Abstract
OBJECTIVE
Many studies of diabetes have examined risk factors at the time of diabetes diagnosis instead of considering the lifetime burden of adverse risk factor levels. We examined the 30-year cardiovascular disease (CVD) risk factor burden that participants have up to the time of diabetes diagnosis.
RESEARCH DESIGN AND METHODS
Among participants free of CVD, incident diabetes cases (fasting plasma glucose ≥126 mg/dL or treatment) occurring at examinations 2 through 8 (1979–2008) of the Framingham Heart Study Offspring cohort were age- and sex-matched 1:2 to controls. CVD risk factors (hypertension, high LDL cholesterol, low HDL cholesterol, high triglycerides, obesity) were measured at the time of diabetes diagnosis and at time points 10, 20, and 30 years prior. Conditional logistic regression was used to compare risk factor levels at each time point between diabetes cases and controls.
RESULTS
We identified 525 participants with new-onset diabetes who were matched to 1,049 controls (mean age, 60 years; 40% women). Compared with those without diabetes, individuals who eventually developed diabetes had higher levels of hypertension (odds ratio [OR], 2.2; P = 0.003), high LDL (OR, 1.5; P = 0.04), low HDL (OR, 2.1; P = 0.0001), high triglycerides (OR, 1.7; P = 0.04), and obesity (OR, 3.3; P < 0.0001) at time points 30 years before diabetes diagnosis. After further adjustment for BMI, the ORs for hypertension (OR, 1.9; P = 0.02) and low HDL (OR, 1.7; P = 0.01) remained statistically significant.
CONCLUSIONS
CVD risk factors are increased up to 30 years before diagnosis of diabetes. These findings highlight the importance of a life course approach to CVD risk factor identification among individuals at risk for diabetes.
Many studies of diabetes have focused on cardiovascular disease (CVD) risk factors at the time of diabetes diagnosis. However, it is likely that CVD risk factors that accompany diabetes, including obesity, hypertension, and dyslipidemia, are increased decades before the clinical onset of diabetes. Two previous studies have suggested that individuals who develop diabetes may have increased CVD risk factor burden up to 15 years before their diabetes diagnosis, relative to those who do not have development of diabetes (1,2) However, one limitation of these studies is that 15 years before diabetes diagnosis may not be a long enough time range to capture the early middle-age period when risk factor intervention might be more feasible.
A better understanding of the life-long risk factor burden that participants bear before the time of diabetes diagnosis can enable us to identify those at greatest risk for ultimate development of CVD. Thus, the objective of our study was to examine CVD risk factor burden during the time period of up to 30 years before diabetes diagnosis among individuals who did and did not develop diabetes.
RESEARCH DESIGN AND METHODS
Study sample
The study sample for this project was derived from individuals participating in the Framingham Heart Study (3–6). The Framingham Heart Study started in 1948 with the enrollment of 5,209 participants, aged 28–62 years, into the Original cohort (3,4). The Offspring cohort was initiated in 1971 with the enrollment of 5,124 offspring of the Original cohort participants and their spouses (5). Individuals in the Offspring cohort underwent medical examinations approximately every 4 years. Written informed consent was provided by all of the participants and the study has been approved by the Boston University Medical Center Institutional Review Board.
The study was conducted using a prospective nested case-control design. Cases were defined as any individual with newly diagnosed type 2 diabetes at Offspring examinations 2 through 8. Each diabetes case was matched to two controls (if available) by sex and 2-year age group at the study examination at which the case was diagnosed with diabetes. Controls were selected using risk set sampling, in which all individuals who did not have diabetes at the time the case received diagnosis were eligible for selection (7,8). Using this method, individuals who were controls during the earlier time periods were eligible to become cases at subsequent examinations. Cases with prevalent CVD at the time of diabetes diagnosis and controls who had prevalent CVD at the time they were matched to a case were excluded, because our ultimate goal was to identify individuals with future risk of CVD. Type 2 diabetes was defined as having a fasting plasma glucose ≥126 mg/dL or treatment with insulin or an oral hypoglycemic agent (9). For one case, there was only one available control that met the matching criteria, resulting in a final sample size of 525 cases and 1,029 controls.
