Abstract
Objective
This study determined the hormonal and subjective appetite responses to exercise (1-h continuous v. intermittent exercise throughout the day) in obese individuals.
Design and Methods
Eleven obese subjects (>30 kg/m2) underwent 3, 12-hour study days: control condition (sedentary behavior-SED), continuous exercise condition ((EX) 1-h exercise), and intermittent exercise condition ((INT) 12 hourly, 5-minute bouts). Blood samples (every 10 min) were measured for serum insulin and total peptide YY (PYY) concentrations, with ratings of appetite (visual analog scale-VAS: every 20 minutes). Both total area under the curve (AUC), 2-h AUC and AUC above baseline, and subjective appetite ratings were calculated.
Results
No differences were observed in total PYY AUC between conditions, but hunger was reduced with INT (INT<EX; P<0.05), and satiety was increased with both SED and INT conditions (INT>EX and SED>EX; P<0.05). A correlation existed between the change in total PYY and insulin levels (r=−0.81; P<0.05), and total PYY and satiety (r=0.80; P<0.05) with the EX condition, not the SED and INT conditions.
Conclusion
The total PYY response to meals is not altered over the course of a 12-h day with either intermittent or continuous exercise; however, intermittent exercise increased satiety and reduced hunger to a greater extent than continuous exercise in obese individuals.
Keywords: gut hormones, exercise, visual analog scale, obesity
Introduction
Peptide YY (PYY) is among the gut hormones which act to control food intake. Obesity is associated with attenuated PYY concentrations in both the fasting and the postprandial state (1,2). The response to PYY infusion in obese individuals seems well preserved with increased indices of satiety and a reduction in subsequent energy intake (3), resulting in PYY being identified as a potential therapeutic target for weight management. Altering dietary habits towards a positive energy balance for three weeks is known to alter appetite-regulating hormone concentrations (4), and is associated with increased energy intake during the subsequent three day period.
Exercise, which can impart a negative energy balance, is also known to alter appetite-regulating hormone concentrations and promote tighter appetite control (5–9). Two recent studies demonstrated that 60 minutes of moderate-intensity exercise in healthy, normal-weight individuals increased plasma PYY concentrations, and transiently reduced subjective scores for hunger (8,10). This increase in PYY has also been demonstrated in obese individuals (11) following moderately-intense exercise (60 min of 50 v. 65% VO2max). Interestingly however, resistance exercise did not result in any increase in PYY levels (10). Research conducted on the acute responses of appetite-related hormones to exercise has only investigated the concentration of these peptides in the immediate post-exercise period (5,6,8), without examining the impact throughout the day when additional meals are consumed. Further since our exercise guidelines now encourage exercise to be done in short intermittent bouts throughout the day, gaining an understanding of this type of exercise regimen on appetite-related hormones and satiety throughout the day is critically important.
An inverse relationship between insulin and PYY concentrations has been reported. PYY seems to have no effect on baseline insulin, glucose, or glucagon secretion, but decreases glucose-stimulated insulin production (12,13). More specifically, an increased PYY concentration may inhibit insulin production through a neuropeptide-Y mechanism acting at the level of the pancreatic islets (14). A exercise-induced increase in endogenous PYY may contribute to decreased insulin levels and it is possible that exercise intensity or duration may modify this relationship between PYY and insulin levels.
The purpose of this study was: 1) to establish the circulating total PYY concentrations and hunger/satiety responses to meal consumption in obese individuals over the course of a 12 h day, 2) to establish how different exercise regimens (continuous v. intermittent exercise) alters total PYY concentration profile and subjective measures of appetite and 3) determine the relationship between total PYY and insulin/glucose concentrations throughout the 12-h study period. It was hypothesized that a continuous bout of exercise would increase total PYY levels to a greater degree than intermittent bouts exercise; however, both exercise conditions were expected to increase total PYY concentration to a greater degree than the sedentary condition. Furthermore, it was hypothesized that the increase in circulating total PYY, induced by continuous and intermittent exercise, would correlate with enhanced satiety and reduced hunger, and that these effects would be altered throughout the day. Additionally, it was expected that an inverse correlation between total PYY and insulin concentrations in obese individuals would become stronger following both exercise conditions due to the increase in total PYY and proposed effects on glucose-stimulated insulin production.
Methods and Procedures
Study subjects
All subjects signed an informed consent document approved by the Syracuse University Institutional Review Board prior to participating in this study. Young (18–35 years old), weight-stable, obese (BMI >30 kg/m2) individuals who were free from gastrointestinal problems and orthopedic limitations to normal walking activity were recruited into this study. Female subjects did not use oral contraceptives, and were consistently tested within the follicular phase (days 2–7) of their menstrual cycles to limit potential hormonal effects on appetite regulation. According to self-report, all subjects met general guidelines for moderate physical activity (3–5 days per week, approximately 150 minutes total).
