Abstract
The purpose of this study was to examine the test-retest reliability of normalization methods for the infraspinatus muscle in a group of healthy subjects. Twelve healthy subjects (male=8, female=4) performed the maximal voluntary isometric contraction (MVIC) with examiner`s resistance, MVIC with a digital tension-meter (MVIC-DT), and sub-MVIC methods. Surface electromyography (EMG) signals were recorded from the infraspinatus muscles according to normalization methods. Reliability was analyzed using the intra-class coefficient (ICC), standard error of measurement (SEM), and minimal detectable difference (MDD). The results of the present study demonstrated that the sub-MVIC method has excellent test-retest reliability (ICC=0.92) with a relatively small SEM (5.9 mV) and MDD95 (16.4 mV), compared to MVIC-DT (ICC=0.73; SEM=11.2 mV; MDD95: 31 mV) and MVIC-E (ICC=0.5; SEM=15.7 mV; MDD95: 43.6 mV). These findings provide evidence that sub-MVIC is more appropriate for comparing the EMG activity for the infraspinatus muscle as a normalization method. If MVIC for normalization is needed, MVIC-DT is more appropriate than MVIC-E.
Keywords: electromyography, infraspinatus muscle, normalization, reliability
Introduction
The infraspinatus muscle produces an approximation force to resist distraction during an overhead throwing motion (Ballantyne et al., 1993). Also, the infraspinatus provides the primary external rotation force (Terry and Chopp, 2000). Because of its critical role in providing dynamic stability and producing external rotation torque at shoulder joint, many authors have advocated emphasis on infraspinatus muscle strengthening during rehabilitation or athletic conditioning programs in order to enhance muscular strength and endurance (Blackburn et al., 1990; Brewster and Schwab, 1993; Reinold et al., 2004; Townsend et al., 1991).
Previous studies were conducted using surface electromyography (EMG) to measure the muscle activity of infraspinatus through EMG studies in a variety of exercises (Ballantyne et al., 1993; Reinold et al., 2004). A major limitation of kinesiologic EMG research is the difficulty in making comparisons between EMG values obtained from identical muscles in different subjects, different muscles from the same subject, or even the same muscle from the same subject on different days. These difficulties may be due to subtle differences in muscle architecture, electrode placement, and electrode construction (Giroux and Lamontagne, 1990; Jonsson and Komi, 1973; Kadaba et al., 1985). To overcome these shortcomings of surface EMG, the concept of normalization has been developed to enable comparing EMG signal (Mirka, 1991).
Numerous studies have been performed using maximal voluntary isometric contraction (MVIC) normalization method to identify effect of exercises or intervention for infraspinatus muscle strengthening (Ballantyne et al., 1993; Bitter et al., 2007; Ekstrom et al., 2003). The MVIC normalization technique is the use of the maximal voluntary contraction of a predetermined isometric movement as the reference EMG signal (Hagberg and Sundelin, 1986; Yang and Winter, 1983). The MVIC has the advantage of having a physiological meaning where derived data are expressed relative to the maximum (Allison et al., 1998). To produce MVIC, resistances of examiner’s hand or digital tension-meter (DT) have been used as a common method (Kendall and McCreary, 2005; Netto and Burnett, 2006). As the reference value for normalization, MVIC may account for much of the potential variability among recording factors (e.g. skin impedance, electrode position, collection methods and devices, electrode size and pick-up area, etc.). However, the reproducibility of this reference point depends on subject`s level of sincerity, motivation, or pain during the exertion. The subjective nature of these exertions may introduce some level of experimental error (Marras and Davis, 2001). Larivière et al. (2002) demonstrated that between-day reliability of MVIC method was poor in the comparison of EMG activities for the back muscles between healthy control subjects and chronic patients with low back pain.
To address these limitations, sub-MVIC is frequently used as a predetermined reference value when MVIC are limited by aging, pain or other symptoms (Allison et al., 1998; Dankaerts et al., 2004; Marras and Davis, 2001). This approach is limited by the difficulty of establishing equivalent sub-maximal loads for different muscles (Allison et al., 1998). To establish equivalent sub-maximal loads, the estimation of the expected maximum contraction, 60% MVIC using isokinetic dynamometer was used to predict a reference point to be used for normalization in the neck and trunk muscles (Burnett et al., 2007; Dankaerts et al., 2004; Marras and Davis, 2001; Netto and Burnett, 2006). Previous studies reported that sub-MVIC are more reliable and are more sensitive than MVIC when assessing low levels of abdominal muscle activities (Allison et al., 1998; O’Sullivan et al., 1998). Also, Sub-MVIC has been reported to be reliable within-day reliability in healthy subjects when assessing EMG for abdominal wall muscles (Allison et al., 1998; O’Sullivan et al., 1998). However, there is no attempt to investigate sub-MVIC for the infraspinatus muscle, compared to MVIC.
