Abstract
Introduction
The scope of practice by general practitioners and family physicians in North America has been changing over time. Are academic practices providing residents the same scope of practice as the urban practices into which they are going?
Methods
A survey describing the activities and scope of general practice/family practice was constructed from the literature and checked with general practitioners/family physicians for face validity. It was administered by mail to academic family physicians at the University of Alberta Department of Family Medicine in Edmonton and to all practicing general practitioners/family physicians in the city and Capital Region around Edmonton. There was a response rate of 78% and 50.9%, respectively.
Results
Academic physicians’ practices differed from those of their urban colleagues. The former were all certified by the College of Family Physicians of Canada, worked in group practices, and included more males and fewer immigrants. They worked as many hours, but did less clinical work than their urban colleagues. Even so, 25% did more than 40 hours of clinical work each week compared with 68% of urban physicians. There was a wide scope of services and procedures provided by both groups and other services that were different from group to group. There was no difference between groups in intention to add or remove services in the next two years, but academic physicians had removed more services in the last two years.
Conclusion
General practitioners/family physicians still provide a wide range of services. Although both academic and urban general practitioners/family physicians have reduced some services in the last two years, they have both added others to their repertoire. Although the teaching and urban general practitioners/family physicians practices have many similarities, they also have differences, which may have implications for the training of future urban family physicians.
Keywords: comprehensiveness, primary care, education
Introduction
There has been a gradual change in the scope of practice by general practitioners in Canada for at least the last 10 years.1,2 Studies of Ontario general practitioners by Woodward et al1 and Chan et al2 showed a reduction in inpatient care, house calls, emergency room services, nursing home attendance, and provision of obstetric and anesthetic services, as evidenced by billing data. There was a simultaneous increase in the number of physicians who provided an “office only” service. Additionally, there was a move to subspecializing, in the form of emergency room only and palliative care only practice by some physicians holding a general licence.2
Hutchinson and Becker3 have shown that, worldwide, the philosophy and structure of primary care has a major influence on the scope of practice by family physicians, but they did not address the effect of training patterns. The National Physician Survey of 20044 demonstrated a change in practice from the previous survey of 2001.5 Also of note is that, in 2004, of 10 core services, the authors found that 63% of respondents provided all of them, but 20% of those physicians described as “general practitioners” did none of the core activities. Katz et al used a set of indicators of comprehensive care in Manitoba.6 Depending on the indicator, the frequency of involvement ranged from 35% to 70% of general practitioners. In the UK, with financial incentives, an overall 91% average achievement of health care indicators has been reported.7 In Alberta, Moores et al found that only 583 of 800 physicians licensed as general practitioners in Edmonton were active in office practice more than 30% of the time, according to their own description.8 In preparation for a recent survey study, we reviewed individual entries in the register of the College of Physicians and Surgeons in Alberta. In the register, for those holding a general license in Edmonton’s Capital Health region, we found that, of 1200 physicians with a general license, only 800 were not self-limiting their practice in their own self-reported entry in the register.9
In Ontario, the advent of family health networks and family health groups has resulted in a definition of a basket of core services that participating physicians have to provide.10 In the UK, the introduction of health targets has successfully increased the provision of those services, but has resulted in other services being given less attention.11 The College of Family Physicians of Canada maintains that family physicians provide a broad comprehensive scope of practice as one of their hallmarks.12
Van Royen et al13 in his review of the research agenda in family medicine found that in studies of comprehensiveness “... there has been limited research conducted on its implications or outcomes”. We were interested in the implications of the changing scope of comprehensiveness upon the structure of resident education and vice versa. With the changing face of practice, are training programs that are centered on academic teaching units preparing family medicine residents for the world of practice they will encounter after graduation? Are the models of practice that residents witness in residency training programs similar to that of the average urban general clinician? This study aims to examine the changing patterns of practice both in the residency program and in urban practice in Edmonton, Alberta. The research questions are.
What clinical services are family physicians/general practitioners providing in the Capital Health region (the health region which includes Edmonton and its conurbation)?
What changes are occurring in the range of services provided?
Are academic physicians in the teaching clinics providing the same range of services as urban family physicians?
