Abstract
Strong associations between radiographic features of knee OA and pain have been demonstrated in persons with unilateral knee symptoms. Our objectives were to compare radiographic with MRI features of knee OA and assess the discrimination between painful and non-painful knees in persons with unilateral symptoms.
283 individuals with unilateral knee pain aged 71 to 80 years from Health ABC, a study of weight-related diseases and mobility, had bilateral knee radiographs, read for KL grade and individual radiographic features, and 1.5T MRIs, read using WORMS. The association of structural features with pain was assessed using a within-person case/control design and conditional logistic regression. Receiver operator characteristics (ROC) were then used to test the discriminatory performance of structural features.
In conditional logistic analyses, knee pain was significantly associated with both radiographic (any JSN grade >=1: OR 3.20 (1.79 – 5.71) and MRI (any cartilage defect:>=2: OR 3.67 (1.49 – 9.04)) features. However, most subjects had MR detected osteophytes, cartilage and bone marrow lesions in both knees and no individual structural feature discriminated well between painful and non-painful knees using ROC. The best performing MRI feature (synovitis/effusion) was not significantly more informative than KL grade >=2 (p=0.42).
In persons with unilateral knee pain, MR and radiographic features were associated with knee pain confirming an important role in the etiology of pain. However, no single MRI or radiographic finding performed well in discriminating painful from non-painful knees. Further work is needed to examine how structural and non-structural factors influence knee pain.
Introduction
Knee osteoarthritis (OA) poses a significant global health burden, ranked 6th among all conditions by the WHO as a cause of moderate and severe disability 1. Pain is the principal symptom but our understanding of the mechanisms involved in pain is incomplete. While there are well established reproducible methods for grading radiographic structural features in OA 2,3, associations in epidemiological studies between structural features using these methods and symptoms have been modest 4,5. Even in studies reporting significant associations between structure and symptoms, 51% of those with knee pain for more than one year did not have radiographic knee OA 6. Equally important, up to 50% of patients with radiographic changes of OA have no symptoms. This suggests that radiographic features of OA have a very limited ability to discriminate between painful and non-painful knees in the general population.
Possible reasons for the modest associations and poor discrimination include: the insensitivity of radiographyto detect structural features of OA; and uncontrolled differences in pain susceptibility and other person level determinants of OA symptoms that confound and obscure structure – pain relationships7.
Two recent developments address these limitations. MR imaging (MRI) of the knee has enabled the measurement of structural features in three dimensions with direct assessment of cartilage damage and other structural features of OA not seen on radiographs that may cause pain, including effusions, synovitis and edema in subchondral bone 8. Secondly, to control for person-level confounders, a recent study used examined subjects with unilateral knee pain and performing a within-person matched comparison of structural features of OA between the knee with, and the knee without, pain 9. In this study, radiographic structural features of OA such as the Kellgren and Lawrence (KL) grade, and the maximum joint space narrowing (JSN) score were very strongly associated with the presence of pain in one knee but not the other, with OR for pain of 9.0 for K-L grade 3 vs. K-L grade 0 knees, for example. Still, in this study half of the subjects had the same K-L grade in the symptomatic and control knees and 31% had a K-L grade of 0 in both knees.
In this study our objectives were to confirm in another cohort the strong association of x-ray findings of OA in a between knee comparison of subjects with unilateral knee pain, to extend this analysis to MRI findings of knee OA, and finally to examine, and compare, the ability of MRI and x-ray findings using marginal models and ROC analysis to discriminate between painful and non-painful knees in all subjects with unilateral pain.
Methods
STUDY POPULATION
The study sample was drawn from the Health, Aging and Body Composition (Health ABC) Study, a prospective cohort study of the effects of weight-related diseases on mobility. The study recruited 3075 black and white men and women aged 70–79 years between April 1997 to June 1998 from the white Medicare beneficiaries and all age-eligible community-dwelling black residents in designated ZIP codes surrounding two field sites, University of Pittsburgh, Pennsylvania and University of Tennessee, Memphis, Tennessee.
Subjects were eligible for Health ABC if they reported no difficulty walking mile, climbing 10 steps, performing basic activities of daily living, no use of special equipment for ambulation, no history of cancer in previous three years and no plan to move from the area for three years. Clinical examination and interview data were collected at baseline then annually.
At the year two clinic visit participants with knee pain underwent bilateral radiographic and MRI examinations of the knee. Side-specific knee symptoms were assessed using questions about whether the participant had “pain, aching or stiffness on most days” for at least one month in the past 12 months. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scale was also administered, asking about knee pain during various activities in the past 30 days (15). Each knee was categorized as having significant symptoms, defined as a report of any of the following in that knee: moderate, severe, or extreme (2, 3, or 4) pain during the last 30 days when walking on flat surface, going up or down stairs, at night in bed, standing upright, getting in/out of chair or getting in/out of car; knee pain lasting ≥1 month in the past 12 months; or knee pain for most days in the past month. Hereafter, we use the term ‘knee pain’ to refer to knees with significant symptoms as defined here, and ‘no knee pain’ to refer to knees without significant symptoms. Bilateral knee imaging was obtained in participants with significant symptoms in at least one knee.
IMAGE ACQUISITION
Weight-bearing PA fixed flexion radiographs were obtained of both knees using a positioning frame (Syna-Flexer; Synarc, San Francisco, CA) in order to fix knee flexion between 20° and 30° and external rotation of the feet at 10° 10,11. Standing skyline views were also obtained of both knees with an angle of flexion of 30 to 40 degrees 12.