CVD risk factor measurements
The following CVD risk factors were measured during each of the eight examination cycles: systolic blood pressure; diastolic blood pressure; LDL cholesterol; HDL cholesterol; triglycerides; and BMI. For the present analysis, CVD risk factor measurements were obtained at the time of diabetes diagnosis and at time points 10, 20, and 30 years previously, when available. The risk factor measurement during the examination closest to each of the time points was selected.
Systolic blood pressure and diastolic blood pressure were measured twice by a study physician and the average of the two measurements was taken. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or current use of antihypertensive treatment. HDL cholesterol and triglycerides were measured after an overnight fast. High LDL cholesterol was defined as LDL level ≥130 mg/dL or treatment with a lipid-lowering medication. Low HDL was defined as HDL <40 mg/dL for men and <50 mg/dL for women. A high triglyceride level was defined as a measurement of ≥150 mg/dL or treatment with a lipid-lowering medication. Use of antihypertensive treatment or lipid-lowering medication was self-reported at each examination. Hypertension control was defined as the proportion of participants with hypertension who had blood pressure <140/90 mmHg. LDL control was defined as the proportion of participants with high LDL cholesterol who had LDL levels <130 mg/dL. Height and weight were measured using standardized protocols. The BMI was calculated by dividing weight in kilograms by the square of height in meters. Obesity was defined as having a BMI ≥30 kg/m2.
Statistical analysis
Conditional logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals for the association between each CVD risk factor and future diabetes status at each point in time. The primary model accounted for the age and sex matching. All models were additionally adjusted for BMI. Conditional logistic regression also was used to calculate P values for comparisons between the diabetes case and control groups to formally test differences in risk factors. All analyses were conducted using SAS 9.2 (Cary, NC). P < 0.05 was considered statistically significant.
RESULTS
A total of 525 diabetes cases and 1,049 age- and sex-matched controls were derived from examinations 2 through 8 (1979–2005). Of these study participants, 516 cases and 1,030 controls had risk factor measurements available 10 years before diabetes diagnosis, 417 cases and 835 controls had measurements available 20 years before diabetes diagnosis, and 176 cases and 350 controls had measurements available 30 years before diabetes diagnosis.
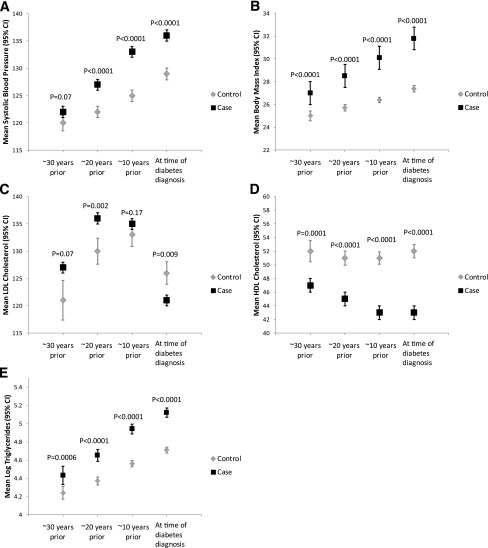
Characteristics of the diabetes cases and controls are presented in Table 1. Overall, at the time of diabetes diagnosis, cases had higher blood pressure, triglycerides, and BMI, and had lower LDL cholesterol and HDL cholesterol than the controls. Cases also had a higher prevalence of lipid and hypertension treatment than the controls. At time points 10, 20, and 30 years before diabetes diagnosis, the cases had higher levels of blood pressure, triglycerides, and BMI, and had lower levels of HDL cholesterol than the controls. (Table 1 and Fig. 1) The cases also had higher levels of LDL cholesterol than the controls. Levels of treatment for hypertension and lipids also were higher for the cases at all time points before diabetes diagnosis.