Methods
The population was composed of two groups. First were 546 self-declared “family physicians”, as defined in the Family Practice Quality and Capacity Study.8 They practiced in the Capital Health region, which includes the city of Edmonton and surrounding conurbation of about 900,000 people. The “academic” group comprised the 18 academic faculty members in the Department of Family Medicine at the University of Alberta in Edmonton.
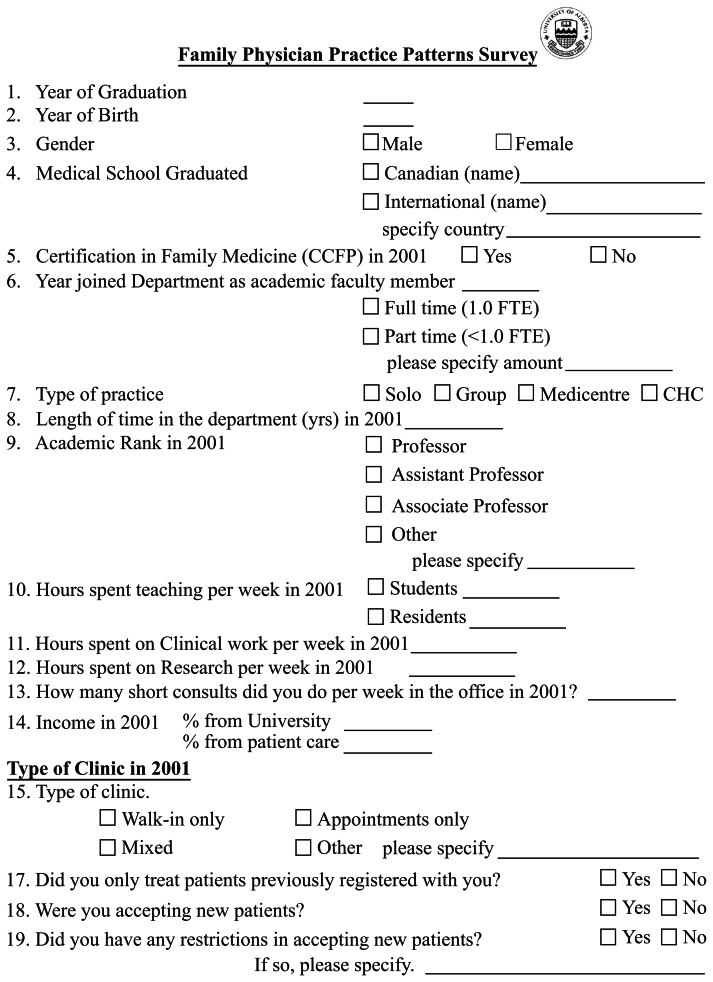
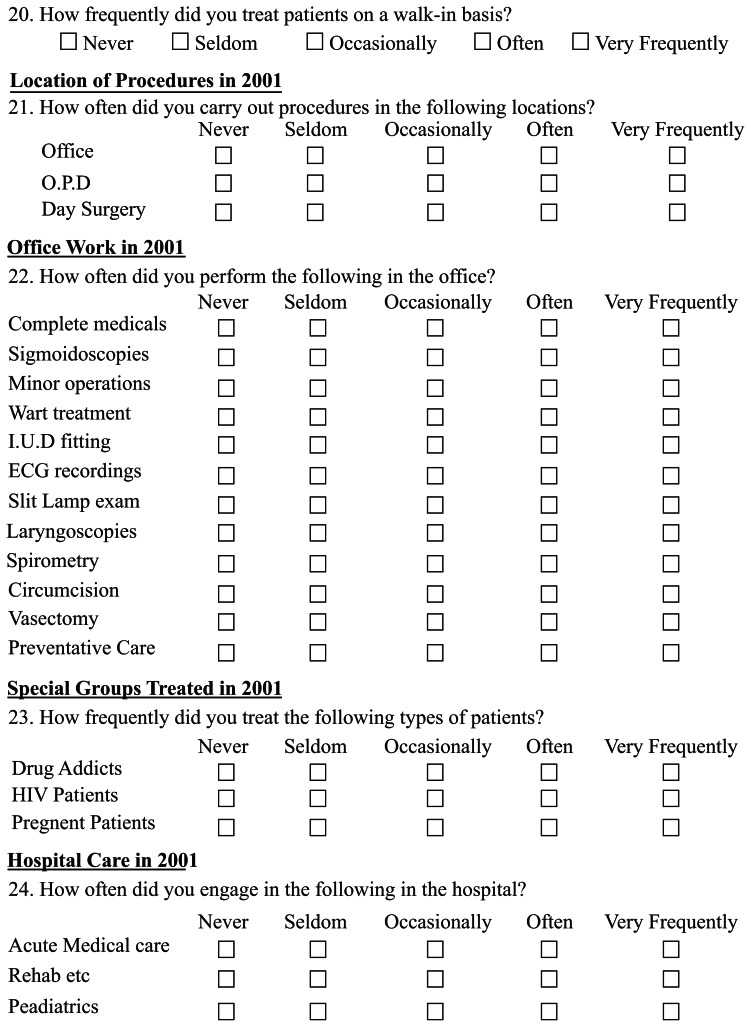
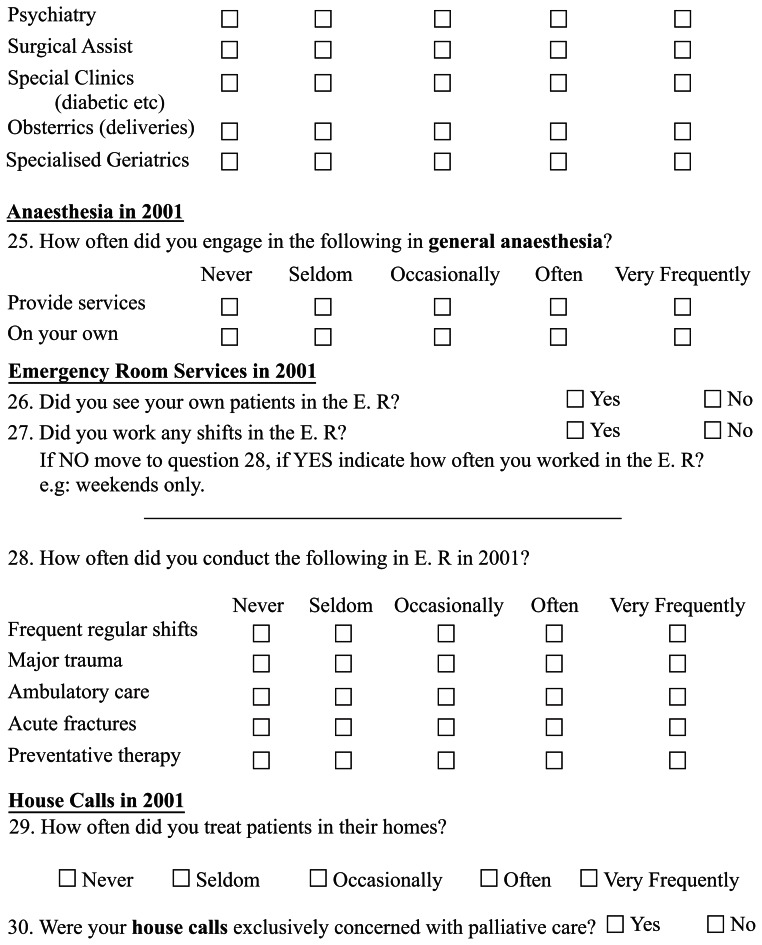
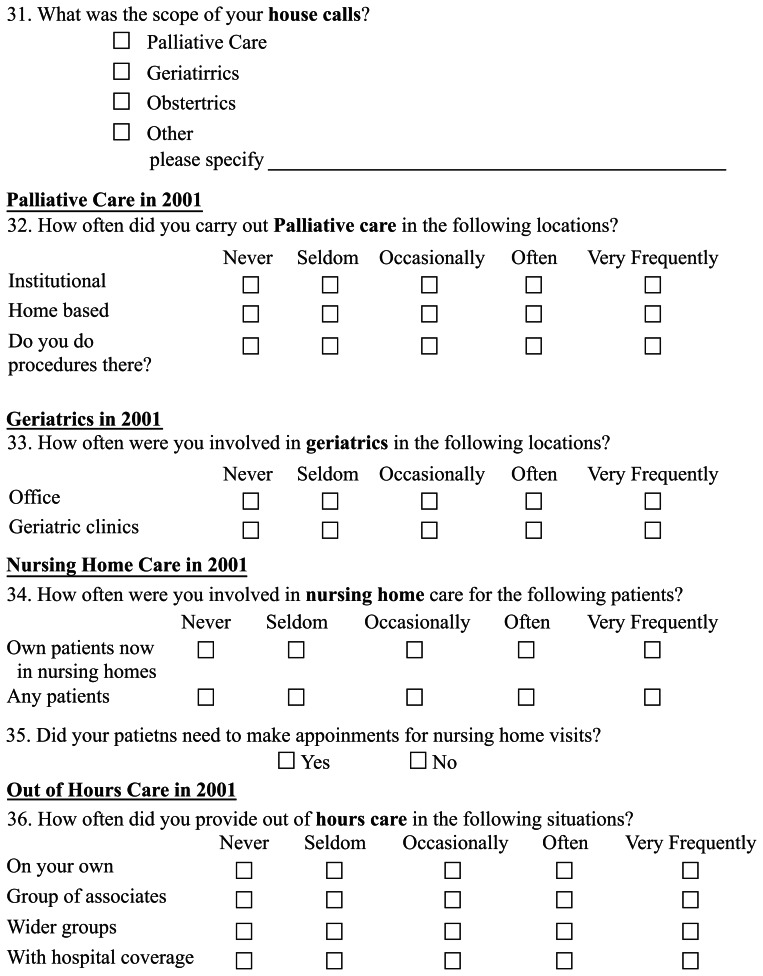
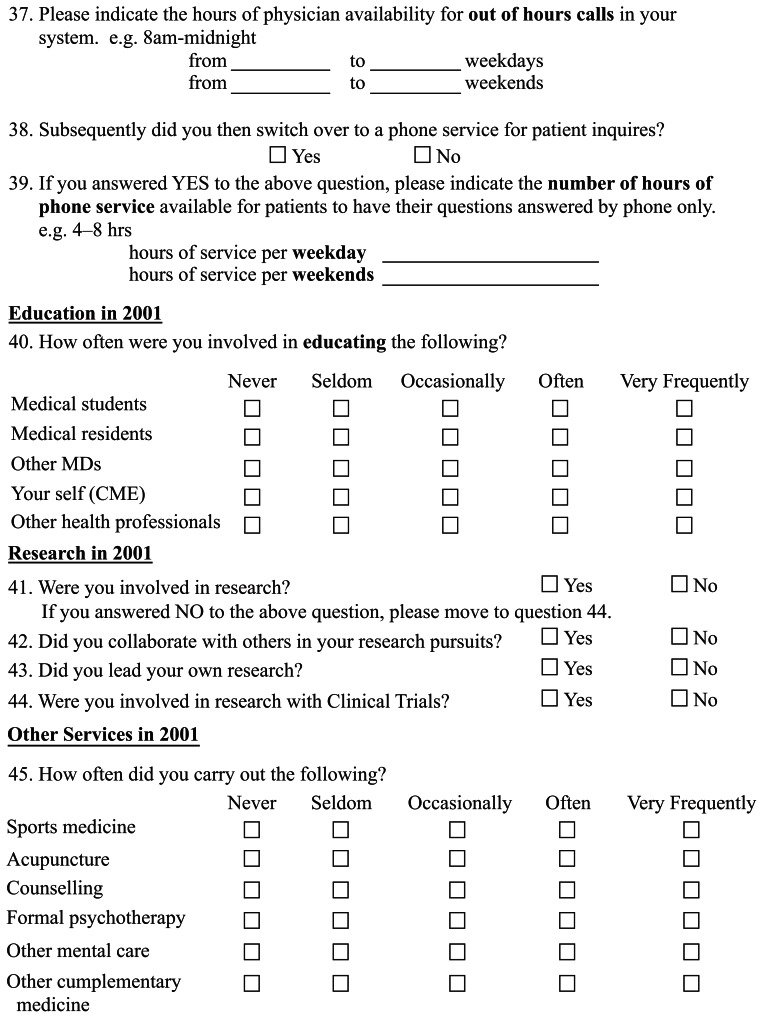
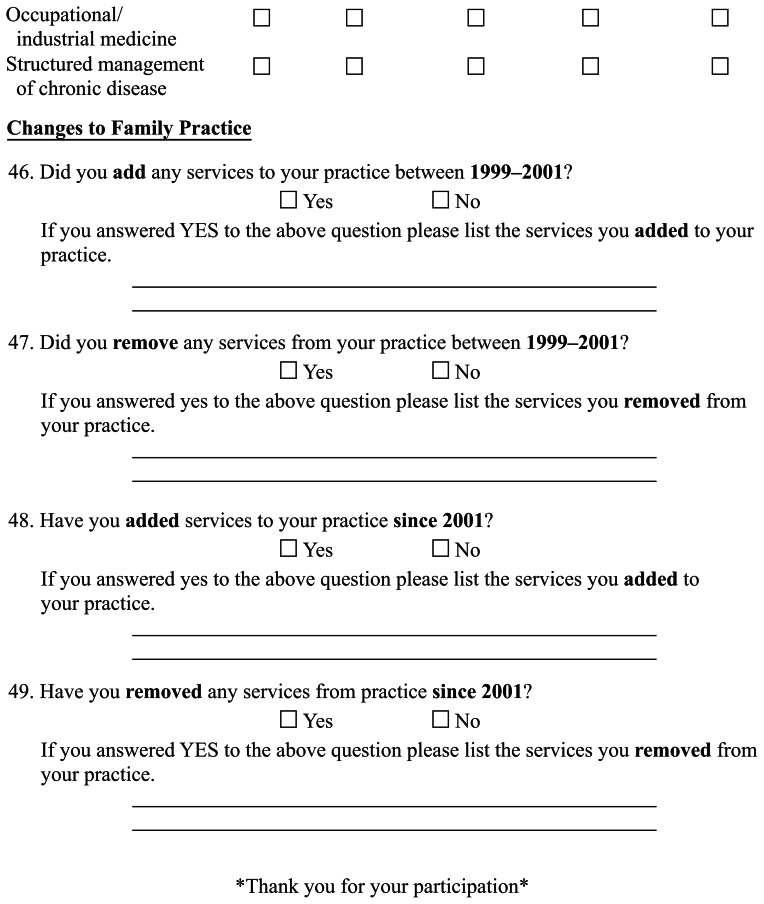
The survey was developed from a review of the current literature on the scope of general practice and comprehensiveness of care. It was tested