Abstract
A femoral hernia containing an appendix, known as de Garengeot hernia, is an uncommon and potentially confusing presentation. Prompt differentiation of this condition from other groin hernias in an acute setting will influence management and reduce morbidity. Computed Tomography (CT) should be performed in all suspected cases and an awareness of likely CT findings can facilitate rapid pre-operative diagnosis. Despite this, we present only the fourth published case of prospective CT diagnosis of de Garengeot hernia.
Keywords: de Garengeot, prospective diagnosis, femoral, hernia
CASE REPORT
A 45 year old female patient presented to the emergency department afebrile and haemodynamically stable, with a one day history of lower abdominal pain and an irreducible, mildly tender lump in her right groin. Physical examination revealed generalised lower abdominal tenderness and a 5cm lump in the right groin.
Serum full blood count revealed mildly elevated white cell count of 11.4 × 109/L (4.0–11.0 × 109/L), but no other derangement. Serum biochemistry, including lactate and lipase, were within normal limits.
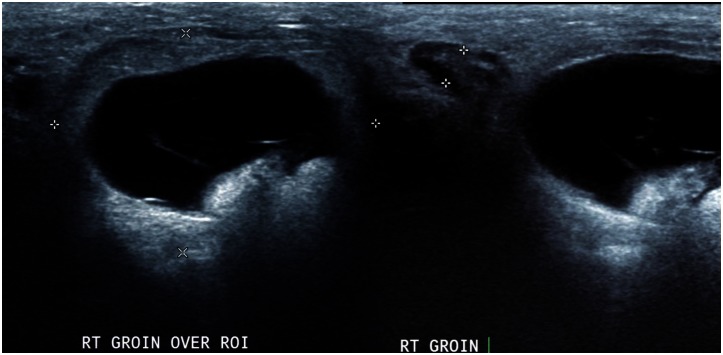
Subsequent Ultrasound examination demonstrated several small right inguinal lymph nodes and a 31 × 20 × 28mm hypoechoic, thick-walled, septated, avascular lesion that was interpreted as a probable necrotic lymph node (figure 1). Following surgical review, the patient was discharged from the emergency department with follow-up imaging, blood tests and nodal fine needle aspiration planned in 5–7 days.
Figure 1.
a) and b) 45-year-old woman presented with right groin pain and a tender lump. Findings: Complex, thick-walled, anechoic lesion in the right groin representing an incarcerated femoral hernia containing the appendix (defined by calipers on left), but which was mis-interpreted as a necrotic lymph node. A separate, small hypoechoic lymph node is demonstrated adjacent to the larger anechoic lesion between calipers on the right hand image. Subsequent CT scan revealed a de Garengeot hernia. Technique: 3.5 MHz curvilinear ultrasound transducer, transcutaneous scanning.