Twenty-three subjects completed an oral glucose tolerance test (75 g glucose), resting blood pressure measurement (Omron HEM automatic blood pressure monitor - Omron, Kyoto, Japan), and lipid profile (Cholestech LDX -Cholestech Corporation, Hayward, CA). General health, cardiovascular disease risk, physical activity, and inactivity levels were recorded through the use of questionnaires.
Anthropometric data including height and weight were recorded, and body mass index calculated to establish obesity criteria (BMI> 30 kg/m2). Air-displacement plethysmography (BODPOD system, Life Measurement, Inc. Concorde, CA) was performed according to manufacturer’s specifications (15). Exclusion criteria for health measures included high blood pressure (>140 systolic and/or >90 diastolic), high cholesterol (total cholesterol>200 mg/dl), or the use of medications to control blood pressure or cholesterol levels. Peak oxygen consumption (VO2peak) was assessed from expired gases (Cosmed Quark b2, Rome, Italy) using a previously reported (16) treadmill-based step protocol until volitional exhaustion.
Experimental Design
Subjects completed three 12 h testing days using a randomized cross-over design. Participants reported to the Human Performance Laboratory at 0700 h following a 12 h fast from food and caffeine, and avoidance of exercise for 24 h. Subjects completed either a sedentary (SED), continuous exercise (EX; 1 h continuous bout from 0705–0805 h), or intermittent exercise protocol (INT; 12, 5-min bouts, performed intermittently every hour). The total exercise duration (60 min) and intensity (60–65% VO2 peak) were matched between the EX and INT study days. Subjects recorded their dietary intake for the three days prior to the first experimental condition using a food-diary, and were asked to match intake prior to subsequent testing as closely as possible.
Study Protocol
At 0700 h, a registered nurse placed a Teflon catheter into the antecubital vein of each subject for blood sampling. Baseline blood samples (10 ml) were drawn prior to the ingestion of the first meal. Each meal (250 kcal) consisted of a mixed, high-carbohydrate liquid (15% protein (PRO), 65% carbohydrate (CHO), 20% fat (FAT)) (Wegmans Nutritional Beverage, Wegmans, Rochester, NY, USA) which was provided every 2 h, so that a total of 1500 kcal was consumed during each study period. Exercise sessions started immediately following baseline blood sampling and consumption of the first meal. Subjects remained sedentary outside of prescribed activity during the EX and INT conditions.
Blood samples were drawn from the indwelling catheter at 10 min intervals over the course of each study day. Samples were assayed in duplicate for serum glucose using a commercially available glucose oxidase assay (Sigma-Aldrich Corp., St. Louis, MO). Additionally, samples were centrifuged (3000 g, 5-minutes, 4°C) and assayed for serum total PYY and insulin concentrations (Millipore, Billerica, MA) using Luminex xMap Technology (Linco Research, St. Charles, MO) on a Luminex 100/200 platform (Luminex Corporation, Austin, TX). All procedures followed manufacturer’s instructions, with quality controls within expected ranges for each assay. Inter-assay and intra-assay coefficients for insulin and total PYY were 4.0 and 9.5%, and 6.0 and 5.3%, respectively. The lowest limits for detection of this assay were 137 and 14 pg/ml, for insulin and total PYY, respectively. All samples for a given subject were analyzed in the same assay series.
Subjective Hunger and Satiety (VAS scores)
Subjects were asked to record an index of their hunger and satiety at 20-minute intervals throughout each study day using a visual analogue scale (17). Participants made a mark along a 100 mm line indicating the intensity of their hunger and satiety on a scale of 1–100. The VAS for hunger asked ‘How hungry do you feel?’ and indicators of ‘Not at all hungry’ and ‘As hungry as I have ever felt’ were included at the left and right ends of the scale, respectively. Similarly, the satiety VAS asked ‘How full do you feel?’ with ‘Not at all full’ and ‘As full as I have ever felt’ included as scale anchors. Each mark in the 100 mm line was measured from the left, and the mm length recorded as the VAS value.
Statistical Analysis
Area under the curve (AUC) for serum total PYY and VAS scores for hunger and satiety were calculated as the area above baseline using the trapezoidal method within each meal condition (GraphPad Prism version 3.00 for Windows, GraphPad Software, San Diego, California, USA). The AUC was calculated for the entire 12-hour period (tAUC) and each 2-h increment starting from first blood sample (iAUC; 0705–1905 h). The change (Δ) in total PYY, insulin, and glucose concentrations; as well as VAS scores for hunger and satiety were calculated for each 2 h meal interval by subtracting 2 h baseline from 2 h peak values. Subsequently, percent change values were calculated from these Δ values by dividing the ((peak-baseline)/baseline values)*100. A one-way ANOVA with repeated measures assessed the differences in the baseline, peak, 2 h and 12 h AUC for total serum PYY concentrations and VAS scores between meal conditions. Two-tailed Pearson’s correlations between the average magnitude of change, and average percent change between 2 h total PYY concentrations and insulin, glucose, and VAS scores for satiety across study days were calculated. Significance levels in all statistical tests was accepted at α=0.05. Statistical analyses were performed with SPSS for Windows, version 16.0 (SPSS, Inc., Chicago, USA), and all data are reported as mean ± standard error of the mean.