Therefore, the purpose of this study was to examine the reliability of normalization methods for the infraspinatus muscle in a group of healthy subjects. Specifically, MVIC with examiner`s resistance (MVIC-E) as a common method, MVIC with digital tension-meter (MVIC-DT), and sub-MVIC methods were examined. The hypothesis of this study was that sub-MVIC method would more reliable than other normalization method.
Material and Methods
Twelve healthy subjects (male=8, female=4) were recruited from the university populations. The characteristics of the subjects are presented in Table 1. There were significant differences in physical characteristics between males and females. Inclusion criteria were 1) ability to perform full shoulder external rotation comfortably, 2) manual muscle testing (MMT) grade was 5/5 (Hislop and Montgomery, 2002; Kendall and McCreary, 2005). Exclusion criteria were past or present neurological, musculoskeletal, or cardiopulmonary diseases that could interfere with shoulder external rotation in the testing position. Before the study, the principal investigator explained all procedures to the subjects in detail. All subjects signed an informed consent form, which was approved by the Yonsei University Wonju Campus Human Studies Commities.
Table 1.
Characteristics of the subjects (N=12)
| Total | Male (n=8) | Female (n=4) | p | |
|---|---|---|---|---|
| Body height (cm) | 170.7 ± 7.3 | 174.9 ± 4.5 | 162.3 ± 2.1 | 0.00 |
| Body mass (kg) | 68.5 ± 15.5 | 76.6 ± 12.2 | 52.3 ± 1.7 | 0.03 |
| Age (years) | 26.0 ± 4.5 | 29.0 ± 3.1 | 21.3 ± 0.5 | 0.01 |
EMG data were collected using a Noraxon TeleMyo 2400T and analyzed using MyoResearch Master Edition 1.06 XP software (Noraxon Inc., Scottsdale, AZ, USA). Skin preparation of electrode sites involved shaving and cleaning with rubbing alcohol. Surface electrode pairs were positioned at an interelectrode distance of 2 cm. The reference electrode was placed on the ipsilateral clavicle. EMG data were collected for the infraspinatus muscle (4 cm below the spine of the scapula, on the lateral aspect over the infrascapular fossa of the scapula) (Cram et al., 1998). The raw signal was full wave rectified and filtered using a Lancosh FIR digital filter. The bandpass filter was used between 20 Hz and 300 Hz. The EMG data were processed into the root mean square (RMS) value, which was calculated from 50-ms windows of data points.
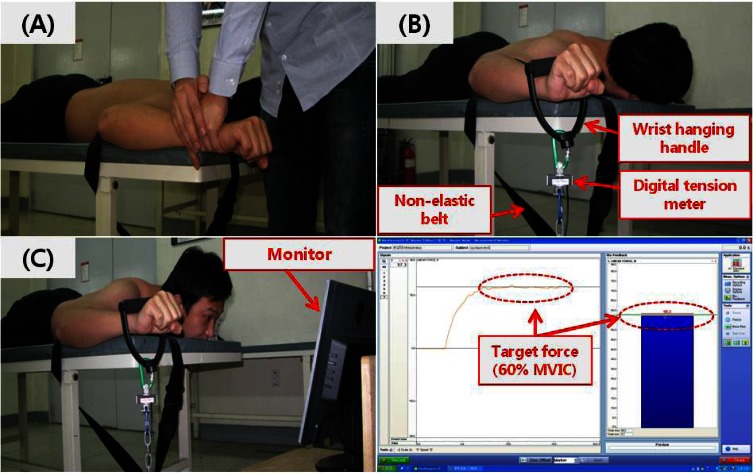
The digital tension-meter using linear force measurement load cell (Noraxon Inc., Scottsdale, AZ, USA) was used to measure maximal force and 60%-maximal force (kg) in the infraspinatus muscle. The force data were collected using a Noraxon TeleMyo 2400T and MyoResearch Master Edition 1.06 XP software (Noraxon Inc., Scottsdale, AZ, USA). The target force to calculate 60%-MVIC (sub-MVIC) was determined based on the maximal force value using digital tension-meter. The sampling rate was 1000 Hz. The digital tension-meter was calibrated prior to each set of measurement (Figure 1).
