Abstract
Background and Aims
Delayed bleeding after lower endoscopy and polypectomy can cause significant morbidity. One strategy to reduce bleeding is to place an endoscopic clip on the polypectomy site. We used decision analysis to investigate the cost effectiveness of routine clip placement after colon polypectomy.
Methods
Probabilities and plausible ranges were obtained from the literature, and a decision analysis was conducted using TreeAge Pro 2011 (TreeAge Software, Williamstown, MA). Our cost-effectiveness threshold was an incremental cost effectiveness ratio of $100,000 per quality adjusted life year. The reference case was a 50 year old patient who had a single 1.0–1.5 cm polyp removed during colonoscopy. We estimated post-polypectomy bleeding rates for patients receiving no medications, those with planned resumption of anti-platelet therapy (nonaspirin), or those receiving anticoagulation therapy after polypectomy. We performed several sensitivity analyses, varying the cost of a clip and hospitalization, number of clips placed, clip effectiveness in reducing post-polypectomy bleeding, reduction in patient utility days related to gastrointestinal bleeding, and probability of harm from clip placement.
Results
Based on the reference case, when patients did not receive anti-coagulation therapy, clip placement was not cost effective. However for patients who did receive anticoagulation and anti-platelet therapies, prophylactic clip placement was a cost-effective strategy. The cost-effectiveness of a prophylactic clip strategy was sensitive to the costs of clips and hospitalization, number of clips placed, and clip effectiveness.
Conclusions
Placement of a prophylactic endoscopic clip after polypectomy appears to be a cost-effective strategy for patients who receive anti-platelet or anticoagulation therapy. This approach should be studied in a controlled trial.
Keywords: resection, endoclip, ICER, QALY
INTRODUCTION
Lower endoscopy (colonoscopy or flexible sigmoidoscopy) is a recommended screening tool for colorectal cancer and adenomatous polyps.1 During endoscopy, up to 40% of patients will have detectable adenomatous polyps.2, 3 Removal of adenomatous polyps is associated with decreased colorectal cancer incidence and mortality.4 However, polypectomy has numerous risks, including post-polypectomy electrocoagulation syndrome, colonic perforation, and bleeding (immediate and delayed).2, 5 The estimated serious complication rate after polypectomy ranges from 0.01%–0.1%, depending on polyp size, shape, and location.6–8 Large (> 1 cm) polyps have higher risk of immediate and delayed bleeding due to an increased vascular supply.7 Broader based polyps have higher risk of perforation due to a larger mucosal defect associated with resection.9, 10
Immediate bleeding and perforation are typically recognized at the time of endoscopy and can be treated acutely. However, delayed post-polypectomy bleeding occurs up to two weeks after endoscopic polypectomy and can lead to hospitalization, transfusion, and need for repeat endoscopy to identify and treat the bleeding site. Hospitalization for post-polypectomy bleeding incurs significant cost and impacts patients’ quality of life in the short-term. In addition, the risk of delayed bleeding is higher in those patients required to take anti-platelet therapy or anticoagulant therapy, and often these medications are restarted soon after lower endoscopy due to risks associated with stopping these medications.10–12
Endoscopic clips appear to be effective in bleeding prevention, however they are costly and there are no large studies or randomized controlled trials to address the cost effectiveness of routine clip placement after polypectomy. Studies have shown that endoscopic clips do not appear to significantly reduce bleeding after removal of small polyps (<1 cm in size).13, 14 Limited data from several small published studies studies presented only in abstract form have shown that prophylactic endoscopic clip placement is effective in significantly reducing the risk of delayed post-polypectomy bleeding after removal of larger polyps (1.0–4.0 cm), with reported reduction in post-polypectomy bleeding risk between 50–100%.15–19 The reduction in bleeding risk also appears to be present in patients on anti-platelet or anti-coagulation therapy at the time of polypectomy.20 In addition, clips are widely used with one study showing that more than 20% of endoscopists routinely use endoscopic clips in an attempt to decrease post-polypectomy bleeding.21 However, societal guidelines do not make any firm recommendations on routine placement of endoscopic clips after polypectomy.22, 23
In this study we aimed to explore the factors that would influence cost-effectiveness of a routine strategy of endoscopic clip placement after polypectomy by employing a decision model for patients undergoing screening colonoscopy. We also examined the differential cost-effectiveness of a clip strategy on patients expected to resume anti-platelet therapy (clopidogrel) or full anticoagulation (warfarin) therapy after polypectomy.
