Abstract
We report an unusual case of an invasive thymoma with a thrombus in the right atrium and describe the radiological findings consistent with the malignant nature of the thrombus. The thrombus showed significant enhancement on computerized tomography images similar to the tumoral mass. On magnetic resonance imaging, both the tumor and the thrombus have heterogeneously high signal intensities on T2-weighted images. On diffusion-weighted images they both exhibit high signal intensity and low apparent diffusion coefficient (ADC) values which support the malignant nature of the thrombus and the mass.
Keywords: invasive thymoma, tumor thrombus, intravascular growth
CASE REPORT
A 53-year-old woman was referred to our hospital for severe dyspnea and facial oedema. Computerized tomography was performed with a 64-detector scanner (Aquillion 64; Toshiba Medical Systems, Tokyo, Japan), before and after the intravenous administration of iodinated contrast material. On the non-contrast-enhanced CT (NCCT) images there was an ill-defined heterogeneous anterior mediastinal mass with rim calcification adjacent to the ascending aorta (Fig. 1). There was no definite invasion to thoracic aorta. There were streaky hyperdense infiltrations into the anterior mediastinal fat around the mass lesion. Both the left brachiocephalic vein (LBCV) and the SVC were enlarged. On the contrast enhanced CT (CCT) images the mass was heterogeneously enhancing and there was an intraluminal thrombus causing a luminal filling defect extending from the LBCV and the SVC to the right atrium (RA). There was no mediastinal lymphadenopathy. Enhancement of mass and thrombus were measured on NCCT, and on CCT at 25 seconds (early arterial phase) and 70 seconds (late phase). All Hounsfield unit (HU) measurements were performed on mediastinal images using a circular region of interest (ROI) placed over the mass and the thrombus filling the atrial cavity, avoiding apparently necrotic parts. The HU values obtained from the mass were 41, 76 and 86; on NCCT, early phase and late phase CCT images, respectively (Fig. 2). The corresponding HU values measured from the thrombus were 36, 66 and 69 (Fig. 3). Using the criterion of an increase greater than 15 HU from NCCT to CCT images, both the primary mass and the thrombus enhanced significantly and similarly.
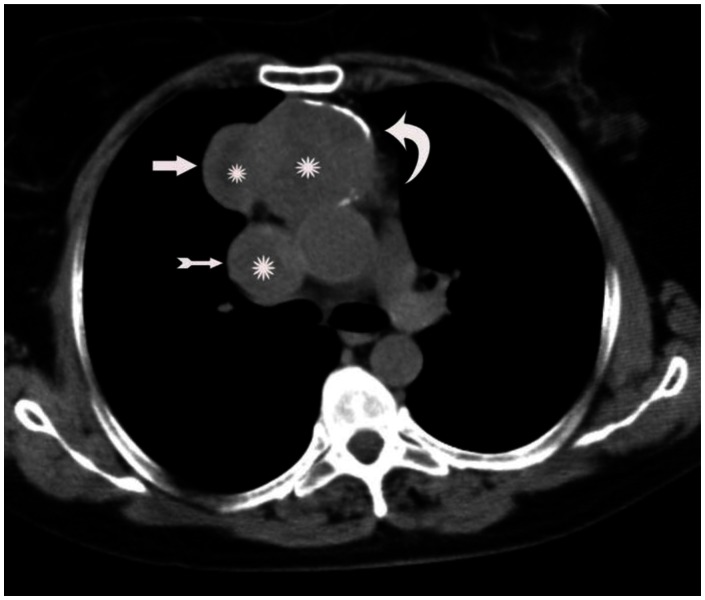
Figure 1.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. Axial plane non-contrast-enhanced CT shows anterior mediastinal mass with lobulated contours (thick arrow) and rim calcification (curved arrow). Note the enlarged superior vena cava (thin arrow). The mass and the thrombus are heterogeneous and central parts are more hypodense consistent with necrosis (stars).(Protocol: 64 detector scanner, 180 mAs, 120 kV, slice thickness: 5 mm.)