for construct and face validity and readability using four family physicians. No detailed reliability or internal consistency testing was undertaken, but it was consistent with other investigators’ descriptions. In all, it consisted of 48 questions covering 17 areas of practice. It included 14 demographic questions to describe the populations accurately (see Appendix). Four questions related to recent or planned changes in practice pattern by the physician. The survey was approved by the Health Research Ethics Board at the University of Alberta and was mailed to the physicians with a stamped return envelope. One reminder was sent after two weeks.
Statistical analysis
The returned questionnaires were coded and responses entered into a computer spreadsheet. Descriptive analyses were undertaken of each group and means were compared using SPSS (SPSS Inc, Chicago, IL)14 using Student t-tests.
Results
Of 546 urban physicians, 278 (50.9%) responded. Fourteen of 18 academic physicians (78%) responded. Table 1 shows that the academic physician group was older, more were male, and almost all were Canadian graduates. All the academic family physicians held their Certification in Family Medicine (a prerequisite for appointment) compared with 56% of urban family physicians. All academics practiced in a group, whereas only 72% of their colleagues did. Although they did fewer hours of patient care than their colleagues, 25% did over 40 hours of clinical work weekly as well as their academic work, compared with 68% of the urban family physicians who worked over 40 hours a week.
Table 1.
Demographics of academic and nonacademic physician responders
