Abstract
While the clinical findings of cocaine-induced enteropathy from mesenteric ischemia are fairly well understood, there is a paucity of imaging description and detail in the literature that describes these findings. Imaging characteristics of cocaine-induced mesenteric ischemia on CT examination include bowel edema, mucosal enhancement, venous engorgement, mesenteric free fluid, and dilatation of the small bowel lumen. A thorough history, physical examination, and laboratory testing are critical for the diagnosis and prompt surgical intervention may be necessary. We present a case of cocaine-induced mesenteric ischemia in a 49 year old male which resolved within 24 hours of supportive therapy.
Keywords: Cocaine Enteritis, Cocaine Enteropathy, Enteritis, Enteropathy, Mesenteric Ischemia
CASE REPORT
A 49-year-old African American male presented to our hospital with complaints of a 2-day history of sharp constant lower quadrant abdominal pain. The patient had associated green bowel movements without diarrhea, nausea, or fever. The patient had experienced a previous similar episode one year previously. The patient’s history was negative for possible predisposing causes of diffuse abdominal pain such as exposure to infection, prior surgery, or atherosclerosis. The patient initially denied illicit drug use. The initial vital signs were unremarkable. A physical examination was performed and revealed diffuse abdominal pain with mild focal tenderness to palpitation in the lower quadrants. Laboratory analysis revealed a normal serum lactate of 0.8 mmol/L. The patient’s urine drug screen was positive for cocaine and marijuana. Upon further questioning, the patient admitted to smoking crack cocaine prior to the episode of abdominal pain. Additional history revealed a similar episode of abdominal pain one-year prior, which was also similarly preceded by cocaine use.
A CT examination with intravenous contrast was performed through the ED for the patient’s diffuse abdominal pain and revealed extensive wall thickening throughout the mid and distal small bowel in long contiguous segments with mucosal enhancement (Figures 1 and 2). Additional findings included mesenteric vascular congestion and free fluid in the perihepatic space. The cecum demonstrated minimal wall edema, while the remainder of the colon was relatively unaffected (Figures 1, 