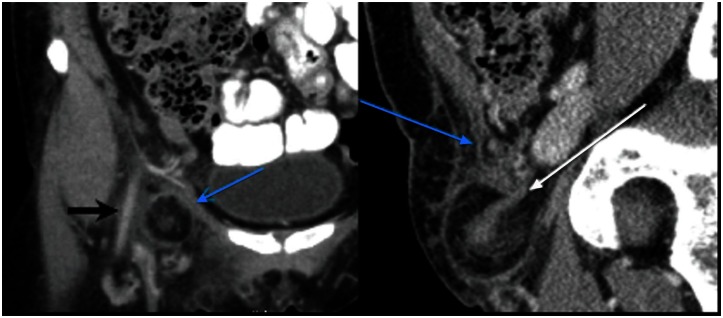
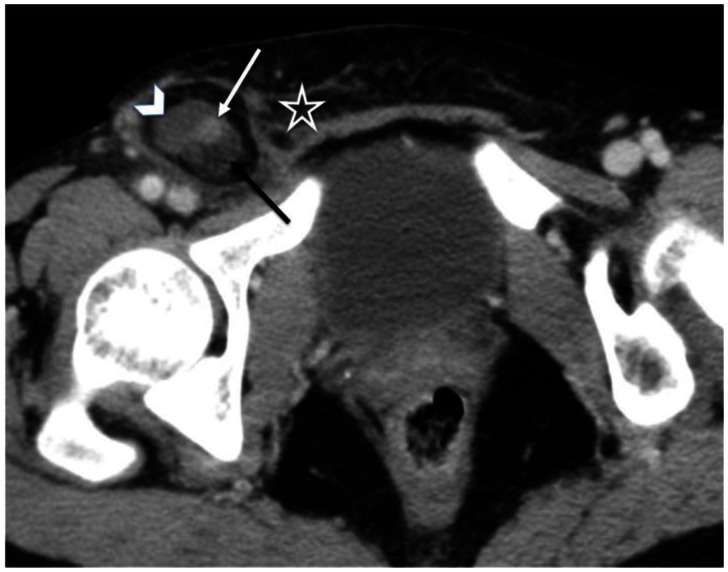
The patient re-presented three days later with worsening pain and abdominopelvic computed tomography (CT) demonstrated a right femoral hernia containing the appendix, mesoappendix and fat (figures 2 and 3). A small volume of fluid adjacent to the appendiceal tip was interpreted as suggesting perforation and the patient underwent urgent surgery. Intraoperative findings confirmed an incarcerated femoral hernia containing a necrotic appendiceal tip and hernia sac wall, without perforation. Open appendicectomy and sac resection was performed with hernia reduction and orifice repair. Histopathology described a 76mm × 6mm appendix displaying haemorrhagic necrosis. A benign lymph node was identified in the adjacent connective tissue. The patient experienced an uncomplicated post-operative recovery and was discharged on day 2.
Figure 2.
The same 45-year-old woman who represented with ongoing right groin discomfort. Findings: a) Coronal and b) sagittal intravenous and oral contrast enhanced CT scan of the pelvis, which demonstrates a de Garengeot hernia (femoral hernia containing appendix) (white arrows) with mesoappendix, fluid and fat also within the hernia sac. Femoral hernias pass medial to the femoral neurovascular bundle (black arrow) and posterior and inferior to the inguinal ligament (blue arrows). Technique: 252 mAs, 120 Kv, 3 mm slice thickness, 100 ml Ultravist 300.
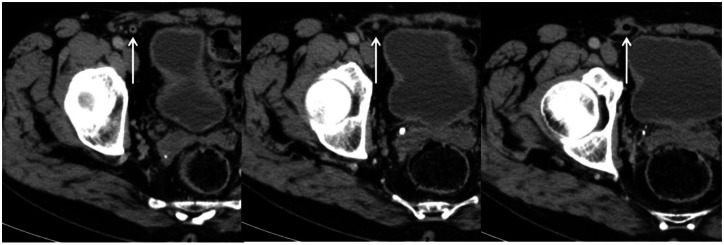
Figure 3.
The same 45-year-old woman with right groin discomfort. Findings: Axial intravenous contrast enhanced CT image from the same, which demonstrates a de Garengeot hernia (femoral hernia containing appendix). Note the appendix (white arrow), engorged mesoappendix (black arrow), fluid (arrow head) and surrounding stranding (star), suggests strangulation and possible perforation. Technique: 252 mAs, 120 Kv, 3 mm slice thickness, 100 ml Ultravist 300.
DISCUSSION
An incarcerated femoral hernia containing the appendix is an uncommon condition named in 2005 by Akopian and Alexander after the French surgeon Rene Jacques Croissant de Garengeot, who first described it in 1731 [1]. The number of reported cases varies with Capt. John Griffin of the US Air Force reporting in 1968 that 239 cases had been recorded since de Garengeot's first description in 1731 [2], but Akopian and Alexander, in their 2005 article first proposing eponymous nomenclature, identified only 70 cases in the literature [1, 3].
