Abstract
This study explores longitudinally a four-factor structure of pathological personality trait dimensions (PPTDs) to examine both its structural stability and intra-individual changes among PPTDs over time. Personality Disorder (PD) scales of the Millon Clinical Multiaxial Inventory-III were administered to 361 low-income women with various psychiatric conditions (drug dependence, depression), who were followed in a two-wave study over 5-years. Cross-sectional and longitudinal factor analyses outlined a robust factorial structure of PPTDs, extrinsically invariant over time, representing Negative Emotionality, Introversion, Antagonism and Impulsivity. Despite moderate rank-order stability in the PPTDs, results also indicated substantial intra-individual variability in the degree and direction of change, consistent with trajectories of change in participants’ clinical diagnoses. Results are discussed in light of current debates on the structure and dynamic of pathological personality.
Keywords: Pathological Personality, Personality Disorders, MCMI, Longitudinal Factor Analysis
1. Introduction
Current debates on the nature of personality disorders (PD) have included calls for an empirical structure of personality pathology to be incorporated in the new edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Toward this end, cross-sectional studies of clinical and non-clinical samples have sought to identify a factor structure of pathological personality trait dimensions (PPTD) that underlie PDs. While consensus is building for a four- to five-factor structure, longitudinal evidence for this structure is lacking, precluding the structural debate to be informed by developmental data. The need for longitudinal evaluation of PPTD is highlighted by a growing body of longitudinal research reporting significant rates of change in PDs over time, a finding that calls into question the notion that PDs are stable and enduring. Thus, ongoing developments in the understanding of PD will require such studies as the present one to determine (a) whether the structure of personality pathology is stable and reproducible over time, and (b) if structural stability excludes intra-individual changes in naturalistic and/or treatment conditions. The present study integrates the structural and developmental controversies of PD in a single model, through a longitudinal structural analysis of the PD scales of the Millon Clinical Multiaxial Inventory III (MCMI-III; Millon, Millon, Davis, & Grossman, 2006) among a sample of at-risk women followed over 5-years (Luthar & Sexton, 2007).
2. The Dimensional Nature of Personality Disorders and the Empirical Structure of Pathological Personality Traits
Proposed changes to the categorical conceptualization of PDs in the American Psychiatric Association’s (APA) Diagnostic and Statistics Manual of Mental Disorders (American Psychiatric Association, 2000) reflect a broader conceptual question of whether to define and describe personality pathology dimensionally, as a quantitatively extreme expression of normal functioning, or categorically, as a qualitatively distinct process (Wright, 2011). Limitations of the categorical model are well-recognized and dimensional models of PDs are favored by many (Eaton, Krueger, South, Simms, & Clark, 2011; Krueger, Skodol, Livesley, Shrout, & Huang, 2007; Widiger & Samuel, 2005; Widiger & Simonsen, 2005). As noted by Westen and Muderrisoglu (2006), virtually all these dimensional models are “trait models” derived from the factor analysis of self-report data. Research on the empirical structure of pathological personality trait dimensions (PPTDs) has identified four broad domains appearing with reasonable consistency in cross-sectional studies. They include: (a) negative emotionality or emotional dysregulation, (b) introversion or detachment, (c) antagonism, and (d) disinhibition (Krueger et al., 2011; Livesley, 2007; Sheets & Craighead, 2007; Widiger & Simonsen, 2005). Many studies (e.g., Tackett, Silberschmidt, Krueger, & Sponheim, 2008), and meta-analyses (e.g., O’Connor, 2005), have identified these same domains that purportedly tap the core traits underlying pathological personality functioning through structural analysis of numerous self-rated pathological personality inventories.
Many have also observed that these four factors are recognizable as maladaptive variants of “normal” personality, as operationalized for instance with the Five Factor Model (FFM) of personality (e.g., Lenzenweger, 2010; Widiger & Costa, In press). Therefore, researchers and clinicians alike have advocated for the reconceptualization of personality pathology within the multidimensional space of a “normal” personality model such as the FFM (e.g., Lynam, in press; Markon, Krueger, & Watson, 2005; O’Connor, 2005; Samuel & Gore, in press). Accordingly, meta-analyses have confirmed the relationship between current DSM personality disorders and the FFM, with strong relationships observed in four of the five domains, excepting the domain of Openness, which overlaps only weakly (Samuel & Widiger, 2008). Consistently, the maladaptive variant of Openness (often referred to as Psychoticism, and covering major features of Schizotypal PD) is the smallest (Widiger & Simonsen, 2005) and least stable, and as such is often under-identified in factor analyses of PD inventories that are not specifically designed to capture this domain, while the other domains appears with great consistency in many PD inventories.
For example, attempts to validate the theoretical model of personality pathology underlying the MCMI-III have found little consistency for the presumed theoretical model (Mullins-Sweatt & Widiger, 2007; O’Connor & Dyce, 1998). In addition, questions have emerged regarding the ability of this instruments to discriminate between distinct PD categories and to serve as robust diagnostic tool in practical settings given the rather high overlap between MCMI-III PD scales (e.g., Rogers, Salekin & Sewell, 1999). This overlap suggests that a careful examination of MCMI structure is needed to reveal the higher-order constructs (PPTDs) underlying the covariation between scale scores (Philippe Rushton and Irwing, 2009). In this line, a four-factor structure often appeared to be the best underlying model with MCMI data gathered from various clinical and non-clinical samples across cultures (e.g., Cuevas, García, Aluja, & García, 2008; Dyce, O’Connor, Parkins, & Janzen, 1997; Rossi, Elklit, & Simonsen, 2010). These four factors have been observed to align well with the four PPTDs introduced above (Krueger et al., 2011; Rossi et al., 2010), thus further supporting the relevance of the four-factor model of maladaptive personality traits underlying PDs, as this structure is identifiable across a number of assessments of personality pathology which sample a comprehensive range of PD facets, such as the MCMI-III. In the present study, we seek to explore the extrinsic (i.e. structural) and intrinsic (i.e. within-individual) stability of this four-factor structure of PD over time, as represented in the MCMI-III. Although the MCMI was designed to understand the development and course of individual psychopathology in the context of an individuals’ personality (Millon, 1983), relatively few longitudinal analyses have been conducted with this instruments.
3. Stability and Change of Pathological Personality Structure and Diagnosis
Until recently, the empirical literature documenting long-term stability of personality pathology has been limited (Lenzenweger, 1999, 2010). Moreover, most longitudinal studies on PDs have exhibited methodological problems that limited their conclusions (Skodol, 2008), including ignoring inherent unreliability in the measurement of change (Ferguson, 2010). A new generation of rigorous longitudinal studies of community population and clinical samples has emerged (Lenzenweger, 2006; Skodol et al., 2005; Skodol, 2008) and has revitalized a debate regarding the stability of PDs (Clark, 2007; Krueger & Tackett, 2005; Skodol, 2008). Longitudinal evidence from clinical and non-clinical samples has revealed that individual change in pathology personality traits occurs for individuals both in- and out-of-treatment, and these changes differ considerably across individuals (Johnson et al., 2000; Lenzenweger, Johnson, & Willett, 2004; Watson, Clark, & Chmielewski, 2008).
As a general trend, longitudinal studies suggest that personality pathology improves over time (i.e. symptoms decrease) at significant rates (Grilo et al., 2004; Grilo et al., 2010; Johnson et al., 2000; Lenzenweger et al., 2004; Lenzenweger, 2010; Sanislow et al., 2009; Skodol et al., 2005; Skodol, 2008). However, several studies report rank-order and mean-level stability difference according to the diagnostic approach used: dimensional or categorical (Johnson et al., 2000; Samuel et al., 2011). The dimensional system yields significantly greater stability, especially when using self-report questionnaires as opposed to structured interviews (Samuel et al., 2011). These findings suggest conceptual limitations inherent in categorical models of PDs, in particular, the use of arbitrary thresholds (Grilo et al., 2004) leading to measurement error in diagnosis (Clark, 2007). Research has also evidenced differential stability across PD categories regardless of the method for diagnosis (e.g., Durbin & Klein, 2006; Nestadt et al., 2010). Usually, Cluster B disorders (Antisocial, Borderline, Histrionic Narcissistic) tend to exhibit the highest long-term stability (Durbin & Klein, 2006).
