Abstract
OBJECTIVE
Long-chain n-3 polyunsaturated fatty acid (n-3 PUFA) supplements may have renoprotective effects in patients with diabetes, but previous trials have been inconsistent. We performed a randomized controlled trial of n-3 PUFA supplementation on urine albumin excretion and markers of kidney injury in adults with type 2 diabetes.
RESEARCH DESIGN AND METHODS
We conducted a randomized, placebo-controlled, two-period crossover trial to test the effects of 4 g/day of n-3 PUFA supplementation on markers of glomerular filtration and kidney injury in adults with adult-onset diabetes and greater than or equal to trace amounts of proteinuria. Each period lasted 6 weeks and was separated by a 2-week washout. The main outcome was urine albumin excretion and, secondarily, markers of kidney injury (kidney injury molecule-1, N-acetyl β-d-glucosaminidase [NAG], neutrophil gelatinase-associated lipocalin [NGAL], and liver fatty acid–binding protein [LFABP]), serum markers of kidney function (cystatin C, β2-microglobulin, and creatinine), and estimated glomerular filtration rate (eGFR).
RESULTS
Of the 31 participants, 29 finished both periods. A total of 55% were male, and 61% were African American; mean age was 67 years. At baseline, mean BMI was 31.6 kg/m2, median eGFR was 76.9 mL/min/1.73 m2, and median 24-h urine albumin excretion was 161 mg/day. Compared with placebo, n-3 PUFA had nonsignificant effects on urine albumin excretion (−7.2%; 95% CI −20.6 to 8.5; P = 0.35) and significant effects on urine NGAL excretion (−16% [−29.1 to −0.5%]; P = 0.04). There was no effect on serum markers of kidney function or eGFR. In subgroup analyses, there were significant decreases in 24-h urinary excretion of albumin, NGAL, LFABP, and NAG among participants taking medications that block the renin-angiotensin-aldosterone system (RAAS).
CONCLUSIONS
These results suggest a potential effect of n-3 PUFA supplementation on markers of kidney injury in patients with diabetes and early evidence of kidney disease. In the context of prior studies, these results provide a strong rationale for long-term trials of n-3 PUFA on chronic kidney disease progression.
Diabetes is a leading cause of chronic kidney disease (CKD) (1). Treatments to slow the progression of CKD in diabetes include blocking the renin-angiotensin-aldosterone system (RAAS), implementing lower blood pressure (BP) treatment goals, and treating hyperglycemia (2). These therapies can also reduce urine protein excretion, a marker of disease severity. Indeed, maximal reduction of urine protein excretion has been proposed as a goal of drug therapy (3). Long-chain n-3 polyunsaturated fatty acid (n-3 PUFA) supplements may improve endothelial function, lower BP, and have independent antiproteinuric effects (4). However, evidence of benefit from supplementation with n-3 PUFA on urine protein excretion in the setting of diabetic kidney disease is inconsistent (5–11).
New markers of kidney function and injury hold considerable promise as a means to evaluate the potential benefits of therapies designed to retard the progression of CKD. Biomarkers of tubulointerstitial kidney damage, including kidney injury molecule-1 (KIM-1), N-acetyl β-d-glucosaminidase (NAG), neutrophil gelatinase-associated lipocalin (NGAL), and liver fatty acid–binding protein (LFABP) may have greater sensitivity for identifying effects on kidney injury than total urine protein or albumin excretion, which reflect both kidney injury and hemodynamic effects (12,13). Novel serum markers, including β2-microglobulin and cystatin C, may provide greater sensitivity for determining short-term effects of therapies on estimated glomerular filtration rate (eGFR) than traditional markers of filtration. These new markers of kidney function and injury might be especially useful in guiding the design of subsequent long-term trials.
In this context, we conducted a randomized, controlled crossover trial to evaluate the efficacy of n-3 PUFA supplements on improving markers of kidney injury and function in adults with adult-onset diabetes and greater than or equal to trace amounts of proteinuria.
RESEARCH DESIGN AND METHODS
Study design and study population
This study was a single-center, randomized, controlled two-period crossover trial of n-3 PUFA supplements versus placebo (corn oil) supplements. Each period lasted 6 weeks. Participants were recruited at the Johns Hopkins ProHealth clinic, a community-based research clinic in Baltimore, MD. The primary recruitment process was mass mailings of invitations to persons with self-reported type 2 diabetes. Study brochures were mailed to zip codes near Johns Hopkins ProHealth. Participants underwent two screening visits to determine eligibility prior to enrollment.
Inclusion criteria were a self-reported diagnosis of diabetes, either treated with oral medication(s) or diet-controlled; age >21 years; an average systolic BP (SBP) <150 mmHg and diastolic BP (DBP) <90 mmHg during two screening visits; and a quantified level of proteinuria greater than or equal to trace but <4+ on urine dipstick analysis during screening. If participants were taking antihypertensive, hypoglycemic, or lipid-lowering medications, we required stable doses for a minimum of 2 months prior to randomization. Exclusion criteria were poorly controlled diabetes (self-reported hemoglobin A1c [HbA1c] >9%); use of insulin; being pregnant or planning on becoming pregnant during the study period; unwillingness to stop taking fish oil supplements 1 month prior to randomization for those on fish oil supplements; or an eGFR <30 mL/min (stage 4 or stage 5 CKD) based on the Modification of Diet in Renal Disease equation (14). The Johns Hopkins Institutional Review Boards approved the study protocol. All participants provided written informed consent.
Randomization and interventions
If participants were eligible based on their screening visits, they were asked to complete a 2–4-week run-in period during which they took four corn oil capsules per day. After run-in, participants who remained interested and eligible were randomized. Randomized assignments were generated from a random-numbers table, placed in sealed opaque envelopes, and opened by the study coordinator in consecutive order. An 8-week supply of capsules was provided to participants in preallocated monthly pill packs. Participants, all study staff, and analytic team members were masked to the randomization sequence.
Participants took four capsules per day during the intervention period. Each 1-g capsule of n-3 PUFA contained ∼85% n-3 fatty acid ethyl esters sourced from fish oils, a combination of ethyl esters of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) in an ∼2:1 ratio. A 2-week washout separated the two periods. The placebo capsules were identical in appearance to the n-3 PUFA capsules and contained an isocaloric equivalent of corn oil. Pharmacokinetic studies suggested that a 6-week period would be adequate for serum levels of n-3 PUFA to reach steady state and that a 4-week period would provide sufficient time for serum levels to return to baseline levels following withdrawal (15,16). Participants were asked not to alter medication regimens of drugs that affect BP, diabetes, or lipids.
Data collection
Study participants completed visits at baseline and at the end of each treatment period. Weight, height, and waist circumference were measured. BP was measured by the oscillometric technique using an OMRON 907 machine (Omron, Vernon Hills, IL). A set of three readings (separated by 30 s) after 5 min of rest was performed following a standardized protocol.