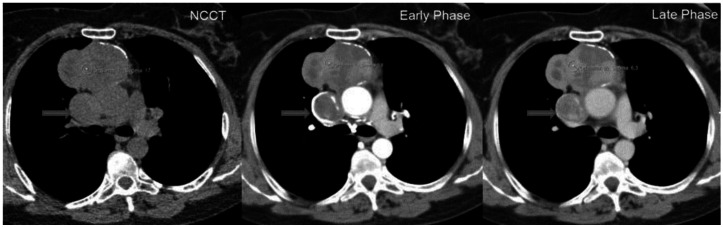
Figure 2.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. HU densities measured on the mass lesion are, 41 on non-contrast-enhanced CT (NCCT) image, 76 on contrast-enhanced CT images in the arterial phase, and 86 on contrast-enhanced CT images in the 70 seconds delayed phase. HU densities are compatible with significant enhancement of the mass. Note all ROIs are placed on non-necrotic solid parts of the mass.(Arrow: SVC) (Protocol: 64 detector scanner, 180 mAs, 120 kV, slice thickness: 5 mm, Contrast material: 60 ml Iohexol.) (Early phase images acquired 25 seconds after contrast administration and late phase images acquired 70 seconds after contrast administration.)
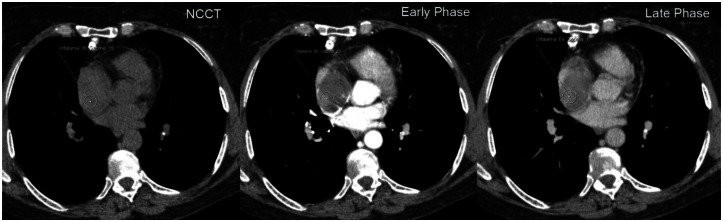
Figure 3.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. HU densities measured on the right atrial thrombus are, 36 on non-contrast-enhanced CT image, 66 on contrast-enhanced CT images in the arterial phase, and 69 on contrast-enhanced CT images in the four minutes delayed phase. HU densities are similar with the primary mass and compatible with significant enhancement. Note all ROIs are placed on eccentric non-necrotic part of the thrombus. (Protocol: 64 detector scanner, 180 mAs, 120 kV, slice thickness: 5 mm, Contrast material: 60 ml Iohexol.) ( Early phase images acquired 25 seconds after contrast administration and late phase images acquired 70 seconds after contrast administration.)
Subsequently, the patient was examined using a 3 Tesla magnetic resonance imaging (MRI) unit (Philips Achieva Intera Release, Eindhoven, The Netherlands), with a four-element phased-array body coil using a partially parallel imaging acquisition and SENSE. The patient underwent a routine MRI session for the thorax that included: axial T1-weighted (W) breath-hold turbo field echo, axial T2-W single-shot turbo spin echo and axial single-shot spin-echo echo-planar diffusion-weighted (DW) imaging using the b values 0 and 1.000 s/mm. ADC maps were reconstructed. The mass and the thrombus were heterogeneously hypointense on T1-W and hyperintense on T2-W images. There were cystic changes on T2-W images in both the mass and the thrombus (Fig. 4). On DW images, both the mass and the thrombus had high signal intensities (SIs) (nearly equal comparing with that of the spinal cord on the same image) (Fig. 5). The ADC values of the mass and the thrombus were found to be 1.15 ×10-3 mm2/s and 0.98 ×10-3 mm2/s, respectively. The ADC values were 1.15 ×10-3 mm2/s for the mass and 0.98 ×10-3 mm2/s for the thrombus (Fig. 6).