The mechanisms by which change in personality pathology occurs are still not well understood. Lenzenweger and Willett (2007) proposed that change in PD features result from changes in neurobehavioral systems that manifest as pathological personality traits. Consistently, Warner and colleagues (2004) have proposed that personality traits (such as the PPTDs) may represent causally proximal mechanisms that influence the expression and variability of PD over time. If so, a greater understanding of the dynamic of change of maladaptive personality traits is of paramount importance for both theory and treatment (see Warner et al., 2004). Despite evidence of change in personality pathology, the DSM-IV-TR still defines PDs as “stable and enduring, reflecting a persistent pattern of maladaptive personality throughout the life course” (e.g., Skodol, 2008).
Although evidence for such stability is mixed, researchers have made limited attempts to integrate the developmental and the structural controversies of personality traits underlying PDs, placing the “core structure” of PPTDs (i.e., the four-factor structure outlined above) in a longitudinal perspective. Among these attempts, an integrative hypothesis suggests that PDs may be characterized by maladaptive trait constellations that are stable in their structure but can change or fluctuate in severity or expression over time (Grilo et al., 2004). Nevertheless, only Sanislow and collaborators (2009) examined the longitudinal invariance of such PD latent constructs (i.e. their “extrinsic” stability), but these constructs were not aligned with the more widely accepted maladaptive variants of the FFM, that is, the core PPTDs. Such a longitudinal examination would provide additional support for the empirical structure of personality pathology. Furthermore, longitudinal analyses of the PPTDs will likely contribute to a better understanding of PDs development and change.
The objective of the present study was (a) to investigate the longitudinal stability of the four PPTDs structure by testing its factorial invariance over a five-year delay (i.e., extrinsic stability), while examining (b) within-individual change in PPTD levels (i.e., intrinsic stability). We then compared the average levels of PPTDs as a function of various groups (such as substance-abusing, depressed, and a non-clinical group), as well as within-individual change in the PPTD levels as a function of patterns of stability, remission, and other forms of change in the clinical diagnosis as derived through an external DSM-based assessment. This focus was meant to elucidate (c) the ability of the PPTD constructs to discriminate various clinical groups, and (d) their sensitivity to change in participant’s mental health condition, informing their usefulness to capture the pathological personality component of various psychopathological conditions beyond PDs solely.
4. Method
The study sample chosen for the study consisted of high-risk clinical and non-clinical mothers, as such a population is expected to have a high prevalence of pathological personality traits. To address many methodological issues generally disregarded in the study of personality stability and change, and in particular, the unreliability in the measurement of change (Ferguson, 2010), both PPTD structure and development were examined at a latent level, in a structural equation modeling framework.
4.1 Participants
Data used in the present study was collected through a longitudinal research project on maternal drug abuse, psychopathology, and child adaptation (Luthar & Sexton, 2007). The initial sample consisted of 361 low-income mother-child dyads living in an urban area of Connecticut, who have been followed since 1996. At the launch of the project, mothers’ age ranged from 23.5 to 55.8 (Mage = 38.2 years, SD = 6.2) and included women of African-American (51.5%), Caucasian (34.2%), Hispanic (6.3%), Native American (0.8%), Asian (0.3%) or Mixed (5%) descent (2% of the participants were unidentified ethnically or culturally). Women were recruited from outpatient treatment facilities for substance abuse and other mental health problems (chiefly depression and anxiety), as well as from community settings. Therefore, the sample comprises both clinical and non-clinical groups, including a high prevalence of substance use disorders, historically associated with PDs (e.g., Jahng et al., 2011). “Clinical group” membership in this study was defined by the presence of a DSM diagnosis at the time of data collection (see Data Analyses section).
4.2 Instruments
4.2.1 DSM diagnoses
The Computerized Version of the Diagnostic Interview Schedule (DIS-IV; Robins et al., 2000) was used to assess major psychiatric disorders as defined in the DSM-IV. The DIS-IV is a fully structured questionnaire designed to identify the presence of psychiatric disorders by quantifying psychiatric symptoms endorsed by a respondent. It offers a lifetime history of symptoms as well as a diagnosis of current syndrome (a disorder is counted as current if any of its symptoms had been present within the past year). Due to the fully structured, highly standardized nature of the measure, non-clinicians may administer the DIS-IV with high level of reliability. Metric properties of the DIS-IV and previous versions have been studied extensively and showed fair to excellent level of inter-diagnostician reliability (Kappa ranging from .40 to .77 with non-clinician interviewer) with various samples, including substance abusers (e.g., Dascalu, Compton, Horton, & Cottler, 2001), and strong agreement between other DSM instruments (e.g., Hasin & Grant, 1987) supporting its good criterion validity (Malgady, Rogler, & Tryon, 1992).
4.2.2 Personality pathology
The MCMI-III (Millon et al., 2006) is a widely used, 175-item, self-report inventory which consists of 24 clinical scales including 14 pathological personality scales. The Clinical Personality Pattern scales which represent mild to moderate personality pathologies include: Schizoid, Avoidant, Depressive, Dependent, Histrionic, Narcissistic, Antisocial, Aggressive (Sadistic), Compulsive, Negativistic, and Masochistic scales. In addition, three severe personality pathology scales are included: Schizotypal, Borderline, and Paranoid. Across contexts (such as substance abusing samples; e.g., Hesse, Guldager, & Holm Linneberg, 2012), this instrument displays strong psychometric properties including proper reliability and validity (Millon et al., 2006).
4.3 Procedure
All women who expressed interest in participation were screened to determine eligibility for the main research program (Luthar & Sexton, 2007). Women were screened for psychotic features and excluded if they were on antipsychotic medications and/or had a history of psychosis. Before being enrolled in the research program, voluntary informed consent was obtained. After each measurement occasion, participants were compensated monetarily for their participation.
The first measurement occasion of this project (T1) occurred in 1996; Participants were contacted by phone and mail to take part to the follow-up (T2) and a large part of the sample returned, after an average of 60 months (five years). For both measurement occasions, DIS-IV interviews were conducted by trained non-clinician interviewers, and MCMI-III protocol were self-administered. Following the MCMI-III scoring guideline (Millon et al., 2006), only complete and valid test-profiles were used. One profile at T1 and 4 profiles at T2 were invalidated. As a result, 80% of the parent sample (N = 288) presented complete data (i.e., DIS-IV diagnoses and MCMI scores) at both T1 and T2. Attrition analysis demonstrated that the prevalence of the various clinical groups at T1 were highly similar across complete (with complete data at both T1 and T2) and incomplete respondents (with complete data at only T1), indicating that attrition was not biased toward a particular clinical group (χ2= 2.4, df = 3, p = .49).
4.4 Data Analyses
4.4.1 Grouping DSM diagnosis and trajectories of change in diagnosis
Current DSM diagnoses for both T1 and T2 (determined with the DIS-IV), were first stratified into four main groups at each measurement occasion in view of planned analyses: Substance only (substance dependence without affective/anxiety disorders); affective/anxiety only (depressive or anxiety diagnoses without substance dependence), comorbid (substance dependence and affective/anxiety diagnoses), and neither (neither substance dependence nor affective/anxiety diagnosis). Specifically, the substance only group included 7.6% of the sample at T1 and 3.1% at T2. The affective/anxiety only group represented 26.7% at T1 and 15.3% at T2. The comorbid group represented 8% of the participants at T1 and 3.1% at T2. Participant with neither substance dependence nor affective/anxiety diagnosis (neither) included 57.6% of the participants at T1 and 74% at T2. Despite the apparent trend of reduction of clinical diagnosis between T1 and T2 (i.e., increase of the prevalence of the neither group), these group distributions mask considerable variability in the observed patterns of change. Figure 1 depicts the four-state transition matrix between DSM diagnosis over time, revealing patterns of remission, stability, and transition across the clinical groups.
Figure 1.