The following MRI sequences were performed on both knees using a Signa 1.5T MRI system with a standard unilateral, commercial circumferential knee coil: coronal (T2-weighted fast spin-echo (FSE) (TR 3,500 msec, TE 60 msec) with a slice thickness of 4 mm, a 0.5-mm interslice gap, 2 excitation, FOV 14 cm, and a matrix of 256 × 256 pixels), sagittal (T2-weighted FSE, including the entire synovial cavity with frequency-selective fat suppression (TR 4,127 msec, TE 60 msec), a 0.5-mm interslice gap, 2 excitation, with the same FOV and matrix), and axial images were obtained and axial (T2-weighted FSE (TR 2,500 msec, TE 60 msec) with a 1-mm interslice gap, 1 excitation, FOV 12 cm, and a matrix of 256 × 256 pixels.
IMAGE READING
Radiograph films were read by one of two expert readers for K-L grade and individual radiographic features (joint space narrowing (JSN), osteophytes, subchondral attrition, cysts and sclerosis) were scored using the Osteoarthritis Research Society International atlas in the medial and lateral compartment of the tibio-femoral joint and the patello-femoral joint 13 from the PA and skyline projections respectively. The weighted kappas for inter-rater reliability of ordinal scores were 0.87 for KL grade and 0.75 for osteophytes and 0.90 for JSN.
The MRIs of the knee were read blinded to radiographic scoring by one of 5 trained radiologists using the semi-quantitative whole-organ MRI scoring (WORMS) method of Peterfy et al.14. Specifically, 14 sub-regions (anterior, central, and posterior of the medial/lateral femoral condyles/tibial plateaus and medial/lateral sub-regions of the patella) were each scored separately for cartilage lesion, osteophytes, sub-articular bone marrow lesions (BML), bone cysts and bone attrition. The tibial sub-spinous sub-region, the site of cruciate ligament insertion, was scored for BML and cysts. As these were non-contrast images, synovial thickening and effusion were scored together as ‘synovitis/effusion’.
Cartilage lesions were scored 0–6 for severity. As a grade 1 cartilage lesion (signal abnormality) did not reflect a morphological change it was grouped with grade 0 for analysis. Osteophytes were scored 0 – 7 for size; as grade 1 osteophtyes were those considered equivocal, we grouped it with grade 0. BMLs and subchondral cysts were each scored on 0 – 3 scales for lesion size and subchondral bone attrition on a 0–3 scale for severity. Synovitis/effusion scores were grade 0=normal, 1= <33%, 2=33–66% and 3=>66% of the maximum potential distension. Choosing thresholds for lesion scores based on clinical judgment, we categorized each sub-region as normal vs. having any abnormality (lesion present) for each feature and we further classified each sub-region as having a severe abnormality present vs. normal or mild-moderate abnormality present (See Table 1 for cut points used) 15.
Table 1.
Thresholds used in defining the presence of any abnormality and severe abnormality in any compartment of the knee for radiographic and MRI derived measures of structural damage
| Pathologic features | Scale range | Any Abnormality | Severe Abnormality |
|---|---|---|---|
| Radiographic: | |||
| Joint space narrowing | 0–3 | ≥1 | ≥2 |
| Osteophytes | 0–3 | ≥1 | ≥2 |
| Sclerosis | 0–3 | ≥1 | ≥2 |
| Attrition | 0–3 | ≥1 | ≥2 |
| Cysts | 0–3 | ≥1 | ≥2 |
| KL grade | 0–3 | ≥1 | ≥3 |
| MRI: | |||
| Cartilage damage (CRT) | 0–6 | ≥21 | ≥51 |
| Osteophytes (OST) | 0–7 | ≥22 | ≥42 |
| BMLs | 0–3 | ≥13 | ≥23 |
| Cysts | 0–3 | ≥13 | ≥23 |
| Attrition | 0–3 | ≥14 | ≥24 |
| Synovitis/effusion | 0–3 | ≥15 | ≥25 |
Abnormal: any partial thickness or full thickness defect. Severe: full thickness defect > 1cm maximum width.
Abnormal: ≥ a small horizontal or curved spur. Severe: ≥ large horizontal spur or ≥ moderate size curved spur.
Abnormal: presence of one or more lesions of any size. Severe: lesions occupy ≥ 25% of a sub-region.
Abnormal: Mild or worse deviation from expected bony contour. Severe: moderate or worse deviation.
Abnormal: any distension of joint capsule. Severe: ≥ 33% of the maximum potential distension.
Inter-reader reliability in 29 knees for both compartment-specific and total knee scores for all individual MRI features was good, with intra-class correlation coefficients for cartilage damage of 0.71–0.93, 0.84–0.92 for osteophytes, 0.46–0.81 for bone marrow lesions, 0.54 – 0.77 for bone attrition, and 0.45–0.82 for subchondral bone cysts.
DATA ANALYSIS
Consistent with previously used approaches for summarizing or combining WORMS scores of a given feature over different subregions of a knee 16–18, 19,20,21, 21,22 we used the highest score for each feature in any of its constituent sub-regions as the score for a compartment and in any compartment for the whole knee. Compartments and the whole knee were then categorized as having any abnormality present and as having a severe abnormality based on the thresholds in Table 115. In a sensitivity analysis, we repeated this classification excluding lesions in the patello-femoral compartment. This did not change our basic findings.