Figure 1.
Testing Position: A: MVIC-E (maximal voluntary isometric contraction with examiner’s resistance); B: MVIC-DT (maximal voluntary isometric contraction with digital tension-meter); C: Sub-MVIC (sub-maximal voluntary isometric contraction)).
Procedures
The dominant arm (the tendency to prefer a particular arm in performing selected tasks) was tested in all subjects (Yoshizaki et al., 2009). Recent findings have suggested that the determination of a dominant arm was based on hand-path kinematics and muscle activity in performing selected tasks (Bagesteiro and Sainburg, 2002). However, our study used a questionnaire to self-report arm dominance (ex. Daily-use dominant arm). Their self-reported dominant arms were right in all subjects.
Testing position required the subject to lay prone with the shoulder abducted at 90° and the elbow flexed to 90°, while the forearm in neutral position (Kendall and McCreary, 2005). Then, the subject moved to a position of shoulder external rotation to 90°. In a pilot study, isometric external rotation at 0° and 90° shoulder abduction were chosen because these positions are known to generate high levels of activity in the infraspinatus muscle (Kronberg et al., 1990; Jenp et al., 1996; Reinold et al., 2004). Standing or sitting external rotation at 0° and 90° shoulder abduction had a compensatory trunk motion compared to the prone position. Therefore, the prone position with the shoulder abducted at 90° was chosen. Additionally, the subject`s elbow was fastened to the table using a non-elastic belt to prevent compensatory shoulder motion (Figure 1). Subjects were familiarized with each normalization trials during the 30 min period prior to testing. The familiarization period was completed when the subject was able to maintain three normalization methods for 5 s. All of the subjects were comfortable after the familiarization period, and none reported fatigue. A 15 min rest period was allowed after familiarization period before data collection began. The order of testing was randomized using random number generator (Microsoft Corp., Redmond, WA, USA), except for sub-MVIC. Sub-MVIC was calculated after MVIC-DT trial.
Three different testing methods were examined in this study (Figure 1). For the MVIC-E trial, subjects performed the maximal contraction of the dominant side arm by applying a manual resistance of an examiner to the subject`s wrist. All subjects were given consistent verbal encouragement during maximal contraction. For the MVIC-DT trial, each subject performed a maximal contraction of the dominant side arm using a wrist hanging handle. The handle was connected to the digital tension-meter. After MVIC-DT trial, a sub-MVIC value was calculated to 60% MVIC-DT force (Netto and Burnett, 2006). For the sub-MVIC trials, subjects were provided with visual feedback from a computer monitor that was positioned directly in the subject’s line of sight to assist them in achieving the desired level of contraction. Each trial being performed incorrectly was stopped and repeated. If the subject performed the test incorrectly over 5 times, he or she was asked to rest 1 hour to prevent learning effects.
Physiological recovery was facilitated by allowing a 2 min recovery between normalization trials (Burnett et al., 2007). EMG activity was measured during each normalization trials for 5 s. The first and last second of the EMG data from each trial were discarded, and the remaining 3 s of data were used for further analysis (Reinold et al., 2004). An hour after the first session, the subject performed the second session following the identical protocol.
Statistical analysis
A repeated measure ANOVA was used to determine if there was systemic bias (for confirming the learning effects) between the first and second trial. Reliability of normalization methods in the infraspinatus muscle was calculated to determine the within-subject variation using two indices of reliability; ICC (3,1), the standard error of measurement (SEM). ICC values were calculated using the Statistical Package for Social Sciences, Version 12.0 (SPSS Inc, Chicago, IL). ICC is commonly used to assess test–retest reliability and reflects the relative reliability of a measurement. ICC >0.75 is considered excellent, 0.40–0.75 is regarded as fair to good, and 0–0.4 as poor (Crossley et al., 2004). To examine the consistency of the measurement, the SEM was calculated using Microsoft Excel [SEM = standard deviation*(1-ICC)1/2]. Minimal detectable difference (95% confidence interval) (MDD95) scores were calculated [MDD95 = SEM × √2 × 1.96] (Ries et al., 2009). MDD95 scores using a Microsoft Excel (set at a 5 % significance level) were calculated for the three normalization methods.
Results
There were no significant differences (p >0.05) between the first and second test session in all of the normalization methods. These results indicated that the learning effect did not occur between test sessions. The same day test–retest ICC scores, SEM, and MDD95 for the EMG recordings from the infraspinatus muscle during each normalization test are documented in Table 2. The maximal and sub-MVIC force data using digital tension meter are presented in Table 3.