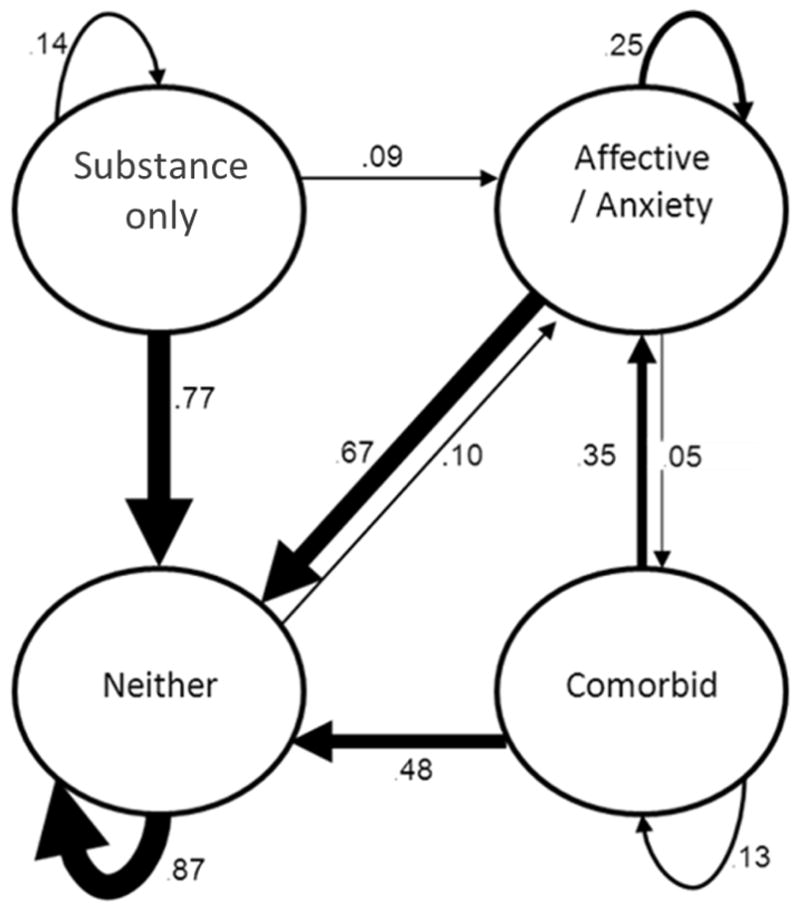
Simple four-state diagram of transition in the DSM diagnosis groups over time. Values represent transition probabilities. The thickness of the lines is proportional to the probabilities of transition. Autoregressive arrows represent probability of stability. Transition path below .05 are not represented in the diagram.
For example, participants assigned to the comorbid group at T1 were mostly found in the neither group at T2. Indeed, 48% of this group was characterized by “remission,” while 35% “transited” to the group with depression or anxiety disorders without substance dependence (they assigned to the affective/anxiety only group). Finally, only 13% of the members of the comorbid group at T1 remained in this group at T2. Based on the main patterns of change observed in our data, we proceeded to a second classification of participants into three main forms of change in the clinical group: “stable”, namely participants assigned to the same group at both T1 and T2 (57.8% of the sample of complete cases); “remission”, participants assigned to a clinical group at T1 (substance only, affective/anxiety only or comorbid) and then assigned to the neither group at T2 (28%), and “newly diagnosed”, herein, participants with no diagnosis of substance dependence nor affective/anxiety at T1, who fell into one of the three clinical group at T2 (8%). Under-represented pathways (including a total of 6.2% of the trajectories) were not included in analyses using this grouping system.
4.4.2 Modeling MCMI-III PD structure, longitudinal invariance, and latent change
Only the 14 MCMI-III PD scales were used in this study, as we focus on PD organization only. Following recommendations in the literature (Cuevas et al., 2008; Dyce et al., 1997; Rossi et al. 2010), MCMI-III Linearly Independent Scales (LIS) scores were used as the basis of all analyses in this study. LIS scores are computed by averaging the “prototypal” items for each PD scale, as these items are the most central indicators of the personality disorder construct (Millon et al., 2006). The resulting scores have the advantage of reducing artificial colinearity between scales without losing content validity (Rossi, van der Ark, Andries, & Sloore, 2007). Preliminary analyses indicated that the LIS scores were highly congruent with the original full-scales scores (i.e. computed following the MCMI-III manual) with median correlation of .96 between LIS and full-scale scores at both Time 1 and Time 2.
Confirmatory Factor Analyses (CFA) in a structural equation modeling approach using Full Information Maximum Likelihood estimation (FIML) were used to estimate the fit of two-, three-, and four-factor models of the MCMI-III PD structure commonly identified in the literature. The specifications of these models were the same as those described by Rossi and colleagues (2010). At a second stage, the initial models were improved using modification indices suggesting which parameter could be fixed or set free (correlated error terms were allowed only if they were tenable conceptually. The chi-square difference test (Δχ2) was used to estimate the statistical significance of the improvement in fit of the various models.
The model fitting the best T1 and T2 data was then extended into a single longitudinal multivariate factor model (e.g., McArdle & Nesselroade, 1994) to test for structural invariance over time. In addition, we implemented a multiple-common-factor latent change score (LCS) model (e.g., Ferrer & McArdle, 2010; McArdle, 2009) allowing estimation of mean-level change in the PPTD factors at a latent level, as well as correlations between these change factors. This approach avoids the problems inherent in using difference scores such as cumulated errors and regression to the mean (McArdle & Nesselroade, 1994; McArdle, 2009), that are rarely addressed in the personality-stability and -change literature (Ferguson, 2010). The fit of all models was assessed using the Chi-square tests of fit and four other widely used indexes: The normed fit index (NFI), the comparative fit index (CFI), the root mean square residual (RMR), and the root mean square error of approximation (RMSEA) with its 90% confidence interval (e.g., Kline, 2010). A final set of multivariate analyses of variance (MANOVA) was conducted to examine the typical profile of PPTDs associated with the four clinical groups. Following recent support for the dynamic modeling of psychological processes (Ferrer & McArdle, 2010), trajectories of change in the clinical group (stable, remission, and newly diagnosed) were also examined using a MANOVA and Tukey post-hoc tests to further explore the association between change in psychiatric condition over time, with level of change in the PPTD.
5. Results
5.1 Preliminary Analyses
Internal consistency of the MCMI-III LIS scores was moderate (e.g., Histrionic, Narcissistic) to high (e.g., Avoidant, Depressive), with consistent Cronbach’s alphas coefficients across measurement occasions, ranging from .62 to .89 (MT1 = .70, MT2 = .71). Distributions of the LIS scores suggested possible violation of the assumption of a multivariate normal data distribution required for planned factor analysis. Consequently, normal scores using the Rankit transformation method (Solomon & Sawilowsky, 2009) were computed and yielded distributional features much closer to the Gaussian distribution. Subsequently, the properties of the correlation matrices obtained from the 14 MCMI-III LIS normal scores for both T1 and T2 were examined to ensure their suitability for use in the factor analyses. The correlation matrices were not identity matrices (T1 Bartlett’s test of sphericity = 3177.7, df = 91, p < .001; T2 Bartlett’s test of sphericity = 2757.7, df = 91, p < .001) and the global measures of sampling adequacy (KMO) were excellent (.94 at both T1 and T2), reflecting individual measures of sampling adequacy (MSA) that were acceptable to excellent (ranging from .61 to .97 at T1, and from .52 to .96 at T2). Thus, the correlation matrices had the proper features to be used in factor analyses.