Study participants provided fasting blood samples and 24-h urine collections at each of the three clinic visits. Blood samples were allowed to clot at room temperature for 15 min and centrifuged at 2°C. Serum aliquots were stored at −70°C. Aliquots of 24-h urine collections were collected and stored at −70°C. Fasting serum levels of total cholesterol, HDL cholesterol, triglycerides, fasting serum glucose, and liver function tests were measured by a local laboratory (Quest Diagnostics). LDL cholesterol was estimated using the Friedewald equation (17). Erythrocyte fatty acids including DHA and EPA were isolated by solid-phase extraction, identified, and quantitated by gas liquid chromatography–mass spectrometry in the Peroxisome Diseases section of the Kennedy Krieger Institute using standard methodologies (18).
Study outcomes
The primary outcome variable was 24-h urine albumin excretion. Secondary outcome variables were eGFR, cystatin C, and β2-microglobulin measured in fasting serum and NAG, LFABP, NGAL, and KIM-1 measured in 24-h urine samples. All outcome variables were measured at baseline and the end of each treatment period. Laboratory assays of outcome measures were performed at the Cincinnati Children’s Hospital Medical Center by personnel who were masked to participant randomized sequence. Urine albumin was measured by immunoturbidometry using Dimension Xpand Plus clinical chemistry system (Siemens). Serum cystatin C and β2-microglobulin were measured by particle-enhanced immunonephelometric assays (Dade Behring, Deerfield, IL). Urine NAG activity was measured using a colorimetric assay (Roche Diagnostics) as previously described (19). Urine NGAL was assayed using a human-specific commercially available ELISA (AntibodyShop, Grusbakken, Denmark), and LFABP was measured using commercially available ELISA kits (CMIC Co., Tokyo, Japan) per the manufacturer’s instructions. The urine KIM-1 ELISA was constructed using commercially available reagents (R&D Systems, Minneapolis, MN). eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation (14).
Statistical considerations
Sample size for this study was based on estimates of the difference in change in 24-h urine albumin excretion (the primary outcome variable) and in eGFR. For urine protein excretion, we anticipated that a sample size of 30 participants would result in 80% power to detect a difference between the n-3 PUFA and placebo periods of 10% at an α of 0.05.
The primary statistical analysis was the comparison of the difference in change in markers of kidney injury between the n-3 PUFA supplementation period and placebo period. The primary variable was the mean change in outcome variables from baseline using repeated-measures analysis (i.e., generalized estimating equations with an exchangeable correlation structure). The distributions of data were checked for normality and transformed where appropriate. Other outcome variables were analyzed with a similar approach. Carryover effects of the n-3 PUFA supplement on the erythrocyte membrane fatty acids were evaluated using treatment by assignment-order interaction terms.
We used interaction terms to evaluate effect modification by prerandomization medication use, namely, diuretics, statins, glucose-lowering medications, and medications that block the RAAS (e.g., ACE inhibitors and angiotensin receptor blockers [ARBs]). Statistical significance was P < 0.05. All analyses were performed using STATA version 11.1 (Stata Corporation, College Station, TX).
RESULTS
Study participants
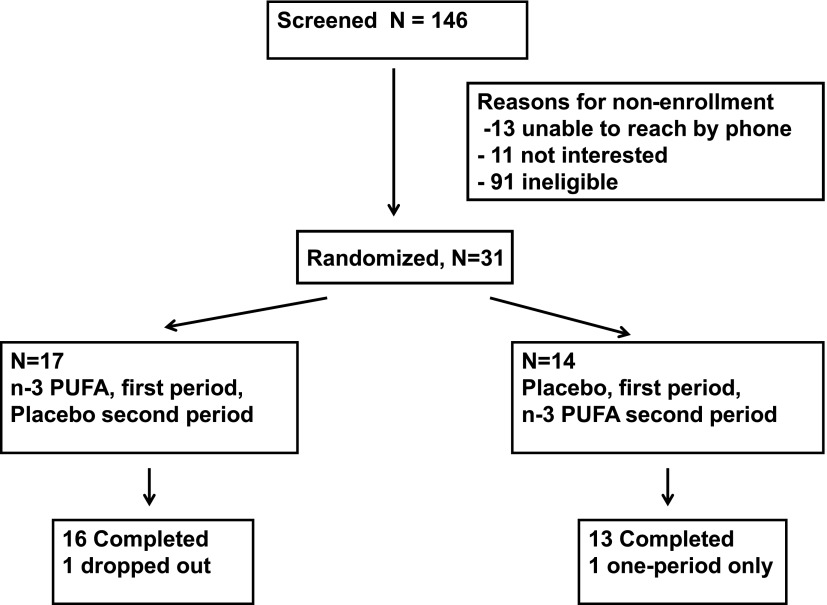
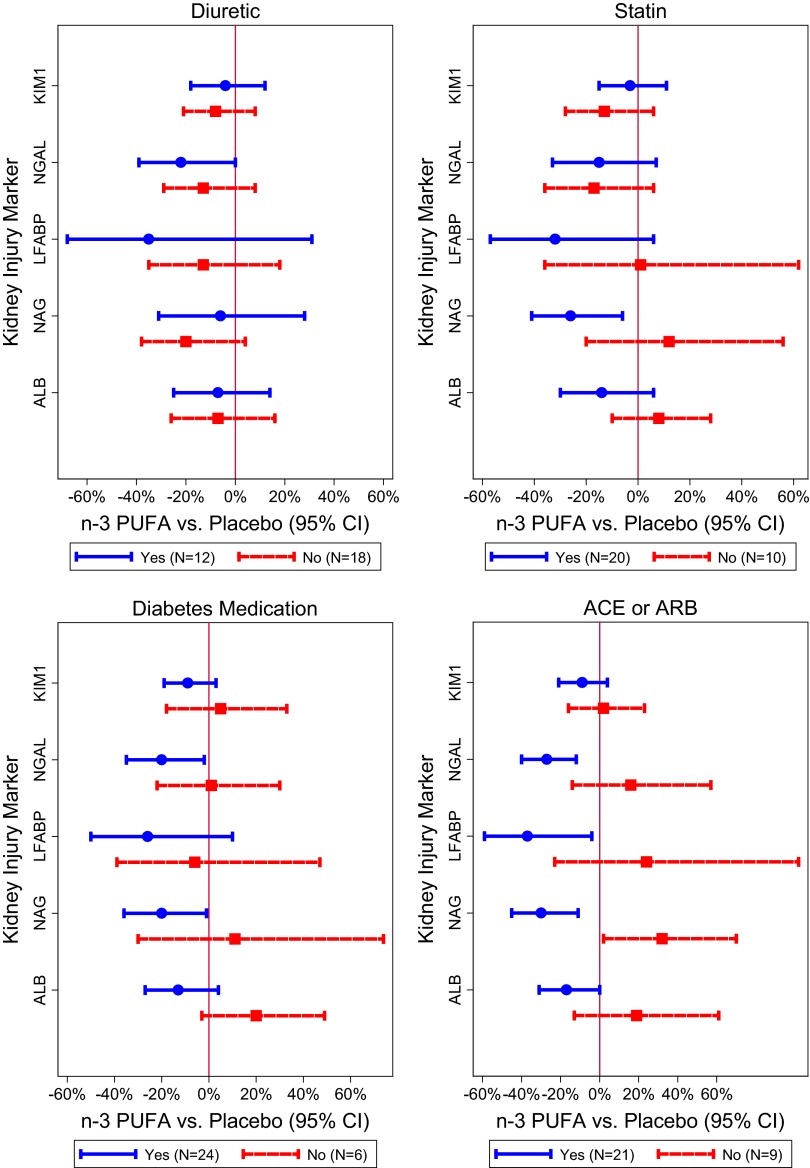
Of 132 prescreened participants, we randomized 31 participants (Fig. 1). A lack of detectable urine dipstick proteinuria at screening was the most common reason for participants being ineligible. One randomized participant withdrew before data collection, and one completed only one period. Baseline characteristics are presented in Table 1, after excluding the participant who withdrew prior to data collection. Mean (SD) age of participants was 67.4 (11.5) years, 55% were male, and 61% were African American. Mean (SD) BMI was 31.6 (5.3) kg/m2. At baseline, 68% of participants had microalbuminuria (30–300 mg/day), and 26% had macroalbuminuria (>300 mg/day). Most participants were taking lipid-lowering therapy (65%), RAAS inhibitors (68%), and/or hypoglycemic medications (81%).
