepares the APN to improve acute stroke treatment use and outcomes in their communities.27 The NET SMART program currently has eighty one enrolled advance practice nurses. NP’s with the appropriate training such as NET SMART can serve as a consultant via telemedicine with success.28 The breadth of the consultation is variable based on the individual state and institution scope of practice and policies for NP’s.
Spoke nurse practitioner
Many NP’s are working in rural or critical access hospitals and are the first responders to the ED stroke alerts. Their availability to lend assistance with stroke patients in their communities is invaluable and has proven to increase patient satisfaction and door to needle time for thrombolytic therapy.29,30 The NP would recognize stroke syndromes and activate a stroke alert. Thereafter they would work with the telestroke neurologist to establish the plan of care for their collaborative patient. Utilizing telemedicine in ED’s for general emergency medicine has been studied and is successful within the rural communities.31
Spoke coordinator
A spoke coordinator position can be an added assignment for an ED nurse manager, nurse educator, or team leader. Establishing a point person to receive hub communications and transmit them to the spoke staff is vital for success. Duties identified consist of preparing stroke packets for ED staff (which include consents both English and Spanish), acute stroke order sets, and NIHSS language cards. The coordinator acts as the “train the trainer” for the camera system, also making sure the system has power and internet connection. This person would also be a liaison with the Information Technology (IT) staff and the computed tomography (CT) staff for any ongoing troubleshooting needs with the camera system.
Spoke quality assurance RN
The QA RN at the spoke site has the opportunity to guide and facilitate the spoke site’s telemedicine quality measurement. The guidelines have been firmly established since 2000 when the Brain Attack Coalition recommended primary stroke centers to decrease death and disability from stroke.32 One of the initiatives to increase awareness of quality has been the use of “Get With The Guidelines” (GWTGs) to benchmark stroke centers with other stroke centers.33 This will assist with meeting core measures and fostering continued maturity of the program at the spoke site.
Spoke emergency department RN
This is one of the most important roles that has become richer within the telemedicine structure. The ED beside nurse completes the stroke assessment with the vascular neurologist. Understanding the National Institutes of Health Stroke Scale (NIHSS) is essential to facilitate the vascular neurologist’s examination. Some spoke sites have elected to encourage and incentivize their staff to complete the NIHSS training and certification. Having an RN at the bedside of the acute stroke patient who understands and knows the NIHSS makes the examination go very quickly. Familiarity with the evaluation tools and algorithm decreases the door to needle time for tPA eligible patients. RN’s in this role have offered feed back explaining that having stroke telemedicine has changed the milieu of their ED’s. RN’s have stated that stroke patients now have a chance to receive tPA whereas before they waited for transportation to a primary stroke centers and frequently missed the opportunity due to time constraints. They have also shared that being the conduit for the assessment empowers them. The nurses feel that they are truly making a difference in the care of the acute stroke patient. It is no longer a feeling of being on the side lines.
Conclusion
Telemedicine, although not novel, is still an evolving field in stroke. At first glance, many conceptualize it as a physician oriented program, but without necessary nursing support the network would not be successful. Telemedicine offers unique opportunities for nurses within urban and rural settings to participate in the continuum of stroke care.
Acknowledgement
This manuscript was presented as an oral presentation at the 2009 American Association of Neuroscience Nursing in Las Vegas, Nevada.
Footnotes
Disclosures
None of the authors have any conflicts to declare.
References
- 1.Broderick J, Brott T, Kothari R, et al. The Greater Cincinnati/Northern Kentucky Stroke Study: Preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29:415–21. doi: 10.1161/01.str.29.2.415. [DOI] [PubMed] [Google Scholar]
- 2.Carandang R, Seshadri S, Beiser A, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296:2939–46. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]
- 3.The American board of psychiatry and neurology, Inc. [Accessed on November 11, 2009]. Available at http://www.abpn.com. Updated 2009.
- 4.Accreditation council for graduate medical education. [Accessed on November 11, 2009]. Available at http://www.acgme.org. Updated 2009.