Table 1.
Comparison of risk factor levels between diabetes cases and controls over time in the Framingham Heart Study
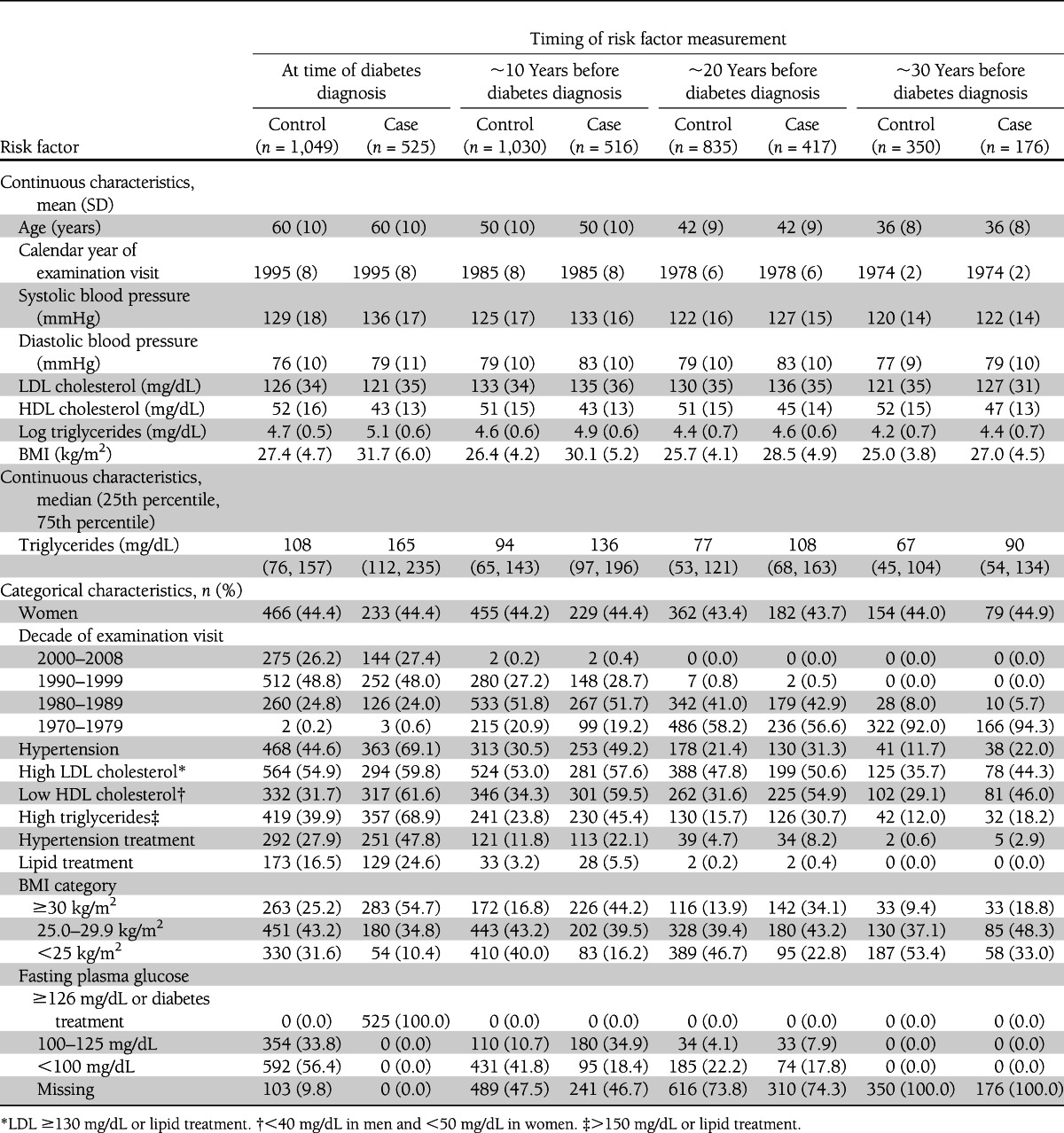
Figure 1.