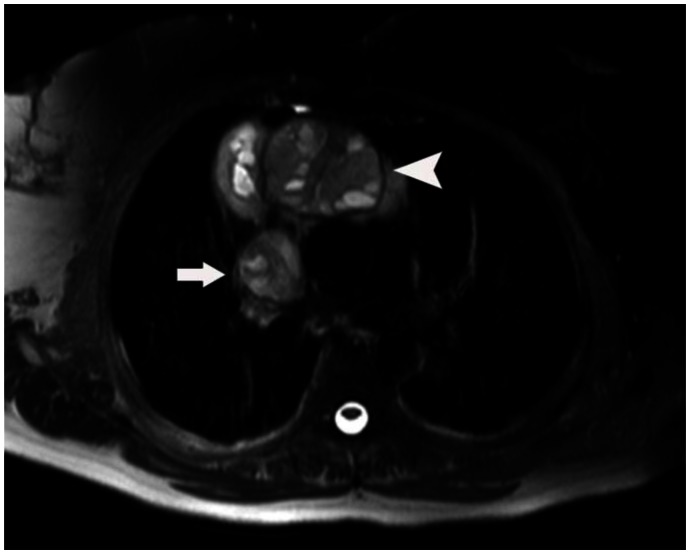
Figure 4.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. Axial T-2 weighted MR image shows heterogeneous-cystic content of the mass (arrow head). The thrombus in the superior vena cava lumen has the same cystic components like the mass (arrow).(Protocol: 3 Tesla MRI, TR:1372, TE:80)
Figure 5.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. The mass lesion (arrow head) and the thrombus in the superior vena cava (arrow) demonstrates high signal intensities on axial DW image for b = 1.000 s/mm2, compatible with restricted diffusion. (Protocol: 3 Tesla MRI, TR:1763, TE:69)
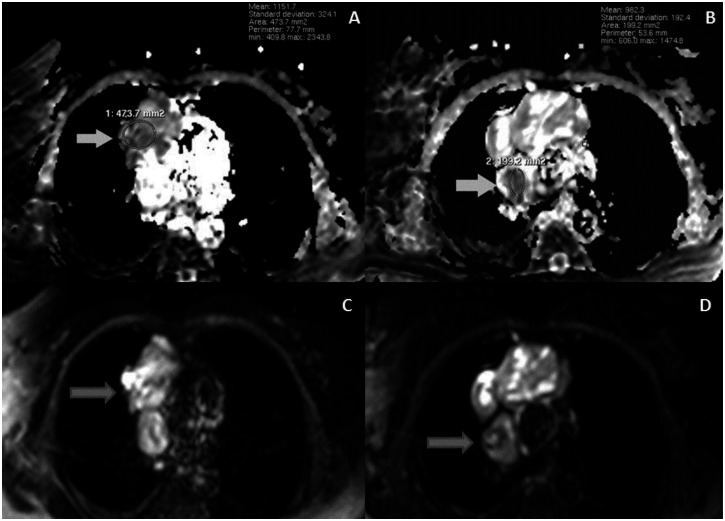
Figure 6.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. ADC maps (A, B) and DWI (C, D) of the mass and the thrombus at same level. The mass (A, arrow) and the thrombus (B, arrow) show significant low intensities on ADC maps with low ADC values, compatible with the malignant character. (Protocol: 3 Tesla MRI, TR:1763, TE:69)
Pathological examination revealed that the mass and the intraluminal tumoral thrombus were type B3 thymoma (WHO classification).
DISCUSSION
Invasive thymoma is typically an anterior mediastinal mass which is radiologically characterized by its ill-defined borders and infiltrative growth into the neighbouring structures, as we observed in our case. It usually grows along the mediastinal fat planes and pleural surfaces. Next, invasion to trachea, pericardium, heart and great vessels can occur, at which time most patients become symptomatic (1). The differential diagnosis for an invasive anterior mediastinal mass includes invasive thymoma, thymic carcinoma, lymphoma, metastasis, malignant germ cell tumors and primary sarcomatous tumors. Thymic carcinomas are more commonly associated with lymphadenopathy than invasive thymomas. Hodgkin’s and non-Hodgkin’s lymphomas commonly involve the thymus. But isolated thymic involvement is much rarer than combined thymic and mediastinal nodal disease. Malignant germ cell tumors have CT and MR features similar to other malignant anterior mediastinal tumors. They can be differentiated with relatively young patient age and laboratory findings like elevated beta human chorionic gonadotropin, alpha-fetoprotein, and lactate-dehydrogenase levels. Sarcomas like angiosarcomas, fibrosarcomas, osteosarcomas, and chondrosarcomas, are also very uncommon.