Femoral hernias account for less than 10% of groin hernias, and only 0.5% – 3.3% of femoral hernias reportedly contain the appendix [4–7]. Overall, only 0.13% of acute appendicitis cases involve the appendix located within an external hernia [3, 4, 6]. Most authors report that de Garengeot hernias represent <1% of all incarcerated femoral hernias, although the presence of the appendix within the femoral hernia sac is found more commonly at elective repair [3, 8, 9]. An inguinal hernia containing an appendix, known as Amyand hernia, is a more common finding because of the higher prevalence of inguinal hernias, and is often confused with de Garengeot hernia.
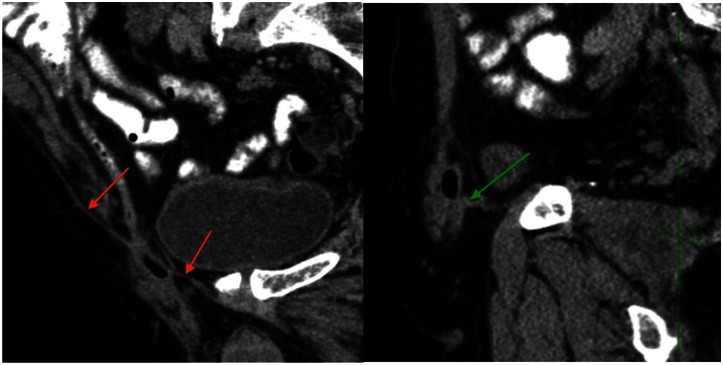
Pre-operative differentiation of femoral from inguinal hernia is essential as operative management of the two conditions is distinct. Femoral hernias pass posterior to the inguinal ligament through the "empty space" of the femoral canal, medial to the femoral vein (often visibly compressing this structure), artery and nerve (figure 2). In contradistinction, the neck of an inguinal or Amyand hernia passes anterior to the inguinal ligament (figure 4) as it runs along the inguinal canal (whether indirect via the deep inguinal ring, or direct) (figure 5). A similar and potentially confusing presentation, which can mimic de Garengeot Hernia, is the Littre Hernia, which involves a herniated Meckel's diverticulum [10]. Another very rare differential is the Velpeau Hernia, located below the inguinal ligament but anterior to the femoral neurovascular bundle. Successful identification of the appendix within the hernia is readily accomplished by following the intra-sac viscus to its junction with the caecum, frequently facilitated by use of multiplanar image reconstructions. Despite this, pre-operative diagnosis of de Garengeot hernia is rare, with only three cases of pre-operative CT diagnosis previously published [6, 8, 11].
Figure 4.
An asymptomatic 80-year-old male patient. Findings: a) Coronal and b) parasagittal MPR intravenous and oral contrast enhanced CT pelvis demonstrating an Amyand Hernia (appendix within the inguinal canal) as an incidental finding in. Note the distal appendix, which is not inflamed and contains distal intraluminal gas, traversing the neck of the hernia sac anterior to the inguinal ligament (red and green arrows). Technique: 312 mAs, 120 Kv, 3 mm slice thickness, 100 ml Ultravist 300.
Figure 5.
The same 80-year old male asymptomatic patient. Findings: Serial axial intravenous contrast enhanced CT images demonstrating an Amyand Hernia (appendix within the inguinal canal) as an incidental finding (white arrows). Technique: 312 mAs, 120 Kv, 3 mm slice thickness, 100 ml Ultravist 300.
Incarceration of the contents of a femoral hernia will often be determinable clinically, however clinical findings can be misleading [12], and identification of concordant CT features can facilitate diagnosis. Reported CT findings in surgically proven cases of incarcerated de Garengeot hernia include free fluid within the hernial sac, an engorged mesoappendix with associated fat stranding, and extraluminal or intramural gas [3, 4, 6]. Our case demonstrated all these features, except extraluminal or intramural gas (figure 3). Hernial strangulation, which is more common in femoral than inguinal hernias due to the narrowness of the femoral ring, often isolates infection and inflammation within the sac, resulting in localised symptoms only. Consequently, small bowel obstruction in de Garengeot hernia is rare and the clinical features of appendicitis may be absent [3].