| Characteristics | Academics (%) | Nonacademics (%) |
|---|---|---|
| Age (years) | ||
| 30–49 | 50.0 | 57.7 |
| 50+ | 50.0 | 42.3 |
| Gender | ||
| Male | 71.4 | 56.3 |
| Female | 28.6 | 43.7 |
| Medical school | ||
| Canadian | 92.9 | 79.1 |
| Non-Canadian | 7.1 | 20.9 |
| CCFP | ||
| Yes | 100.0 | 56.3 |
| No | 0.0 | 43.7 |
| Teaching | ||
| Clinical teacher | 100.0 | 26.3 |
| Full time | 100.0 | 0.0 |
| None | 0.0 | 73.7 |
| Type of practice | ||
| Solo | 0.0 | 15.3 |
| Group | 100.0 | 71.6 |
| Walk-in-clinic | 0.0 | 10.9 |
| Other | 0.0 | 2.2 |
| Hours of clinical work* | ||
| 0–39 | 75.0 | 32.6 |
| 40–60 | 25.0 | 59.5 |
| 61–100 | 0.0 | 7.9 |
| Clinic type | ||
| Walk-in | 0.0 | 6.1 |
| Appointment only | 64.3 | 54.5 |
| Mixed | 35.7 | 37.9 |
Note:
Clinical work = direct patient contact and related activity.