- 5.Bambauer KZ, Johnston SC, Bambauer DE, Zivin JA. Reasons why few patients with acute stroke receive tissue Plasminogen activator. Archives of Neurology. 2006;63:661–4. doi: 10.1001/archneur.63.5.661. [DOI] [PubMed] [Google Scholar]
- 6.Brown DL, Barsan WG, Lisabeth LD, Gallery ME, Morgenstern LB. Survey of emergency physicians about recombinant tissue Plasminogen activator for acute ischemic stroke. Annals of Emergency Medicine. 2005;46:56–60. doi: 10.1016/j.annemergmed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 7.Bobrow BJ, Demaerschalk BM, Wood JP, Villarin A, Clark L, Jennings A. Journal of Brain Disease. 2009;1:29–73. doi: 10.4137/jcnsd.s2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO) Stroke. 2005;36:1512–8. doi: 10.1161/01.STR.0000170700.45340.39. [DOI] [PubMed] [Google Scholar]
- 9.Demaerschalk BM, Bobrow BJ, Paulsen M. Development of a metropolitan matrix of primary stroke centers: The phoenix experience. Stroke. 2008;39:1246–53. doi: 10.1161/STROKEAHA.107.500678. [DOI] [PubMed] [Google Scholar]
- 10.Gladstone DJ, Rodan LH, Sahlas DJ, et al. A citywide prehospital protocol increases access to stroke thrombolysis in Toronto. [Accessed November 19, 2009];Stroke [serial online] 2009 40:00–00. doi: 10.1161/STROKEAHA.108.540377. Available at: http://stroke.ahajournals.org. [DOI] [PubMed] [Google Scholar]
- 11.Joubert J, Prentice LF, Moulin T, et al. Stroke in rural areas and small communities. Stroke. 2008;39:1920–8. doi: 10.1161/STROKEAHA.107.501643. [DOI] [PubMed] [Google Scholar]
- 12.Leira EC, Hess DC, Torner JC, Adams HP. Rural-urban differences in acute stroke management practices. Archives of Neurology. 2008;65:887–91. doi: 10.1001/archneur.65.7.887. [DOI] [PubMed] [Google Scholar]
- 13.Miley ML, Demaerschalk BM, Olmstead NL, et al. The state of emergency stroke resources and care in rural Arizona: a platform for telemedicine. Telemed J E Health. 2009;15:691–9. doi: 10.1089/tmj.2009.0018. [DOI] [PubMed] [Google Scholar]
- 14.Demaerschalk BM, Miley ML, Kiernan TJ, et al. For the STARR co-investigators. Stroke Telemedicine. Mayo Clinic Proceedings. 2009;84:53–64. doi: 10.4065/84.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Telemedicine Association. [Accessed November 19, 2009]. http://www.americantelemed.org.
- 16.Schwamm LH, Holloway RG, Amareco P, et al. on behalf of the American Heart Association Stroke Council and the Interdisciplinary Council on Peripheral Vascular Disease. A review of the evidence for the use of telemedicine within stroke systems of care: A scientific statement from the American heart association/American stroke association. Stroke. 2009;40:2616–34. doi: 10.1161/STROKEAHA.109.192360. [DOI] [PubMed] [Google Scholar]
- 17.Schwamm LH, Audebert HJ, Amarenco P, Chumbler NR, Frankel MR, George MG, et al. on behalf of the American Heart Association Stroke Council; Council on Epidemiology and Prevention; Interdisciplinary Council on Peripheral Vascular Disease; and the council on Cardiovascular Radiology and Intervention. Stroke. 2009;40:2635–60. [Google Scholar]
- 18.Williams J, Murphy P. Better project management better patient outcomes. Nursing Management. 2005;36:41–7. doi: 10.1097/00006247-200511000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Kleinman CS. Leadership roles, competencies, and education. JONA. 2003;33:451–5. doi: 10.1097/00005110-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Westphal JA. Resilient organizations: Matrix model and service line management. JONA. 2005;35:414–9. doi: 10.1097/00005110-200509000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Seagraves KB. How to be a catalyst for change. Nursing. 2009;39:18–9. doi: 10.1097/01.NURSE.0000365017.08493.08. [DOI] [PubMed] [Google Scholar]
- 22.Adams HP, Jr, del Zoppo F, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research interdisciplinary Working Groups. Stroke. 2007;38:1655–711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 23.Gawlinski A. The power of clinical nursing research: engage clinicians, improve patients’ lives, and forge a professional legacy. AJCC. 2008;17:315–27. [PubMed] [Google Scholar]
- 24.Audebert HJ, Schenkel J, Heuschmann PU, et al. Effects of the implementation of a telemedical stroke network: the telemedic pilot project for integrative stroke care TEMPiS in Bavaria, Germany. Lancet Neurology. 2006;5:742–8. doi: 10.1016/S1474-4422(06)70527-0. [DOI] [PubMed] [Google Scholar]
- 25.Fisher M. Developing and implementing future stroke therapies: The potential of telemedicine. Annals of Neurology. 2005;58:666–71. doi: 10.1002/ana.20659. [DOI] [PubMed] [Google Scholar]
- 26.Henderson K. TelEmergency: Distance emergency care in rural emergency departments using nurse practitioners. Journal of Emergency Nursing. 2006;32:388–93. doi: 10.1016/j.jen.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Alexandrov AW, Brethour M, Cudlip F, et al. Post-graduate fellowship education and training for nurses: The NET SMART Experience. Critical Care Nursing Quarterly. 2009;21(4):435–449. doi: 10.1016/j.ccell.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Demaerschalk BM, Kiernan TJ. Vascular neurology nurse practitioner provision of telemedicine consultations. International Journal of Telemedicine and Applications. doi: 10.1155/2010/507071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green T, Newcommon N. Advancing nurse practice: The role of the nurse practitioner in an acute stroke program. Journal of Neuroscience Nursing. 2006;38:328–30. [PubMed] [Google Scholar]
- 30.Carter AJ, Chockinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. Canadian Journal of Emergency Medicine. 2007;9:286–95. doi: 10.1017/s1481803500015189. [DOI] [PubMed] [Google Scholar]
- 31.Gali R, Keith JC, McKenzie K, Hall GS, Henderson K. TelEmergency: A novel system for delivering emergency care to rural hospitals. Annals of Emergency Medicine. 2007;51:275–84. doi: 10.1016/j.annemergmed.2007.04.025. [DOI] [PubMed] [Google Scholar]
- 32.Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;21:283(23):3102–9. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 33.The American Stroke Association. [Accessed on November 20, 2009]. Available at http://www.strokeassociation.org. Updated November 18, 2009.