Table 2.
Test-retest ICC scores, SEM, and MDD95 among three methods.
| MVIC-E | MVIC-DT | Sub-MVIC | |
|---|---|---|---|
| ICC | 0.42 | 0.73 | 0.98 |
| SEM | 14.5 mV | 6.3 mV | 1.3 mV |
| MDD95 | 40.3 mV | 17.3 mV | 3.5 mV |
ICC = intraclass correlation coefficient; MDD = minimal detectable difference; SEM = standard error of measurement; MVIC-E = maximal voluntary isometric contraction with examiner`s resistance; MVIC-DT = maximal voluntary isometric contraction with digital tension-meter; Sub-MVIC = sub-maximal voluntary isometric contraction.
Table 3.
The force data using a digital tension meter.
| MVIC-DT | Sub-MVIC | |||
|---|---|---|---|---|
|
| ||||
| 1st trial | 2nd trial | 1st trial | 2nd trial | |
| Force (kg) | 56±14.9 | 54.1±15.4 | 32.4±8.2 | 32.3±8.5 |
MVIC-DT = maximal voluntary isometric contraction with digital tension-meter; Sub-MVIC = sub-maximal voluntary isometric contraction.
Discussion
The purpose of this study was to determine optimal normalization methods for the infraspinatus muscle in healthy subjects. The results of present study demonstrated that the sub-MVIC method has excellent test-retest reliability (ICC = 0.98) with a relatively small SEM (1.3 mV) and MDD95 (3.5 mV), compared to MVIC-DT (ICC = 0.73; SEM = 6.3 mV; MDD95: 17.3 mV) and MVIC-E (ICC = 0.42; SEM = 14.5 mV; MDD95: 40.3 mV). Consistent with results of the present study, it has been previously reported that sub-MVIC methods were more reliable than MVIC in healthy controls when examining EMG data from biceps femoris and triceps muscles (Allison et al., 1993; Yang and Winter, 1983).
Several possible explanations exist for our results. First, providing visual bio-feedback at the reference point (60% MVIC torque) may have reduced the variability of measurement in the sub-MVIC method, compared with no visual feedback (MVIC-DT and MVIC-E). Previous studies suggested that providing visual feedback through monitor at the reference point markedly increased the reliability of the normalization method in the sub-MVIC (60% MVIC) (Burnett et al., 2007; Netto and Burnett, 2006). Second, the differences between MVIC-DT and MVIC-E are influenced by methods of applying resistance. Although the same investigator applied manual resistance during the MVIC-E, the use of manual resistance is a potential source for variability (Dankerts et al., 2004). In contrast to MVIC-E, MVIC-DT is applied by fixed wrist hanging handle. During the measurement of MVIC, this method is useful for reducing variability introduced by the manual resistance method. Thus, MVIC-DT has higher reliability with a relatively small SEM and MDD95 than MVIC-E.
Although MVIC is the most commonly used normalization technique, the MVIC may vary depending upon the sincerity, motivation or pain level of the individual. This variability may result in substantial MVIC variability and influence the interpretation of the EMG signal (Marras and Davis, 2001). Also, it is limited in application because it applies only to healthy subjects and requires substantial rest periods and thus, significant time. MVIC techniques would also have limited utility when evaluating individuals who are suffering from pain since they may not be willing to generate “true” MVICs (Baratta et al., 1998). Lund et al. (1991) reported that pain reduces maximal muscle activation, but has no influence on sub-maximal muscle activation in patients with musculoskeletal pain. Therefore, we suggest that sub-MVIC is appropriate for normalization during EMG studies, compared to MVIC. If MVIC for normalization is needed, MVIC-DT is more optimal than MVIC-E.
The present study had some limitations. First, our results are not widely generalizable because all of our subjects were the healthy males. Thus, additional research is needed to establish whether our findings apply to subjects with shoulder pain as well as female subjects. Second, we did not measure between-day reliability. Between-days reliability becomes critical when assessing EMG parameters that are used as outcome measures (Elfving et al., 1999). However, it has been suggested that replacing the electrodes may be a major source of between-days test–retest variance, even if these are intended to be identically re-positioned (Veiersted, 1991). In conclusions, the present study demonstrated that sub-MVIC method using a providing visual bio-feedback at the reference point (60% MVIC torque) has excellent test-retest reliability in the infraspinatus muscle, compared to MVIC methods. This study also demonstrated that MVIC-DT is more reliable than MVIC-E. These findings provide evidence that sub-MVIC is more appropriate for comparing the EMG activity for the infraspinatus muscle as a normalization method. If MVIC for normalization is needed, MVIC-DT is more appropriate than MVIC-E.