These analyses include only subjects who are discordant for pain between their two knees. The standard analysis for within person comparisons between knees in this type of study design is conditional logistic regression modeling, which derives an odds ratio for the association of the presence of structural abnormalities with pain based on the ratio of the number of subjects with the structural feature in the painful knee only to subjects with the structural feature in the painless knee only. A limitation of this analysis is that subjects whose knees are discordant for pain but concordant for structural features, i.e. with a structural feature in both knees or with the feature in neither knee, are treated as “non-informative” and do not affect the OR estimate.
To determine how well individual structural findings discriminate between painful and non-painful knees in all subjects with unilateral pain, we combined all the knees of those who were informative and non-informative for further analysis. We then evaluated the association between the presence of structural findings and pain in this sample by calculating the marginal odds ratios. Next we determined the ability of the full range of each of the features to discriminate painful from non-painful knees using receiver operator curves (ROC)23. We also compared the areas under the curve for different features, focusing the comparison on radiographic vs. MRI features of the same type. To account for clustering of knees within person we used a cluster resampled bootstrap with 1000 replicates to calculate confidence intervals for differences in the area under the curve (AUC) from the ROC and comparisons between AUC for different features 24.
RESULTS
Of the 636 participants in the Health ABC knee OA study with both radiographic and MRI images in both knees, 283 had unilateral knee pain, 263 had bilateral knee pain and 90 had no pain. Compared with the remainder of the cohort, those with unilateral pain were of similar age, body mass index (BMI) and gender (Table 2). As expected, compared with those with unilateral knee pain, there was more radiographic damage in those with bilateral knee pain and less in those with no knee pain. In those with unilateral knee pain, K&L grade ≥2 findings were present in 50% of the painful knees and 36% of the non-painful knees, while K&L grade 3–4 was present in 44% of painful and 28% of non-painful knees.
Table 2.
Description of study participants
| Participant and knee characteristics | Full cohort (n=636) | Participants with discordant knee pain (n=283) | Participants without discordant knee pain† (n=353) | p-value |
|---|---|---|---|---|
| Age (years), median (IQR) | 73 (71,76) | 73 (71,76) | 73 (71,76) | 0.787 |
| BMI (kg/m2), mean (SD) | 28.1 (4.6) | 28.0 (4.4) | 28.2 (4.7) | 0.318 |
| Sex | ||||
| Female, % | 64.5% | 60.4% | 67.7% | 0.057 |
| Male, % | 35.5% | 39.6% | 32.3% | |
| Race, % white | 53.1% | 56.5% | 50.4% | 0.125 |
| Painful knee | ||||
| Left, % painful | 64.3% | 51.6% | 74.5% | <0.0005 |
| Right, % painful | 62.9% | 48.4% | 74.5% | <0.0005 |
| KL grade | ||||
| Non-painful knee† | n=373 | n=90 | ||
| 0, % | 53.1% | 48.1% | 68.9% | |
| 1, % | 15.6% | 15.5% | 15.5% | |
| 2, % | 8.0% | 8.1% | 7.8% | 0.001 |
| 3, % | 20.1% | 24.4% | 6.7% | |
| 4, % | 3.2% | 3.9% | 1.1% | |
| Painful knee† | n=546 | n=263 | ||
| 0, % | 36.3% | 39.9% | 32.3% | |
| 1, % | 11.5% | 9.9% | 13.3% | |
| 2, % | 6.4% | 6.0% | 6.9% | 0.379 |
| 3, % | 31.7% | 31.1% | 32.3% | |
| 4, % | 14.1% | 13.1% | 15.2% | |
Participants not used in the analysis comprise of 263 with bilateral knee pain and 90 with no pain. For participants with bilateral knee pain, the highest KL grade was used.
Participants used in the analysis are tested against those not used, using the 2-tail t-test for continuous normal data, the Wilcoxon rank-sum test for continuous non-normal data and the chi-square test for categorical data.
Table 3 shows the presence of each imaging finding in pairs of knees with and without pain and the conditional ORs for the association of each structural feature with unilateral knee pain. For nearly all structural findings, both radiographic and MRI, the presence of an abnormality of any severity somewhere in the knee was significantly associated with knee pain, with ORs ranging from 1.5 to 7.3. The presence of severe radiographic and MRI abnormalities in a knee was also strongly associated with unilateral knee pain compared to less severe or no abnormality, with ORs ranging from 1.9 to 5.3 (all P < 0.05). The ORs for association with pain were substantially larger for severe abnormalities compared to defining the same abnormality using a lower threshold for several radiographic findings (K&L grades, osteophytes and sclerosis) and for MRI findings of osteophytes and synovitis/effusion. There were too few instances of severe radiographic attrition and cysts for analysis. Radiographic K-L grade and JSN and MRI cartilage lesions, bone marrow lesions and synovitis/effusion all showed a strong dose-response relationship, with increasing severity associated with greater odds of knee pain (Figure 1).
Table 3.