Comparison of mean systolic blood pressure (A), BMI (B), LDL cholesterol (C), HDL cholesterol (D), and triglycerides (E) between diabetes cases and matched controls at time points before diabetes diagnosis.
Table 2 shows the logistic regression model results for the categorical CVD risk factors. At the time of diabetes diagnosis, cases were more likely to have hypertension, high LDL cholesterol, low HDL cholesterol, high triglycerides, obesity, hypertension treatment, and lipid treatment as compared with the controls after adjustment for age, sex, and calendar year of diabetes diagnosis. For example, individuals with newly diagnosed diabetes had a three-fold increased odds of having hypertension compared with those without diabetes. After further adjustment for BMI, individuals with newly diagnosed diabetes had an approximate two-fold increased odds of having hypertension compared with those who did not develop diabetes. For all risk factors except high LDL cholesterol, further adjustment for BMI measured at the time of diabetes diagnosis resulted in a statistically significant, although attenuated, OR.
Table 2.
ORs of diabetes by categorical CVD risk factors in the Framingham Heart Study
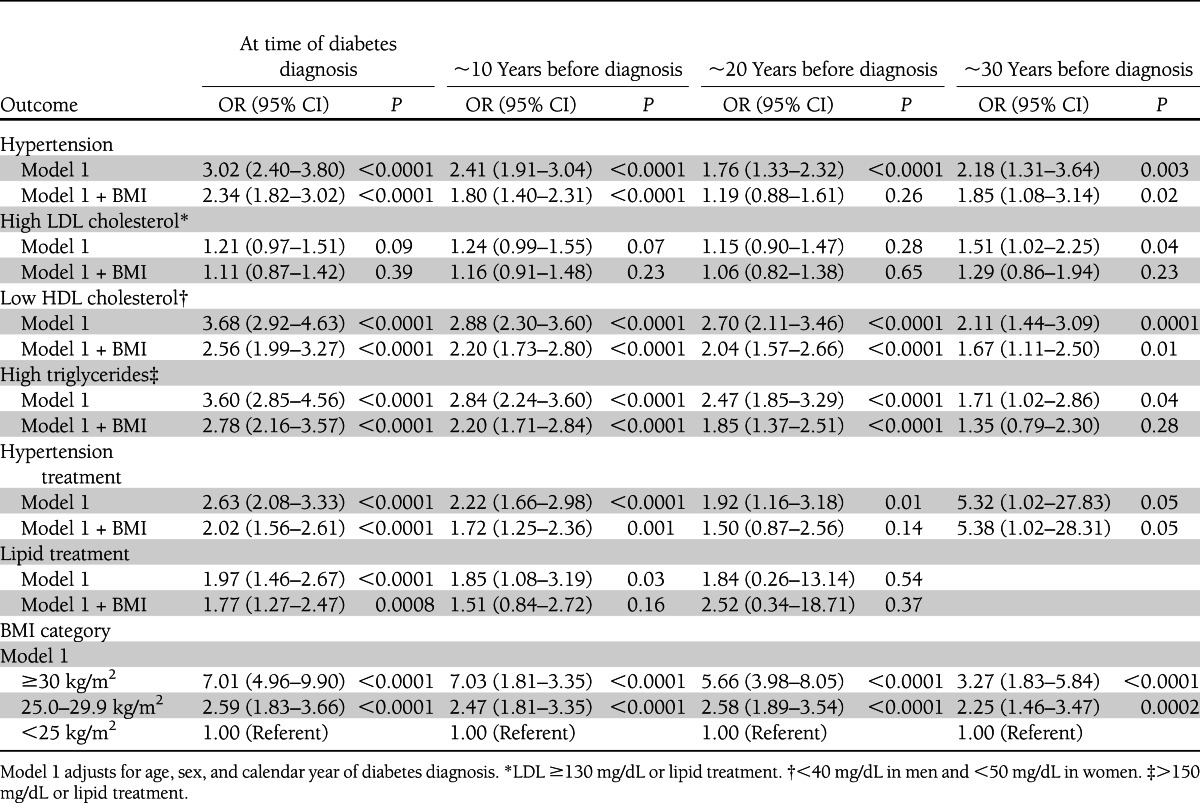
At time points 10 years before diabetes diagnosis, the diabetes cases were more likely to have higher levels of hypertension, low HDL cholesterol, high triglycerides, hypertension treatment, lipid treatment, and obesity relative to those who did not go on to develop diabetes. For example, cases with newly diagnosed diabetes had 2.4-times the odds of having hypertension 10 years before diagnosis as compared with controls. Further adjustment for BMI measured 10 years before diabetes diagnosis resulted in an OR of 1.8. Overall, further adjustment for BMI attenuated the ORs, but they remained statistically significant for all factors except lipid treatment.
At 20 years before diabetes diagnosis, the diabetes cases were more likely to have hypertension, low HDL cholesterol, high triglycerides, hypertension treatment, and obesity as compared with individuals who did not develop diabetes. These differences persisted for low HDL cholesterol and high triglycerides after adjustment for BMI measured 20 years before diagnosis.