Abbreviation: CCFP, Certificate of the College of Family Physicans.
Table 2 demonstrates the wide scope of services provided by large numbers of family physicians in either group, some of which were significantly different between the two groups. Table 3 shows the differences in procedures performed, which were again significantly different. Table 4 shows that there was no significant difference when comparing the groups for plans to add or remove services in the next two years, or in the number of physicians who had added services in the last two years. However, significantly more academic physicians had removed services in the past two years.
Table 2.
Services provided by academic and nonacademic family physicians
| Service | Academics (%) | Nonacademics (%) |
|---|---|---|
| Treating patients with human immunodeficiency | 85.7 | 71.8 |
| Seeing their own patients in nursing homes | 64.3 | 55.4 |
| Delivering sports medicine | 85.7 | 81.5 |
| Providing psychotherapy | 57.1 | 52.9 |
| Providing occupational medicine | 64.3 | 51.5 |
| See own patients in emergency room | 92.9 | 22.7* |
| Provide out of hours care in group | 92.9 | 77.4* |
| Provide out of hours care including hospital | 85.7 | 34.6* |
| Educate other doctors | 92.9 | 39.6* |
| Educate other health professionals | 92.9 | 57.4* |
| Conduct research | 85.7 | 19.4* |
| Provide palliative care house calls | 7.1 | 32.1* |
| Provide phone services for patient inquiries | 7.1 | 37.6* |
Note:
P < 0.05 versus academic family physicians.
Table 3.
Procedures performed by academic and nonacademic family physicians
| Clinical activity | Academics | Nonacademics |
|---|---|---|
| Perform spirometry | 78.6 | 42.3* |
| Perform electrocardiogram | 71.3 | 33.9* |
| Perform slit lamp examination | 35.7 | 6.6* |
| Attendance in rehabilitation hospital | 57.1 | 24.6* |
| Attend in psychiatric hospital | 57.1 | 23.7* |
| Attend in special clinics | 21.4 | 5.5* |
| Provide obstetric hospital care | 42.9 | 11.0* |
| Provide geriatric hospital care | 35.7 | 14.0* |
Note:
P < 0.05 versus academic family physicians.
Table 4.
Services provided by academic and nonacademic family physicians
| Characteristics | Academics | Nonacademics |
|---|---|---|
| Added services in last two years | 21.4 | 14.0 |
| Planning to add services to practice | 14.3 | 6.3 |
| Planning to remove services from practice | 7.1 | 12.1 |
| Removed services in last two years | 57.1 | 26.2* |
Note:
P < 0.05 versus academic family physicians.
Discussion
The demographic differences between the academic group and their urban colleagues are concerning (Table 1). It is reasonable to expect the teachers to be more experienced and therefore older, but the gender difference in the face of increasing numbers of female residents nationally may need corrective action, such as preferential recruiting of experienced females for teaching roles. Sixty percent of the graduates in 2004 were female, up from 52% in 2001.4 The National Physician Survey in 2001 found that in Edmonton, 36.4% of physician respondents overall were female, and that their relative numbers rose to 48.6% in the under 35-year age cohort.5
In this study, more than one in five urban physicians were from non-Canadian medical schools versus only one in 14 of the academic/teaching physicians. This lack of representation may reflect a missed opportunity to access the available diversity in the physician population due to some system factors or may reflect disinterest by immigrant physicians in the academic role. This warrants an indepth study with such physicians and an examination of other departments to see if this is an idiosyncratic finding.
The questionnaire was developed to cover as many areas as were found documented in the literature and from the experience of the physicians who pilot-tested it. We believe it is inclusive of enough areas of practice to describe comprehensive family practice fully. It also includes all the items on Wong’s list of scope developed later.15 As with all surveys, these data must be interpreted bearing in mind that this was self-reported activity. It compares in several respects with the data from the National Physician Survey in 2004,4 and so we believe it is valid. The authors are currently preparing the results of another study16 approaching the issue from the evidence of billing data, as did Chan.2 Each method, ie, self-reporting and billing data, has its limitations and these we acknowledge.