They show non-specific appearance, but some dense areas of calcification or ossification are in favor of the latter. CT features generally cannot help to distinguish them from invasive thymomas (2).
The most appropriate treatment for invasive thymoma is complete resection (3,4).
Invasive thymoma commonly causes superior vena cava (SVC) syndrome by extrinsic encasement and compression of the SVC, but rarely by intraluminal growth (3). Although a tendency to infiltrate is to be expected to from invasive thymoma, intravascular growth is rather rare. Tumoral cells are thought to invade the venous vascular system through the thymic veins and malignant tumoral thrombus grows into the LBCV, SVC and then the RA (4). It is important to diagnose malignant vascular invasion during the preoperative assessment because the operation team in this case needs to include vascular surgeons, especially when there is RA involvement. The capacity for CT and MRI to show vascular invasion is well established, but it is sometimes difficult to use these modalities to consistently differentiate between malignant and bland thrombus.
There are reports on radiological differentiation between malignant and benign thrombi, especially in liver and kidney tumors. The presence of enhancement on CT was found to be a strong proof of malignant portal vein thrombus by Tublin et al. (5) although they did not measure the enhancement quantitatively. Shah et al. (6) stated that the intensity ratio of enhanced to non-enhanced CT images is valuable and an enhancing portal vein thrombus is suggestive of hepatocellular cell carcinoma. In our case, quantitative enhancement of the thrombus was found significantly high (>15 HU). The thrombus had almost the same HU density as the primary tumor on CCT images, which is also a valuable clue for diagnosing malignant thrombus. The amount of change in HU values from early to late phases (<15 HU) were also similar.
MRI was found to be helpful for characterizing thrombus composition because of the superior soft tissue contrast resolution. Because of the T2 shortening effect of blood breakdown products, bland thrombi are low in SI compared with tumoral thrombi, which are of intermediate SI (7). Enhancement can be also useful but it is usually LESS conspicuous and not as easy to evaluate on MRI compared to CT imaging (7). In our case, the thrombus had the same heterogeneously hyperintense appearance as the anterior mediastinal mass on T2-W images. We did not use contrast enhanced images because of difficulties in interpretation.
In the reports about malignant and benign differentiation of mediastinal masses using DWI, malignant mass lesions were found to have significant low ADC values (8–9). Catalano et al. (10) stated that SIs and ADC values of portal vein tumoral thrombi are similar to those of the primary masses in cases of hepatocellular carcinoma. They found that an ADC value < 2 ×10-3 mm2/s was likely to indicate a malignant thrombus. There are no reported cases about DWI characteristics of intraluminal malignant thrombi in the chest. In our case, we demonstrated that the thrombus and the coexisting thymoma had the same high SI compared to the spinal cord on the same image, suggesting that the thrombus was malignant. Evaluating signal intensity on DWI is a relatively subjective finding. Uto et al (11) reported that lesion to spinal cord ratio for lung cancer was significantly higher than that for benign lesions. Based on this finding we compared the DWI signal intensities of the tumor and thrombus with the spinal cord in order to get more reliable results. The ADC of the atrial thrombus (0.98 ×10-3 mm2/s) was similar to the ADC value of the coexisting thymoma (1.15 ×10-3 mm2/s) and both measurements were quite low, highly suggestive of a malignancy according to previously reported threshold ADC values (8–10).
Our findings suggest that the quantitative assessment of contrast enhancement on CT and DW imaging features on MRI may be helpful to arise suspicion of a malignant thrombus, when accompanied by a mediastinal mass such as an invasive thymoma.