Finally, individuals who developed diabetes also were more likely to have hypertension, high LDL cholesterol, low HDL cholesterol, high triglycerides, and obesity at time points up to 30 years before the development of diabetes. After further adjustment for BMI measured 30 years before diagnosis, the differences between cases and controls remained statistically significant for hypertension and low HDL cholesterol.
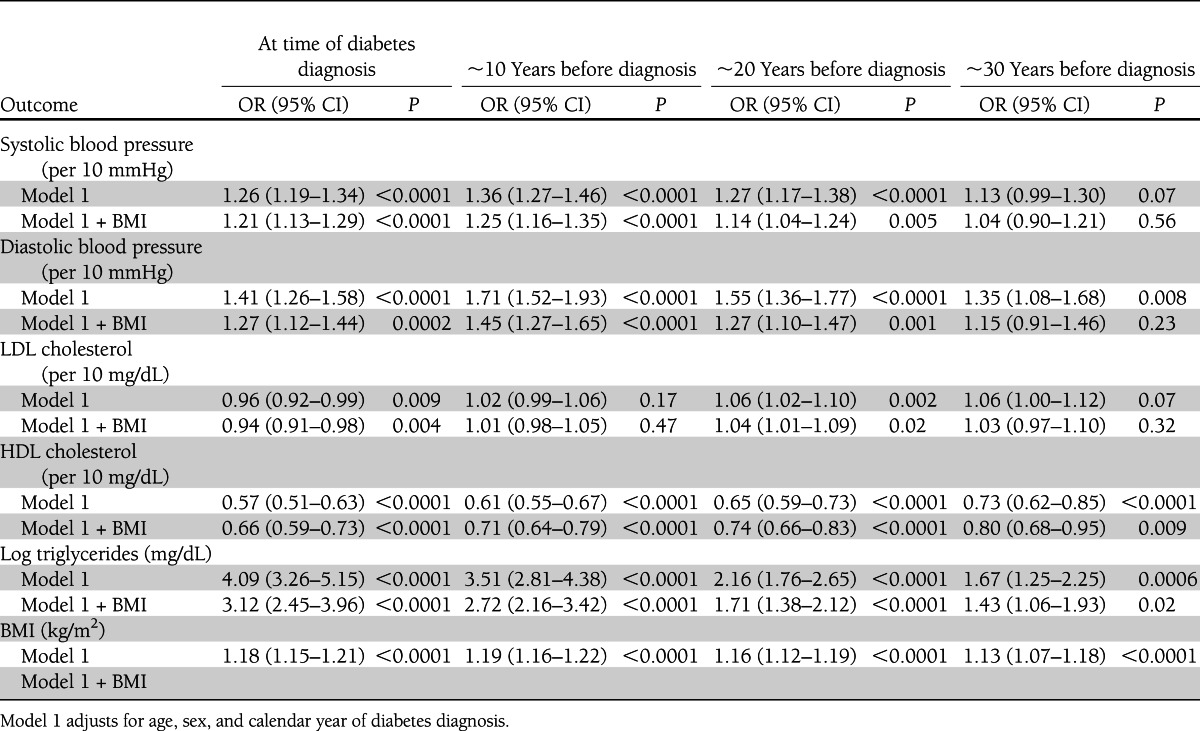
The logistic regression model results for the continuous CVD risk factors are presented in Table 3. Similar to the categorical outcomes, individuals who developed diabetes had higher levels of all cardiovascular risk factors at the time of diabetes diagnosis. Individuals who ultimately developed diabetes also had higher levels of blood pressure, LDL cholesterol, triglycerides, and BMI, and had lower levels of HDL cholesterol at time points up to 30 years before the time of diagnosis. After further adjustment for BMI measured 30 years before diabetes diagnosis, individuals who went on to develop diabetes had lower absolute levels of HDL cholesterol and higher levels of triglycerides.
Table 3.
ORs of diabetes per unit increase of continuous CVD risk factors in the Framingham Heart Study
CONCLUSIONS
Principal findings
We examined the midlife CVD risk factor burden among individuals who did and did not develop diabetes at time points 10, 20, and 30 years before diagnosis. There are four main findings from our study. First, individuals with newly diagnosed diabetes have an increased burden of CVD risk factors at the time of their diagnosis relative to age- and sex-matched controls. Second, the overall prevalence of treatment for both elevated blood pressure and lipids is low at the time of diabetes diagnosis. Third, we demonstrated that this increased CVD risk factor burden among individuals who go on to develop diabetes exists at time points up to 30 years before diagnosis. Fourth, the increased risk factor burden among individuals who develop diabetes remained after adjustment for BMI. Taken together, these results highlight that diabetes is a life course disease and underscores the point that CVD risk associated with diabetes does not begin at the time of clinical diabetes diagnosis.
In the context of the current literature