Results
Subject Characteristics
Twenty-three subjects met the requirements for this study, completed the initial screening visit, and came to the lab for the first experimental session. Of these individuals, one did not return subsequent scheduling requests, and eleven were unable to complete all three trials due to difficulties in maintaining the antecubital catheter for the full 12 h sessions. Eleven subjects (3 women, 8 men) completed all trials (Table 1). Female subjects had a higher percent body fat, and total and LDL cholesterol levels than their male peers (Table 1; P<0.05). All of the subjects (n=11) had impaired fasting glucose concentrations (>110 mg/dL). None of the study subjects had more than a ±2% change in weight between testing days. Subjects reported an average of 4.7±0.4 meals per day, and participation in 3.3±0.6 bouts of moderate-intensity physical activity per week. The female subjects had a lower VO2 peak (25.5±1.8 ml/kg/min) than the male subjects (32.6±2.5 ml/kg/min). During the study days, treadmill speeds ranged from 3 to 3.5 mph (3.2±0.1 mph), with ranges in grade between 0 and 8% (2.9±1.0%).
Table 1.
Subject Characteristics
| Female (n=3) | Male (n=8) | Total (n=11) | |
|---|---|---|---|
| Age (yrs) | 25±3.1 | 25.3±1.5 | 25.2±1.3 |
| Height (cm) | 170±0.5 | 176.0±2.7 | 174.4±2.1 |
| Weight (kg) | 103.6±10.2 | 104.5±4.7 | 104.3±4.1 |
| BMI (kg/m2) | 35.8±3.3 | 33.8±1.4 | 34.3±1.3 |
| Body Fat % | 42.0±3.3 | 28.9±2.7* | 32.5±2.8 |
| Physical Inactivity (self-report hours per day) | 19.7±1.6 | 16.9±0.9 | 17.6±0.8 |
| Fasting Blood Glucose (mg/dl) | 91.3±4.7 | 84.8±2.2 | 86.5±2.1 |
| 2h OGTT Glucose (mg/dl) | 112.7±8.1 | 103.6±5.9 | 106.1±4.8 |
| Resting Systolic BP (mmHg) | 125.3±7.7 | 120.8±3.1 | 122.0±2.9 |
| Resting diastolic BP (mmHg) | 68.3±3.8 | 65.9±1.8 | 66.5±1.6 |
| Total Cholesterol (mg/dL) | 181±2.4 | 127.3±2.6* | 145.2±8.6 |
| LDL Cholesterol (mg/dL) | 91.5±10.2 | 51.3±5.7* | 64.7±7.7 |
| HDL Cholesterol (mg/dL) | 57.5±8.6 | 38.8±4.3 | 45±4.5 |
| Cholesterol Ratio (TC/HDL) | 3.3±0.4 | 3.5±0.6 | 3.41±0.4 |
Mean±SEM.
P<0.05 vs. female subjects.
Hormone Concentrations
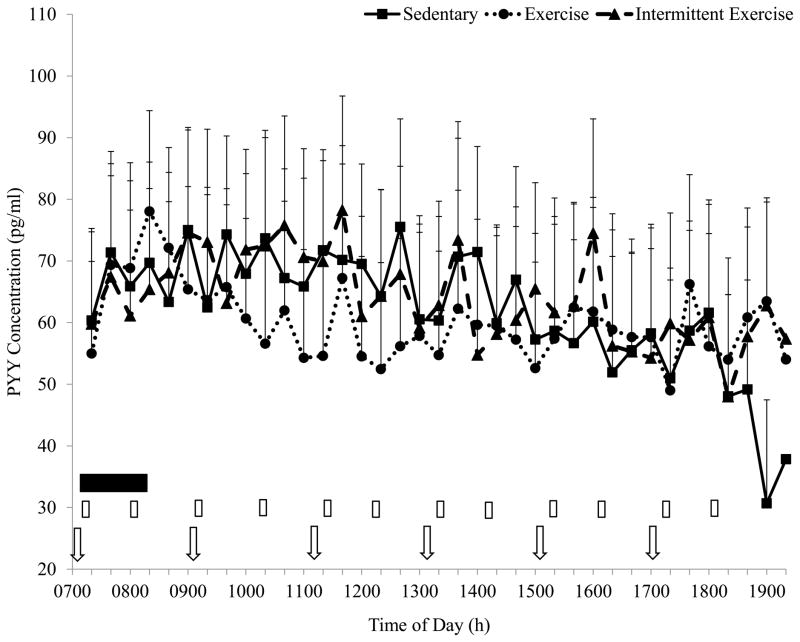
Baseline total PYY values did not differ across conditions following the overnight 12 h fast. The pattern of hormone release was similar across conditions (Figure 1; P>0.05). Similarly, there were no significant differences in the change in total PYY between conditions (Table 2; P<0.05). Integrated area under the curve analysis for total PYY over the course of the day were comparable among the SED, EX, and INT conditions, and examination of the 2 h total PYY responses to each meal revealed no significant differences between conditions during any of these meal blocks (P>0.05).