TEACHING POINT
Coexisting intravascular thrombus may be problematic in malignant masses and differentiation of malignant from bland thrombus is crucial. Radiological differentiation can be achieved when thrombus has the matching quantitative enhancement values on enhanced computed tomography, the similar hyperintense appeareance in T2 weighted magnetic resonance imaging and similar ADC values as the original mass.
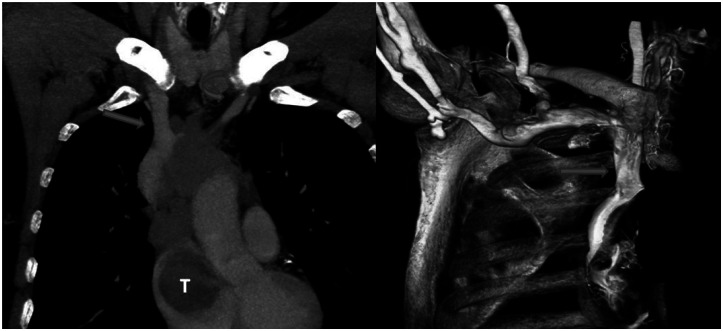
Figure 7.
A 53-year-old woman with invasive thymoma with extensive intraluminal tumor thrombus. CT angiography (A) and 3D reconstructed CT image of a CT angiography (B) show the thrombus and filling defects of SVC (straight arrow) and LBCV (curved arrow). CT angiography (A) also demonstrates the right atrial thrombus (T). (Protocol: 64 detector scanner, 180 mAs, 120 kV, Contrast material: 60 ml Iohexol.)
Table 1.
HU density measurements and ADC values of primary mass and the thrombus.
| Lesion | Hounsfield Unit density of… | ADC Values (x10−3 mm2/s) | ||
|---|---|---|---|---|
| NCCT | Early Phase CCT | Late Phase CCT | ||
| Thymoma | 41 | 76 | 86 | 1.15 |
| Thrombus | 36 | 66 | 69 | 0.98 |
Note: NCCT = non-contrast-enhanced CT, CCT = contrast-enhanced CT, HU = Hounsfield Unit.
Table 2.
Summary table for invasive thymoma with intravascular growth.
| Etiology | Tumoral cells are thought to invade venous vascular system through the thymic veins and malignant tumoral thrombus grows into the LBSV, SVC and then the RA |
| Incidence | Invasive thymomas usually infiltrate adjacent organs in the mediastinal pleura, including the lungs, pericardium, great vessels, and heart, and extrathoracic metastases are very uncommon, occurring in only about 5% of cases |
| Gender ratio | There is no gender ratio for intravascular growth of invasive thymoma |
| Age predilection | There is no age predilection for intravascular growth of invasive thymoma |
| Risc factors | Rics factors for intravascular growth of invasive thymoma is unknown. |
| Treatment | The optimal treatment for invasive thymomas is complete resection, and therefore vascular wall reconstruction is necessary in invasive cases. |
| Prognosis | excellent long-term survival after extended resections for thymoma |
| Imaging findings | Ill-defined borders and infiltrative growth into the neighbouring structures. Significant low ADC values on MRI. |
Table 3.
Differential table for imaging of benign and malignant thrombus.