Presence of at least one radiographic or MRI any and severe structural lesion within the whole knee in 283 participants with unilateral knee pain
| Feature | Imaging | Severity of grade1 | Occurrence of structural findings
|
Odds ratios from Conditional logistic model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any knee2 | Neither knee | Knee without pain only | Knee with pain only | Both knees | ||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | OR | 95% CI | p | ||||
| KL grade | X-ray | Any | 56.0% | 99 | (35.0%) | 14 | (5.0 %) | 37 | (13.1%) | 133 | (47.0%) | 2.64 | 1.43,4.89 | <0.001 |
| Severe | 36.2% | 147 | (51.9%) | 11 | (3.9%) | 56 | (19.8%) | 69 | (24.4%) | 5.09 | 2.67, 9.71 | <0.001 | ||
|
| ||||||||||||||
| JSN | X-ray | Any | 58.5% | 86 | (30.4%) | 15 | (5.3%) | 48 | (17.0%) | 134 | (47.3%) | 3.20 | 1.79,5.71 | <0.001 |
| Severe | 47.5% | 141 | (49.8%) | 19 | (6.7%) | 61 | (21.6%) | 62 | (21.9%) | 3.21 | 1.92,5.37 | <0.001 | ||
| Cartilage | MR | Any | 89.8% | 15 | (5.3%) | 6 | (2.1%) | 22 | (7.8%) | 240 | (84.8%) | 3.67 | 1.49,9.04 | 0.005 |
| Severe | 47.5% | 107 | (37.8%) | 19 | (6.7%) | 64 | (22.6%) | 93 | (32.9%) | 3.37 | 2.02,5.62 | <0.001 | ||
|
| ||||||||||||||
| Osteophyte | X-ray | Any | 63.8% | 76 | (26.9%) | 18 | (6.4%) | 35 | (12.4%) | 154 | (54.4%) | 1.94 | 1.10,3.43 | 0.022 |
| Severe | 32.5% | 165 | (58.3%) | 10 | (3.5%) | 42 | (14.8%) | 66 | (23.3%) | 4.20 | 2.11,8.37 | <0.001 | ||
| MR | Any | 83.9% | 22 | (7.8%) | 19 | (6.7%) | 28 | (9.9%) | 214 | (75.6%) | 1.47 | 0.83,2.63 | 0.19 | |
| Severe | 39.8% | 132 | (46.6%) | 21 | (7.4%) | 56 | (19.8%) | 74 | (26.1%) | 2.67 | 1.61,4.40 | <0.001 | ||
|
| ||||||||||||||
| Attrition | X-ray | Any | 9.7% | 239 | (84.5%) | 4 | (1.4%) | 29 | (10.2%) | 11 | (3.9%) | 7.25 | 2.55,20.62 | <0.001 |
| Severe | 2.3% | 272 | (96.1%) | 0 | (0) | 9 | (3.2%) | 2 | (0.7%) | / | / | / | ||
| MR | Any | 53.1% | 90 | (31.8%) | 25 | (8.8%) | 60 | (21.2%) | 108 | (38.2%) | 2.40 | 1.51,3.83 | <0.001 | |
| Severe | 24.0% | 185 | (65.4%) | 15 | (5.3%) | 45 | (15.9%) | 38 | (13.4%) | 3.00 | 1.67,5.38 | <0.001 | ||
|
| ||||||||||||||
| Cyst | X-ray | Any | 9.5% | 236 | (83.4%) | 8 | (2.8%) | 32 | (11.3%) | 7 | (2.5%) | 4.00 | 1.84,8.68 | <0.001 |
| Severe | 0.7% | 279 | (98.6%) | 2 | (0.7%) | 2 | (0.7%) | 0 | (0) | / | / | / | ||
| MR | Any | 58.1% | 78 | (27.6%) | 31 | (11.0%) | 50 | (17.7%) | 124 | (43.8%) | 1.61 | 1.03,2.52 | 0.037 | |
| Severe | 17.7% | 204 | (72.1%) | 20 | (7.1%) | 38 | (13.4%) | 21 | (7.4%) | 1.90 | 1.11,3.27 | 0.020 | ||
|
| ||||||||||||||
| Sclerosis | X-ray | Any | 54.8% | 93 | (32.9%) | 20 | (7.1%) | 50 | (17.7%) | 120 | (42.4%) | 2.50 | 1.49,4.20 | 0.001 |
| Severe | 14.7% | 217 | (76.7%) | 9 | (3.2%) | 40 | (14.1%) | 17 | (6.0%) | 4.44 | 2.16,9.16 | <0.001 | ||
|
| ||||||||||||||
| BML | MR | Any | 66.3% | 55 | (19.4%) | 30 | (10.6%) | 51 | (18.0%) | 147 | (51.9%) | 1.70 | 1.08,2.67 | 0.021 |
| Severe | 32.3% | 145 | (51.2%) | 32 | (11.3%) | 61 | (21.6%) | 45 | (15.9%) | 1.91 | 1.24,2.92 | 0.003 | ||
|
| ||||||||||||||
| Synovitis/effusion | MR | Any | 73.1% | 50 | (17.7%) | 15 | (5.3%) | 37 | (13.1%) | 181 | (64.0%) | 2.47 | 1.35, 4.49 | 0.003 |
| Severe | 20.9% | 186 | (65.7%) | 12 | (4.2%) | 64 | (22.6%) | 21 | (7.4%) | 5.33 | 2.88, 9.88 | <0.001 | ||
See table 1 for definitions of ‘any’ and ‘severe’ structural abnormality.
For any knee, proportion derived from 566 knees.
Figure 1. Conditional OR (95% CI) for association of grade of structural damage with the painful knee in subjects with unilateral knee pain.