Figure 1.
Total PYY pattern of response over 12 h for the three study conditions. No significant differences across condition (P>0.05). ⇩- meal ingestion.
Table 2.
Change in Total PYY, Insulin, and Satiety per Meala
| Time of Day (h) | 0700–0900 | 0900–1100 | 1100–1300 | 1300–1500 | 1500–1700 | 1700–1900 |
|---|---|---|---|---|---|---|
| PYY (pg/ml)- SED | 17.7 | 11.4 | 0.3 | 6.2 | 5.4 | 11.7 |
| EX | 22.4 | −2.7 | 5.5 | 7.3 | 5.0 | 10.2 |
| INT | 16.4 | 13.0 | 5.3 | 10.4 | 14.8 | −6.7 |
| Insulin (pg/ml)- SED | 804.5 | 581.3 | 624.8 | 593.6 | 561.1 | 740.9 |
| EX* | 207.3 | 584.3 | 477.3 | 418.6 | 484.4 | 600.7 |
| INT* | 513.8 | 539.0 | 430.8 | 494.8 | 479.0 | 441.1 |
| VAS Satiety (mm)- SED | 9.2 | 3.2 | 10.0 | 10.2 | 11.3 | 15.3 |
| EX | 1.0 | −8.7 | −10.6 | −8.3 | −5.1 | −7.7 |
| INT | 9.0 | 5.8 | 5.4 | 3.1 | 12.1 | 8.4 |
Mean
P<0.05 vs. SED condition.
Calculated as 2h - baseline value for each meal condition. EX-exercise, INT-intermittent exercise
VAS Scores
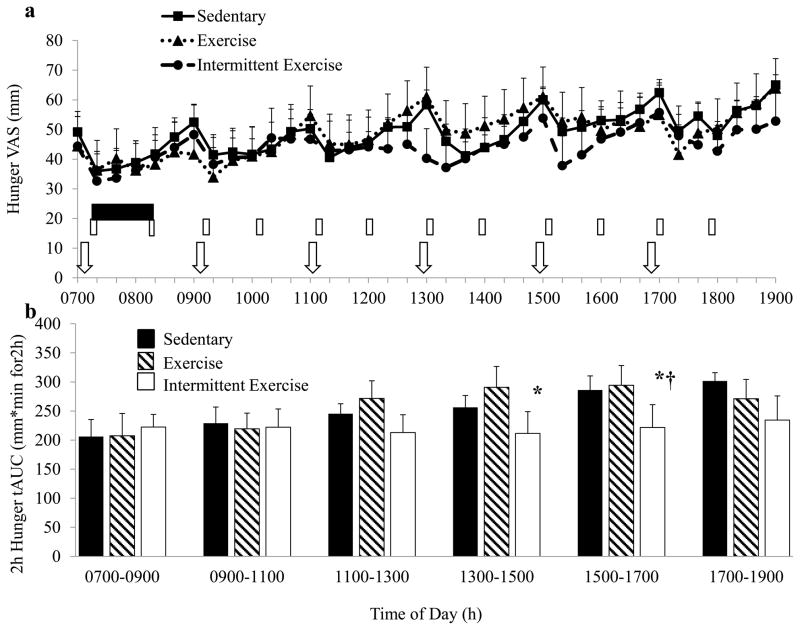
Baseline hunger VAS values following the 12 h fast were not different between conditions (Figure 2a; SED: 49.2±22.9, EX: 42.8±24.9, INT: 51.7±17.3 mm). When the 12 h tAUC and iAUC for the VAS scores for hunger were compared, no significant differences were noted across conditions (tAUC: SED: 1705.4±315.8, EX: 1744.9±584.2, INT: 1490.617.8 mm*min for 12 h; iAUC SED: 1622.5±298.8, EX: 1669.2±573.2, INT: 1402.4±623.2 mm*min for 12 h).
Figure 2.
a) Hunger pattern of response over 12 h for the three study conditions. No significant differences by condition (P>0.05). ⇩- meal ingestion.
 - exercise condition; 1-hour walking bout. ▯- intermittent exercise condition; hourly 5-minute walking bouts. b) 2 h tAUC for hunger VAS scores. *Significantly different from EX condition (P<0.05). †Significantly different from SED condition (P<0.05).
- exercise condition; 1-hour walking bout. ▯- intermittent exercise condition; hourly 5-minute walking bouts. b) 2 h tAUC for hunger VAS scores. *Significantly different from EX condition (P<0.05). †Significantly different from SED condition (P<0.05).
Examination of the VAS scores during each 2 h meal period revealed a significant effect of condition in the hunger response between 1300–1500 h (Figure 2b; SED: 256.2±20.5, EX: 290.7±36.0, INT: 211.4±37.4 mm*min for 2 h; P<0.05), where intermittent exercise resulted in a reduced hunger AUC than in the EX condition. Between 1500–1700 h, the hunger tAUC was lower in response to the INT compared to the SED and EX conditions (Figure 2b; SED: 286.1±24.2, EX: 294.3±33.9, INT: 221.7±39.2 mm*min for 2 h; P<0.05). A similar trend of a lower 2 h hunger AUC in the INT condition approached significance (P=0.068) in the hunger response between 1700–1900 h.