METHODS
Case Definition
The guidelines published by the Panel on Cost-Effectiveness in Health and Medicine were used to establish a reference case for decision analysis.24 The reference case was a 50 year-old patient undergoing index lower endoscopy with polypectomy (blended coagulation-cut current) for a 1.0–1.5 cm polypoid lesion (Paris Classification Type O-Ip or O-Is)25 without immediate post-polypectomy bleeding. This polyp size was chosen because 1 to 2 clips could be effectively used to close the defect left at the polypectomy site.26
Decision Model
A model of the reference case scenario was constructed using decision analysis software (TreeAge Pro 2011; TreeAge Software, Williamstown, MA). The complete decision tree is shown in Figure 1. Alternative outcome pathways were created for polypectomy with and without endoscopic clip placement. In accordance with PRISMA guidelines, the systematic review of the published literature was conducted to determine the rate of delayed post-polypectomy bleeding and clip effectiveness in reducing bleeding. For the systematic review of articles reporting on delayed post-polypectomy bleeding, we conducted a search of the MEDLINE and EMBASE databases, using the MeSH terms, “delayed” AND “post-polypectomy” and “bleeding.” The initial search revealed 16 articles after thorough review of the articles and their bibliographies, 7 articles were included in the analysis. The articles were further stratified by whether they reported on bleeding risk for patients on anticoagulant or anti-platelet (non-aspirin) therapy. The systematic review to determine the effectiveness of clips was conducted by a search of the MEDLINE and EMBASE databases, using the MeSH terms “clip” and “endoscopic” and “bleeding” and “polyp.” The initial search revealed 63 articles and after individual review, 3 articles were included in the analysis. In order to increase the number of data sources for the effectiveness of clips, we also searched meeting proceedings for relevant sources and included two additional abstracts in our analysis.
Fig. 1.

Decision tree for prophylactic clip placement
The event pathways and probabilities used in the model were aggregated based upon our systematic literature review. (Table 1). Cost data were in 2011 US dollars and obtained from institutional data based upon the Centers for Medicare and Medicaid Services reimbursement. Clip cost was $155 and was obtained from institutional data. The optimal strategy was defined as the strategy that produced the greatest quality-adjusted life expectancy that did not exceed an incremental cost-effectiveness ratio (ICER) of $100,000 per quality-adjusted life year (QALY). Costs were calculated from the perspective of the medical system (3rd party payor and medical facility). The time horizon for the analysis was 6 months. The model was adjusted to consider cases of patients who would resume full dose anticoagulation therapy (e.g. warfarin, low molecular weight heparin) or antiplatelet medication (e.g. clopidogrel). Sensitivity analyses were performed across varying bleeding rates (without clip placement) and the following: reduction in bleeding rate, cost of hospitalization, cost of clip, number of clips placed, the utility reduction in days, and probability of harm from clip placement.
Table 1.