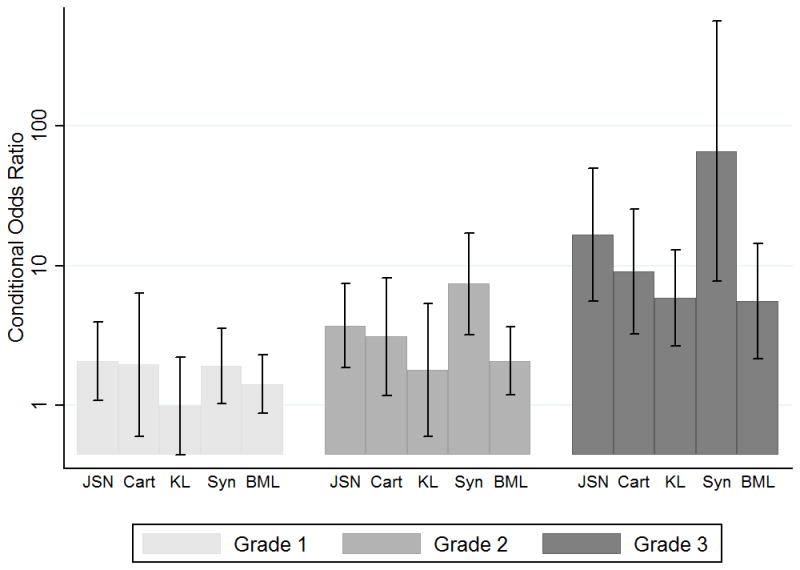
For all ORs, the referent category is a score of 0 for the feature. JSN= Radiographic OARSI grade of Joint Space Narrowing; CART = MRI WORMS grade of cartilage lesion (referent = grade 0/1; 1= grade 2; 2= grade 3/4; 3= grade 5/6); KL = Radiographic Kellgren and Lawrence grade (1=1; 2=2; 3=3/4); SYN= MRI WORMS synovitis/effusion grade BML= MRI WORMS Bone marrow lesion.
However, a large proportion of subjects with unilateral knee pain were non-informative for the association of structural damage with pain (Table 3); in other words, while discordant for pain their knees were concordant for the specific structural abnormalities. 72% to 88% of subjects were non-informative for radiographic abnormalities and 66% to 90% were non-informative for MRI abnormalities. As expected, uncommon abnormalities were more likely to be non-informative in terms of subjects not having the abnormality in either knee, while abnormalities that were relatively more common were more likely to be non-informative by having the abnormality in both knees.
In marginal logistic models using all knees of subjects with unilateral pain, all ORs for the association of structural features with pain were attenuated compared to the conditional ORs in Table 3. For example, for severe KL grade the marginal OR was 2.01 (95% CI: 1.58–2.56), and for severe synovitis/effusion was 3.25 (95% CI: 2.21–4.78)).
We then tested the ability of different structural features to distinguish painful vs. non-painful knees in all subjects with unilateral knee pain using ROC curves for the full range of scores (Figure 2). The AUC for each structural feature was low, ranging from 0.54 to 0.60. Further, we found no statistically significant differences between the AUCs for radiographic and MR assessments of the equivalent feature (Table 4). We also compared the best performing radiographic (K-L grade) and MR (synovitis/effusion) features using this method and no significant difference was found (p=0.42).
Figure 2. ROC curves for radiographic and MR based measurements of structural features of OA to predict knee pain in patients with unilateral knee pain.
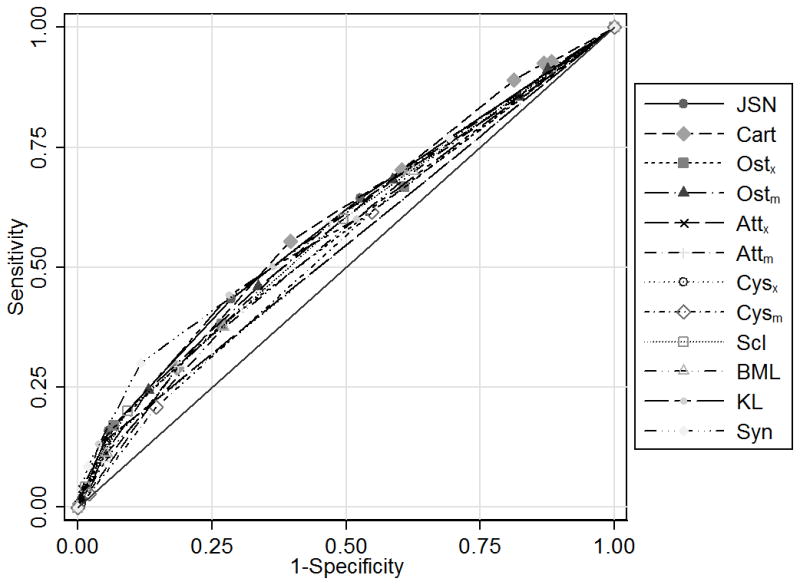
With Area under the curve: JSN: joint space narrowing (0.59); Cart: cartilage lesion (0.59); Ostx: radiographic osteophyte (0.57); Ostm: MR osteophyte (0.58); Attx: radiographic attrition (0.54); Attm: MR attrition (0.58); Cysx: radiographic cyst (0.54); Cysm: MR subchondral cyst (0.55); Scl: radiographic sclerosis (0.58); KL: Kellgren and Lawrence grade (0.58); BML: MR bone marrow lesion (0.56); Syn: synovitis (0.60).
Table 4.