Figure 1.
Participant flow during the trial.
Table 1.
Characteristics of trial participants (N = 31)
Urine markers of kidney injury
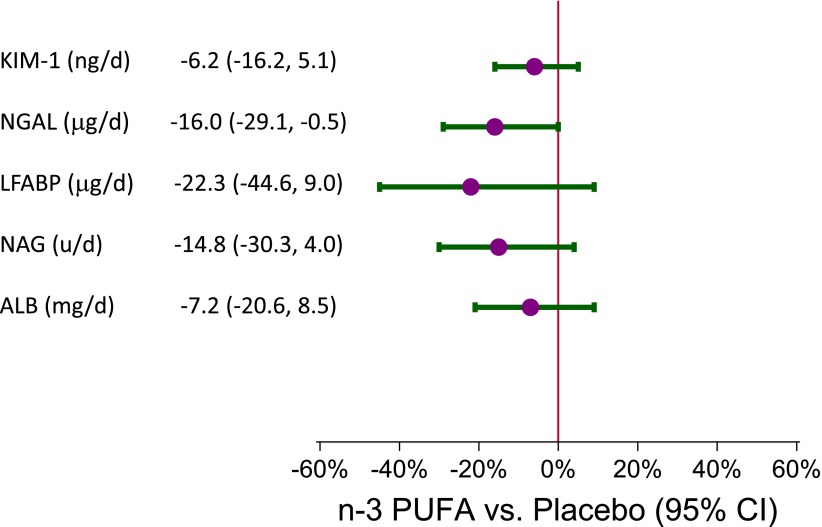
Baseline values and changes in urine markers of kidney injury are reported in Table 2. Compared with the placebo period, n-3 PUFA had no significant effects on the 24-h urine excretion of albumin but significantly lowered NGAL (−16%; 95% CI −29.1 to −0.5%; P = 0.04). Although n-3 PUFA did not significantly lower other markers of kidney injury, there was a consistent trend of reduction during the n-3 PUFA supplementation period (Fig. 2).
Table 2.
Baseline, change from baseline, and difference between placebo and n-3 PUFA groups in serum markers of kidney function and urine kidney injury molecules
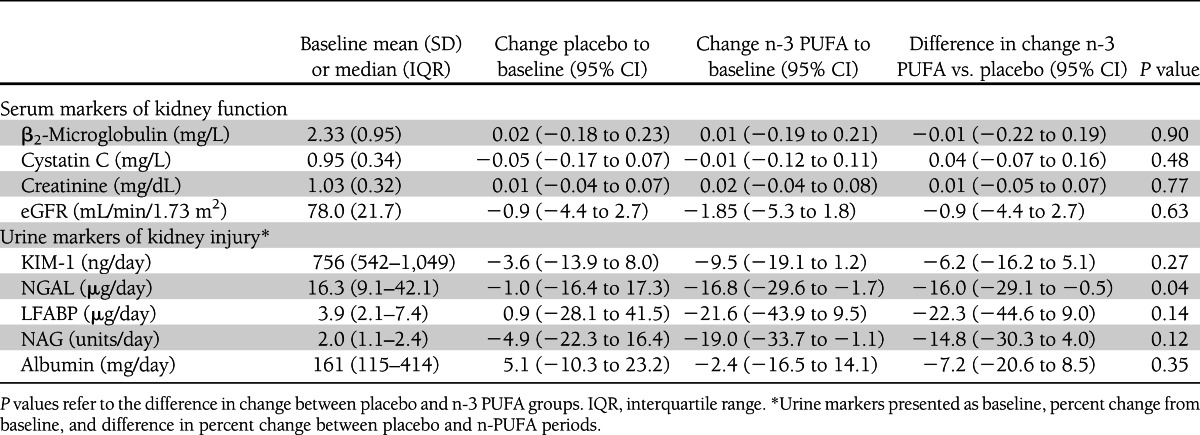
Figure 2.
Mean percent difference in 24-h urinary excretion of KIM-1, NGAL, LFABP, NAG, and albumin (ALB) comparing the n-3 PUFA to the control period. (A high-quality color representation of this figure is available in the online issue.)