The study may be criticized for the relatively lower response rate from the urban physicians compared with their academic colleagues, which may have introduced sampling bias, but in recent surveys of family physicians, this 50.9% is an acceptable return. The response rate for the National Physician Survey was 37% and for the Family Practice Quality and Capacity Study was 52%.4,8 Just over half of eligible physicians responded. The effect of response bias may be of importance. It is likely for a subject like this that physicians who believe in and practice comprehensive care will have found the topic both relevant and important enough to respond, whilst those less broadly active will be less motivated to do so. Even so, if only half of 72% (ie, 36%) of urban family physicians treat patients with human immunodeficiency virus or half of the 82% (ie, 41%) of urban family physicians offer sports medicine, there are still large percentages of urban physicians providing these services.
Wong15 found that “... none of the Canadian studies excluded family physicians and GPs with specialized practices” which would have affected the average scope of practice. This is because many licensing bodies list physicians in their registry by specialty, and nonspecialists are listed together, even though they are not all providing general services. We addressed this by including only urban physicians who declared that they were active in general practice more than 30% of the time.8
In this study we looked at urban physicians. Hutten-Czapski et al,17 using 1997 National Physician Survey data, showed that the greatest determinant of differences in procedures performed in general practice was size of community and distance from the nearest major centre.17 He also concluded that “... as geographic isolation increases, Canadian family physicians provide an increasingly broad range of services”. Altering the resident experience to include more time in rural practice might increase the scope of practice, and certainly those intending to practice rurally need to be trained in the widest scope.
What our data show is that large numbers of both academic and urban family physicians are providing a wide range of services and are performing a wide range of procedures which they have in common (Table 2). There are also differences between the two groups with respect to academic activities (as would be expected) and in out- of-hours care, which was not anticipated (Table 2). The higher out-of-hours coverage of hospital patients by academic physicians may reflect the activity of residents taking call for educational purposes, which would also make it less onerous for the academics to continue to provide. The educational role is also likely responsible for the significant differences in the procedures performed and the hospital-based activities, such as obstetrics and geriatrics (Table 3). Of interest is the reverse finding of greater activity on the part of the urban physicians in performing palliative care house calls and providing phone services for patient enquiries (Table 2).
Almost 40% of the urban physicians were involved in medical teaching. Gray has shown that, when comparing teaching and nonteaching general practitioners in the UK, the teaching general practitioners had shorter patient lists, devoted less time to clinical activities, and their practices had significantly better performance on quality indicators.18 There may be a causal relationship between these factors, but we did not examine quality in this study.
As regards planned changes in practice, the National Physician Survey 2004 found 25% of family physicians intended to reduce their hours worked and 11% intended to increase their teaching, research, or administrative work.4 It also found that involvement in mental health work had increased in the previous three years, and the amount of surgical assisting had increased, despite fewer family physicians performing this activity. In this study too, both groups of physicians were making some changes to their scope of practice (Table 4). The academic group had added slightly more services in the last two years, and was planning to add slightly more than the urban physicians in the next two years. They were considering withdrawing a few more services than their urban colleagues. This may represent an aspect of trend setting, shedding more and adding more activities than their urban colleagues, or may represent a response to perceived future directions in education.
Conclusion
Our study demonstrates that family physicians in the Capital Region are providing a wide range of services. Although academic and urban family physicians provide a wide range of services and share many similarities, there are also significant differences between them which may have consequences for the training of future urban family physicians. Forty percent of urban family physicians are involved in teaching, and 11% plan to increase this aspect of their work. Perhaps to align training to future practice, this trend should be encouraged. Although over 25% of urban family physicians have reduced services in the last two years and 12% are planning reductions, 14% have added services in the last two years and 6% are planning to add them The imbalance that we have demonstrated between academic practice and regular urban practice supports the current trend to increase the use of community-based practices as teaching sites and the trend to continuous integrated clerkships in which the learner is based in one rural or urban practice for all the family medicine experience. The postgraduate training model in the UK is based on longer-term placement in community-based practices, and this may be a model we might wish to follow in Canada.