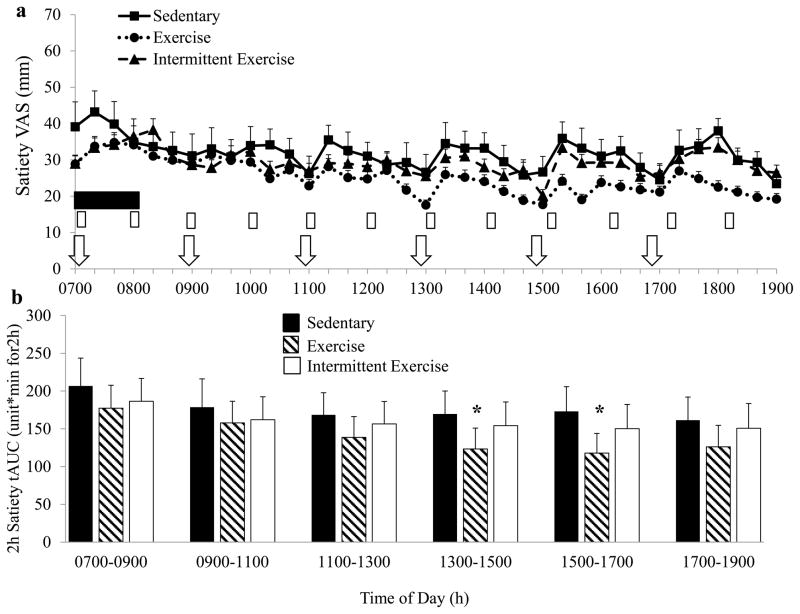
No significant differences were noted between conditions for the baseline satiety VAS at the beginning of each testing day (Figure 3a; SED: 39.1±24.1, EX: 28.8±17.7, INT: 29.0±19.0 mm). Similar to the hunger VAS scores, there were no significant differences between conditions when total or incremental satiety AUC over the course of the study days were compared. However the 2 h meal intervals for satiety demonstrated improvements later in the day in the SED and INT, compared to the EX condition. Between 1300–1500 h and 1500–1700 h, the 2 h tAUC for satiety was higher (P<0.05) in the SED and INT conditions than the EX condition (Figure 3b; 1300: SED: 167.9±30.3, EX: 123.3±27.6, INT: 154.2±31; 1500: SED: 173.1±32.7, EX: 117.9±26.1, INT: 150.2±31.3 mm*min for 2 h; P<0.05).
Figure 3.
a) Satiety pattern of response over 12h for the three study conditions. No significant differences by condition (P>0.05). ⇩- meal ingestion.
 - exercise condition; 1-hour walking bout. ▯- intermittent exercise condition; hourly 5-minute walking bouts. b) 2 h tAUC for satiety VAS scores. *Significantly different from SED and INT conditions (P<0.05).
- exercise condition; 1-hour walking bout. ▯- intermittent exercise condition; hourly 5-minute walking bouts. b) 2 h tAUC for satiety VAS scores. *Significantly different from SED and INT conditions (P<0.05).
Relationship between Total PYY and Insulin, Glucose, and Satiety
A significant inverse relationship was reported between the in Δ total PYY and insulin concentrations within each 2 h meal interval in the EX (r=−0.81; P=0.05), but not the SED (r=0.70; P>0.05) and INT conditions (r=0.72; P>0.05). This finding was supported by the fact that the percentage change values for total PYY and insulin during each 2 h interval were also significantly correlated in only the EX condition (P=−0.88; P<0.05).
There were no significant correlations reported between the Δ total PYY or percentage change in total PYY and glucose levels across the 2 h meal intervals in any of the experimental conditions. However, the Δ total PYY was strongly correlated with the ΔVAS scores for satiety across 2 h meal intervals (r=0.80, P<0.05) in the EX condition. There were no significant correlations noted between total PYY and satiety; or insulin and satiety in the SED and INT conditions.
Discussion
Exercise has been shown to alter appetite-regulating hormone concentrations, and in particular total PYY concentration, as well as promoting tighter appetite control (5–9). This research however, has typically focused on continuous exercise, and monitored appetite and appetite-regulating hormones during the period immediately (1–3 h) post-exercise (5,6,8). This study extends these findings by examining the effects of exercise on appetite-related hormones and satiety beyond the first few hours of the post-exercise period and extending these observations out over 12 h. This study reports for the first time that the addition of a one hour morning exercise (EX) or intermittent 5-minute exercise bouts every hour throughout the day (INT) does not alter total PYY concentrations over the course of a 12 h day in obese individuals with impaired fasting glucose. However the intermittent exercise resulted in lower perceived hunger and increased satiety in the mid-afternoon hours, which did not occur in the sedentary or exercise condition.