Estimates of the values of the variables extracted from the literature and used in the analysis
| Variables considered | Base case | Plausible range | References |
|---|---|---|---|
|
| |||
| Delayed post-polypectomy risk | |||
| No anticoagulation | 0.64% | 0.2%–1.2% | 30–34 |
| Anti-platelet therapy (Non-Aspirin) | 2.5% | 0.85–5.8% | 30, 34, 35 |
| Anticoagulation therapy | 3.4% | 1.4–6.8% | 32, 33, 35, 36 |
|
| |||
| Relative risk reduction of delayed post-polypectomy bleeding with clip placement | 82% | 100%-50% | 16–19, 28 |
|
| |||
| Clips placed | 1 | 1–6 | |
|
| |||
| Cost of clip | $155 | ||
|
| |||
| Cost of hospitalization for post-polypectomy bleeding | $9,150 | $5,000–$25,000 | |
Model Assumptions
We assumed all significant delayed post-polypectomy bleeding resulted in patient hospitalization. Hospitalization for post-polypectomy bleeding was assumed to reduce quality-adjusted life expectancy by one day. In the base case scenario, endoscopic placement of one prophylactic clip was assumed to provide 82% reduction in the risk of delayed post-polypectomy bleeding.
RESULTS
Reference Case
The reference case results are summarized in Table 2 and reflect prophylactic clip placement for a patient undergoing polypectomy not on anti-platelet or anti-coagulation therapy. The reference case bleeding rate was set at 0.64%, based on the mean values reported in the existing literature. Prophylactic clip placement for the reference case strategy was not cost effective. It had an expected incremental cost of $106.98 for an added effectiveness of .000014 QALYs. The ICER for this strategy was approximately $7.4 million USD.
Table 2.
Reference Case Results
| Strategy | Cost (USD) | Incremental Cost (USD) | Effectiveness (QALYs) | Incremental Effectiveness | ICER (USD) |
|---|---|---|---|---|---|
| No Clip Placement | $58.56 | - | 0.499982 | - | - |
| Clip Placement | $165.54 | $106.98 | 0.499997 | 0.000014 | $7,445,643 |
USD- United States dollars; QALYs – quality life years; ICER – incremental cost-effectiveness
Sensitivity Analysis
Prophylactic clip placement
Due to the wide variation in bleeding rates reported in the literature depending on anti-platelet/anti-coagulation therapy (Table 1), sensitivity analyses were performed to further evaluate the cost effectiveness of prophylactic clip placement. As shown in Figure 2, prophylactic clip placement was not cost effective until the risk of post-polypectomy bleeding increased to 2.01%; prophylactic clip placement was cost saving when the probability was 2.07%. Figure 2 also illustrates that the cost-effectiveness of prophylactic clip placement is highly sensitive to the probability of post-polypectomy bleeding rates, with a wide range of ICER values over a bleeding rate from 0–3%. For example, the ICER increases significantly (to over $3 million) as the probability of bleeding decreases to 1.0%.
Fig. 2.

Sensitivity Analysis on Probability of Post-Polypectomy Bleed
Two-way sensitivity analyses
Two-way sensitivity analysis demonstrated that the decision model was sensitive to the simultaneous variation of the initial probability of post-polypectomy bleeding and 5 independent factors: 1) clip effectiveness in reducing bleeding rate, 2) cost of GI bleed/hospitalization, 3) cost of clips, 4) number of clips placed, and 5) theoretical risk of harm from clip placement. Figure 3 shows the model is sensitive to simultaneous variation in the effectiveness of clip placement and bleeding rate without clip placement. Even if clip placement is 100% effective at reducing the bleeding rate, this strategy is not cost effective in the reference case (bleeding rate of 0.64%). Conversely, clip placement is favorable in patients on anti-coagulation and anti-platelet therapy, assuming 100% effectiveness. In fact, for patients on anti-platelet therapy, clip placement is favorable when clip associated bleeding risk reduction is ~70% or greater. The clip placement strategy need only be 50% effective (or greater) in reducing the bleeding risk to be cost effective in patients on anti-coagulation and with comparable bleeding rates.
Fig. 3.