Two previous studies have examined the prevalence of midlife CVD risk factors among individuals who go on to develop diabetes (1,2). One study examined the CVD risk factor profiles of 1,847 individuals aged 40–79 years from Rancho Bernardo, California, who were free of diabetes and impaired fasting blood glucose at baseline in 1972–1974 (2). After an average of 12 years of follow-up (range, 10–15 years; 1984–1987), individuals who went on to develop diabetes had higher levels of blood pressure, BMI, fasting plasma glucose, and triglycerides at the baseline examination when compared with those who had normal fasting plasma glucose levels at the end of the follow-up period. Similar trends were seen among individuals who developed impaired fasting plasma glucose at the end of follow-up compared with individuals who did not develop either diabetes or impaired fasting glucose.
In a study of 614 Mexican Americans from the San Antonio Heart Study (mean age, 41–48 years at baseline) who were free of diabetes at their baseline visit in 1979–1982, those who developed diabetes after 8 years of follow-up had higher baseline levels of total cholesterol, LDL cholesterol, triglycerides, fasting plasma glucose, BMI, and blood pressure, and had lower levels of HDL cholesterol than the participants who did not develop diabetes (1). These results persisted after adjustment for baseline levels of BMI and fasting plasma glucose. Our study is consistent with previous studies showing that individuals who go on to develop diabetes have modestly higher CVD risk factors levels up to three decades before diagnosis. We found that individuals with diabetes had lower LDL levels than the controls at the time of diagnosis, possibly because of the greater prevalence of lipid treatment among diabetes cases. Looking at the time periods up to 30 years previously, this trend is reversed where the LDL levels are higher among individuals who eventually develop diabetes. Our results from the current study expand on the current literature by examining a longer time period of up to 30 years before clinical diabetes diagnosis and by using more contemporary data. Additionally, the participants in our study were slightly younger, having a mean age of 36 years at time points ∼30 years before diabetes diagnosis, allowing us to examine a longer time range.