Acknowledgments
We deny any conflicts of interest including personal, financial, or other related to our submitted manuscript titled “Reliability of Electromyographic Normalization Methods for the Infraspinatus Muscle in Healthy Subjects.”
References
- Allison GT, Godfrey P, Robinson G. EMG signal amplitude assessment during abdominal bracing and hollowing. J Electromyogr Kinesiol. 1998;8:51–57. doi: 10.1016/s1050-6411(97)00004-7. [DOI] [PubMed] [Google Scholar]
- Bagesteiro LB, Sainburg RL. Handedness: dominant arm advantages in control of limb dynamics. J Neurophysiol. 2002;88:2408–2421. doi: 10.1152/jn.00901.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballantyne BT, O’Hare SJ, Paschall JL, Pavia-Smith MM, Pitz AM, Gillon JF, Soderberg GL. Electromyographic activity of selected shoulder muscles in commonly used therapeutic exercises. Phys Ther. 1993;73:668–677. doi: 10.1093/ptj/73.10.668. [DOI] [PubMed] [Google Scholar]
- Baratta RV, Solomonow M, Zhou BH, Zhu M. Methods to reduce the variability of EMG power spectrum estimates. J Electromyogr Kinesiol. 1998;8:279–285. doi: 10.1016/s1050-6411(97)00031-x. [DOI] [PubMed] [Google Scholar]
- Bitter NL, Clisby EF, Jones MA, Magarey ME, Jaberzadeh S, Sandow MJ. Relative contributions of infraspinatus And deltoid during external rotation in healthy shoulders. J Shoulder Elbow Surg. 2007;16:563–568. doi: 10.1016/j.jse.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Blackburn TA, McLeod WD, White B, Woford I. EMG analysis of posterior rotator cuff exercises. Athl Train. 1990;25:40–45. [Google Scholar]
- Brewster C, Schwab DR. Rehabilitation of the shoulder following rotator cuff injury or surgery. J Orthop Sports Phys Ther. 1993;18:422–426. doi: 10.2519/jospt.1993.18.2.422. [DOI] [PubMed] [Google Scholar]
- Burnett A, Green J, Netto K, Rodrigues J. Examination of EMG normalisation methods for the study of the posterior and posterolateral neck muscles in healthy controls. J Electromyogr Kinesiol. 2007;17:635–641. doi: 10.1016/j.jelekin.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Cram JR, Kasman GS, Holtz J. Introduction to surface electromyography. 1st ed. Gaithersburg (MD): Aspen Publishers; 1998. p. 287. [Google Scholar]
- Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815–822. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- Dankaerts W, O’Sullivan PB, Burnett AF, Straker LM, Danneels LA. Reliability of EMG measurements for trunk muscles during maximal and sub-maximal voluntary isometric contractions in healthy controls and CLBP patients. J Electromyogr Kinesiol. 2004;14:333–342. doi: 10.1016/j.jelekin.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2000;33:247–258. doi: 10.2519/jospt.2003.33.5.247. [DOI] [PubMed] [Google Scholar]
- Elfving B, Németh G, Arvidsson I, Lamontagne M. Reliability of EMG spectral parameters in repeated measurements of back muscle fatigue. J Electromyogr Kinesiol. 1999;9:235–243. doi: 10.1016/s1050-6411(98)00049-2. [DOI] [PubMed] [Google Scholar]
- Ellenbecker TS, Mattalino AJ. Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. J Orthop Sports Phys Ther. 1997;25:323–328. doi: 10.2519/jospt.1997.25.5.323. [DOI] [PubMed] [Google Scholar]
- Giroux B, Lamontagne M. Comparisons between surface electrodes and intramuscular wire electrodes in isometric and dynamic conditions. Electromyogr Cin Neurophysiol. 1990;30:397–405. [PubMed] [Google Scholar]
- Hagberg M, Sundelin G. Discomfort and load on the upper trapezius muscle when operating a wordprocessor. Ergonomics. 1986;29:1637–1645. doi: 10.1080/00140138608967275. [DOI] [PubMed] [Google Scholar]
- Hislop H, Montgomery J. Muscle testing and function. 7th ed. Philadelphia: WB Saunders; 2002. [Google Scholar]