Performance of radiographic vs. MR detected structural features using Receiver operator characteristics area under the curve.
| Radiographic feature | MR feature | P-value for Difference | ||
|---|---|---|---|---|
| Area under the curve | 95% CI | Area under the curve | 95% CI | |
| JSN | Cartilage lesion | |||
| 0.59 | 0.55–0.64 | 0.59 | 0.54–0.64 | 0.97 |
| Osteophytes | ||||
| 0.57 | 0.52–0.61 | 0.58 | 0.53–0.63 | 0.49 |
| Attrition | ||||
| 0.55 | 0.52–0.57 | 0.58 | 0.53–0.62 | 0.16 |
| Subchondral cysts | ||||
| 0.54 | 0.52–0.57 | 0.55 | 0.50–0.59 | 0.86 |
| KL | Synovitis/effusion | |||
| 0.58 | 0.54–0.63 | 0.60 | 0.56–0.64 | 0.42 |
P-value from difference in area for ROC curve using bootstrapping (1000 replicates) comparing radiographic with MR features.
Discussion
We confirmed previous studies of persons with unilateral knee pain showing that structural features of knee OA assessed by radiograph are strongly associated with pain in a within-person, matched knee analysis that controls for individual differences in non-structural pain determinants9. We extended these findings to MRI-detected structural damage using the same study design and found similarly strong and highly significant associations, such that when these features were present in only one of a subject’s knees they were substantially more likely to occur in the knee with pain. These results support an important role for structural abnormalities in the etiology of knee pain. However, to put these findings into a clinical context, we found that for the majority of all the subjects with unilateral knee pain the knee pairs were concordant on specific structural findings, either having the finding in both knees or not having the finding in either knee. Further, in ROC analyses of all knees in subjects with unilateral knee pain we found that neither MRI nor radiographic features of knee OA performed well in discriminating between painful vs. non-painful knees and that there were no differences in performance of the two imaging modalities.
The within-person, matched knee analysis of discordant pain has the important advantage of controlling for individual differences in non-structural pain determinants, such as factors influencing pain susceptibility, that may obscure structure-pain relationships9. Our results are consistent with those of a recent studyto use this approach for knee pain9, and confirm its potential for uncovering strong, and possibly causal, associations between pain and structural abnormalities detected with knee imaging. These results support a role of for structural abnormalities in the etiology of knee pain and the continued use of MRI and other advanced imaging modalities.
The findings of studies using the within-person matched-knee design appear to conflict with both clinical experience and with previous epidemiological and clinical studies that suggest widespread discordance between structure and pain 4,5. However, as correctly noted by Neogi and colleagues9, the apparent conflict reflects different ways of approaching the structure-pain relationship, with one focused on identifying associations and risk factors and the other concerned with diagnostic discrimination and prediction23. Only pairs of knees discordant for both pain and also for a given structural finding are used in evaluating the association of structure and pain by means of the conditional odds ratios in the matched knee analysis.
We found that even for knee pairs discordant for pain yet matched on person-level pain determinants, in the majority of subjects the individual structural features did not differ between the painful and non-painful knee, frequently not present in either knee or present in both knees. This suggest that regardless of asymmetry in symptoms, MRI structural findings tend be symmetrical between an individual’s knees, as has been observed for structural findings of hand OA25,26.
Consistent with the above, in analyses that included both knees of all subjects with unilateral pain, the marginal odds ratios for the association of structural features with pain were smaller than the conditional odds ratios estimated in the matched knee analyses. In order for a structural feature to perform well in classifying knees for the presence of pain, the marginal odds ratios for pain would need to be very large, at least an order of magnitude larger than we observed 23. This was born out in the ROC analyses of all knees of persons with unilateral pain, where neither MRI nor radiographic features of knee OA performed well in discriminating between painful vs. non-painful knees, with AUCs that were very modest (all were less than 0.61, which is considered poor discriminative ability27). This suggests that while common structural features of OA detectable with knee imaging are etiological factors in knee pain, other factors are also likely to make a substantial contribution to determining which knees are painful, even between one individual’s two knees. This emphasizes the importance, from a clinical perspective, of continued investigation into non-structural determinants of knee pain.
We further compared the discriminatory performance of the two imaging modalities in ROC analyses, and found no significant differences in AUCs between analogous MRI and radiographic findings (e.g. JSN vs. cartilage loss, attrition on x-ray vs. MRI, etc). MRI findings were more common in general than radiographic findings, especially when defined as present using a low threshold. However, using similar scoring methods, namely the presence or absence of specific features, the greater sensitivity of MRI appeared to provide little extra information over radiographs in predicting the occurrence of knee pain. For findings with a similar prevalence by the two modalities, conditional ORs were no larger for MRI than for x-ray. There were also no consistent differences between imaging modalities in the proportion of knee pairs that were informative vs. non-informative, with both MRI and radiographic features present in both knees or absent in both knees in over two-thirds of subjects with unilateral pain. Consistent with their higher prevalence, MRI findings were more frequently non-informative by being present in both knees of a pair. Further, we found no differences in ability to discriminate between painful and non-painful knees when we compared the AUCs from ROC analyses of analogous MRI and radiographic findings (e.g. JSN vs. cartilage loss, attrition on x-ray vs. MRI, etc). The best performing MRI feature was synovitis/effusion, which does not have a radiographic equivalent; it performed no better than the KL grade of the knee.