2). The remaining abdominal and pelvic viscera were normal in appearance. There was no fatty infiltration of the bowel wall, skip lesions, mesenteric adenopathy, or “creeping fat” to suggest an inflammatory bowel process such as Crohn’s disease. Imaging demonstrated patent vessels without mesenteric atherosclerotic calcification. The patient was admitted to the medicine team for observation and conservative treatment. The gastroenterology team was consulted for evaluation of the patient’s symptoms and recommended a dedicated CT enterogram and supportive care.
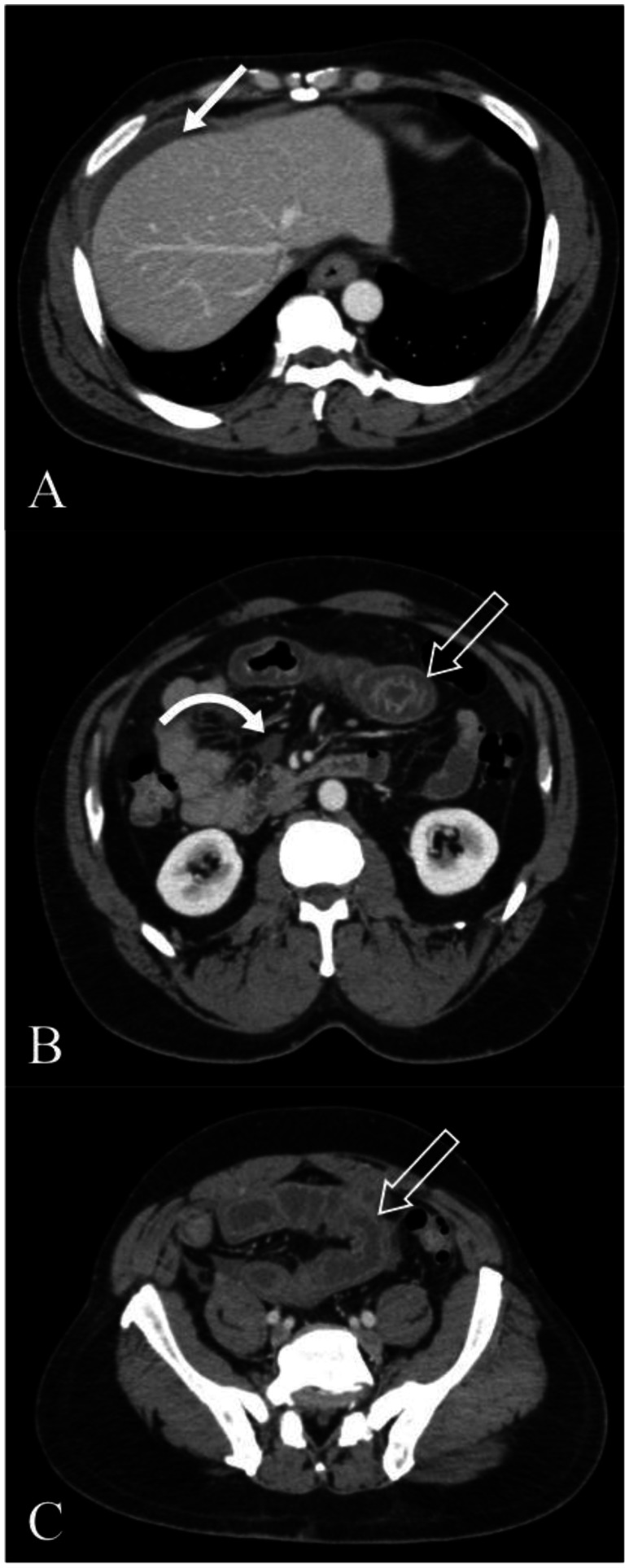
Figure 1.
Axial CT Images (Toshiba Aquilion 32 slice, 106 mAs, 120 kVp, 3 mm axial slices, 120 cc of Optiray 350 contrast in portal venous phase) of a 49-year-old male with cocaine-induced mesenteric ischemia at the time of initial presentation. Images demonstrate perihepatic free fluid (1a closed arrow), mild distention and wall thickening of the small bowel (1b and 1c open arrow), mucosal enhancement and trace adjacent fluid (1b curved arrow). The thickened long segments of small bowel have low attenuation of the bowel wall. No atherosclerotic calcification is seen within the aorta or mesenteric vessels. With exception to minimal edema in the cecum, the colon was relatively unaffected.
Figure 2.
A 49-year-old male with cocaine-induced mesenteric ischemia. Initial coronal reformat CT images with intravenous contrast at the time of presentation (Toshiba Aquilion 32 slice, 106 mAs, 120 kVp, 5 mm coronal reformats, 120 cc of Optiray 350 contrast in portal venous phase). Images demonstrate perihepatic fluid (closed arrow), mild distention and wall thickening of the small bowel (open straight arrow), and vascular engorgement (open curved arrow).
After 24 hours, repeat CT imaging was performed with intravenous and oral contrast. The examination was performed with a positive oral contrast agent (presumably due to clerical error as we use negative contrast such as VoLumen for CT enterography at our institution). The CT images at 24 hours demonstrated complete resolution of the free fluid and abnormal small bowel findings (Figures 3 and 4). No significant imaging abnormalities were noted and a diagnosis of cocaine-induced mesenteric ischemia was made. The patient was discharged home in good condition and was counseled to discontinue his cocaine use.