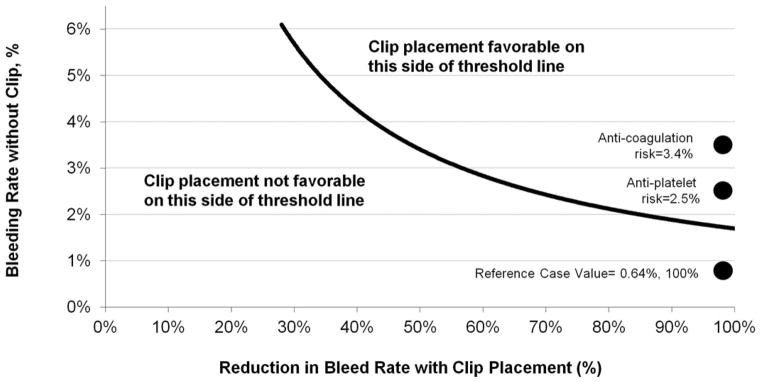
Two-Way Sensitivity Analysis of Reduction in Bleed Rate with Clip and Bleeding Rate
Figure 4a illustrates that prophylactic clip placement becomes favorable when the probability of bleeding is sufficiently high in relation to the cost of hospitalization. Prophylactic clip placement in the reference case strategy is not favorable based on the reference cost of hospitalization ($9,150). However, clip placement dominates for those patients on anti-platelet or anticoagulation therapy based on mean reported bleeding rates (Table 1). If the cost of hospitalization is low (<$5000), prophylactic clip placement is favorable only at high bleeding rates.
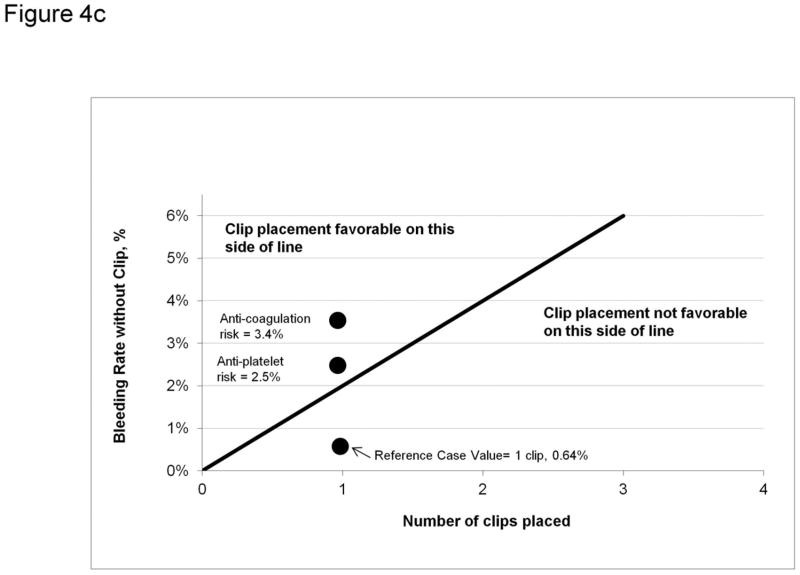
Fig. 4.
Fig. 4a: Two-Way Sensitivity Analysis of Cost of GI Bleed and Bleeding Rate; Fig. 4b: Two-Way Sensitivity Analysis of Cost of Clip and Bleeding Rate; Fig. 4c: Two-Way Sensitivity Analysis on Number of Clips Placed and Bleeding Rate; Fig 4d: Two-Way Sensitivity Analysis of Utility Reduction for Hospitalization and Bleeding Rate; Fig. 4e: Two Way Sensitivity Analysis on Number of Clips Placed and Probability of harm from clip
Based on current costs of prophylactic clips and reference case bleeding rates, prophylactic clip placement is not favorable based on reference clip cost and bleeding rate values (Figure 4b). Similarly, as the cost of clips increases, a no clip strategy dominates even at bleeding rates as high as 3%. However, based on listed current clip costs, prophylactic clip placement is favorable for those patients on anti-platelet and anticoagulation therapy.
Figure 4c demonstrates that placing more than one prophylactic clip is only cost effective at very high bleeding rates (>3.5%). Placing more than 2 clips is not favorable based on all mean bleeding rates reported. Placing one prophylactic clip in patients on anti-platelet/anticoagulation therapy appears cost effective. However, the use of 2 clips is equivocal and not favorable in those patients on anti-coagulation and anti-platelet therapy, respectively, based on mean bleeding rates reported.