Biological mechanisms
Individuals who have elevated risk factors early in life have an increased risk of CVD. For example, a study of 1,017 young men (mean age, 22 years) found that higher levels of total cholesterol in early adulthood were associated with increased risk of coronary heart disease and CVD mortality after 30 years of follow-up (10). Early life CVD risk factor levels also have been shown to be associated with higher levels of coronary artery calcium, a preclinical form of coronary heart disease (11,12). The importance of early-life levels of CVD risk factors also was recently underscored in an analysis of risk factor levels for the prediction of elevated coronary artery calcium, which showed that early-life risk factors were more strongly related as compared with contemporary risk factors (11). Autopsy studies of adolescents and young adults suggest that atherosclerotic plaques can be found among individuals as young as 15 years old (13). Our data suggest that diabetes follows a similar pattern in which the disease begins early in life with the presence of elevated CVD risk factors.
Implications
Once clinically diagnosed with diabetes, many guidelines suggest aggressive risk factor management, particularly for glycemic control, hypertension, dyslipidemia, and smoking cessation (14–17). In addition, therapeutic lifestyle management may include counseling regarding weight reduction, increasing physical activity, and improved nutrition (15). However, our data suggest that CVD risk factor elevation is present well before the time of clinical diabetes diagnosis. Therefore, waiting to aggressively intervene on CVD risk factors at the time of diabetes diagnosis may mean the loss of important clinical opportunities to reduce the ultimate life-long burden of CVD risk. This also may explain why it is difficult to achieve major benefits in CVD risk reduction among individuals with diabetes by focusing on glucose control alone (18). It has been shown that intensive management of risk factors among individuals with diabetes resulted in lower mortality rates as compared with standard therapy regimens (19). However, this finding has not been confirmed in subsequent larger studies (20,21). Our findings suggest that it may be more important to focus on adverse risk factor levels earlier in life, before diabetes is present.
Our results are particularly notable for the increased levels of BMI that antedate diabetes onset at all points in time, with an increased prevalence of obesity of two-fold to three-fold higher in those destined to develop diabetes as compared with controls at each time point. Because obesity is an important risk factor for the development of hypertension, dyslipidemia, and diabetes, these results highlight the importance of aggressive weight management through the entire life course as a means to ultimately reduce the burden of diabetes, concomitant CVD risk factors, and ultimately CVD (16,22). However, it is also important to acknowledge that adjustment of our main results for BMI did not completely attenuate the observed associations, suggesting that measures of BMI alone may not completely explain the risk. It is possible that differences in body composition, which may not be captured by BMI, may be more important than overall adiposity.
Strengths and limitations
The strengths of our study include the long follow-up period of risk factor measurement as well as the availability of contemporary data. Risk factor data were carefully measured in a standardized way across 30 years of our study. Participants were primarily younger adults at the time of their first study examination, allowing us to generalize our data back to a wide age range. Finally, we were able to follow-up study participants to when they were a mean of 60 years, allowing us to ascertain who was ultimately destined to develop diabetes. Our study is limited by the all-white composition of the study population, which may limit generalizability to other ethnic or racial groups. Additionally, although we had a long duration of data, we did not have true life-long data for the individuals in our study. Because we used a nested case-control design, we did not have complete data for all of the participants for the 30 years before their diabetes diagnoses. Our main results were adjusted for BMI; however, we were unable to adjust for other adiposity measurements, such as waist circumference or visceral fat, because they were not available at all examination cycles. Overall, participants who went on to develop diabetes had more adverse risk factor profiles at every time point than those who did not develop diabetes. However, it is important to note the majority of these participants did not have elevated lipid or blood pressure levels ∼30 years before diagnosis. Our study was not able to identify the determinants of the “residual risk” that these participants have.
