Abstract
Background/Aims
The management of asymptomatic erosive esophagitis is controversial. We surveyed physicians' opinions on asymptomatic erosive esophagitis using e-mail.
Methods
All members of the Korean Society of Neurogastro-enterology and Motility were invited to answer the questionnaire on the treatment and follow-up of patients with asymptomatic erosive esophagitis by e-mail.
Results
A total of 73 members answered the questionnaire (response rate, 18%). As initial management, 41% of respondents chose pharmacologic treatment, whereas 59% chose nonpharmacologic treatment. In the case of pharmacologic treatment, proton pump inhibitors were the preferred medication. The most common treatment duration was 4 weeks (43%), followed by 8 weeks (38%), and 6 months (11%). Sixty-two percent of the respondents recommended follow-up endoscopy annually, whereas 29% chose no endoscopic follow-up. Thirty-four percent of the respondents answered that they would talk about reflux-related sleep disturbances. Only 25% of the respondents explained the possibility of Barrett's esophagus or esophageal adenocarcinoma to their patients.
Conclusions
There are substantial practice variations in the management of asymptomatic erosive esophagitis in Korea.
Keywords: Esophagitis, Endoscopy, Asymptomatic diseases, Therapeutics
INTRODUCTION
Gastroesophageal reflux disease (GERD) can be divided into two categories: symptomatic GERD and asymptomatic GERD. Asymptomatic GERD can be defined as the presence of esophageal mucosal injury that is typical for GERD (erosions, peptic ulceration, and/or Barrett's esophagus) during upper endoscopy in individuals who lack typical or atypical/extraesophageal manifestations of GERD.1
With recent westernization of Korean lifestyles, prevalence of GERD in Korea has increased. The prevalence of reflux esophagitis was 1% to 3% in the early period of 1990's,2,3 4% to 5% in the early of period of 2000's,4,5 9% to 11% in late period of 2000's6,7 in routine check-up population, and the prevalence of symptoms of reflux esophagitis was 7% to 10% in the middle period of 2000's.8-10
Esophagogastroduodenoscopy is frequently performed as a part of gastric cancer screening program in Korea. Accordingly, the number of asymptomatic patients with erosive esophagitis is increasing continuously. It was reported that 62% to 80% of subjects with erosive esophagitis who were diagnosed by endoscopy in a routine health check-up program do not have any symptoms in Korea.2,4,11 Because little is known about natural history of asymptomatic erosive esophagitis, there is currently no consensus regarding the best management strategy for asymptomatic erosive reflux esophagitis. In order to examine how the patients with asymptomatic erosive esophagitis are managed in Korea, we surveyed the physician's opinion about this issue.
MATERIALS AND METHODS
E-mail invitations were sent to 403 members of the Korean Society of Neurogastroenterology and Motility between July 2009 and August 2009. E-mails were sent three times at 1 week interval.
The questionnaire was composed of two parts. In the first part of the survey, participants were asked to describe their practice settings and specialities. The second part of the survey evaluated endoscopists' practice patterns regarding treatment, surveillance, and explanation to patients of asymptomatic erosive esophagitis, which was confined to the Los Angeles classification A. Respondents were asked to choose the best answer from the choices relevant to each question, excepting one question about how to treat (multiple response questions). The questions are as follows: 1) What is your choice for diagnosis code in medical insurance claim bills? 2) How do you explain to patient about endoscopic finding? 3) How do you treat patients with asymptomatic erosive esophagitis? 4) How long is the duration of your treatment? 5) When do you exam following endoscopy? 6) Do you ask or explain to patients about sleep disturbance? 7) Do you explain to patients about the possibility of Barrett's esophagus or esophageal adenocarcinoma, or not?
The survey was reviewed independently for content and format of the questionnaire by several expert endoscopists. Skipped questions were not included in the overall response totals. Descriptive statistics were used to summarize the responses of the survey, including participant characteristics and clinical questions. Percentages were calculated and used for display in the figures. Proportions of the responses were compared between private practice and academic groups with the chi-square test. A p-value less than 0.05 was considered as statistically significant.