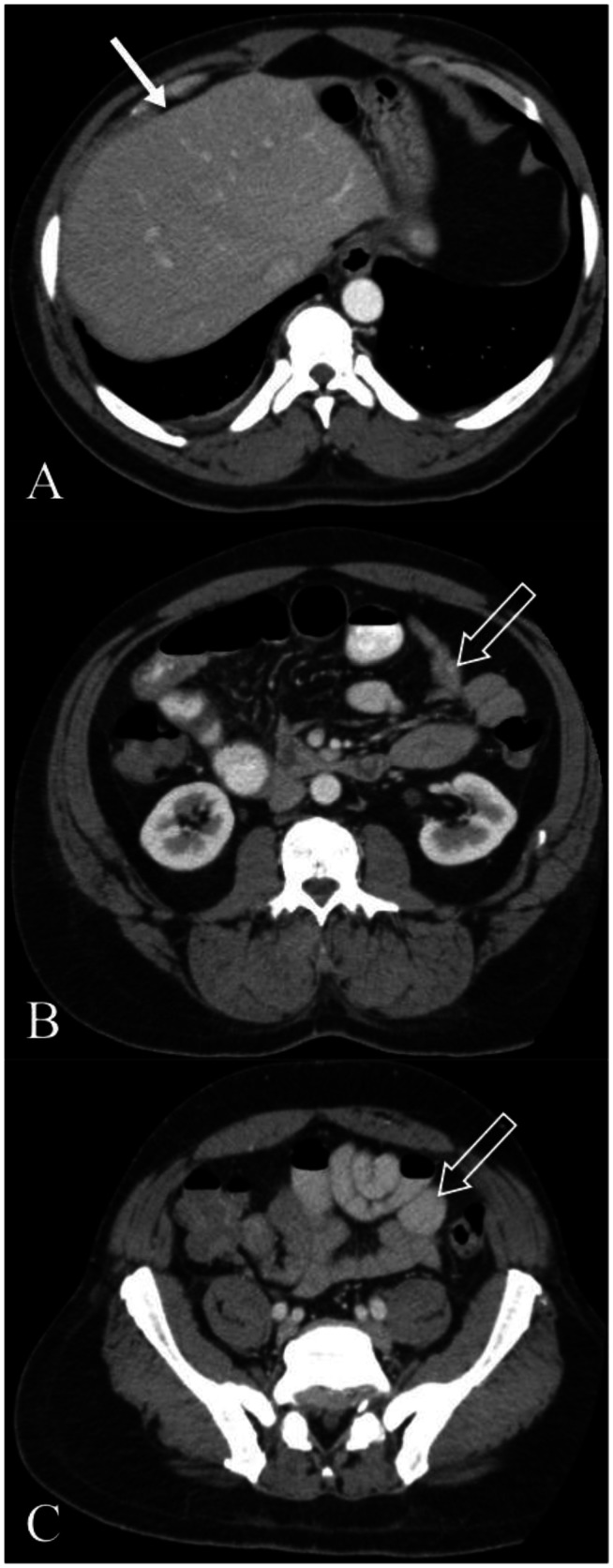
Figure 3.
A 49-year-old male with resolved cocaine-induced mesenteric ischemia. Axial CT images (Toshiba Aquilion 32 slice, 121 mAs, 120 kVp, 3 mm axial slices, 120 cc of Optiray 350 contrast in portal venous phase, 900 cc of Readi-CAT given 2 hours prior to image acquisition) with intravenous and positive oral contrast 24 hours after initial presentation. Images demonstrate normal appearance of small bowel (3b and 3c open straight arrow) and resolution of the perihepatic free fluid (3a closed straight arrow). No abnormal findings were noted.
Figure 4.
A 49-year-old male with resolved cocaine-induced mesenteric ischemia. Coronal reformat (Toshiba Aquilion 32 slice, 121 mAs, 120 kVp, 5 mm coronal reformats, 120 cc of Optiray 350 contrast in portal venous phase, 900 cc of Readi-CAT given 2 hours prior to image acquisition) images with intravenous and positive oral contrast 24 hours after presentation. Images demonstrate near normal appearance of small bowel (open straight arrow) and resolution of the free fluid (closed straight arrow). The vascular congestion also resolved (open curved arrow). No abnormal findings were noted.
DISCUSSION
Cocaine enteropathy is a phenomenon that has been described in the medical literature along with other causes of reversible ischemic bowel disease [1–3]. However, there have been no reports of the imaging findings of cocaine-induced enteritis.