Surgical management options for de Garengeot hernia include both laparoscopic and open approaches with mesh or suture hernia repair, with or without appendicectomy. Doddi et al (2010) and Sharma et al (2007) report that a normal appendix need not be removed at surgery and cite successful cases involving simple reduction of the normal appendix followed by laparoscopic mesh repair of the hernial orifice [3, 7]. Conversely, in cases likely to involve difficult reductions, or with clinical or imaging features suggestive of appendicitis or perforation, the risk of sepsis and abscess formation will necessitate open appendicectomy with sutured hernia repair.
Delay in treatment increases the risk of infection and complications associated with perforation [13], and it is important that CT scanning be performed immediately in cases of suspected incarcerated de Garengeot hernia [4]. It is also critical to identify CT features that suggest either appendiceal inflammation or perforation. Features associated with perforation or necrosis are limited essentially to the presence or absence of intramural or extraluminal gas [14]. While findings such as free fluid within the hernia sac or peri-appendiceal stranding are associated with appendiceal inflammation [15], they are less reliable indicators of perforation, as demonstrated by the case presented. All such features are of utility in clinical decision-making and should be conveyed in the imaging interpretation.
TEACHING POINT
Prospective CT diagnosis of de Garengeot hernia, and differentiation from other groin hernias, is achievable and important for determining appropriate treatment options. Cross sectional imaging should be considered in suspected cases to allow for confirmation of diagnosis, pre-operative assessment for inflammation or perforation, and for determining an appropriate surgical approach.
Table 1.
Summary table for de Garengeot Hernia
| Etiology | Herniation of intraabdominal contents, including vermiform appendix, through the femoral canal. |
| Incidence | 1 in 2000 to 1 in 330 of all groin hernias |
| Gender ratio | More common in women |
| Age predilection | None |
| Risk factors | Idiopathic; obesity; raised intraabdominal pressure; previous surgery |
| Treatment | Laparoscopic or open appendectomy and hernia repair. |
| Prognosis | Good prognosis with timely surgical care. Risks from delayed diagnosis include perforated viscous, sepsis or post-surgical complications. |
| Findings on imaging | Hernial sac passing through the femoral canal (posterior and inferior to the inguinal ligament, and medial to the femoral neurovascular bundle) containing the appendix, which may or may not be inflamed. Presentation is usually secondary by incarcerated hernia or acute appendicitis. |
Table 2.
Differential diagnosis table for de Garengeot Hernia
| Differential Diagnosis | CT | Ultrasound |
|---|---|---|
| De Garengeot Hernia | Appendix within hernial sac passing posterior and inferior to the inguinal ligament, and medial to the femoral neurovascular bundle. Appendix may or may not be inflamed. Intramural gas suggests ischaemia. Extraluminal gas is diagnostic of perforation. | Hernial positioned medial to the femoral artery and nerve. Hernial sac may or may not be seen to contain viscous, mesentery, fluid or gas. |
| Amyand Hernia | Appendix within the inguinal canal, passing anterior to the inguinal ligament. | Groin mass with sonographic appearance of an inguinal hernia containing bowel or mesentery. |
| Littre Hernia | Meckel’s diverticulum within a hernial sac. | Sonographically similar to femoral or inguinal hernia. |
| Velpeau Hernia | Hernia passing inferior to the inguinal ligament but anterior to the femoral neurovascular bundle. | Sonographically similar to femoral hernia. Hernia passes superficial to the femoral neurovascular bundle. |