- Jenp YN, Malanga GA, Growney ES, An KN. Activation of the rotator cuff in generating shoulder rotation torque. Am J Sports Med. 1996;24:477–485. doi: 10.1177/036354659602400412. [DOI] [PubMed] [Google Scholar]
- Jonsson B, Komi PV. Reproducibility problems when using wire electrodes in electromyographic kinesiology. New Developments in Electromyography und Clinical Neurophysiology. 1973;1:540–546. [Google Scholar]
- Kadaba MP, Wootten ME, Gainey J, Cochran GV. Repeatability of phasic muscle activity: performance of surface and intramuscular wire electrodes in gait analysis. J Orthop Res. 1985;3:350–359. doi: 10.1002/jor.1100030312. [DOI] [PubMed] [Google Scholar]
- Kendall FP, McCreary EK. Muscles: Testing and Function. 5th ed. Baltimore, MD: Williams & Wilkins; 2005. [Google Scholar]
- Kronberg M, Nemeth G, Brostrom LA. Muscle activity and coordination in the normal shoulder. An electromyographic study. Clin Orthop. 1990;257:76–85. [PubMed] [Google Scholar]
- Larivière C, Arsenault AB, Gravel D, Gagnon D, Loisel P. Evaluation of measurement strategies to increase the reliability of EMG indices to assess back muscle fatigue and recovery. J Electromyogr Kinesiol. 2002;12:91–102. doi: 10.1016/s1050-6411(02)00011-1. [DOI] [PubMed] [Google Scholar]
- Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol. 1991;69:683–694. doi: 10.1139/y91-102. [DOI] [PubMed] [Google Scholar]
- Marras WS, Davis KG. A non-MVC EMG normalization technique for the trunk musculature: Part 1. Method development. J Electromyogr Kinesiol. 2001;11:1–9. doi: 10.1016/s1050-6411(00)00039-0. [DOI] [PubMed] [Google Scholar]
- Mirka GA. The quantification of EMG normalization error. Ergonomics. 1991;34:343–352. doi: 10.1080/00140139108967318. [DOI] [PubMed] [Google Scholar]
- Netto KJ, Burnett AF. Reliability of normalisation methods for EMG analysis of neck muscles. Work. 2006;26:123–130. [PubMed] [Google Scholar]
- O’Sullivan PB, Twomey L, Allison GT. Altered abdominal muscle recruitment in patients wih chronic back pain following a specific exercise intervention. J Orthop Sports Phys Ther. 1998;27:114–124. doi: 10.2519/jospt.1998.27.2.114. [DOI] [PubMed] [Google Scholar]
- Reinold MM, Wilk KE, Fleisig GS, Zheng N, Barrentine SW, Chmielewski T, Cody RC, Jameson GG, Andrews JR. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34:385–394. doi: 10.2519/jospt.2004.34.7.385. [DOI] [PubMed] [Google Scholar]
- Ries JD, Echternach JL, Nof L, Gagnon Blodgett M. Test-retest reliability and minimal detectable change scores for the timed ‘up & go’ test, the six-minute walk test, and gait speed in people with Alzheimer disease. Phys Ther. 2009;89:569–579. doi: 10.2522/ptj.20080258. [DOI] [PubMed] [Google Scholar]
- Terry GC, Chopp TM. Functional anatomy of the shoulder. J Athl Train. 2000;35:248–255. [PMC free article] [PubMed] [Google Scholar]
- Townsend H, Jobe FW, Pink M, Perry J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1991;19:264–272. doi: 10.1177/036354659101900309. [DOI] [PubMed] [Google Scholar]
- Veiersted KB. The reproducibility of test contractions for calibration of electromyographic measurements. Eur J Appl Physiol Occup Physiol. 1991;62:91–98. doi: 10.1007/BF00626762. [DOI] [PubMed] [Google Scholar]
- Yang JF, Winter DA. Electromyography reliability in maximal and submaximal isometric contractions. Arch Phys Med Rehabil. 1983;64:417–420. [PubMed] [Google Scholar]
- Yoshizaki K, Hamada J, Tamai K, Sahara R, Fujiwara T, Fujimoto T. Analysis of the scapulohumeral rhythm and electromyography of the shoulder muscles during elevation and lowering: comparison of dominant and nondominant shoulders. J Shoulder Elbow Surg. 2009;18:756–763. doi: 10.1016/j.jse.2009.02.021. [DOI] [PubMed] [Google Scholar]