Acknowledgments
The authors wish to thank Olga Szafran, Shufen Edmondstone, and Lana Atkinson for assistance with data analysis and preparation of the manuscript. The study was funded under the Family Practice Quality and Capacity Study.
Appendix
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Woodward CA, Cohen M, Ferrier B, Brown J. Physicians certified in family medicine. What are they doing 8 to 10 years later? Can Fam Physician. 2001;47:1404–1410. [PMC free article] [PubMed] [Google Scholar]
- 2.Chan BTB. The declining comprehensiveness of primary care. CMA J. 2002;167:429–434. [PMC free article] [PubMed] [Google Scholar]
- 3.Hutchinson A, Becker LA. How the philosophies, styles, and methods of family medicine affect the research agenda. Ann Fam Med. 2004;2:S41–S44. doi: 10.1370/afm.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada. National Physician Survey. Mississauga, ON: College of Family Physicians of Canada; 2004. [Accessed November 16, 2010.]. Available from: http://www.nationalphysiciansurvey.ca/nps/home-e.asp. [Google Scholar]
- 5.National Family Physician Workforce Survey. The Janus Project. College of Family Physicians of Canada; 2001. [Accessed April 21, 2011]. Available from www.cfpc.ca/uploadedFiles/Research/_pdfs/NFPWS2001EN.pdf. [Google Scholar]
- 6.Katz A, Soodeen RA, Bogdanovic B, De Coster C, Chateau D. Can the quality of care in family practice be measured using administrative data? Health Serv Res. 2006;4:2238–2254. doi: 10.1111/j.1475-6773.2006.00589.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quality and Outcomes Framework Statistics for England 2005/2006. London, UK: National Health Service; 2006. [Accessed November 16, 2010.]. Available from: http://www.ic.nhs.uk/webfiles/publications/qof/NationalQualityOutcomesFramework280906_PDF.pdf. [Google Scholar]
- 8.Moores DG, Wilson D, Cave AJ, Donoff M, Woodhead Lyons S. Family Physician Quality and Capacity Report. Edmonton, Canada: University of Alberta, Department of Family Medicine Research; 2001. [Google Scholar]
- 9.College of Physicians and Surgeons of Alberta. Find a Physician. 2005. [Accessed on March 13, 2006]. Available from: http://www.cpsa.ab.ca.
- 10.Lee RL. Family health networks in Ontario. CMAJ. 2003;168:152. [PMC free article] [PubMed] [Google Scholar]
- 11.Steel N. Differences in the quality of clinical primary care and targeted incentive payments: Do incentives work?. Presented at the Royal College of General Practitioners National Annual Conference; October 4–6, 2007; Edinburgh, Scotland. [Google Scholar]
- 12.Triple-C Competency-based Curriculum. Report of the Working Group on Postgraduate Curriculum Review. Mar, 2011. [Accessed April 21, 2011]. Available from www.cfpc.ca/uploadedFiles/education/_PDFs/WGCR_TripleC_Report_English_Final_18Mar11.pdf.
- 13.Van Royen P, Beyer M, Chevallier P, et al. The research agenda for general practice/family medicine and primary health care in Europe. Part 3. Results: Person-centred care, comprehensive and holistic approach. Eur J Gen Pract. 2010;16:113–119. doi: 10.3109/13814788.2010.481018. [DOI] [PubMed] [Google Scholar]
- 14.Statistical Package for Social Sciences.
- 15.Wong E, Stewart M. Predicting the scope of practice of family physicians. Can Fam Physician. 2010;56:219–225. [PMC free article] [PubMed] [Google Scholar]
- 16.Saunders D, Alibhai A, Cave AJ, Moores D, Woodhead-Lyons S. The work patterns of family physicians and general practitioners in Alberta. Edmonton, Canada: Department of Public Health Sciences, University of Alberta; 2006. [Google Scholar]
- 17.Hutten-Czapski P, Pitblado R, Slade S. Short report; scope of family practice in rural and urban settings. Can Fam Physician. 2004;50:1548–1550. [PMC free article] [PubMed] [Google Scholar]
- 18.Gray RW, Carter YH, Hull SA, Sheldon MG, Ball C. Characteristics of general practices involved in undergraduate medical teaching. Br J Gen Pract. 2001;51:371–374. [PMC free article] [PubMed] [Google Scholar]