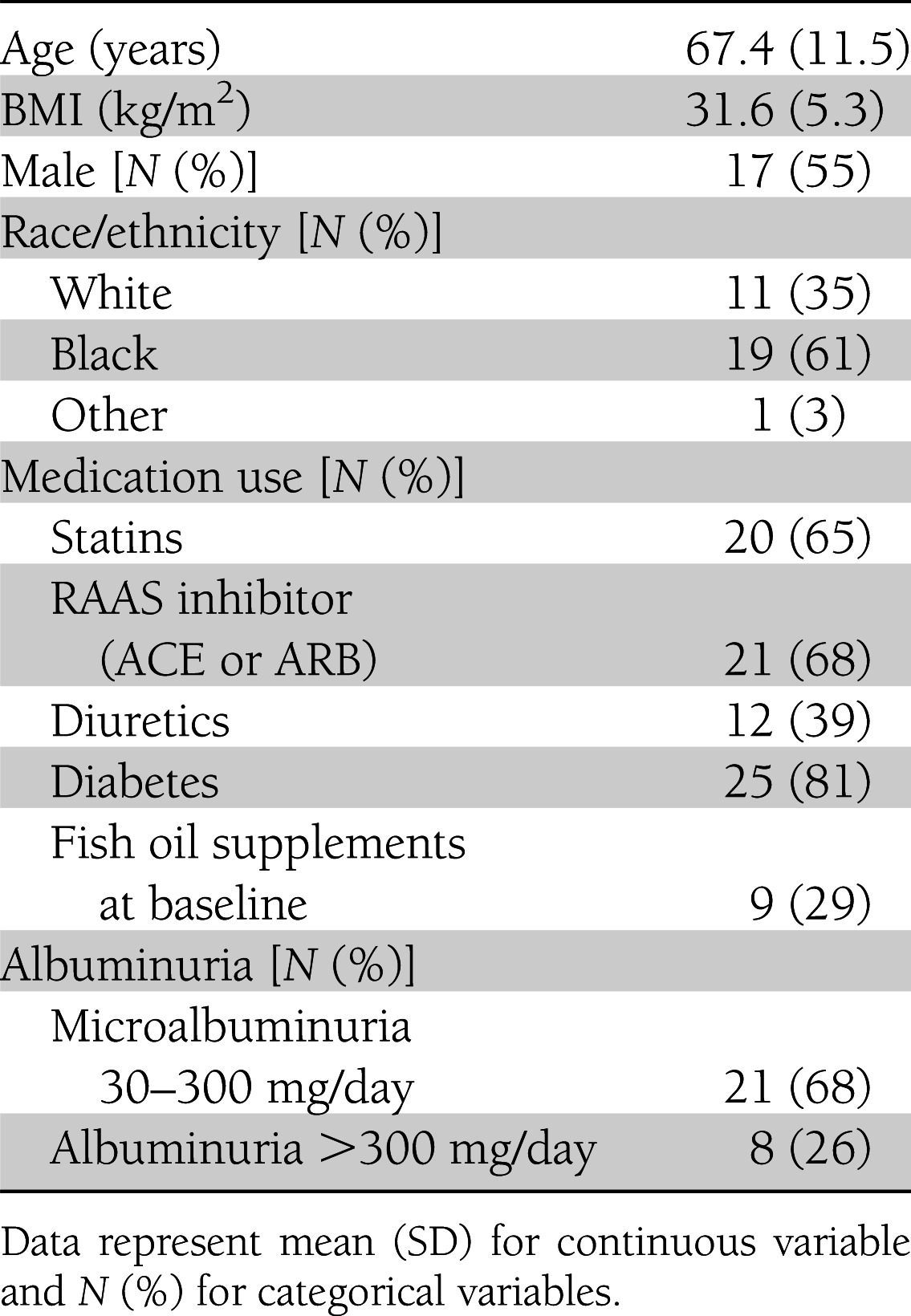
In stratified analysis by use of chronic stable doses of diuretics, statins, oral hypoglycemic medications, and RAAS-inhibitor medications, interaction terms used to evaluate the effects of RAAS and n-3 PUFA supplementation use were significant for NGAL (P = 0.01), NAG (P < 0.01), and microalbuminuria (P = 0.04), borderline significant for LFABP (P = 0.06), and nonsignificant for KIM-1 (P = 0.35) (Table 3). Within the stratum of RAAS-inhibitor users, there were significant reductions in all of the urinary kidney injury markers except KIM-1. In contrast, among those not taking RAAS inhibitors, we observed nonsignificant increases in most markers and a significant increase in NAG (1.32 units/day; 95% CI 1.02–1.70). The other medication classes did not demonstrate a similar consistent pattern of effect modification (Fig. 3).
Table 3.
Test for interactions between concurrent medication use and n-3 PUFA effects on markers of kidney injury
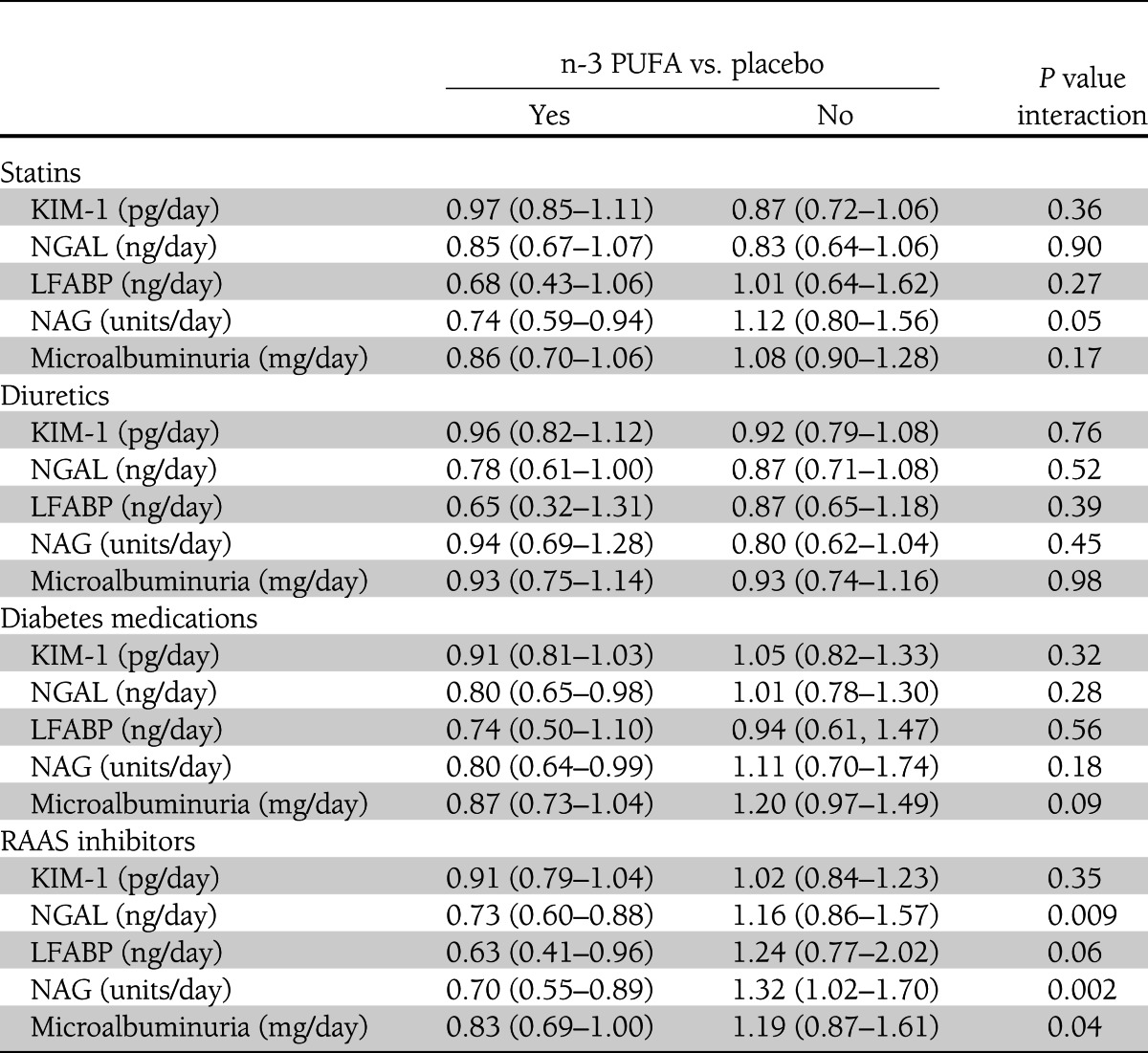
Figure 3.