Despite no change in the hormonal responses, intermittent exercise was more effective in reducing the perception of hunger as the day progressed with a robust attenuation of hunger perception (32.3%) demonstrated between the INT and EX conditions between 1500–1700 h, and a 24.6 and 26.9% reduction in hunger between 1700–1900 h when compared to the SED and EX conditions, respectively. Intermittent activity also improved the perception of satiety, with increased indices of meal-induced satiety reported in the INT compared to the EX and SED conditions. Between 1500–1700 h, intermittent exercise resulted in a 25.7% increase in satiety when compared to EX. Similarly, in the 2 h period between 1700–1900 h, the perceived scores for satiety in the EX condition were 42.6 and 24.8% lower than the SED and INT conditions, respectively. The current findings demonstrate little to no effect of continuous exercise (EX) on appetite over the course of a twelve hour day, in agreement with a previous review (18). However, there is evidence of an accumulating effect of intermittent exercise (INT) on appetite, independent of changes in total PYY, which may result in sustained appetite modulation over the course of the day. Intermittent exercise therefore presents a promising alternative for weight maintenance and weight loss.
Previous studies have demonstrated that prolonged, moderate-intensity exercise increases PYY concentrations (9,11,19), though this has not been demonstrated exclusively (20) and these changes are often elevated transiently (11). While total PYY was elevated immediately following the morning exercise bout (EX) as compared to the SED (11.9%) and INT conditions (19.3%), this effect had disappeared by 2 h (Figure 1). The 12 and 2 h AUC for total PYY concentrations were not different between conditions, which is consistent with previous findings (11).
While Martins et al (7) did not report differences between VAS measures of hunger and satiety in response to a 1 h bout of moderate exercise (65% of max heart rate), their measurements were restricted to a 3 h period after the exercise bout. Likewise we did not observe any changes in hunger or satiety in the immediate 3-h period following the acute, continuous exercise bout. While one-hour of moderate-intensity exercise at the beginning of the day did not result in changes in the hunger and satiety perception in our obese subjects with impaired fasting glucose, intermittent exercise participation resulted in a decreased hunger perception (Figure 2) and increased satiety later in the day (Figure 3). This finding is surprising, as previous work has demonstrated that intermittent aerobic exercise results in a higher excess post-exercise oxygen consumption and energy expenditure than an intensity- and duration-matched single bout of aerobic exercise (21,22). The potential for an exercise intervention that increases overall daily energy expenditure, while decreasing hunger and increasing satiety, is promising.
An inverse relationship was confirmed between insulin and total PYY concentrations over the course of the day during the EX condition; where an increase in total PYY concentration was associated with an attenuated increase in insulin concentrations. This was not demonstrated in the SED and INT conditions. This inverse relationship during the EX condition occurred despite no differences in the indices of total PYY (12 h or 2h AUC, Δ or percent change per meal) between the study conditions. The continuous physiological stimulus of the 1 h morning exercise bout may have been sufficient in increasing the total PYY concentration or action which may have inhibited insulin release. A similar strengthening of the relationship between glucose-stimulated insulin production and PYY has been demonstrated in older, obese individuals with impaired glucose tolerance following a strict, twelve-week exercise intervention (23). It was postulated that this response was due to the incretin effect of glucose-dependent insulinotropic polypeptide (GIP) (23). Additional investigations in obese individuals concerning the relationship between PYY and insulin levels with exercise are needed to better understand these phenomena. In addition, the complex milieu of appetite hormones including the redundant physiological mediators and pathways which control of appetite regulation (23,24), both at rest and during exercise, warrant further study.
The strength of this project is that we have extended previous research by frequently sampling blood over a 12 h period providing insight into the hormonal profile to subsequent meals, and not just the meal immediately following the exercise bout. This study design also allowed us to examine the effect of intermittent exercise throughout the day which is now being widely prescribed. Discrepancies in our findings from the previous report can be attributed to the extended period of sampling done in the present study. The six-meal, 1500 kcal diet utilized in this project was selected since this would approximate the energy needs throughout the study days, and mimics the frequent snacking often observed in the general public. This 1500 kcal diet represented a reasonable caloric intake for adults considering we did not include a dinner time meal. It is possible that subjects were in a slight caloric deficit on the exercise days, which may have somewhat influenced the subjective hunger and satiety responses. The decision to adopt a study design where participants consumed a meal immediately prior to exercise participation in the EX and INT conditions was imperative in order to prevent an extreme energy deficit following the 12 h fast. Previous work has demonstrated that a large energy deficit can potentially affect insulin concentrations and appetite perception (25), and may in turn influence insulin sensitivity.
A limitation of the present study was that total PYY was measured rather than PYY3-36. Much of the previous research concerned with circulating PYY has reported total PYY levels using assays which detect both the PYY1-36 and PYY3-36 (3,26,27,28). PYY3-36 is the predominant form both in the fed and fasted states and in lean and obese subjects (29,30), thus it is possible that we may have noted different findings if we had measured PYY3-36 only. However, since both PYY1-36 and PYY3-36 are considered physiologically relevant to appetite regulation, particularly over the course of an entire day, the decision was made to measure total PYY (31,32).