An exploratory analysis was also performed to evaluate the effect of utility reduction (days) and probability of harm from the clip placement. As shown in Figure 4d, the model is fairly insensitive to further reduction in utility, up to 20 days of hospitalization. As there are no published estimates on the probability of harm from clip placement, we conservatively estimated a maximum harm of 1.0% (~equal to risk of bleeding). Overall, the model was relatively insensitive to the range of harm probabilities from 0–1% (Figure 4e). However, if the probability of harm from clip placement exceeded 0.5%, clip placement for patients on anti-platelet therapy ceased to be cost-effective.
DISCUSSION
Delayed post-polypectomy bleeding is a morbid and costly consequence after lower endoscopic removal of polyps. Endoscopic clip placement during polypectomy is employed to prevent delayed post-polypectomy bleeding. While some advocate for routine clip placement when removing polyps27, this is the first report on the strategy’s cost-effectiveness. Our decision model showed that the cost-effectiveness of clip placement is highly sensitive to bleeding rates after polypectomy. For patients on neither anti-coagulation nor anti-platelet therapy, routine clip placement after polypectomy of a 1–1.5 cm polyp is not a cost-effective strategy. However, if patients are expected to resume anticoagulation or anti-platelet therapy after colonoscopy, routine clip placement appears to be a cost effective preventative strategy. Our sensitivity analysis showed that the cost effectiveness of clip placement is sensitive to the cost of a hospitalization for a lower GI bleed, cost of clip, number of clips placed, and effectiveness of the clip in reducing post-polypectomy bleeding. However, further controlled data on the efficacy of clips in preventing bleeding is needed before specific recommendations on clip placement can be made. Our analysis does allow clinicians to assess their own post-polypectomy bleeding rates in addition to other factors, such as clip costs and cost of hospitalization, to determine whether routine clip placement may be cost-effective in their practice.
There have been no large randomized trials to date assessing a clip strategy, so it is unclear how effective a strategy of clip placement would be in prevention of post-polypectomy bleeding. Several small studies found that clips are effective in preventing post-polypectomy bleeding of larger polyps. 16–19, 28 We also modeled scenarios where clip effectiveness varies between 50–100% (Figure 6), which corresponds with a decreasing cost effectiveness of clip placement. The risk of harm from clip placement is likely very low, and our model was fairly insensitive to this variable.
Our study has several strengths and limitations. We were comprehensive in our analysis of the literature to find differential bleed rates for the three different groups of patients. However, our data were derived from a small number of studies, which suffers from reporting bias. In addition, we included data published only in abstract form. We assumed patient quality of life was very poor if hospitalized for a post-polypectomy bleed, however we have no psychometric data to back this assumption. Conversely, we may have underestimated the cost of hospitalization as we assumed a 1 day hospitalization in patients with postpolypectomy bleed. We also did not model other strategies alone or in combination with clip placement that may be effective in prevention of post-polypectomy bleeding, such as epinephrine injection or endoscopic ligature placement.28 Our cost data were obtained from institutional records, however we did perform a sensitivity analysis to determine the effect of varying the hospital cost on cost effectiveness of a clip strategy (Figure 4a).
Certainly there are other factors that may predispose to post-polypectomy bleeding. Evidence suggests that right-sided polyps have significantly higher risk (OR: 4.03–4.67) of bleeding and perforation when compared to left sided polyps.7, 29 Therefore it may be cost effective to place clips on large right-sided polyps to prevent bleeding, however this warrants further study. Additionally the role of aspirin in increasing the risk of delayed bleeding is controversial, 11 thus we did not include it as a risk factor in the model.