The following search terms were entered into PubMed for a literature review: “cocaine enteropathy,” “cocaine enteritis,” “cocaine induced gastrointestinal ischemia,” “‘cocaine enteritis’ and CT,” and “cocaine and ‘mesenteric ischemia.’“ Even though several reports of cocaine-induced mesenteric ischemia were found; however, none had clearly documented imaging findings during and/or after the event.
The pathophysiology of cocaine-induced ischemia is fairly well understood. Cocaine inhibits the reuptake of norepinephrine at presynaptic terminals, which subsequently leads to catecholamine accumulation at postsynaptic membranes [1]. Some of the effects of the catecholamine surge are tachycardia, vasoconstriction and hypertension. Vasoconstriction can lead to ischemia, which in turn involves multiple organ systems. Another mechanism of ischemia includes cocaine’s vasoconstrictive effect on the arterial endothelium via changes in calcium channels [1].
Symptoms of acute mesenteric ischemia are variable but can include: nausea, vomiting, diffuse abdominal pain out of proportion to the physical examination, diarrhea, and hematochezia [8, 9]. Abdominal complications from cocaine-induced ischemia include: abdominal pain, bowel infarction, bowel perforation, hemorrhage, and other visceral ischemia [2, 3, 6]. Death has also been reported [5].
Imaging characteristics of mesenteric ischemia on CT examination include bowel edema, mucosal enhancement, venous engorgement, mesenteric free fluid, and dilatation of the lumen. Advanced ischemia can lead to bowel infarction, mural hemorrhage, pneumatosis intestinalis, free intraperitoneal air, and portal venous air. Bowel wall edema will typically manifest as thickening greater than 3 mm and can have decreased attenuation [4]. Typical thickness in the setting of mesenteric ischemia is 8–9 mm [4,11]. Mucosal enhancement can result from either venous occlusion or secondary hyperemia after bowel ischemia, as it is in this case. However, in the setting of acute arterial occlusion, mucosal enhancement would not be expected [11]. Mesenteric free fluid as it pertains to cocaine-induced bowel ischemia can be related to inflammation of the ischemic tissue. After a prolonged period of ischemia, adynamic ileus can lead to dilatation of the small bowel [11].
The differential diagnosis for acute mesenteric ischemia is extensive. Most causes of mesenteric ischemia can be grouped into five broad categories based on pathogenesis: reversible causes, arterial occlusion, venous occlusion, strangulation due to mechanical forces, and direct insult to the mesentery from trauma, vasculitis, cytotoxic drug exposure, or radiotherapy (Figure 6) [13,14].
Common reversible causes of mesenteric ischemia include hypovolemia and hypotension. Additionally, vasoconstrictive agents, such as cocaine, amphetamines, ergot derivatives, vasopressin, and digoxin, reduce blood flow to the mesentery [4,13]. A history of hypotension, volume loss, or exposure to vasoactive drugs should help narrow the differential.
Arterial occlusion leading to subsequent small bowel ischemia is often the result of a central embolus from a cardiac arrhythmia or valvular disease traveling into the mesenteric arteries, in addition to thromboembolic phenomena within the native mesenteric vessel. On imaging studies, filling defects within the artery and arterial luminal irregularities are important discriminators for arterial occlusion [4,13].
Venocclusive causes of ischemia are often more subacute in presentation, and risk factors for mesenteric venous occlusion include slowed venous transit from portal hypertension or right-sided heart failure and hypercoagulable states, which have long been associated with a risk of venous thrombosis. In the setting of venous occlusion, the bowel wall typically has decreased attenuation, unless hemorrhage is present. Adjacent mesenteric fluid is often also present [4,13].
Vasculitis is another cause of mesenteric ischemia that can result from a number of autoimmune vascular diseases, including Takayasu’s arteritis, polyarteritis nodosa, and microscopic polyangiitis, among others [13,14]. The imaging findings are very nonspecific and tend to involve smaller peripheral vessels.