| CT | MRI | |
|---|---|---|
| Benign thrombus | There is no enhancement on contrast enhanced CT. | Lower signal intensity on T2W MRI compared to malignant thrombus. There are no significant lower ADC values. |
| Malignant thrombus | The presence of enhancement is a strong proof of malignant thrombus. | Higher signal intensity on T2W MRI compared to benign thrombus. Similar signal intensity and ADC values to those of the primary mass. Lower ADC values similar to the primary mass. |
ABBREVIATIONS
- ADC
Apparent diffusion coefficient
- CCT
Contrast enhanced CT
- DW
Diffusion-weighted
- HU
Hounsfield unit
- LBCV
Left brachiocephalic vein
- MRI
Magnetic resonance imaging
- NCCT
Non-contrast-enhanced CT
- RA
Right atrium
- ROI
Region of interest
- SIs
Signal intensities
- SVC
Superior vena cava
- W
Weighted
REFERENCES
- 1.Nomori H, Horio H, Morinaga S, Suemasu K. Minimally invasive thymoma with extensive intravascular growth. Jpn J Clin Oncol. 1999;29(12):630–632. doi: 10.1093/jjco/29.12.630. [DOI] [PubMed] [Google Scholar]
- 2.Laurent F, Latrabe V, Lecesne R, Zennaro H, Airaud JY, Rauturier JF, Drouillard J. Mediastinal masses: diagnostic approach. Eur Radiol. 1998;8(7):1148–59. doi: 10.1007/s003300050525. [DOI] [PubMed] [Google Scholar]
- 3.Motoori K, Shimura H, Funabashi N, Takiguchi Y, Imamaki Y, Ito H. Thymoma presenting as an intraluminal growth into the superior vena cava and the cardiac cavity. European Journal of Radiology Extra. 2008;68:13–15. [Google Scholar]
- 4.Terada Y, Ono N, Noguchi T, Kamaraki K, Kitano M. A case of thymoma protruding into the superior vena cava through the thymic vein. Ann Thorac Surg. 2004;77:1088–1090. doi: 10.1016/S0003-4975(03)01172-X. [DOI] [PubMed] [Google Scholar]
- 5.Tublin ME, Dodd GD, Baron RL. Benign and malignant portal vein thrombosis: differentiation by CT characteristics. Am J Roentgenol. 1997;168:719–723. doi: 10.2214/ajr.168.3.9057522. [DOI] [PubMed] [Google Scholar]
- 6.Shah ZK, McKernan MG, Hahn PF, Sahani D. Enhancing and expansile portal vein thrombosis: value in the diagnosis of hepatocellular carcinoma in patients with multiple hepatic lesions. Am J Roentgenol. 2007;188:1320–1323. doi: 10.2214/AJR.06.0134. [DOI] [PubMed] [Google Scholar]
- 7.Engelbrecht M, Akin O, Dixit D, Schwartz L. Bland and tumor thrombi in abdominal malignancies: magnetic resonance imaging assessment in a large oncologic patient population. Abdom Imaging. 2011;36:62–68. doi: 10.1007/s00261-010-9608-6. [DOI] [PubMed] [Google Scholar]
- 8.Gumustas S, Inan N, Sarisoy HT, An?k Y, Arslan A, Çiftçi E. Malignant versus benign mediastinal lesions: quantitative assessment with diffusion weighted MR imaging. Eur Radiol. 2011;21:2255–2260. doi: 10.1007/s00330-011-2180-9. [DOI] [PubMed] [Google Scholar]
- 9.Abdel Razek A, Elmorsy A, Elshafey M, Elhadedy T, Hamza O. Assessment of mediastinal tumors with diffusion- weighted single-shot echo-planar MRI. J Magn Reson Imaging. 2009;30:535–540. doi: 10.1002/jmri.21871. [DOI] [PubMed] [Google Scholar]
- 10.Catalano O, Choy G, Zhu A, et al. Differentiation of malignant thrombus from bland thrombus of the portal vein in patients with hepatocellular carcinoma: application of diffusion-weighted MR Imaging. Radiology. 2010;254:154–162. doi: 10.1148/radiol.09090304. [DOI] [PubMed] [Google Scholar]
- 11.Uto T, Takehara Y, Nakamura Y, Naito T, Hashimoto D, Inui N, Suda T, Nakamura H, Chida K. Higher sensitivity and specificity for diffusion-weighted imaging of malignant lung lesions without apparent diffusion coefficient quantification. Radiology. 2009 Jul;252(1):247–54. doi: 10.1148/radiol.2521081195. Epub 2009 May 6. [DOI] [PubMed] [Google Scholar]