Conclusion
CVD risk factors are increased at the time of diabetes diagnosis and up to 30 years before the diagnosis of diabetes. These findings suggest that diabetes should be considered a life course disease and that treatment and control of risk factors should begin early in life rather than at the time of diabetes diagnosis.
Acknowledgments
This work was supported by the National Heart, Lung, and Blood Institute’s Framingham Heart Study (N01-HC-25195).
No potential conflicts of interest relevant to this article were reported.
S.R.P., M.J.P., D.M.M., and C.S.F. researched data. S.R.P. wrote the manuscript. M.J.P., R.B.D., P.J.S., and C.S.F. reviewed and edited the manuscript. C.S.F. contributed to discussion.
S.R.P. and C.S.F. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Haffner SM, Stern MP, Hazuda HP, Mitchell BD, Patterson JK. Cardiovascular risk factors in confirmed prediabetic individuals. Does the clock for coronary heart disease start ticking before the onset of clinical diabetes? JAMA 1990;263:2893–2898 [DOI] [PubMed] [Google Scholar]
- 2.McPhillips JB, Barrett-Connor E, Wingard DL. Cardiovascular disease risk factors prior to the diagnosis of impaired glucose tolerance and non-insulin-dependent diabetes mellitus in a community of older adults. Am J Epidemiol 1990;131:443–453 [DOI] [PubMed] [Google Scholar]
- 3.Dawber TR , Meadors GF, Moore FEJ. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health 1951;41:279–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci 1963;107:539–556 [DOI] [PubMed] [Google Scholar]
- 5.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol 1979;110:281–290 [DOI] [PubMed] [Google Scholar]
- 6.Splansky GL, Corey D, Yang Q, et al. The Third Generation Cohort of the National Heart, Lung, and Blood Institute’s Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 2007;165:1328–1335 [DOI] [PubMed] [Google Scholar]
- 7.Rothman KJ, Greenland S. Modern Epidemiology. Philadelphia, PA, Lippincott-Raven Publishers, 1998 [Google Scholar]
- 8.Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of controls in case-control studies. III. Design options. Am J Epidemiol 1992;135:1042–1050 [DOI] [PubMed] [Google Scholar]
- 9.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 10.Klag MJ, Ford DE, Mead LA, et al. Serum cholesterol in young men and subsequent cardiovascular disease. N Engl J Med 1993;328:313–318 [DOI] [PubMed] [Google Scholar]
- 11.Loria CM, Liu K, Lewis CE, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol 2007;49:2013–2020 [DOI] [PubMed] [Google Scholar]
- 12.Mahoney LT, Burns TL, Stanford W, et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J Am Coll Cardiol 1996;27:277–284 [DOI] [PubMed] [Google Scholar]
- 13.Strong JP, Malcom GT, McMahan CA, et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA 1999;281:727–735 [DOI] [PubMed] [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association Executive summary: standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl 1):S4–S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association Standards of medical care in diabetes—2008. Diabetes Care 2008;31(Suppl 1):S12–S54 [DOI] [PubMed] [Google Scholar]
- 18.Gerstein HC, Miller ME, Byington RP, et al. Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–591 [DOI] [PubMed] [Google Scholar]
- 20.Cushman WC, Evans GW, Byington RP, et al. ACCORD Study Group Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ginsberg HN, Elam MB, Lovato LC, et al. ACCORD Study Group Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 2010;362:1563–1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burke GL, Bertoni AG, Shea S, et al. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med 2008;168:928–935 [DOI] [PMC free article] [PubMed] [Google Scholar]