Clinical history is crucial in identifying the pathogenesis of each of these entities. Management of mesenteric ischemia involves supportive care with the correction of the underlying cause, if possible, and potential surgical consultation for exploratory laparotomy and resection of nonviable bowel [3]. In many cases the primary bowel pathology, such as a large mass, infection, inflammation, or small bowel obstruction, may be readily apparent, but findings of secondary ischemia may be overlooked. Noting ischemia secondary to mechanical strangulation, vasospasm, or extrinsic compression can be important information to a referring clinician and can often guide clinical decision-making. A history of prior abdominal surgery or known malrotation can be an important clue in raising suspicion for a closed loop obstruction with possible resultant ischemia. Imaging findings of ischemia in the setting of a mechanical obstruction include wall thickening and adjacent mesenteric fluid; however, the enhancement pattern is variable [4]. In the case of a mechanical obstruction, a closed loop or “whirl” sign can be seen.
Cocaine is a potent drug commonly found in urban populations and can result in potentially life threatening complications. The reported lifetime incidence was 34.9 million people in the USA in 2003 alone [7]. The 2007 World Drug Report lists the use of cocaine in the USA at 1.6% of the adult population using 2006 data. Degenhardt et al report a lifetime prevalence in the US of 16% based on the WHO World mental health surveys. As cocaine remains a commonly encountered illicit drug, radiologists should be aware of its potential imaging characteristics and know when to appropriately include it in the differential.
TEACHING POINT
Mucosal enhancement, continuous long segment bowel wall thickening without skip segments, absence of mesenteric lymphadenopathy and “creeping fat,” mesenteric free fluid, mesenteric fat stranding, venous congestion, small bowel dilatation, and abnormal attenuation are small bowel findings that when found together are suggestive of mesenteric ischemia. Cocaine enteropathy remains a potential sequela of cocaine abuse and should be included in the differential considerations for bowel ischemia, especially with a history of cocaine use.
Table 1.
Summary table of cocaine-induced enteropathy
| Etiology |
|
| Incidence |
|
| Gender Ratio | 1.6:1 (Male:Female) for cocaine; approximately 1.1:1 (Male:Female) in sample of case reports for cocaine induced mesenteric ischemia[2] |
| Age Predilection | Affects all age groups, Average age 32 |
| Risk Factors | Cocaine use |
| Treatment | Cocaine cessation, supportive care |
| Prognosis | Can result in resolution of symptoms without permanent morbidity, but can also result in bowel infarction, hemorrhage, perforation, and death. |
| Findings on Imaging | Bowel wall thickening, changes in bowel wall attenuation, dilation of the bowel lumen, congestion of the mesenteric vessels, mesenteric free fluid, mesenteric fat stranding |
Table 2.
Differential diagnosis table for acute mesenteric ischemia
| Differential of Mesenteric Ischemia | History | CT Findings |
|---|---|---|
| Reversible causes of mesenteric ischemia (cocaine, shock bowel, other drugs) | History of Cocaine or other drug use, variable onset (acute in the case of cocaine), history of hypovolemia or heart failure | Variable bowel wall thickness and contrast enhancement (can have decreased enhancement, increased enhancement, or target like appearance), variable appearance of the mesenteric vessels and mesenteric fat, imaging findings are dependent on phase of ischemia |
| Arterial Occlusion (from atherosclerosis, aneurism, dissection, or embolism) | History of atherosclerosis, cardiac arrhythmia, valvular disease, acute onset | Variable thickness of bowel wall, filling defect within mesenteric vessels, variable bowel wall attenuation, no significant change in caliber of small bowel (unless late phase), no significant mesenteric changes (in early phase), variable enhancement |