Mean percent difference in 24-h urinary excretion of KIM-1, NGAL, LFABP, NAG, and albumin (ALB) comparing the n-3 PUFA to the control period, stratified by diuretic use (yes/no), statin use (yes/no), diabetes medication use (yes/no), and RAAS-inhibitor (ACE/ARB) use (yes/no). (A high-quality color representation of this figure is available in the online issue.)
Serum markers of kidney function
At baseline, the mean (SD) eGFR, serum cystatin C, and β2-microglobulin levels were 76.9 (22.3) mL/min/1.73 m2, 0.95 (0.34) mg/L, and 2.33 (0.95) mg/L, respectively. eGFR was highly correlated with serum β2-microglobulin (r = −0.69) and cystatin C (r = −0.76). n-3 PUFA had nonsignificant effects on serum markers of kidney function and eGFR. Specifically, the difference in eGFR comparing n-3 PUFA supplementation to control was −0.9 mL/min/1.73 m2 (95% CI −3.1 to 1.4; P = 0.45). The differences in β2-microglobulin and cystatin C were −0.01 mg/L (−0.12 to 0.09; P = 0.79) and 0.04 mg/L (−0.10 to 0.18; P = 0.55), respectively.
Other outcomes
Baseline change and treatment-arm comparisons of other outcomes are shown in Table 4. Compared with placebo, n-3 PUFA supplementation was associated with a nonsignificant change in SBP (−3.4 mmHg; 95% CI −7.7 to −1.0; P = 0.13) and DBP (−1.5 mmHg [−3.8 to 0.8]; P = 0.19) and significant reduction in triglycerides (−24.8 mg/dL [ −43.7 to −5.8]; P = 0.01). In contrast, when compared with placebo, n-3 PUFA supplementation was associated with increases in serum glucose (mean difference 6.5 mg/dL [0.6–12.3]; P = 0.03). There was also a significant increase in alanine aminotransaminase of 2.6 units/L (0.4–4.8; P = 0.02).
Table 4.
Baseline, change from baseline, and difference in change between placebo and n-3 PUFA groups in BP, lipid profile, glucose, and erythrocyte membrane n-3 PUFA
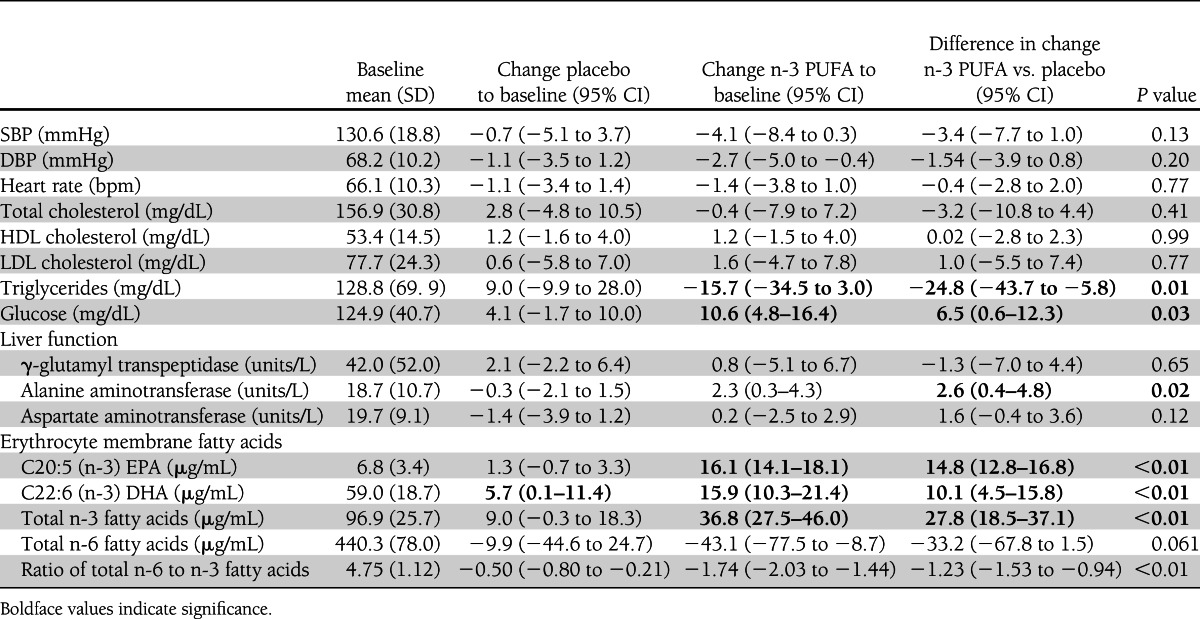
Compliance and safety
Analyses of erythrocyte membrane fatty acids (Table 4) revealed significant increases in EPA, DHA, and total n-3 fatty acids during the n-3 PUFA intervention period compared with placebo, suggesting compliance with the intervention protocols. Carryover effects were statistically significantly for erythrocyte membrane levels of EPA (P = 0.05), but not of DHA (P = 0.12) or total n-3 fatty acids (P = 0.08). Specifically, EPA levels in erythrocytes did not return to baseline in those first assigned to the n-3 PUFA.