In conclusion, this exploratory analysis examined the cost-effectiveness of a strategy of placement of prophylactic clips in the prevention of post-polypectomy bleeding, based upon the published post-polypectomy bleeding rates. Prophylactic clip strategy is cost-effective in those patients on anti-platelet or anti-coagulation therapy. The cost-effectiveness of a prophylactic clip strategy is sensitive to the clip effectiveness, cost of hospitalization, clip cost, and number of clips placed. In situations where post-polypectomy bleeding is high and clip placement significantly reduces bleeding risk, prophylactic clip placement is cost effective in preventing delayed post-polypectomy bleeding. The clinical and cost effectiveness of this strategy warrants study in a larger randomized trial.
Acknowledgments
Grant Support: Neehar D. Parikh’s preparation of this article was supported in part by grant 5T32DK077662-04 from the National Institute of Diabetes and Digestive and Kidney Diseases (PI: Michael Abecassis MD MBA). Kyle Zanocco and Andrew Gawron’s preparation of this article was supported in part by the Center for Healthcare studies under an institutional award from the Agency for Healthcare Research and Quality, T-32 HS 000078 (PI: Jane L. Holl, MD MPH).
Abbreviations
- ICER
Incremental cost-effectiveness ratio
- QALY
quality adjusted life year
- USD
United States dollar
Footnotes
Disclosures: The authors have no disclosures or conflicts of interest
Author Contributions:
Neehar Parikh - study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript
Kyle Zanocco - statistical analysis; drafting of the manuscript
Rajesh Keswani - critical revision of the manuscript for important intellectual content
Andrew Gawron - study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Winawer SJ, Krabshuis J, Lambert R, et al. Cascade colorectal cancer screening guidelines: a global conceptual model. J Clin Gastroenterol. 2011;45(4):297–300. doi: 10.1097/MCG.0b013e3182098e07. Epub 2011/02/09. [DOI] [PubMed] [Google Scholar]
- 2.Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. The American journal of gastroenterology. 2006;101(4):873–85. doi: 10.1111/j.1572-0241.2006.00673.x. Epub 2006/04/26. [DOI] [PubMed] [Google Scholar]
- 3.Munroe CA, Lee P, Copland A, et al. A tandem colonoscopy study of adenoma miss rates during endoscopic training: a venture into uncharted territory. Gastrointest Endosc. 2012;75(3):561–7. doi: 10.1016/j.gie.2011.11.037. Epub 2012/02/22. [DOI] [PubMed] [Google Scholar]
- 4.Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366(8):687–96. doi: 10.1056/NEJMoa1100370. Epub 2012/02/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S, Saunders BP, Fraser C, et al. The first 3 years of national bowel cancer screening at a single UK tertiary centre. Colorectal Dis. 2012;14(2):166–73. doi: 10.1111/j.1463-1318.2011.02567.x. Epub 2011/06/22. [DOI] [PubMed] [Google Scholar]
- 6.Rutter CM, Johnson E, Miglioretti DL, et al. Adverse events after screening and follow-up colonoscopy. Cancer Causes Control. 2012;23(2):289–96. doi: 10.1007/s10552-011-9878-5. Epub 2011/11/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buddingh KT, Herngreen T, Haringsma J, et al. Location in the right hemi-colon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am J Gastroenterol. 2011;106(6):1119–24. doi: 10.1038/ajg.2010.507. Epub 2011/01/27. [DOI] [PubMed] [Google Scholar]