| Venous occlusion (from portal/mesenteric venous thrombus or venous stasis) | Portal hypertension, right sided heart failure, hypercoagulable state | Wall thickening, decreased attenuation of bowel wall (unless hemorrhage is present), mesenteric fluid and ascites, variable enhancement |
| Mechanical strangulation (from closed loop obstruction, mass, or fibrosis) | Acute onset, intestinal malrotation, prior abdominal surgery | “whirl” sign, “spoke wheel” sign, hazy mesentery, thickened bowel wall with decreased enhancement (unless there is hemorrhage), variable enhancement, bowel dilatation with air fluid levels, venous engorgement |
| Miscellaneous direct mesenteric insults | History of vasculitis, trauma, cytotoxic drugs (chemotherapy agents, prior radioembolization) | Wall thickening, variable enhancement pattern, bowel dilatation, bowel necrosis (advanced stage) |
ABBREVIATIONS
- CT
Computed Tomography
- ED
Emergency Department
- mmol/L
millimoles per liter
REFERENCES
- 1.Tiwari A, Moghal M, Meleagros L. Life threatening abdominal complications following cocaine abuse. Journal of the Royal Society of Medicine. 2006;99(2):51–2. doi: 10.1258/jrsm.99.2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linder JD, Mönkemüller KE, Raijman I, Johnson L, Lazenby aJ, Wilcox CM. Cocaine-associated ischemic colitis. Southern Medical Journal. 2000;93(9):909–13. [PubMed] [Google Scholar]
- 3.Scharff JR, Longo WE, Vartanian SM, Jacobs DL, Bahadursingh AN, Kaminski DL. Ischemic colitis: Spectrum of disease and outcome. Surgery. 2003;134(4):624–629. doi: 10.1016/s0039-6060(03)00308-8. [DOI] [PubMed] [Google Scholar]
- 4.Furukawa A, Kanasaki S, Kono N, Wakamiya M, Tanaka T, Takahashi M, Murata K. CT diagnosis of acute mesenteric ischemia from various causes. AJR American Journal of Roentgenology. 2009;192(2):408–16. doi: 10.2214/AJR.08.1138. [DOI] [PubMed] [Google Scholar]
- 5.Lingamfelter DC, Knight LD. Sudden death from massive gastrointestinal hemorrhage associated with crack cocaine use: case report and review of the literature. The American Journal of Forensic Medicine and Pathology. 2010;31(1):98–9. doi: 10.1097/PAF.0b013e3181c6bed9. [DOI] [PubMed] [Google Scholar]
- 6.Maddox PR, Gardner-Thorpe D. Abdominal complications from crack cocaine. Annals of the Royal College of Surgeons of England. 2005;87(1):72–3. doi: 10.1308/1478708051289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations. Office on Drugs and Crime. World drug report. 2007. pp. 63–94. [Google Scholar]
- 8.Shaheen K, Alraies MC, Marwany H, Elueze E. Illicit drug, ischemic bowel. The American Journal of Medicine. 2011;124(8):708–10. doi: 10.1016/j.amjmed.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Umphrey H, Canon CL, Lockhart ME. Differential diagnosis of small bowel ischemia. Radiologic Clinics of North America. 2008;2008;46(5):943–52. vi–vii. doi: 10.1016/j.rcl.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Romano S, Niola R, Maglione F, Romano L. Small bowel vascular disorders from arterial etiology and impaired venous drainage. Radiologic Clinics of North America. 2008;46(5):891–908. doi: 10.1016/j.rcl.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Horton KM, Fishman EK. Multidetector CT angiography in the diagnosis of mesenteric ischemia. Radiologic Clinics of North America. 2007;45:275–288. doi: 10.1016/j.rcl.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 12.Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS medicine. 2008;5(7) doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rha SE, et al. CT and MR Imaging Findings of Bowel Ischemia from Various Primary Causes. Radiographics. 2000;20(1):29–42. doi: 10.1148/radiographics.20.1.g00ja0629. [DOI] [PubMed] [Google Scholar]
- 14.Ha HK, et al. Radiologic Features of Vasculitis Involving the Gastrointestinal Tract. Radiographics. 2000;20(3):779–94. doi: 10.1148/radiographics.20.3.g00mc02779. [DOI] [PubMed] [Google Scholar]