In conclusion, total PYY concentration was not affected in obese individuals following either a 1 h bout of exercise or multiple short bouts of exercise over a 12-h time period. However, short bouts of exercise over the course of the day improved subjective measures of appetite; a finding which is particularly significant considering that intermittent exercise is expected to have resulted in increased energy expenditure over the SED condition. Future work should examine whether short, intermittent exercise bouts throughout the day will lead to decreased food intake over the long-term, and assist with weight management in obesity.
Acknowledgments
This project was supported in part by NIH grant R21DK063179.
Footnotes
There were no conflicts of interest for any of the authors of this manuscript.
References
- 1.McGowan BM, Bloom SR. Peptide YY and appetite control. Curr Opin Pharmacol. 2004;4(6):583–588. doi: 10.1016/j.coph.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Roth CL, Bongiovanni KD, Gohlke B, Woelfle J. Changes in dynamic insulin and gastrointestinal hormone secretion in obese children. J Pediatr Endocrinol Metab. 2010;23(12):1299–1309. doi: 10.1515/jpem.2010.204. [DOI] [PubMed] [Google Scholar]
- 3.Batterham RL, Cohen MA, Ellis SM, et al. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. 2003;349(10):941–948. doi: 10.1056/NEJMoa030204. [DOI] [PubMed] [Google Scholar]
- 4.Jebb SA, Siervo M, Fruhbeck G, Goldberg GR, Murgatroyd PR, Prentice AM. Variability of appetite control mechanisms in response to 9 weeks of progressive overfeeding in humans. Int J Obes (Lond) 2006;30(7):1160–1162. doi: 10.1038/sj.ijo.0803194. [DOI] [PubMed] [Google Scholar]
- 5.Hagobian TA, Sharoff CG, Stephens BR, et al. Effects of exercise on energy-regulating hormones and appetite in men and women. Am J Physiol Regul Integr Comp Physiol. 2009;296(2):R233–42. doi: 10.1152/ajpregu.90671.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balaquera-Cortes L, Wallman KE, Fairchild TJ, Guelfi KJ. Energy intake and appetite-related hormones following acute aerobic and resistance exercise. Appl Physiol Nutr Metab. 2011;36(6):958–966. doi: 10.1139/h11-121. [DOI] [PubMed] [Google Scholar]
- 7.Martins C, Morgan LM, Bloom SR, Robertson MD. Effects of exercise on gut peptides, energy intake, and appetite. J Endocrinol. 2007;193(2):251–258. doi: 10.1677/JOE-06-0030. [DOI] [PubMed] [Google Scholar]
- 8.Eriksen L, Dahl-Petersen I, Haugaard SB, Dela F. Comparison of the effect of multiple short-duration with single long-duration exercise sessions on glucose homeostasis in type 2 diabetes mellitus. Diabetologia. 2007;50(11):2245–2253. doi: 10.1007/s00125-007-0783-0. [DOI] [PubMed] [Google Scholar]
- 9.Ueda SY, Yoshikawa T, Katsura Y, Usui T, Fujimoto S. Comparable effects of moderate intensity exercise on changes in anorectic gut hormone levels and energy intake to high intensity exercise. J Endocrinol. 2009;203(3):357–364. doi: 10.1677/JOE-09-0190. [DOI] [PubMed] [Google Scholar]
- 10.Broom DR, Batterham RL, King JA, Stensel DJ. Influence of resistance and aerobic exercise on hunger, circulating levels of acylated ghrelin, and peptide YY in healthy males. Am J Physiol Regul Integr Comp Physiol. 2009;296(1):R29–35. doi: 10.1152/ajpregu.90706.2008. [DOI] [PubMed] [Google Scholar]
- 11.Ueda SY, Yoshikawa T, Katsura Y, Usui T, Nakao H, Fujimoto S. Changes in gut hormone levels and negative energy balance during aerobic exercise in obese young males. J Endocrinol. 2009;201(1):151–159. doi: 10.1677/JOE-08-0500. [DOI] [PubMed] [Google Scholar]
- 12.Guo YS, Singh P, Draviam E, Greeley GH, Jr, Thompson JC. Peptide YY inhibits the insulinotropic action of gastric inhibitory polypeptide. Gastroenterology. 1989;96(3):690–694. [PubMed] [Google Scholar]
- 13.Nieuwenhuizen AG, Karlsson S, Fridolf T, Ahren B. Mechanisms underlying the insulinostatic effect of peptide YY in mouse pancreatic islets. Diabetologia. 1994;37(9):871–878. doi: 10.1007/BF00400941. [DOI] [PubMed] [Google Scholar]
- 14.Burcelin R, Brunner H, Seydoux J, Thorensa B, Pedrazzini T. Increased insulin concentrations and glucose storage in neuropeptide Y Y1 receptor-deficient mice. Peptides. 2001;22(3):421–427. doi: 10.1016/s0196-9781(01)00357-6. [DOI] [PubMed] [Google Scholar]