5.2 Underlying Pathological Personality Trait Dimensions
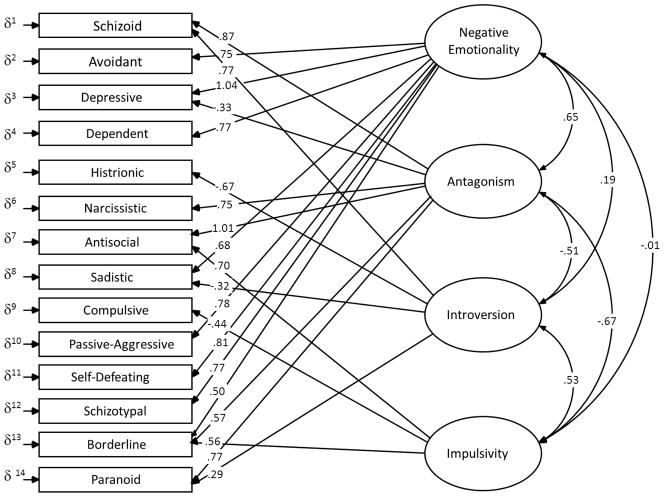
Table 1 display the fit indices obtained from the three initial models (i.e., two-, three-, and four-factor models) and their adjusted version as suggested by the modification indices, with T1 and T2 data, separately. The adjusted models consist of improved versions of the initial models, adding 1 to 3 modest correlated errors terms which made substantive sense. In accordance with prior results (Rossi et al., 2010), the two-factor and three-factor models were associated with poor fit, even in their “adjusted” form. As confirmed by the Δχ2 significance, the best-fitting models for each measurement occasion were the models with four factors (in both their “initial” and “adjusted” versions), with all fit statistics indices falling within the acceptable to excellent range (Kline, 2010). This solution was parsimonious with four factors explaining a total of 62.1% of the variance of the 14 MCMI PD scales used in the model, with explained variance ranging from 19.7% (Compulsive) to 84% (Borderline) across indicators. Factor loadings of this four-factor model were similar at both time points (Tucker-Burt-Wrigley-Neuhaus congruence coefficient = .91, .75, .83 and .86 for Factors 1, 2, 3 and 4 respectively). Thus, we derived a consensus factor structure (cf. O’Connor, 2005) from both loading matrices, used for the sake of clarity when interpreting the factor composition. This structure and its related factor consensus loadings are depicted in Figure 2.
Table 1.
Goodness of Fit Indices of the Cross-sectional and Longitudinal Models
| Model | χ2 | df | χ 2/df | p | Δ χ2 | NFI | CFI | RMR | RMSEA (CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Models T1 | ||||||||||
| 2F Initial | 322.1 | 70 | 4.6 | < .001 | _ | .90 | .92 | .056 | .100 | (.089 – .111) |
| 2F Adjusted | 263.6 | 68 | 3.9 | < .001 | < .001 | .92 | .94 | .056 | .089 | (.078 –.101) |
| 3F Initial | 223.5 | 64 | 3.5 | < .001 | < .001 | .93 | .95 | .042 | .083 | (.071 – .095) |
| 3F Adjusted | 200.4 | 63 | 3.2 | < .001 | < .001 | .94 | .96 | .040 | .078 | (.066 – .090) |
| 4F Initial | 118.4 | 55 | 2.2 | < .001 | < .001 | .96 | .98 | .024 | .057 | (.043 – .071) |
| 4F Adjusted | 94.3 | 54 | 1.7 | < .01 | < .001 | .97 | .99 | .022 | .046 | (.030 – .061) |
| Models T2 | ||||||||||
| 2F Initial | 290.1 | 70 | 4.1 | < .001 | _ | .90 | .92 | .054 | .105 | (.092 – .117) |
| 2F Adjusted | 255.7 | 69 | 3.7 | < .001 | < .001 | .91 | .93 | .043 | .097 | (.082 –.110) |
| 3F Initial | 204.4 | 64 | 3.2 | < .001 | < .001 | .93 | .95 | .034 | .087 | (.074 – .101) |
| 3F Adjusted | 173.0 | 62 | 2.8 | < .001 | < .001 | .94 | .96 | .033 | .079 | (.065 – .093) |
| 4F Initial | 147.2 | 55 | 2.7 | < .001 | < .001 | .95 | .97 | .026 | .076 | (.062 – .091) |
| 4F Adjusted | 86.1 | 52 | 1.7 | < .001 | < .001 | .97 | .99 | .021 | .048 | (.029 – .065) |
| Longitudinal Modelsc | ||||||||||
| 4F Free change | 436.8 | 276 | 1.58 | < .001 | _ | .93 | .97 | .025 | .045 | (.037 – .053) |
| 4F Invariant | 464.0 | 302 | 1.54 | < .001 | .40 | .93 | .97 | .030 | .043 | (.035 – .051) |
| 4F Latent Change Score | 531.4 | 314 | 1.69 | < .001 | _ | .92 | .96 | .071 | .049 | (.049 – .056) |
Note. χ2 = chi-square; df = degrees of freedom; p = p value of the chi-square test; Δ χ2 = p value of the chi-square difference test; NFI = Bentler-Bonett normed fit index; CFI = Comparative fit index ; RMR = root mean square residual ; RMSEA = root mean square error of approximation; CI = 90% confidence interval of RMSEA value.
Figure 2.
Four factor model of PPTD outlying the MCMI-III PD scores. For the sake of clarity, loadings under |.25| are not represented in the model.
Based upon the most salient loadings estimated in this model (which were ordered in a similar way to those obtained by Dyce et al.1997; Rossi et al., 2010), we named each factor as follows: Factor 1 was labeled “Negative Emotionality” as it displayed high loadings on many PD scale items, in particular on the Depressive, Self-Defeating, and Avoidant scales. Factor 2 was labeled “Antagonism” and was mostly loaded with the Antisocial, Schizoid, Paranoid and Narcissistic scale items. Factor 3 was identified as the “Introversion” bipolar dimension, with high and negative loading on the Histrionic scale on one end, and a high, positive loading in the Schizoid scale on the other end. Finally, Factor 4 was labeled “Impulsivity”, representing Compulsivity on one end, and the Antisocial and Borderline scales on the other end. Given the composition of this factor and its pattern of association with the other PPTDs in the tested population, this factor was thought to represent mainly the self-damaging and self-injurious impulsivity features (rather than impulse aggression for example) often associated with Borderline personality disorders. The correlations between the factors were as follows: Factor 1 correlated .65, .19, and −.01 with factor 2, 3 and 4, respectively. Factor 2 correlated −.51, and −.67 with factor 3 and factor 4 respectively, and factor 3 correlated .53 with factor 4 (Figure 2).
5.3 Longitudinal Structural Invariance and Individual Change
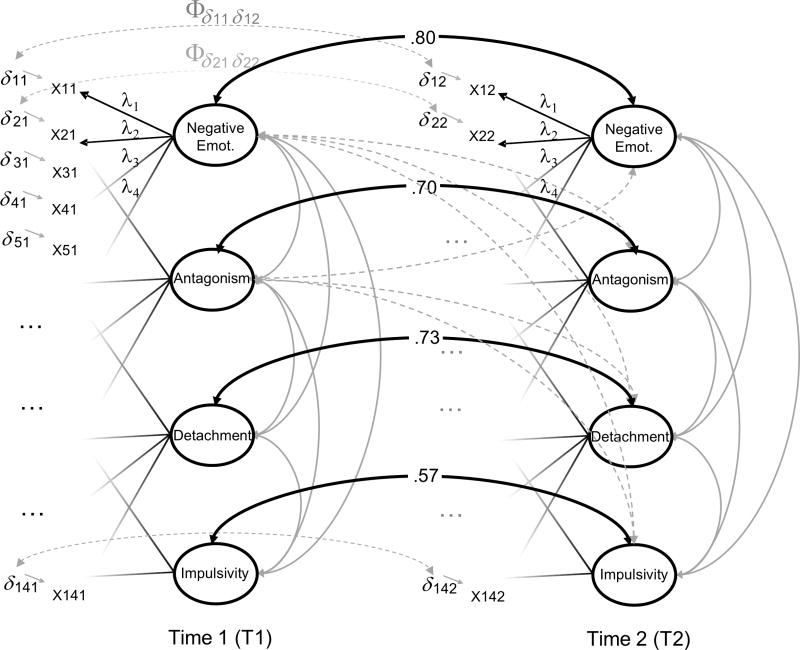
In order to confirm longitudinally this outlined four-factor structure of PPTD as represented in the MCMI-III, we specified a single longitudinal multivariate factor model (e.g., McArdle & Nesselroade, 1994), as shown in Figure 3a. Specifically, two versions of this longitudinal factorial model were tested to estimate measurement invariance over time. In the first model, we set free the estimation of the factor loadings at each time point (“free change” model). The second model tested the hypothesis of the equality of the factor loading over time (“invariance” model), to confirm that the latent construct measured at each time point had the same substantive meaning (McArdle & Nesselroade, 1994). Model fit indices of these two alternative models are presented in Table 1. As indicated, both models displayed very similar, adequate fit to the data with fit indices in the acceptable to good range. More importantly, the measurement invariance model did not display a significant degradation in fit as compare to the free change model (Δ χ2 = 27.2, df = 26, p = .40; Δ CFI = .000), holding the hypothesis of the equality of the factors loading over time.