- 8.Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135(6):1899–906. 906, e1. doi: 10.1053/j.gastro.2008.08.058. Epub 2008/10/22. [DOI] [PubMed] [Google Scholar]
- 9.Warren JL, Klabunde CN, Mariotto AB, et al. Adverse events after outpatient colonoscopy in the Medicare population. Ann Intern Med. 2009;150(12):849–57. W152. doi: 10.7326/0003-4819-150-12-200906160-00008. Epub 2009/06/17. [DOI] [PubMed] [Google Scholar]
- 10.Shiffman ML, Farrel MT, Yee YS. Risk of bleeding after endoscopic biopsy or polypectomy in patients taking aspirin or other NSAIDS. Gastrointest Endosc. 1994;40(4):458–62. doi: 10.1016/s0016-5107(94)70210-1. Epub 1994/07/01. [DOI] [PubMed] [Google Scholar]
- 11.Hui AJ, Wong RM, Ching JY, et al. Risk of colonoscopic polypectomy bleeding with anticoagulants and antiplatelet agents: analysis of 1657 cases. Gastrointest Endosc. 2004;59(1):44–8. doi: 10.1016/s0016-5107(03)02307-1. Epub 2004/01/15. [DOI] [PubMed] [Google Scholar]
- 12.Anderson MA, Ben-Menachem T, Gan SI, et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc. 2009;70(6):1060–70. doi: 10.1016/j.gie.2009.09.040. Epub 2009/11/06. [DOI] [PubMed] [Google Scholar]
- 13.Shioji K, Suzuki Y, Kobayashi M, et al. Prophylactic clip application does not decrease delayed bleeding after colonoscopic polypectomy. Gastrointest Endosc. 2003;57(6):691–4. doi: 10.1067/mge.2003.193. Epub 2003/04/24. [DOI] [PubMed] [Google Scholar]
- 14.Iqbal R, Lee I, Uddin FS, et al. Su1333 The Prophylactic Placement of Hemoclips to Prevent Delayed Post Polypectomy Bleeding: An Unnecessary Practice? Gastrointest Endosc. 2012;75(4):AB296–AB7. doi: 10.1007/s10620-014-3055-0. [DOI] [PubMed] [Google Scholar]
- 15.Boo SJ, Byeon JS, Park SY, et al. Clipping for the prevention of immediate bleeding after polypectomy of pedunculated polyps: a pilot study. Clin Endosc. 2012;45(1):84–8. doi: 10.5946/ce.2012.45.1.84. Epub 2012/06/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gimeno-Garcia AZ, de Ganzo ZA, Sosa AJ, et al. Incidence and predictors of postpolypectomy bleeding in colorectal polyps larger than 10 mm. Eur J Gastroenterol Hepatol. 2012;24(5):520–6. doi: 10.1097/MEG.0b013e328350fcdc. Epub 2012/04/03. [DOI] [PubMed] [Google Scholar]
- 17.Liaquat H, Rohn EA, Rex DK. Su1481 Large Sessile Colorectal Polyps: Reduction in Delayed Bleeding With Prophylactic Clipping. Gastrointest Endosc. 2012;75(4):AB348. [Google Scholar]
- 18.Sobrino-Faya M, Martinez S, Gomez Balado M, et al. Clips for the prevention and treatment of postpolypectomy bleeding (hemoclips in polypectomy) Rev Esp Enferm Dig. 2002;94(8):457–62. Epub 2002/12/19. [PubMed] [Google Scholar]
- 19.Ji J-S, Lee S-W. 525 Comparison of Prophylactic Clip and Detachable Snare for the Prevention of Postpolypectomy Bleeding for the Large Pedunculated Colonic Polyps: A Prospective, Randomized Study. Gastrointest Endosc. 2011;73(4):AB134. [Google Scholar]
- 20.Howell DA, Eswaran SL, Loew BJ, et al. Use of Hemostatic Clips in Patients Undergoing Colonoscopy in the Setting of Coumadin Anticoagulation Therapy. Gastrointest Endosc. 2006;63(5):AB98. [Google Scholar]
- 21.Singh N, Harrison M, Rex DK. A survey of colonoscopic polypectomy practices among clinical gastroenterologists. Gastrointest Endosc. 2004;60(3):414–8. doi: 10.1016/s0016-5107(04)01808-5. Epub 2004/08/28. [DOI] [PubMed] [Google Scholar]