These findings may have implications for the use of MRI to investigate the sources of knee pain in individual patients. The ideal structural feature for predicting the presence of unilateral symptoms would have a high frequency in only the painful knees and a low frequency in only the non-painful knee, but also would infrequently be present in both knees of a discordant pair. MRI may be disadvantaged in this regard by its greater sensitivity compared to radiographs, since features that are very common overall may be more likely to exhibit poor discrimination. A high proportion of subjects also had specific radiographic features in both knees, a finding consistent with other studies of unilateral knee pain28. Our findings suggest that to realize the potential value of MRI as both a research and clinical tool, future work needs to determine whether certain anatomic locations or combinations of lesions in cartilage, bone, synovium and meniscus are associated with, and predict, knee symptoms 29,30 and how nonstructural factors modify these relationships.
Our study has several limitations that should be noted. All of our subjects were elderly (ages 71–80) and because of a high prevalence of structural findings of knee OA in the elderly some of our findings may not apply to younger age groups in which these abnormalities are less common. However, we were able to replicate the significant structure-pain associations found by others using the same analytical design in subjects of a younger age 9. It is also well recognized that the symptoms of knee OA fluctuate 31, and our definition of discordant pain may misclassify subjects who develop bilateral pain with further follow-up. Ways of defining unilateral knee pain over several years may produce different results and should be examined in future studies. We used a definition of pain from anywhere in the knee. It is not known if more refined classification of pain in terms of severity, anatomical location of symptoms and/or signs or features of neuropathic pain would improve the correspondence between structural abnormalities and pain. The presence of severe pain in one knee may suppress the experience of lesser pain in the other knee. However, severe knee pain may also increase pain in the contralateral knee through an increase loading to spare the painful knee or via sensitization of the other knee to be painful with a less noxious stimulus. In addition the MRIs of a subject’s two knees may have been assessed by different readers, while a subject’s x-ray of both knees was always assessed by the same reader and inter-reader variation in MRI readings may have reduced the strength of associations between MRI features and unilateral knee pain compared to radiographic features. Finally we used classified structural features of OA separately for each feature using the highest grade of damage, we propose that methods of analysis of structural features that take into account combinations of features/sub regions affected may provide better discrimination/prediction and should be explored when analyzing the structural information of the knee.
SUMMARY
In conclusion, among elderly subjects with unilateral knee pain, an individual imaging (MRI or radiographic) feature of OA was infrequently found in just one of a subject’s knees, but when this occurred the feature was significantly more likely to be found in the painful than in the non-painful knee, suggesting that in some individuals these findings play an important role in the etiology of knee pain. At the same time, in the majority of subjects with unilateral knee pain the presence of individual radiographic and MRI features of OA did not differ between a subject’s two knees, and as a result the two modalities had an equivalent, but poor, ability to discriminate between painful and non-painful knees among all persons with unilateral pain. Further work is required to explore whether new approaches to utilizing information on structural findings of OA from knee imaging better predict knee pain, as well as to identify the important non-structural determinants of knee pain.
Acknowledgments
Funding/Support: This research was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050, and NINR grant R01-NR012459. We are grateful to the readers of the radiographs: D. Hunter, B. Sack and D. Felson. Dr. Javaid was supported in part by the Oxford NIHR Musculoskeletal BRU and travelling fellowship from the ARUK.
Role of the Sponsor: The NIA and NIHR had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
We wish to acknowledge Kathryn Wildy for the initial concept of the analysis.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the views of the NIH or NIHR.
Author Contributions: Dr Javaid and Kiran had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Javaid, Lane, Felson, Nevitt, Harris, Kwoh
Acquisition of data: Guermazi, Zaim, Felson, Nevitt
Analysis and interpretation of data: Javaid, Kiran, Kwoh, McCulloch, Arden, Lane, Nevitt, Felson
Drafting of the manuscript: Javaid, Kiran, Nevitt
Critical revision of the manuscript for important intellectual content: Javaid, Kiran, Guermazi, Kwoh, Carbone, Harris, McCulloch, Arden, Lane, Felson, Nevitt
Statistical analysis: Javaid, Kiran, McCulloch
Obtained funding: Nevitt, Harris
Administrative, technical, or material support:
Study supervision: Nevitt, Harris
References
- 1.Mathers C, Boerma T, Fat DM. The global burden of disease: 2004 update. WHO Press; 2008. [Google Scholar]
- 2.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957 Dec;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis and Cartilage. 2007;15:A1–A56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Dieppe PA, Cushnaghan J, Shepstone L. The Bristol ‘OA500’ study: progression of osteoarthritis (OA) over 3 years and the relationship between clinical and radiographic changes at the knee joint. Osteoarthritis Cartilage. 1997 Mar;5(2):87–97. doi: 10.1016/s1063-4584(97)80002-7. [DOI] [PubMed] [Google Scholar]