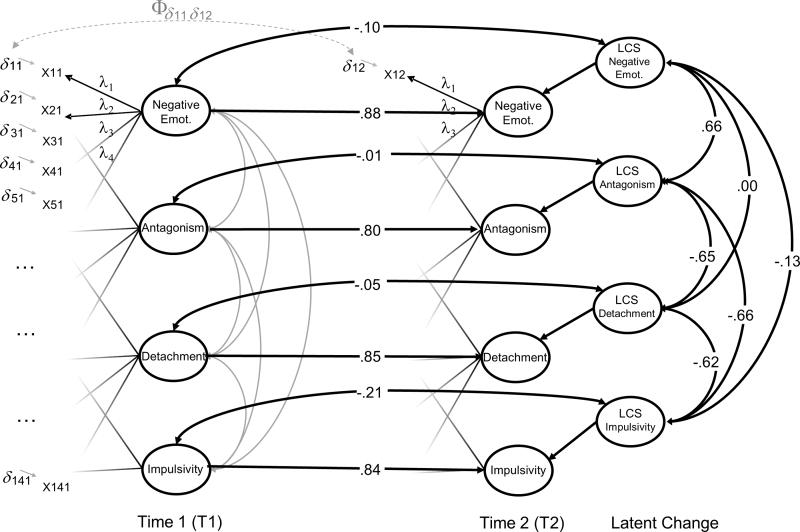
Figure 3.
(a) Longitudinal factorial model of PPTD with loadings invariance; (b) Multivariate latent difference score model of PPTD. Negative Emot. = Negative Emotionality; LCS = Latent change scores.
The evidence of “extrinsic” stability of the PPTD factor structure underlying the MCMI-III PD scores allowed the examination of intrinsic, or within-person change in two common-factor scores over time (McArdle & Nesselroade, 1994): cross-lagged correlation of two common-factor scores indicated rank-order stability of .80, .70, .73 and .57 respectively for Negative Emotionality, Antagonism, Introversion and Impulsivity (Figure 3a). In contrast, rank-order stability coefficients of the 14 individual MCMI-III PD scales (at the basis of the four PPTD constructs) yielded lower stability, with test-retest intra-class correlation coefficients ranging from ICC = .38 (p < .001) for the Compulsive Scale to ICC = .69 (p < .001) for the Avoidant Scale (average ICC = .59, SD = .07). Given the delay between the measurement occasions in this test-retest analysis (five years), stability coefficients obtained with both the PPTDs and PPTD indicators (i.e., PD scales) are interpreted in terms of stability of the constructs measured, rather than in terms of reproducibility of the scores per se (i.e., test-rest reliability). In this context, results suggest rather high levels of rank order stability in the PPTDs constructs (latent factor scores) and moderate stability of the PD constructs (manifest scale scores).
In a second step, we built upon the longitudinal invariant model (Figure 3a) to introduce new latent scores that represented the latent change between two common-factor scores (one latent change factor for each PPTD construct). This multiple-common-factor latent change score (LCS) model (e.g., McArdle, 2009) represented in Figure 3b, fit our data adequately (Table 1). The mean estimated in the LCS were all different from 0 suggesting significant change over time (with MNegative Emotionality = −.11, p < .001; MAntagonism = −.12, p < .001; MIntroversion = .08, p = .06; MImplulsivity = .10, p = .011). In addition, the variances in the LCS factors were all different from 0 (p < .001) indicating substantial individual differences in the level and direction of change, and allowing the estimation of inter-correlations between the four LCS which were as follows: Negative Emotionality LCS correlated .66, .00, and −.13 with Antagonism LCS, Introversion LCS and Impulsivity LCS respectively. Antagonism LCS correlated −.65, and −.66 with Introversion LCS and Impulsivity LCS respectively, and Introversion LCS correlated .63 with Impulsivity LCS.
5.4 DSM Diagnoses Groups and their Pathological Personality Traits Correlates
Individual factor-scores were derived for each PPTD factor and their LCS extension using the regression method. The MANOVA on the PPTD factor scores at T1, using the clinical group (substance only, affective/anxiety only, comorbid and neither) as group factor, yielded a significant effect (F [12, 743.7] = 12.78; p < .001; η2 =.17). This effect is considered to be large in size (η2 < .14) as suggested by accepted benchmarks in the literature. This analysis was replicated with T2 data, showing a lower, yet substantial effect size (F [12, 709.4] = 4.88; p < .001; η 2 = .08). This reduction in effect size could be explained by the reduction of sample size in some clinical groups at T2 (as patterns of remission between T1 and T2 were frequent). The Tukey’s post hoc tests used in complement of these MANOVAs, permitted to identify the variables for which the groups differed significantly.
As indicated by the descriptive statistics in Table 2, each clinical group was associated with significant level differences on the four PPTD factors scores. The main features of the participants in the neither group were lower levels on all four PPTD factor score. The substance only group was associated with moderate scores on Negative Emotionality, Antagonism and Impulsivity, and rather low scores on Introversion. Finally, the affective/anxiety and comorbid groups (with affective/anxiety disorders and substance dependence) displayed similar average profiles, except on the Impulsivity factor where the comorbid group tended to show higher levels. The one-way ANOVA suggested that it was mostly the Negative Emotionality factor that differentiated the best between the four clinical groups (η 2= .26).
Table 2.
Average Differences in PPTD Factor Scores as a Function of the Clinical Group and Result of the Univariate Analyses
| PPTD Factor | Substance Only | Affective/Anxiety Only | Comorbid | Neither | Univariate Results | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M (SD) | M (SD) | M (SD) | M (SD) | F (3, 284) | p | η² | |
| Negative Emotionality | .05 (.90) | .69 (.96) | .81 (.78) | −.44 (.79) | 38.82 | < .001 | .26 |
| Antagonism | .13 (.87) | .31 (1.18) | .29 (.89) | −.20 (.89) | 5.87 | <.001 | .06 |
| Introversion | −.19 (.66) | .27 (1.26) | .33 (1.17) | −.15 (.83) | 4.35 | <.01 | .04 |
| Impulsivity | .09 (.91) | .20 (1.19) | .72 (1.12) | −.20 (.82) | 7.91 | < .001 | .08 |
5.5 Change in DSM Diagnosis and Associated Changes in Personality Pathology Traits
The MANOVA on the LCS (representing change between T1 and T2), using the Trajectories of Change in the clinical group (stable, remission and newly diagnosed patterns) indicated a moderate but significant effect (F [8, 504] = 3.46; p < .001; η 2 = .08). As detailed in Table 3, patterns of stability in DSM diagnoses over time (stable group) were associated with mean-level stability of all the PPTD factor scores. Pattern of remission was associated with a mean-level decrease in both Negative Affectivity and Antagonism factor scores. Finally, patterns of “newly diagnosed” (no diagnosis of substance use nor affective/anxiety at T1 followed by any diagnosis at T2) were characterized by a mean-level increase in Negative Affectivity, Introversion, and Impulsivity.
Table 3.
Average T1-T2 Level of Change in the PPTD Factor scores as a function of the Pattern of Change in the Clinical Group.
| PPTD Factor | Stability | Remission | Newly Diagnosed | Univariate Results | ||
|---|---|---|---|---|---|---|
|
| ||||||
| M (SD) | M (SD) | M (SD) | F (2, 255) | p | η2 | |
| Negative Emotionality | −.03 (.39) | −.27 (.36) | .07 (.46) | 11.78 | <.001 | .08 |
| Antagonism | −.04 (.44) | −.22 (.37) | −.08 (.41) | 4.86 | <.01 | .04 |
| Introversion | .02 (.30) | .03 (.32) | .15 (.33) | 1.71 | ns | - |
| Impulsivity | .03 (.29) | .05 (.26) | .12 (.20) | 1.14 | ns | - |
6. Discussion
The results presented in this study offer new insight into the underlying structure and development of PDs. Both contributions are discussed separately, then in combination, to outline the strengths and limitations of this study, as well as important directions for future research.