- 22.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–95. doi: 10.1053/j.gastro.2008.02.002. Epub 2008/04/04. [DOI] [PubMed] [Google Scholar]
- 23.Fisher DA, Maple JT, Ben-Menachem T, et al. Complications of colonoscopy. Gastrointest Endosc. 2011;74(4):745–52. doi: 10.1016/j.gie.2011.07.025. Epub 2011/09/29. [DOI] [PubMed] [Google Scholar]
- 24.Gold MR. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. p. xxiii.p. 425. [Google Scholar]
- 25.The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(6 Suppl):S3–43. doi: 10.1016/s0016-5107(03)02159-x. Epub 2003/12/04. [DOI] [PubMed] [Google Scholar]
- 26.Turner J, Dolwani S, Green J. The Role of Prophylactic Clips in Endoscopic Mucosal Resection (EMR) Gastrointest Endosc. 2009;69(5):AB209. [Google Scholar]
- 27.Nagri S, Anand S. Prophylactic clip application should be the standard of care to prevent postpolypectomy bleeding. Gastrointest Endosc. 2007;65(1):182. doi: 10.1016/j.gie.2006.07.018. author reply 3. Epub 2006/12/23. [DOI] [PubMed] [Google Scholar]
- 28.Kouklakis G, Mpoumponaris A, Gatopoulou A, et al. Endoscopic resection of large pedunculated colonic polyps and risk of postpolypectomy bleeding with adrenaline injection versus endoloop and hemoclip: a prospective, randomized study. Surg Endosc. 2009;23(12):2732–7. doi: 10.1007/s00464-009-0478-3. Epub 2009/05/12. [DOI] [PubMed] [Google Scholar]
- 29.Metz AJ, Bourke MJ, Moss A, et al. Factors that predict bleeding following endoscopic mucosal resection of large colonic lesions. Endoscopy. 2011;43(6):506–11. doi: 10.1055/s-0030-1256346. Epub 2011/05/28. [DOI] [PubMed] [Google Scholar]
- 30.Singh M, Mehta N, Murthy UK, et al. Postpolypectomy bleeding in patients undergoing colonoscopy on uninterrupted clopidogrel therapy. Gastrointest Endosc. 2010;71(6):998–1005. doi: 10.1016/j.gie.2009.11.022. Epub 2010/03/17. [DOI] [PubMed] [Google Scholar]
- 31.Watabe H, Yamaji Y, Okamoto M, et al. Risk assessment for delayed hemorrhagic complication of colonic polypectomy: polyp-related factors and patient-related factors. Gastrointest Endosc. 2006;64(1):73–8. doi: 10.1016/j.gie.2006.02.054. Epub 2006/07/04. [DOI] [PubMed] [Google Scholar]
- 32.Witt DM, Delate T, McCool KH, et al. Incidence and predictors of bleeding or thrombosis after polypectomy in patients receiving and not receiving anticoagulation therapy. J Thromb Haemost. 2009;7(12):1982–9. doi: 10.1111/j.1538-7836.2009.03598.x. Epub 2009/09/02. [DOI] [PubMed] [Google Scholar]
- 33.Sawhney MS, Salfiti N, Nelson DB, et al. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy. 2008;40(2):115–9. doi: 10.1055/s-2007-966959. Epub 2008/02/07. [DOI] [PubMed] [Google Scholar]
- 34.Feagins LA, Uddin FS, Davila RE, et al. The rate of post-polypectomy bleeding for patients on uninterrupted clopidogrel therapy during elective colonoscopy is acceptably low. Dig Dis Sci. 2011;56(9):2631–8. doi: 10.1007/s10620-011-1682-2. Epub 2011/04/02. [DOI] [PubMed] [Google Scholar]
- 35.Khubchandani IT, Heyrosa MG, Thekkeurumbil SV. Optimal timing of anticoagulation pre- and post-colonoscopy with polypectomy. Tech Coloproctol. 2011;15(2):185–9. doi: 10.1007/s10151-010-0668-y. Epub 2011/03/25. [DOI] [PubMed] [Google Scholar]
- 36.Gerson LB, Michaels L, Ullah N, et al. Adverse events associated with anticoagulation therapy in the periendoscopic period. Gastrointest Endosc. 2010;71(7):1211–7. e2. doi: 10.1016/j.gie.2009.12.054. Epub 2010/07/06. [DOI] [PMC free article] [PubMed] [Google Scholar]