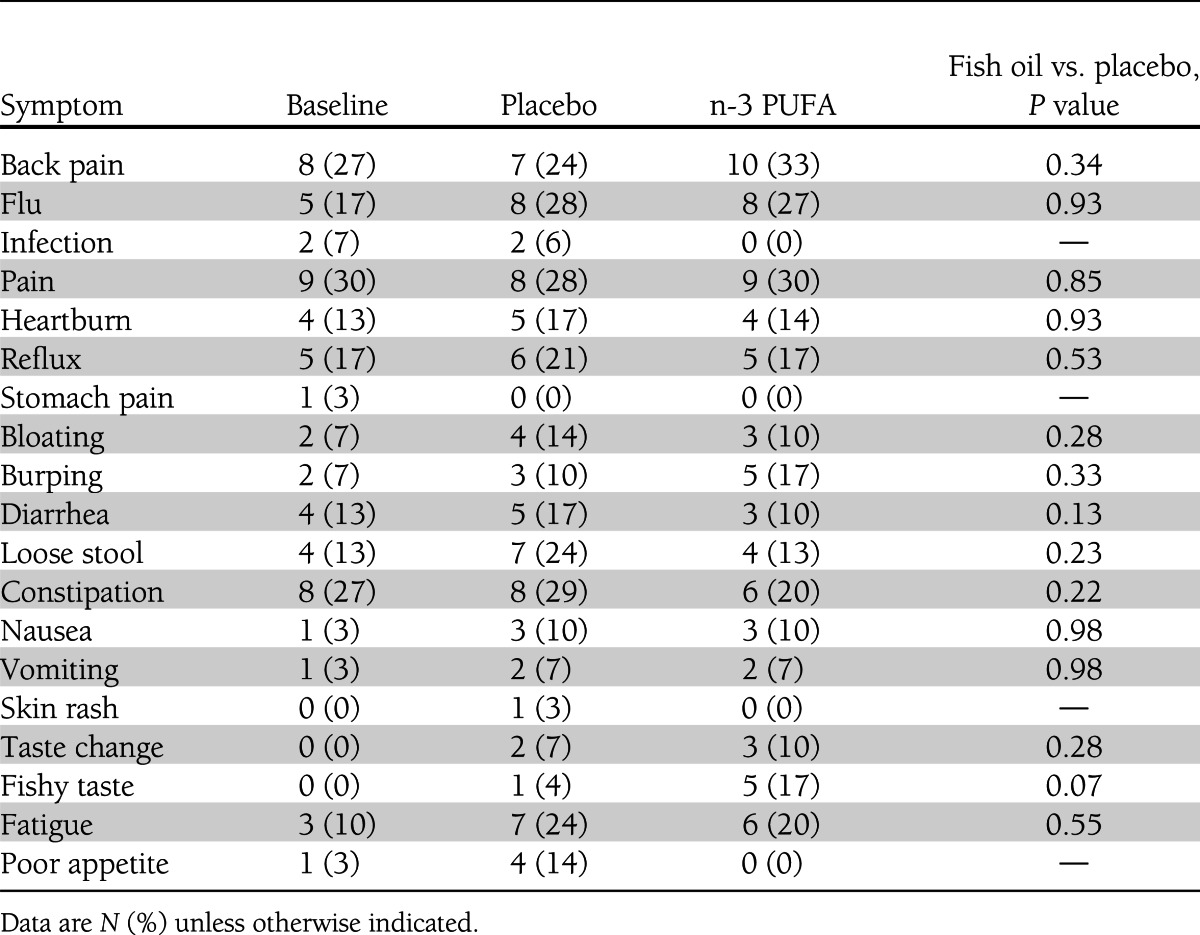
A summary of adverse effects is presented in Table 5. Overall, adverse effects were infrequently reported, and there were no significant differences between treatment groups. Furthermore, when participants were asked at the end of each period to identify the type of capsules that they believed they were taking, 48% (n = 14) of participants taking placebo thought they were taking n-3 PUFA, whereas 47% (n = 14) of participants taking n-3 PUFA thought they were taking placebo, and 4% (n = 1) did not report treatment assignment (χ2, P = 0.3).
Table 5.
Reported side effects at the end of treatment periods
CONCLUSIONS
In this randomized, controlled clinical trial, daily supplementation with n-3 PUFA had nonsignificant effects on urine albumin excretion (−7.2%; 95% CI −20.6 to 8.5; P = 0.35) and significant effects on urine NGAL excretion (−16% [−29.1 to −0.5%]; P = 0.04) in adults with diabetes and proteinuria. In contrast, n-3 PUFA supplements increased fasting glucose by 6.5 mg/dL. In the subgroup of participants taking stable doses of RAAS inhibitors, n-3 PUFA supplementation significantly reduced multiple markers of kidney injury including NGAL (−27%), LFABP (−37%), NAG (−30%), and albuminuria (−17%).
The effects of n-3 PUFA supplements on urine protein excretion have been tested in trials of primarily nondiabetic participants with diverse underlying causes of CKD. In a meta-analysis of 17 trials, we reported a 19% reduction (95% CI −34 to −4; P = 0.01) in urine protein excretion with n-3 PUFA across all trials (20). A similar magnitude of effect was noted in the subgroup of trials (n = 7) that enrolled participants with diabetic kidney disease (−21% [−46 to 4]; P = 0.10).
We can only speculate on mechanisms that may account for the beneficial effects of n-3 PUFA supplementation on kidney-injury processes. Effects on vascular function and renal hemodynamics are possible (4,21). A systematic review of fish oil supplements in hypertensive patients (five trials) reported that an average of 3 g/day of n-3 PUFA reduced SBP/DBP by 5.5/3.5 mmHg (22). Our trial demonstrated a similar reduction in SBP, which could explain reductions in proteinuria and other markers of kidney injury via hemodynamic effects. However, in spite of small differences in BP between the n-3 PUFA and placebo periods, we did not detect an effect of n-3 PUFA supplementation on β2-microglobulin, cystatin C, or creatinine-based eGFR. These results suggest that n-3 PUFA effects on kidney injury markers are likely independent of hemodynamic effects that effect GFR.
n-3 PUFA supplementation may also alter the balance of n-3 and n-6 fatty acids available for prostaglandin production, causing a favorable shift toward production of prostaglandins with more vasodilator effects, enhanced immune function, and reduced inflammation (16,23), mechanisms that may contribute to CKD progression in diabetic kidney disease. n-3 PUFA supplementation may also decrease renal ischemic effects through rheostatic changes on erythrocyte membranes. Stirban et al. (21) noted improved postprandial microvascular reactive hyperemia after ischemia in adults with non–insulin-dependent diabetes with 2 g/day of n-3 PUFA. This mechanism was believed to be largely independent of nitric oxide–mediated regulations of vascular tone and more related to the influence of n-3 PUFA on prostaglandin pathways.
In our trial, n-3 PUFA had nonsignificant effects on urine albumin excretion (−7.2%; 95% CI −20.6 to 8.5; P = 0.35). The nonsignificant overall effects of n-3 PUFA supplementation on the primary outcome variable of urine albumin excretion suggest a lack of benefit or reflect a trial is underpowered. Nonetheless, in subgroup analyses, n-3 PUFA significantly reduced urine albumin excretion only in participants on RAAS-inhibition therapy, representing 70% of participants in this trial. Indeed, the use of RAAS-inhibition therapy would be considered a standard of care for patients with diabetes and evidence of kidney disease (2). A priori, one would expect that RAAS inhibitors would have had considerable antiproteinuric effects, limiting the ability to detect the effects of additional agents. In our trial, the opposite occurred. For the most part, previous trials did not report whether the antiproteinuric effects of n-3 PUFA were affected by the concurrent use of RAAS inhibition, but similar results were reported in a trial of patients with immunoglobulin A nephropathy treated with RAAS. In this trial, enhanced antiproteinuric effects were noted with the addition of 3 g/day of n-3 PUFA compared with RAAS treatment alone (24). Possible causes of additional antiproteinuric effects may include anti-inflammatory effects, reduced blood viscosity, and increased erythrocyte flexibility leading to reduced renal tubular ischemia (5,25). The potential interaction between RAAS inhibitors and n-3 PUFA may have important clinical implications and needs to be further investigated as a potential renoprotective combination in patients with diabetes and proteinuria.