- 5.Cooper C, Snow S, McAlindon TE, et al. Risk factors for the incidence and progression of radiographic knee osteoarthritis. Arthritis Rheum. 2000 May;43(5):995–1000. doi: 10.1002/1529-0131(200005)43:5<995::AID-ANR6>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Duncan R, Peat G, Thomas E, Hay E, McCall I, Croft P. Symptoms and radiographic osteoarthritis: not as discordant as they are made out to be? Ann Rheum Dis. 2007 Jan;66(1):86–91. doi: 10.1136/ard.2006.052548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gwilym SE, Keltner JR, Warnaby CE, et al. Psychophysical and functional imaging evidence supporting the presence of central sensitization in a cohort of osteoarthritis patients. Arthritis Rheum. 2009 Sep 15;61(9):1226–1234. doi: 10.1002/art.24837. [DOI] [PubMed] [Google Scholar]
- 8.Conaghan PG, Felson D, Gold G, Lohmander S, Totterman S, Altman R. MRI and non-cartilaginous structures in knee osteoarthritis. Osteoarthritis Cartilage. 2006;14 (Suppl A):A87–94. doi: 10.1016/j.joca.2006.02.028. [DOI] [PubMed] [Google Scholar]
- 9.Neogi T, Felson D, Niu J, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ. 2009;339:b2844. doi: 10.1136/bmj.b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le Graverand MP, Mazzuca S, Lassere M, et al. Assessment of the radioanatomic positioning of the osteoarthritic knee in serial radiographs: comparison of three acquisition techniques. Osteoarthritis Cartilage. 2006;14 (Suppl A):A37–43. doi: 10.1016/j.joca.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 11.Kothari M, Guermazi A, von Ingersleben G, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004 Sep;14(9):1568–1573. doi: 10.1007/s00330-004-2312-6. [DOI] [PubMed] [Google Scholar]
- 12.Hunter DJ, Zhang YQ, Niu JB, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis Cartilage. 2007 May 12; doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altman RD, Hochberg M, Murphy WA, Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995 Sep;3 (Suppl A):3–70. [PubMed] [Google Scholar]
- 14.Peterfy CG, Guermazi A, Zaim S, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004 Mar;12(3):177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Javaid MK, Lynch JA, Tolstykh I, et al. Pre-radiographic MRI findings are associated with onset of knee symptoms: the most study. Osteoarthritis Cartilage. Mar;18(3):323–328. doi: 10.1016/j.joca.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruyere O, Genant H, Kothari M, et al. Longitudinal study of magnetic resonance imaging and standard X-rays to assess disease progression in osteoarthritis. Osteoarthritis Cartilage. 2007 Jan;15(1):98–103. doi: 10.1016/j.joca.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Hunter DJ, Conaghan PG, Peterfy CG, et al. Responsiveness, effect size, and smallest detectable difference of Magnetic Resonance Imaging in knee osteoarthritis. Osteoarthritis Cartilage. 2006;14 (Suppl A):A112–115. doi: 10.1016/j.joca.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 18.Bruyere O, Collette J, Kothari M, et al. Osteoarthritis, magnetic resonance imaging, and biochemical markers: a one year prospective study. Ann Rheum Dis. 2006 Aug;65(8):1050–1054. doi: 10.1136/ard.2005.045914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torres L, Dunlop DD, Peterfy C, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006 Oct;14(10):1033–1040. doi: 10.1016/j.joca.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Moisio K, Eckstein F, Chmiel JS, et al. Denuded subchondral bone and knee pain in persons with kneeosteoarthritis. Arthritis Rheum. 2009 Dec;60(12):3703–3710. doi: 10.1002/art.25014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hunter DJ, Lavalley M, Li J, et al. Biochemical markers of bone turnover and their association with bone marrow lesions. Arthritis Res Ther. 2008 Aug 29;10(4):R102. doi: 10.1186/ar2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reichenbach S, Guermazi A, Niu J, et al. Prevalence of bone attrition on knee radiographs and MRI in a community-based cohort. Osteoarthritis Cartilage. 2008 Sep;16(9):1005–1010. doi: 10.1016/j.joca.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004 May 1;159(9):882–890. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 24.Flynn TN, Peters TJ. Use of the bootstrap in analysing cost data from cluster randomised trials: some simulation results. BMC Health Serv Res. 2004 Nov 18;4(1):33. doi: 10.1186/1472-6963-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalichman L, Cohen Z, Kobyliansky E, Livshits G. Patterns of joint distribution in hand osteoarthritis: contribution of age, sex, and handedness. Am J Hum Biol. 2004 Mar-Apr;16(2):125–134. doi: 10.1002/ajhb.20007. [DOI] [PubMed] [Google Scholar]
- 26.Niu J, Zhang Y, LaValley M, Chaisson CE, Aliabadi P, Felson DT. Symmetry and clustering of symptomatic hand osteoarthritis in elderly men and women: the Framingham Study. Rheumatology (Oxford) 2003 Feb;42(2):343–348. doi: 10.1093/rheumatology/keg110. [DOI] [PubMed] [Google Scholar]
- 27.Swets JA, Getty DJ, Pickett RM, D’Orsi CJ, Seltzer SE, McNeil BJ. Enhancing and evaluating diagnostic accuracy. Med Decis Making. 1991 Jan-Mar;11(1):9–18. doi: 10.1177/0272989X9101100102. [DOI] [PubMed] [Google Scholar]
- 28.McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis. 1992 Jul;51(7):844–849. doi: 10.1136/ard.51.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernandez-Molina G, Neogi T, Hunter DJ, et al. The association of bone attrition with knee pain and other MRI features of osteoarthritis. Ann Rheum Dis. 2008 Jan;67(1):43–47. doi: 10.1136/ard.2007.070565. [DOI] [PubMed] [Google Scholar]
- 30.Kothari A, Guermazi A, Chmiel JS, et al. The within-subregion relationship between bone marrow lesions and subsequent cartilage loss in knee osteoarthritis. Arthritis Care & Research. 2010 doi: 10.1002/acr.20068. NA-NA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peters TJ, Sanders C, Dieppe P, Donovan J. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. Br J Gen Pract. 2005 Mar;55(512):205–211. [PMC free article] [PubMed] [Google Scholar]