RESULTS
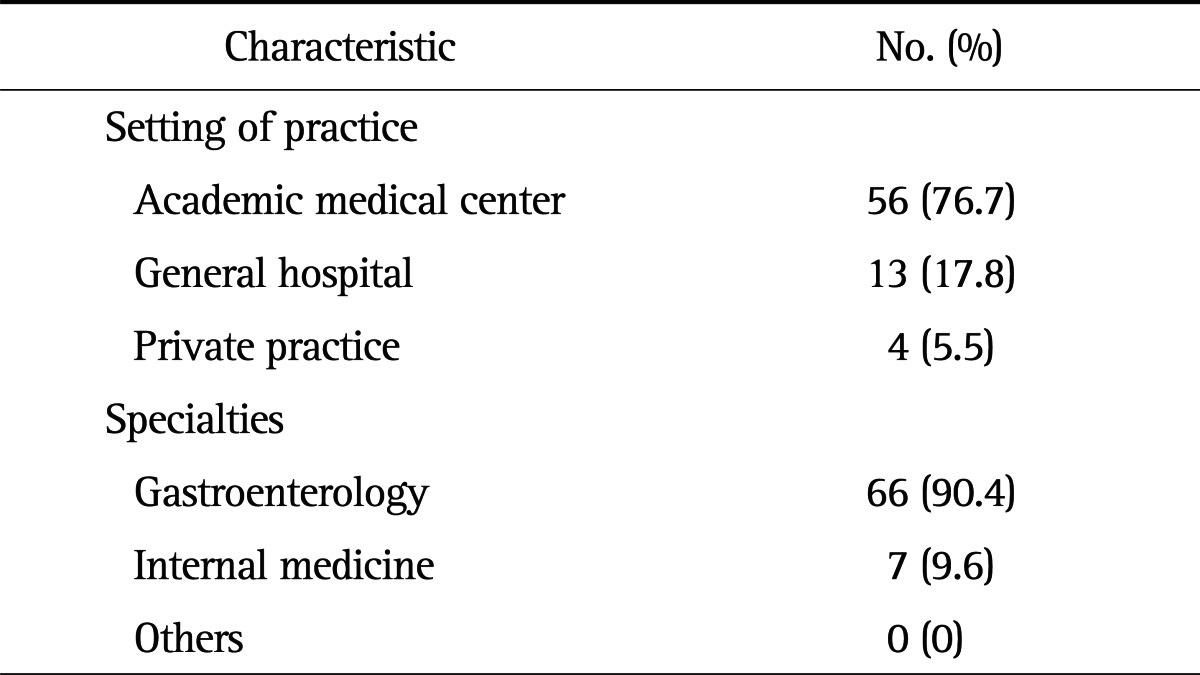
Of the 403 invitations to participate, 73 (response rate, 18.1%) physicians responded. The demographics of the respondents are shown in Table 1. Among the 73 physicians who responded to the survey, 56 (76.7%) practiced in academic medical center, 13 (17.8%) in general hospital, and four (5.5%) in private practice. The specialties of respondents were gastroenterology (90.4%) and internal medicine (9.6%), and no other specialties.
Table 1.
Characteristics of Survey Respondents
In the question about diagnosis code usage in medical records, the most common response was GERD with esophagitis (K21.0, 93.2%). Other responses were GERD without esophagitis (K21.9, 4.1%), dyspepsia (K30, 1.4%), and esophagitis (K20, 1.4%).
The major 41 respondents (56.2%) explained to patients that they have GERD but do not need treatment. Twenty-four (32.9%) explained that the patients have GERD and need to treat it. A small number (2.7%) did not mention anything about endoscopic findings of erosive esophagitis.