- 15.Fields DA, Goran MI, McCrory MA. Body-composition assessment via air-displacement plethysmography in adults and children: A review. Am J Clin Nutr. 2002;75(3):453–467. doi: 10.1093/ajcn/75.3.453. [DOI] [PubMed] [Google Scholar]
- 16.Baynard T, Carhart RL, Jr, Weinstock RS, Ploutz-Snyder LL, Kanaley JA. Short-term exercise training improves aerobic capacity with no change in arterial function in obesity. Eur J Appl Physiol. 2009;107(3):299–308. doi: 10.1007/s00421-009-1126-2. [DOI] [PubMed] [Google Scholar]
- 17.Rogers PJ, Blundell JE. Effect of anorexic drugs on food intake and the microstructure of eating in human subjects. Psychopharmacology (Berl) 1979;66(2):159–165. doi: 10.1007/BF00427624. [DOI] [PubMed] [Google Scholar]
- 18.King NA, Tremblay A, Blundell JE. Effects of exercise on appetite control: implications for energy balance. Med Sci Sports Exerc. 1997;29(8):1076–1089. doi: 10.1097/00005768-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Cooper JA, Watras AC, Paton CM, Wegner FH, Adams AK, Schoeller DA. Impact of exercise and dietary fatty acid composition from a high-fat diet on markers of hunger and satiety. Appetite. 2011;56(1):171–178. doi: 10.1016/j.appet.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.King JA, Wasse LK, Ewens J, et al. Differential acylated ghrelin, peptide YY3-36, appetite, and food intake responses to equivalent energy deficits created by exercise and food restriction. J Clin Endocrinol Metab. 2011;96(4):1114–1121. doi: 10.1210/jc.2010-2735. [DOI] [PubMed] [Google Scholar]
- 21.Lyons S, Richardson M, Bishop P, Smith J, Heath H, Giesen J. Excess post-exercise oxygen consumption in untrained males: effects of intermittent durations of arm ergometry. Appl Physiol Nutr Metab. 2006;31:196–201. doi: 10.1139/h05-017. [DOI] [PubMed] [Google Scholar]
- 22.Almuzaini KS, Potteiger JA, Green SB. Effects of split exercise sessions on excess postexercise oxygen consumption and resting metabolic rate. Can J Appl Physiol. 1998;23:433–443. doi: 10.1139/h98-026. [DOI] [PubMed] [Google Scholar]
- 23.Kelly KR, Brooks LM, Solomon TP, Kashyap SR, O’Leary VB, Kirwan JP. The glucose-dependent insulinotropic polypeptide and glucose-stimulated insulin response to exercise training and diet in obesity. Am J Physiol Endocrinol Metab. 2009;296(6):E1269–1274. doi: 10.1152/ajpendo.00112.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng H, Berthoud HR. Neural systems controlling the drive to eat: Mind versus metabolism. Physiology (Bethesda) 2008;23:75–83. doi: 10.1152/physiol.00047.2007. [DOI] [PubMed] [Google Scholar]
- 25.Hagobian TA, Sharoff CG, Stephens BR, et al. Effects of exercise on energy-regulating hormones and appetite in men and women. Am J Physiol Regul Integr Comp Physiol. 2009;296:R233–42. doi: 10.1152/ajpregu.90671.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.le Roux CW, Batterham RL, Alywin SJ, et al. Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology. 2006;148:3–8. doi: 10.1210/en.2005-0972. [DOI] [PubMed] [Google Scholar]
- 27.Maier C, Reidl M, Vila G, et al. Cholinergic regulation of ghrelin and PYY release may be impaired in obesity. Diabetes. 2008;57:2332–2340. doi: 10.2337/db07-0758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martins C, Robertson MD, Morgan LM. Effects of exercise and restrained eating behaviour on appetite control. Proc Nutr Soc. 2008;67:28–41. doi: 10.1017/S0029665108005995. [DOI] [PubMed] [Google Scholar]
- 29.Batterham RL, Heffron H, Kapoor S, et al. Critical role for peptide YY in protein-mediated satiation and body weight regulation. Cell Metab. 2006;4:223–233. doi: 10.1016/j.cmet.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Korner J, Inabet W, Conwell IM, et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity. 2006;14:1553–1561. doi: 10.1038/oby.2006.179. [DOI] [PubMed] [Google Scholar]
- 31.Hill BR, DeSouza MJ, Williams NI. Characterization of the diurnal rhythm of peptide YY and its association with energy balance parameters in normal-weight premenopausal women. Am J Physiol Endocrinol Metab. 2011;301:E409–E415. doi: 10.1152/ajpendo.00171.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sloth B, Holst JJ, Flint A, Gregersen NT, Astrup A. Effects of PYY1-36 and PYY3-36 on appetite, energy intake, energy expenditure, glucose and fat metabolism in obese and lean subjects. Am J Physiol Endocrinol Metab. 2006;292:E1062–E1068. doi: 10.1152/ajpendo.00450.2006. [DOI] [PubMed] [Google Scholar]