6.1 Structure of the Higher-Order Pathological Personality Trait Dimensions
The PPTDs identified in our study are comparable to those presented by Rossi and collaborators (2010) except for the fourth factor (Impulsivity) which appeared less independent than expected. This discrepancy may be due to the nature of our sample (women only, with over-representation of substance dependence), as the dimension of impulsivity has been implicated in many forms of substance use disorder (e.g., Hicks, Markon, Patrick, Krueger, & Newman, 2004). As a result (or due to other factors not controlled in this study), the pattern of loadings obtained here suggest an impulsivity factor that aligns more with self-injurious impulsivity rather than the aggressive impulsivity that is represented in structural analyses of MCMI-III PD scales obtained with other samples. As a whole, the pattern of inter-correlation between PPTDs is also consistent with a broad “general maladjustment factor” suggested by Millon and collaborators (2006) from the overall pattern of moderate to high intercorrelations between MCMI-III scales scores, further confirmed by Philippe Rushton and Irwing (2009).
However, excluding the fifth PPTD which is underrepresented in the MCMI-III, our results confirm that a four-factor solution best achieves the goal of simplification without excessive loss of information (Dyce et al., 1997; O’Connor & Dyce, 1998), as suggested by the rather high amount of total variance in MCMI-III PD scores explained by four factors. It results in a meaningful structure of PPTDs, which represent four delineated constructs, interpretable independently, and associated soundly with various clinical conditions. Indeed, beyond the relative alignment of our PPTD constructs with four of the five higher-order constructs of PPTD proposed for the DSM-5 (Krueger et al., 2011), our results revealed coherent average profiles of PPTD factor scores as a function of four broad clinical groups identified with an external DSM-based measure (substance only, affective/anxiety only, comorbid, and neither), supporting their interpretability and practical relevance. Low scores on the four PPTD were observed in the group with no present DSM diagnosis, while the groups with substance dependence (substance only and comorbid) showed similar profiles (higher scores for the comorbid group) with a relative “apex” on the Impulsivity domain. The affective/anxiety only and comorbid groups showed a coherent average profile with high Negative Emotionality associated with high Impulsivity for the comorbid group. Together, these group differences suggest that the four core PPTD discriminate, albeit broadly, various forms of psychopathology (i.e. broad quasi-syndromal diagnostic groups).
6.2 Rank-order and Mean-level Stability and Change in PPTD
The question of structure stability of PPTD was examined longitudinally, demonstrating the robustness of the four PPTD structure over time, and allowing the study of these construct in a developmental perspective. As pointed out above, the relatively long delay between the two measurement occasions in this study (five years) allowed an analysis of the PPTD constructs stability and changes. However, further study of the PPTD constructs using shorter test-retest delay would allow for estimating the PPTD scores reproducibility, and further strengthening the interpretability of their stability and change across longer periods. Consistent with prior studies (e.g., Grilo et al., 2004; Grilo et al., 2010), the relative stability of individual differences (rank-order stability) was moderate (Impulsivity) to high (Negative Emotionality) given the study period. The relatively lower rank-order stability of the Impulsivity domain may indicate a higher sensitivity to change in this domain, possibly influenced by other factors such as differential effects of treatment or environmental influences. We also observed that the change on the PPTDs differ considerably across individuals (as evidenced by the significant variance in the LCS factor), supporting earlier results (Johnson et al., 2000; Lenzenweger et al., 2004). As a whole, changes in the Antagonism, Introversion, and Impulsivity domains were highly related (with change in Antagonism being on the opposite direction than the two other domains, i.e. increases in Introversion and Impulsivity were associated with decreases in Antagonism, and vice versa). Interestingly, change in Negative Emotionality was only related to change in Antagonism, and was independent to change in Introversion and Impulsivity. This new set of results appears highly informative to better understand PPTD dynamics of change, which could translate into a new perspective for understanding the dynamic underlying change in PDs in the setting of other psychiatric conditions.
When stability is considered at the mean level, our results suggest an overall pattern of decrease on the PPTD scores, and a prevalent trajectory of remission with the DSM group change. These results are consistent with well-established findings that suggest a general trend of improvement in PDs and other psychopathology over time (Johnson et al., 2000; Lenzenweger et al., 2004; Sanislow et al., 2009; Skodol et al., 2005; Skodol, 2008). It is worth noting here that a majority of participants in the present study’s clinical sub-groups were in treatment at the time of recruitment, which was not controlled for in this study, due to its naturalistic design (cf., Sanislow et al., 2009). Whether this general trend of remission was due to treatment condition or not (some of the reduction may have been the result of the treatments that many of the participants received), what is important for the scope of the present study is that the various patterns of change in the DSM diagnosis were associated with meaningful changes in the PPTD factors scores as well, supporting the relative intrinsic plasticity of the four- PPTD structure.
However, some of the changes observed in the PPTD factor scores as a function of the change in the DSM diagnosis were not significant. For example, Introversion and Impulsivity appeared less related to change in the DSM diagnosis. It is possible that the small representation of participants in some of the groups such as the group of participants acquiring a diagnosis over time (newly diagnosed group) may have weakened the power of the analyses. On the other hand, the groups (i.e. stability, remission, and newly diagnosed) may have been too broad to capture the variety of patterns of change in the PPTD factors (especially for the domains apparently more sensitive to change, such as Impulsivity).
Consistent with this interpretation, we observed high intra-group variability among the PPTD change factors (revealing that within each group, individuals did not change at the same speed). It is possible that, by disentangling various trajectories within our “change in DSM diagnosis groups”, the results may have been clearer. For example, the pattern of changes in the PPTD factor scores may certainly be different for participant who acquired a diagnosis of substance abuse between T1 and T2, than for those who acquired a diagnosis of any affective/anxiety disorders only. In the study presented here, both trajectories were grouped into a single form of change labeled “newly diagnosed.” Future studies with larger samples should attempt to model trajectories using the specific diagnosis (e.g., major depression vs. anxiety disorder) rather than our broad quasi-syndromal diagnostic groups. However, such analyses are highly demanding in sample size and were thus not feasible in this study. Nevertheless, the proposed approach to capture the dynamic of change in PPTD as a function of the change in current DSM diagnosis, may offer a useful agenda for future research using existing longitudinal datasets with larger sample sizes.
6.3. Study Limitations and Future Directions
In addition to those already described, a number of other limitations warrant mention. Because “peculiarity” features are underrepresented in the MCMI-III and other PD inventories, we were not able to examine the fifth PPTD described in the literature (i.e., Psychoticism). As noted by Rossi and collaborators (2010) in line with the Personality Disorders Work Group, future research should include this fifth PPTD in order to represent oddity or peculiarity features (e.g., Tackett et al., 2008), that is, the negative variant of the Openness domain in the FFM. Future longitudinal research incorporating broader assessment of PD (such as the Personality Psychopathology-Five, PSY-5; Harkness, McNulty, & Ben-Porath, 1995) are of importance in order to elucidate all five domains together, their structural stability, and dynamic of change.
Although the sample was diverse, including clinical and non-clinical participants with the same high-risk background (high prevalence of ethnic minorities associated with low-income), the exclusion of participants with a history of psychosis from this study may have reduced the generalizability of the findings, with some clinical groups that are prevalent in the community being underrepresented in our analyses. Similarly, only women were recruited though gender differences in personality construct in both cross-sectional (e.g., Schmitt, Realo, Voracek, & Allik, 2008) and longitudinal studies (e.g., Klimstra, Hale, Raaijmakers, Branje, & Meeus, 2009) are often observed. For example, Jane, Oltmanns, South and Turkheimer, (2007) identified a differential item functioning in the diagnostic features of 10 personality disorder categories, suggesting that men and women with equivalent levels of pathology tend to endorse items of common PD inventories at different rates. This points out another limit of this study: its reliance on a self-report measure which usually maps only partially onto PD-related behavior (e.g., Rogers et al. 1999), although this format is commonly used to capture dimensional “trait models” of maladaptive personality (Westen & Muderrisoglu, 2006).