Our trial has several strengths. First, the crossover design and relatively short-term intervention periods allowed for assessments of the acute effects on urine albumin excretion and eGFR in the setting of stable doses of medications that may affect urine protein excretion. Second, we enrolled diabetic participants with proteinuria, a common complication and early sign of CKD in patients with diabetes. Third, the diabetes, hyperlipidemia (if present), and hypertension were treated. Hence, supplementation with n-3 PUFA may have added benefit to conventional therapies in those with diabetes and early CKD. Fourth, the high rates of adherence and follow-up, the use of 24-h urine sample collections, and the use of high-quality laboratory methods enhance the internal validity of the trial. Fifth, novel markers of kidney injury are not susceptible to hemodynamic changes that may alter urine albumin excretion.
There are also several limitations. We used a short-term crossover trial design, selected to enhance power to detect differences. Although no carryover effects were detected in the analyses of outcome variables, we detected a carryover effect of the intervention on EPA levels in erythrocytes. Erythrocyte EPA levels did not return to baseline at the end of the study in the group first assigned to n-3 PUFA despite a 2-week washout period and a 6-week period on placebo. We note that this type of carryover effect will tend to mask the effects of n-3 PUFA in the crossover analysis. Hence, future short-term trials of n-3 PUFA would benefit from a longer washout period or a parallel-arm design. Another limitation pertains to our reporting a large number of secondary outcomes and subgroup analyses stratified by baseline medication use. With this approach, one must be cautious in interpreting statistical significance due to multiple comparisons and the risk of type 1 errors. For example, although we report significant reductions in urine excretion of albumin, NAG, NGAL, and LFABP in those participants on RAAS therapy at baseline, there was evidence of increased urine excretion of NAG in those not taking RAAS therapy. This finding can either reflect the truth or, because of type 1 error associated with post hoc subgroup analyses, may be inappropriate. However, we feel that subgroup reporting from this small trial is both informative and clinically relevant and may be helpful in the design of future trials of n-3 PUFA on kidney injury.
Each intervention capsule was a highly concentrated source of DHA/EPA derived from marine fish oils, and the dose was 4.0 g/day. This high dose of n-3 PUFA is far above the daily average intake of U.S. adults (0.15 g/day) (26) and contributes minimally to total calorie intake (∼40 kcal/day). This dose has therapeutic efficacy for triglyceride reduction (∼25–40%) and is the dose currently sold by prescription for the treatment of hypertriglyceridemia. A lower dose of n-3 PUFA (1.0 g/day) has reduced cardiovascular events in some (27,28) but not all (29) clinical trials. In our prior meta-analysis of n-3 PUFA supplementation on urine protein excretion, the dose of n-3 PUFA did not modify the findings, but few trials used doses ≤1 g/day. Since 1 g/day is the currently recommended daily dose of EPA/DHA for adults with coronary heart disease (30), further research is also needed to evaluate the effects of n-3 PUFA across a wider range of doses. Within the Vitamin D and Omega-3 Trial, a National Institutes of Health–funded trial, 1,500 Vitamin D and Omega-3 Trial participants with diabetes, randomly assigned in a 2 × 2 factorial design to vitamin D3 (cholecalciferol) 1,600 IU daily versus placebo and to EPA 500 mg plus DHA 500 mg daily versus placebo, will be studied to ascertain effects of study interventions on albuminuria and GFR (31). Their trial is expected to finish in the year 2015.
Dose effects are also relevant to the observed adverse effects of n-3 PUFA supplements on fasting serum glucose. Increased fasting glucose with n-3 PUFA supplementation has been reported in many, but not all, trials. A recent Cochrane meta-analysis of 15 trials of fish oil supplementation on glucose homeostasis reported a nonsignificant pooled increase in fasting glucose of 2.9 mg/dL (95% CI −2.3 to 8.3 mg/dL), with no effects on HbA1c (32). The mechanisms involved in increasing fasting glucose are unclear, but n-3 PUFA reduce hepatic synthesis of triglycerides and increase hepatic fatty acid β-oxidation, resulting in increased hepatic glucose output through increased glycogenolysis and/or gluconeogenesis (33). Nonetheless, whether a lower dose of n-3 PUFA is sufficient to lower kidney injury but below a threshold to cause hyperglycemic effects needs to be tested.
In conclusion, in this randomized, controlled clinical trial, n-3 PUFA failed to reduce the primary outcome of urine albumin excretion. However, there was a consistent trend of benefit for all urine biomarkers and a significant reduction in NGAL. Furthermore, our post hoc subgroup findings raise the intriguing possibility that the greatest effects of n-3 PUFA are in individuals on RAAS inhibitors. There were small reductions in SBP and DBP, an increase in fasting glucose, but no apparent effect on eGFR with n-3 PUFA supplementation. Our results in the context of prior studies provide a strong rationale for larger trials that are adequately powered for smaller effects on urine albumin excretion or trials that are conducted in participants who take ACE/ARB therapy. In long-term trials of n-3 PUFA with clinical outcomes such as CKD progression, which are underway, careful consideration should be given for the potential beneficial interactions between RAAS therapy and n-3 PUFA.
Acknowledgments
This study was supported by National Institute of Diabetes and Digestive and Kidney Diseases Grant R21-DK-080372 awarded to E.R.M. Lovaza (n-3 PUFA) and placebo were kindly provided by GlaxoSmithKline. No other potential conflicts of interest relevant to this article were reported.
E.R.M. analyzed and interpreted data, conceptualized and designed the study, and drafted the manuscript. S.P.J. analyzed and interpreted data and drafted the manuscript. C.A.A., E.G., K.H.-R., S.T., and M.R.B. drafted the manuscript. J.C. and L.J.A. conceptualized and designed the study and drafted the manuscript. E.R.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was presented in abstract form at the American Society of Nephrology Kidney Week, San Diego, California, 30 October–4 November 2012.
Footnotes
Clinical trial reg. no. NCT01092390, clinicaltrials.gov.