| Cloquet Hernia | Hernia through the pectineus fascia, overlying the pectineus. | Sonographically similar to femoral hernia, medial to the femoral neurovascular bundle. |
| Laugier Hernia | Hernia through the lacunar ligament, along the inferomedial edge of the inguinal ligament. | Sonographically similar to femoral hernia, usually superior to the femoral neurovascular bundle. |
| Serafini Hernia | Hernia inferior to the inguinal ligament but posterior to the femoral neurovascular bundle. | Sonographically similar to femoral hernia, deep to the femoral veins and arteries. |
| Infected/necrotic lymphadenopathy | Enlarged inguinal lymph nodes with a hypodense central core and surrounding fat stranding. | Enlarged, hypervascular, hypoechoic lesion in the groin surrounding by other prominent lymph nodes. |
ABBREVIATIONS
- CT
Computed Tomography
- US
United States
- USS
Ultrasound Scan
REFERENCES
- 1.Akopian G, Alexander M. De Garengeot hernia: appendicitis within a femoral hernia. Am Surg. 2005 Jun;71(6):526–527. [PubMed] [Google Scholar]
- 2.Griffin J. Incarcerated Inflamed Appendix in a Femoral Hernia Sac. Am J Surg. 1968 Mar;115:364–366. doi: 10.1016/0002-9610(68)90161-x. [DOI] [PubMed] [Google Scholar]
- 3.Doddi S, Sagar V, Singhal T, et al. Femoral hernia with a twist. Case Report Med. [serial online] 2010. Aug, [Accessed September 5, 2012]. Available at http://ukpmc.ac.uk/articles/PMC2931410. [DOI] [PMC free article] [PubMed]
- 4.Ebisawa K, Yamazaki S, Kimura Y, et al. Acute appendicitis in an incarcerated femoral hernia: A case of De Garengeot hernia. Case Rep Gastroenterol. 2009 Nov;3:313–317. doi: 10.1159/000250821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barut I, Tarhan O. A rare variation of Amyand's hernia: gangrenous appendicitis in an incarcerated inguinal hernia sac. Eur J Gen Med. 2008;5(2):112–114. [Google Scholar]
- 6.D'Ambrosio N, Katz D, Hines J. Perforated appendix within a femoral hernia. AJR. 2006 Mar;186:906–907. doi: 10.2214/AJR.05.0080. [DOI] [PubMed] [Google Scholar]
- 7.Sharma H, Jha P, Shekhawat N, et al. De Garengeot hernia : an analysis of our experience. Hernia. 2007 Jun;11(3):235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 8.Zissin R, Brautbar O, Shapiro-Feinberg M. CT diagnosis of acute appendicitis in a femoral hernia. Br J Radiol. 2000 Sep;73(873):1013–1014. doi: 10.1259/bjr.73.873.11064659. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen E, Komenaka I. Strangulated femoral hernia containing a perforated appendix. Can J Surg. 2004 Feb;47(1):68–69. [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips A, Aspinall S. Appendicitis and Meckel's diverticulum in a femoral hernia: simultaneous De Garengeot and Littre's hernia. Hernia. 2011 Mar; doi: 10.1007/s10029-011-0812-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Fukukura Y, Chang S. Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom Imaging. 2005 Sep-Oct;30(5):620–622. doi: 10.1007/s00261-004-0283-3. [DOI] [PubMed] [Google Scholar]
- 12.Hsiao T, Chou Y. Appendiceal pus in a hernia sac simulating strangulated femoral hernia: a case report. Int J Gen Med. 2011 Mar;4:235–247. doi: 10.2147/IJGM.S16413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caygill P, Nair R, Sajjanshetty M, Francis D. An unusual groin exploration: De Garengeot's hernia. Int J Surg Case Rep. 2011 Mar; doi: 10.1016/j.ijscr.2011.01.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luchs J, Halpern D, Katz D. Amyand's Hernia: Prospective CT Diagnosis. J Comput Assist Tomogr. 2000 Nov-Dec;24(6):884–886. doi: 10.1097/00004728-200011000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Maizlin Z, Mason A, Brown C, Brown J. CT findings of normal and inflamed appendix in groin hernia. Emerg Radiol. 2007 Jun;14(2):97–100. doi: 10.1007/s10140-007-0601-5. [DOI] [PubMed] [Google Scholar]