Finally, we must note several limitations of the various grouping strategies used in this study related to DSM diagnostic groups and change in diagnostic groups, and their derivation from categorical diagnostic systems. First, although the DIS-IV used in this study to derived DSM diagnosis is a measure that proved robust levels of inter-diagnostician reliability in several studies, this reliability indicator was not evaluated here, precluding the estimation of “interviewer effects” that may account for error in diagnosis classification. Second, clinical diagnoses stability depends at least partially on the method of assessment, and structured interviews have yielded lower stability (Samuel et al., 2011). Third, the use of thresholds often arbitrary for a categorical diagnosis (Grilo et al., 2004) are likely to lead to measurement error in diagnostic and cumulated errors in measurement of change. Together, these limitations should be considered for future studies involving larger and more diverse samples, using multiple PDs and other clinical diagnoses techniques to assess psychopathology.
7. Conclusion
This study extends prior efforts to derive an empirical structure of PPTD for inclusion in official nosologies, by providing a unique set of longitudinal evidence of four higher-order PPTD underlying PDs and other psychiatric conditions. This model does not represent the “true” structure of PDs (O’Connor, 2005), but at least represents an increasingly consistent framework to understand pathological personality trait structure and dynamic of change. As a result, we were able to achieve the first developmental analyses using these higer-order constructs of personality pathology traits, which provide an innovative understanding of PD development and dynamic of change. Ultimately, a better knowledge of this dynamic can prove useful to trigger change in the maladaptive personality component of psychopathology. To that end, we recommend extending the present research using longitudinal examination of PPTDs, particularly in an effort to explore the fifth domain of Psychoticism, and examine further relevance of a higher-order, general factor of pathological personality (cf. Philippe Rushton & Irwing, 2009). Finally, future research should focus on the developmental relation between PPTD and other domains of the psychological functioning, in an effort to better understand the mechanisms by which change in PPTD affects -- and is affected by -- other features of psychological functioning.
Acknowledgments
We would like to thank Theresa Babuscio, Gabrielle Santa-Donato, Julia Chafkin, Jeremy Rothstein and Pamela Brown for their help with data collection, data management, and editorial assistance in the preparation of this manuscript. We also thank Gina Rossi for her data-analytic advices. Preparation of this manuscript was supported by DA010726, DA11498 and DA14385 (PI: Luthar).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Publishing, Inc; 2000. [Google Scholar]
- Clark LA. Assessment and diagnosis of personality disorder: Perennial issues and an emerging reconceptualization. Annual Review of Psychology. 2007;58(1):227–257. doi: 10.1146/annurev.psych.57.102904.190200. [DOI] [PubMed] [Google Scholar]
- Cuevas L, García LF, Aluja A, García Ó. Exploratory and confirmatory factorial structure of the MCMI-III personality disorders: Overlapping versus non-overlapping scales. The European Journal of Psychiatry. 2008;22(2):59–68. [Google Scholar]
- Dascalu M, Compton W, Horton J, Cottler L. Validity of DIS-IV in diagnosing depression and other psychiatric disorders among substance users. Drug and Alchohol Dependence. 2001;63:S37. [Google Scholar]
- Durbin CE, Klein DN. Ten-year stability of personality disorders among outpatients with mood disorders. Journal of Abnormal Psychology. 2006;115(1):75–84. doi: 10.1037/0021-843X.115.1.75. [DOI] [PubMed] [Google Scholar]
- Dyce JA, O’Connor BP, Parkins SY, Janzen HL. Correlational structure of the MCMI-III personality disorder scales and comparisons with other data sets. Journal of Personality Assessment. 1997;69(3):568–582. doi: 10.1207/s15327752jpa6903_10. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, South SC, Simms LJ, Clark LA. Contrasting prototypes and dimensions in the classification of personality pathology: Evidence that dimensions, but not prototypes, are robust. Psychological Medicine. 2011;41:1151–1163. doi: 10.1017/S0033291710001650. [DOI] [PubMed] [Google Scholar]
- Ferguson CJ. A meta-analysis of normal and disordered personality across the life span. Journal of Personality and Social Psychology. 2010;98(4):659–667. doi: 10.1037/a0018770. [DOI] [PubMed] [Google Scholar]
- Ferrer E, McArdle JJ. Longitudinal modeling of developmental changes in psychological research. Current Directions in Psychological Science. 2010;19(3):149–154. doi: 10.1177/0963721410370300. [DOI] [Google Scholar]
- Grilo CM, Shea MT, Sanislow CA, Skodol AE, Gunderson JG, Stout RL, McGlashan TH. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology. 2004;72(5):767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo C, Stout R, Markowitz J, Sanislow C, Ansell E, Skodol A, McGlashan T. Personality disorders predict relapse after remission from an episode of major depressive disorder: A 6-year prospective study. The Journal of Clinical Psychiatry. 2010;71(12):1629–1635. doi: 10.4088/JCP.08m04200gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness AR, McNulty JL, Ben-Porath YS. The personality psychopathology five (PSY-5): Constructs and MMPI-2 scales. Psychological Assessment. 1995;7(1):104–114. doi: 10.1037/1040-3590.7.1.104. [DOI] [Google Scholar]
- Hasin DS, Grant BF. Psychiatric diagnosis of patients with substance abuse problems: A comparison of two procedures, the DIS and the SADS-L: Alcoholism, drug abuse/dependence, anxiety disorders and antisocial personality disorder. Journal of Psychiatric Research. 1987;21(1):7–22. doi: 10.1016/0022-3956(87)90005-7. [DOI] [PubMed] [Google Scholar]
- Hesse M, Guldager S, Holm Linneberg I. Convergent validity of MCMI-III clinical syndrome scales. British Journal of Clinical Psychology. 2012;51(2):172–184. doi: 10.1111/j.2044-8260.2011.02019.x. [DOI] [PubMed] [Google Scholar]
- Hicks B, Markon K, Patrick C, Krueger R, Newman J. Identifying psychopathy subtypes on the basis of personality structure. Psychological Assessment. 2004;16(3):276–288. doi: 10.1037/1040-3590.16.3.276. [DOI] [PubMed] [Google Scholar]
- Jahng S, Trull TJ, Wood PK, Tragesser SL, Tomko R, Grant JD, Sher KJ. Distinguishing general and specific personality disorder features and implications for substance dependence comorbidity. Journal of Abnormal Psychology. 2011;120(3):656–669. doi: 10.1037/a0023539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jane JS, Oltmanns TF, South SC, Turkheimer E. Gender bias in diagnostic criteria for personality disorders: An item response theory analysis. Journal of Abnormal Psychology. 2007;116(1):166–175. doi: 10.1037/0021-843X.116.1.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102(4):265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Klimstra TA, Hale WW, Raaijmakers QA, Branje SJ, Meeus WH. Maturation of personality in adolescence. Journal of Personality and Social Psychology. 2009;96(4):898–912. doi: 10.1037/a0014746. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3. New York, NY: The Guilford Press; 2010. [Google Scholar]