References
- 1.Burrows NR, Li Y, Williams DE. Racial and ethnic differences in trends of end-stage renal disease: United States, 1995 to 2005. Adv Chronic Kidney Dis 2008;15:147–152 [DOI] [PubMed] [Google Scholar]
- 2.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2012;55:1577–1596 [DOI] [PubMed] [Google Scholar]
- 3.Palmer BF. Proteinuria as a therapeutic target in patients with chronic kidney disease. Am J Nephrol 2007;27:287–293 [DOI] [PubMed] [Google Scholar]
- 4.Shapiro H, Theilla M, Attal-Singer J, Singer P. Effects of polyunsaturated fatty acid consumption in diabetic nephropathy. Nat Rev Nephrol 2011;7:110–121 [DOI] [PubMed] [Google Scholar]
- 5.Haines AP, Sanders TA, Imeson JD, et al. Effects of a fish oil supplement on platelet function, haemostatic variables and albuminuria in insulin-dependent diabetics. Thromb Res 1986;43:643–655 [DOI] [PubMed] [Google Scholar]
- 6.Hamazaki T, Takazakura E, Osawa K, Urakaze M, Yano S. Reduction in microalbuminuria in diabetics by eicosapentaenoic acid ethyl ester. Lipids 1990;25:541–545 [DOI] [PubMed] [Google Scholar]
- 7.Jensen T, Stender S, Goldstein K, Hølmer G, Deckert T. Partial normalization by dietary cod-liver oil of increased microvascular albumin leakage in patients with insulin-dependent diabetes and albuminuria. N Engl J Med 1989;321:1572–1577 [DOI] [PubMed] [Google Scholar]
- 8.Lungershausen YK, Howe PR, Clifton PM, et al. Evaluation of an omega-3 fatty acid supplement in diabetics with microalbuminuria. Ann N Y Acad Sci 1997;827:369–381 [DOI] [PubMed] [Google Scholar]
- 9.Mori TA, Burke V, Puddey I, et al. The effects of [omega]3 fatty acids and coenzyme Q10 on blood pressure and heart rate in chronic kidney disease: a randomized controlled trial. J Hypertens 2009;27:1863–1872 [DOI] [PubMed] [Google Scholar]
- 10.Nielsen SE, Hansen HP, Jensen BR, Parving HH, Rossing P. Urinary neutrophil gelatinase-associated lipocalin and progression of diabetic nephropathy in type 1 diabetic patients in a four-year follow-up study. Nephron Clin Pract 2011;118:c130–c135 [DOI] [PubMed] [Google Scholar]
- 11.Rossing P, Hansen BV, Nielsen FS, Myrup B, Hølmer G, Parving HH. Fish oil in diabetic nephropathy. Diabetes Care 1996;19:1214–1219 [DOI] [PubMed] [Google Scholar]
- 12.Vaidya VS, Waikar SS, Ferguson MA, et al. Urinary biomarkers for sensitive and specific detection of acute kidney injury in humans. Clin Transl Sci 2008;1:200–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waikar SS, Bonventre JV. Biomarkers for the diagnosis of acute kidney injury. Curr Opin Nephrol Hypertens 2007;16:557–564 [DOI] [PubMed] [Google Scholar]
- 14.Levey AS, Coresh J, Greene T, et al. Chronic Kidney Disease Epidemiology Collaboration Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 2006;145:247–254 [DOI] [PubMed] [Google Scholar]
- 15.Metherel AH, Armstrong JM, Patterson AC, Stark KD. Assessment of blood measures of n-3 polyunsaturated fatty acids with acute fish oil supplementation and washout in men and women. Prostaglandins Leukot Essent Fatty Acids 2009;81:23–29 [DOI] [PubMed] [Google Scholar]
- 16.Di Stasi D, Bernasconi R, Marchioli R, et al. Early modifications of fatty acid composition in plasma phospholipids, platelets and mononucleates of healthy volunteers after low doses of n-3 polyunsaturated fatty acids. Eur J Clin Pharmacol 2004;60:183–190 [DOI] [PubMed] [Google Scholar]
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502 [PubMed] [Google Scholar]
- 18.Doyle KM, Cluette-Brown JE, Dube DM, Bernhardt TG, Morse CR, Laposata M. Fatty acid ethyl esters in the blood as markers for ethanol intake. JAMA 1996;276:1152–1156 [PubMed] [Google Scholar]
- 19.Sundaram N, Bennett M, Wilhelm J, et al. Biomarkers for early detection of sickle nephropathy. Am J Hematol 2011;86:559–566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller ER, 3rd, Juraschek SP, Appel LJ, et al. The effect of n-3 long-chain polyunsaturated fatty acid supplementation on urine protein excretion and kidney function: meta-analysis of clinical trials. Am J Clin Nutr 2009;89:1937–1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stirban A, Nandrean S, Götting C, et al. Effects of n-3 fatty acids on macro- and microvascular function in subjects with type 2 diabetes mellitus. Am J Clin Nutr 2010;91:808–813 [DOI] [PubMed] [Google Scholar]
- 22.Appel LJ, Miller ER, 3rd, Seidler AJ, Whelton PK. Does supplementation of diet with ‘fish oil’ reduce blood pressure? A meta-analysis of controlled clinical trials. Arch Intern Med 1993;153:1429–1438 [PubMed] [Google Scholar]
- 23.Massaro M, Scoditti E, Carluccio MA, Montinari MR, De Caterina R. Omega-3 fatty acids, inflammation and angiogenesis: nutrigenomic effects as an explanation for anti-atherogenic and anti-inflammatory effects of fish and fish oils. J Nutrigenet Nutrigenomics 2008;1:4–23 [DOI] [PubMed] [Google Scholar]
- 24.Ferraro PM, Ferraccioli GF, Gambaro G, Fulignati P, Costanzi S. Combined treatment with renin-angiotensin system blockers and polyunsaturated fatty acids in proteinuric IgA nephropathy: a randomized controlled trial. Nephrol Dial Transplant 2009;24:156–160 [DOI] [PubMed] [Google Scholar]
- 25.Rizza S, Tesauro M, Cardillo C, et al. Fish oil supplementation improves endothelial function in normoglycemic offspring of patients with type 2 diabetes. Atherosclerosis 2009;206:569–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simopoulos AP, Leaf A, Salem N., Jr Workshop on the essentiality of and recommended dietary intakes for omega-6 and omega-3 fatty acids. J Am Coll Nutr 1999;18:487–489 [DOI] [PubMed] [Google Scholar]
- 27.Yokoyama M, Origasa H, Matsuzaki M, et al. Japan EPA lipid intervention study (JELIS) Investigators Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 2007;369:1090–1098 [DOI] [PubMed] [Google Scholar]
- 28.Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Lancet 1999;354:447–455 [PubMed] [Google Scholar]
- 29.The ORIGIN Trial Investigators. Bosch J, Gerstein HC, et al. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med 2012;367:309–318 [DOI] [PubMed] [Google Scholar]
- 30.Kris-Etherton PM, Harris WS, Appel LJ, American Heart Association. Nutrition Committee Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 2002;106:2747–2757 [DOI] [PubMed] [Google Scholar]
- 31.Manson JE, Bassuk SS, Lee IM, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials 2012;33:159–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartweg J, Perera R, Montori V, Dinneen S, Neil HA, Farmer A. Omega-3 polyunsaturated fatty acids (PUFA) for type 2 diabetes mellitus. Cochrane Database Syst Rev 2008;1:CD003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kelley DS, Adkins Y, Woodhouse LR, Swislocki A, Mackey BE, Siegel D. Docosahexaenoic acid supplementation improved lipocentric but not glucocentric markers of insulin sensitivity in hypertriglyceridemic men. Metab Syndr Relat Disord 2012;10:32–38 [DOI] [PubMed] [Google Scholar]