- Krueger RF, Skodol AE, Livesley WJ, Shrout PE, Huang Y. Synthesizing dimensional and categorical approaches to personality disorders: Refining the research agenda for DSM-V axis II. International Journal of Methods in Psychiatric Research. 2007;16(1):65–73. doi: 10.1002/mpr.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR, Clark LA, Watson D, Markon KE, Derringer J, Livesley WJ. Deriving an empirical structure of personality pathology for DSM-5. Journal of Personality Disorders. 2011;25(2):170–191. doi: 10.1521/pedi.2011.25.2.170. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Tackett JL. Progress and innovation: Personality disorders and the vanguard of psychopathology research. Journal of Personality Disorders. 2005;19(5):540–546. doi: 10.1521/pedi.2005.19.5.540. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Stability and change in personality disorder features: The longitudinal study of personality disorders. Archives of General Psychiatry. 1999;56(11):1009–1015. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. The longitudinal study of personality disorders: History, design considerations, and initial findings. Journal of Personality Disorders. 2006;20(6):645–670. doi: 10.1521/pedi.2006.20.6.645. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Current status of the scientific study of the personality disorders: An overview of epidemiological, longitudinal, experimental psychopathology, and neurobehavioral perspectives. Journal of the American Psychoanalytic Association. 2010;58(4):741–778. doi: 10.1177/0003065110386111. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Johnson MD, Willett JB. Individual growth curve analysis illuminates stability and change in personality disorder features: The longitudinal study of personality disorders. Archives of General Psychiatry. 2004;61(10):1015–1024. doi: 10.1001/archpsyc.61.10.1015. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Willett JB. Predicting individual change in personality disorder features by simultaneous individual change in personality dimensions linked to neurobehavioral systems: The longitudinal study of personality disorders. Journal of Abnormal Psychology. 2007;116(4):684–700. doi: 10.1037/0021-843X.116.4.684. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. A framework for integrating dimensional and categorical classifications of personality disorder. Journal of Personality Disorders. 2007;21(2):199–224. doi: 10.1521/pedi.2007.21.2.199. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Sexton CC. Maternal drug abuse versus maternal depression: Vulnerability and resilience among school-age and adolescent offspring. Development and Psychopathology. 2007;19(1):205–225. doi: 10.1017/S0954579407070113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR. Assessment of maladaptive variants of five factor model traits. Journal of Personality. doi: 10.1111/j.1467-6494.2012.00775.x. in press. [DOI] [PubMed] [Google Scholar]
- Malgady RG, Rogler LH, Tryon WW. Issues of validity in the diagnostic interview schedule. Journal of Psychiatric Research. 1992;26(1):59–67. doi: 10.1016/0022-3956(92)90016-H. [DOI] [PubMed] [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88(1):139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle J, Nesselroade JR. Using multivariate data to structure developmental change. In: Cohen S, Reese H, editors. Life-span developmental psychology: Methodological contributions. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1994. pp. 223–267. [Google Scholar]
- McArdle J. Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology. 2009;60(1):577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- Millon T. Millon clinical multiaxial inventory. Minneapolis, MN: National Computer Systems; 1983. [Google Scholar]
- Millon T, Millon C, Davis R, Grossman S. Millon clinical multiaxial inventory-III manual. 3. Minneapolis, MN: Pearson Assessments; 2006. [Google Scholar]
- Mullins-Sweatt SN, Widiger TA. Millon’s dimensional model of personality disorders: A comparative study. Journal of Personality Disorders. 2007;21(1):42–57. doi: 10.1521/pedi.2007.21.1.42. [DOI] [PubMed] [Google Scholar]
- Nestadt G, Di C, Samuels JF, Bienvenu OJ, Reti IM, Costa P, Bandeen-Roche K. The stability of DSM personality disorders over twelve to eighteen years. Journal of Psychiatric Research. 2010;44(1):1–7. doi: 10.1016/j.jpsychires.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor BP, Dyce JA. A test of models of personality disorder configuration. Journal of Abnormal Psychology. 1998;107(1):3–16. doi: 10.1037/0021-843X.107.1.3. [DOI] [PubMed] [Google Scholar]
- O’Connor BP. A search for consensus on the dimensional structure of personality disorders. Journal of Clinical Psychology. 2005;61(3):323–345. doi: 10.1002/jclp.20017. [DOI] [PubMed] [Google Scholar]
- Philippe Rushton J, Irwing P. A general factor of personality in the millon clinical multiaxial inventory-III, the dimensional assessment of personality pathology, and the personality assessment inventory. Journal of Research in Personality. 2009;43(6):1091–1095. [Google Scholar]
- Robins L, Cottler L, Bucholz K, Compton W, North C, Rourke K. Diagnostic interview schedule for DSM-IV (DIS-IV) St. Louis, MO: Washington University; 2000. [Google Scholar]
- Rogers R, Salekin RT, Sewell KW. Validation of the millon clinical multiaxial inventory for axis II disorders: Does it meet the daubert standard? Law and Human Behavior. 1999;23(4):425–443. doi: 10.1023/A:1022360031491. [DOI] [PubMed] [Google Scholar]
- Rossi G, Elklit A, Simonsen E. Empirical evidence for a four factor framework of personality disorder organization: Multigroup confirmatory factor analysis of the millon clinical multiaxial inventory-III personality disorder scales across belgian and danish data samples. Journal of Personality Disorders. 2010;24(1):128–150. doi: 10.1521/pedi.2010.24.1.128. [DOI] [PubMed] [Google Scholar]
- Rossi G, van der Ark L Andries, Sloore H. Factor analysis of the dutch-language version of the MCMI-III. Journal of Personality Assessment. 2007;88(2):144–157. doi: 10.1080/00223890701267977. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Gore WL. Maladaptive variants of conscientiousness and agreeableness. Journal of Personality. doi: 10.1111/j.1467-6494.2012.00770.x. in press. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review. 2008;28(8):1326–1342. doi: 10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel DB, Hopwood CJ, Ansell EB, Morey LC, Sanislow CA, Markowitz JC, Grilo CM. Comparing the temporal stability of self-report and interview assessed personality disorder. Journal of Abnormal Psychology. 2011;120(3):670–680. doi: 10.1037/a0022647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanislow CA, Little TD, Ansell EB, Grilo CM, Daversa M, Markowitz JC, McGlashan TH. Ten-year stability and latent structure of the DSM-IV schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Journal of Abnormal Psychology. 2009;118(3):507–519. doi: 10.1037/a0016478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt DP, Realo A, Voracek M, Allik J. Why can’t a man be more like a woman? sex differences in big five personality traits across 55 cultures. Journal of Personality and Social Psychology. 2008;94(1):168–182. doi: 10.1037/0022-3514.94.1.168. [DOI] [PubMed] [Google Scholar]
- Sheets E, Craighead WE. Toward an empirically based classification of personality pathology. Clinical Psychology: Science and Practice. 2007;14(2):77–93. doi: 10.1111/j.1468-2850.2007.00065.x. [DOI] [Google Scholar]
- Skodol AE. Longitudinal course and outcome of personality disorders. Psychiatric Clinics of North America. 2008;31(3):495–503. doi: 10.1016/j.psc.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, Stout RL. The collaborative longitudinal personality disorders study (CLPS): Overview and implications. Journal of Personality Disorders. 2005;19(5):487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon SR, Sawilowsky SS. Impact of rank-based normalizing transformations on the accuracy of test scores. Journal of Modern Applied Statistical Methods. 2009;9(2):448–462. [Google Scholar]
- Tackett JL, Silberschmidt AL, Krueger RF, Sponheim SR. A dimensional model of personality disorder: Incorporating DSM cluster A characteristics. Journal of Abnormal Psychology. 2008;117(2):454–459. doi: 10.1037/0021-843X.117.2.454. [DOI] [PubMed] [Google Scholar]
- Warner MB, Morey LC, Finch JF, Gunderson JG, Skodol AE, Sanislow CA, Grilo CM. The longitudinal relationship of personality traits and disorders. Journal of Abnormal Psychology. 2004;113(2):217–227. doi: 10.1037/0021-843X.113.2.217. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Chmielewski M. Structures of personality and their relevance to psychopathology: II. further articulation of a comprehensive unified trait structure. Journal of Personality. 2008;76(6):1545–1586. doi: 10.1111/j.1467-6494.2008.00531.x. [DOI] [PubMed] [Google Scholar]
- Westen D, Muderrisoglu S. Clinical assessment of pathological personality traits. American Journal of Psychiatry. 2006;163(7):1285–1287. doi: 10.1176/ajp.2006.163.7.1285. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Costa PT., Jr Integrating normal and abnormal personality structure: The five factor model. Journal of Personality. doi: 10.1111/j.1467-6494.2012.00776.x. In press. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the diagnostic and statistical manual of mental disorders-V. Journal of Abnormal Psychology. 2005;114(4):494–504. doi: 10.1037/0021-843X.114.4.494. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Simonsen E. Alternative dimensional models of personality disorder: Finding a common ground. Journal of Personality Disorders. 2005;19(2):110–130. doi: 10.1521/pedi.19.2.110.62628. [DOI] [PubMed] [Google Scholar]
- Wright AGC. Qualitative and quantitative distinctions in personality disorder. Journal of Personality Assessment. 2011;93(4):370–379. doi: 10.1080/00223891.2011.577477. [DOI] [PMC free article] [PubMed] [Google Scholar]