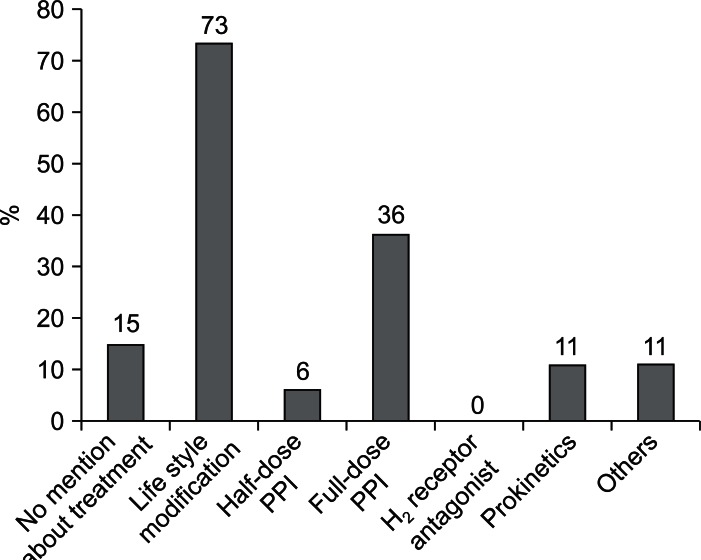
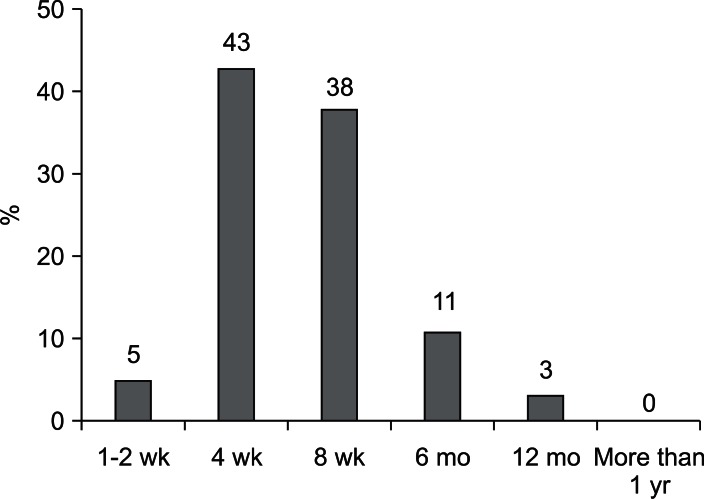
In the question about initial management of asymptomatic esophagitis, 41.1% of respondents chose pharmacologic treatment, whereas 58.9% chose nonpharmacologic treatment. In the multiple response question, when asked about how they treat patients with asymptomatic erosive esophagitis, the most common treatment of choice was lifestyle modification (72.6%), followed by full-dose proton pump inhibitor (PPI) (35.6%). Eleven of the respondents (15.1%) would not talk about treatment (Fig. 1). In case of pharmacologic treatment, PPI was preferred medication. The most common treatment duration was 4 weeks (43.3%), followed by 8 weeks (36.7%), and 6 months (13.3%) (Fig. 2). Forty-five (61.6%) of the respondents recommended follow-up endoscopy annually, whereas 21 (28.8%) chose no endoscopic follow-up.
Fig. 1.
Distribution of opinions regarding the treatment for asymptomatic erosive esophagitis (multiple response question).
PPI, proton pump inhibitor.
Fig. 2.
Distribution of opinions regarding the duration of pharmacologic treatment.
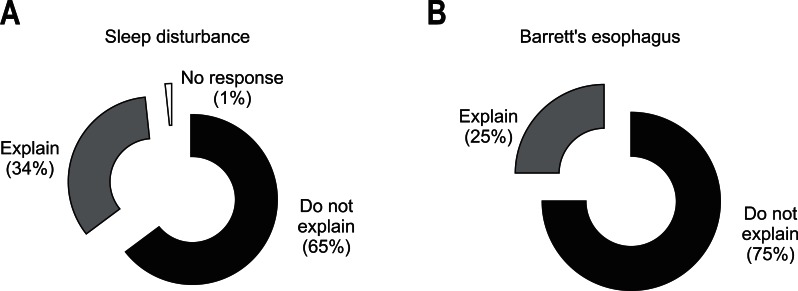
Twenty-five (34.2%) of the respondents answered that they would talk about the GERD-related sleep disturbance. Only 18 (24.7%) of the respondents explain the possibility of Barrett's esophagus or esophageal adenocarcinoma to their patients (Fig. 3).
Fig. 3.
Distribution of opinions regarding discussing the following with patients: (A) sleep disturbances and (B) the possibility of Barrett's esophagus or esophageal adenocarcinoma.
DISCUSSION
Asymptomatic GERD is a common phenomenon that involves the incidental finding of erosive esophagitis, Barrett's esophagus, and the evolution of esophageal adenocarcinoma in asymptomatic patients. The clinical consequences of asymptomatic GERD are various. Son et al.12 reported that most patients with asymptomatic reflux esophagitis showed improvement or a stable course during 3 years of endoscopic follow-up. This report, albeit with many limitations, suggests that the medical treatment such as PPI is unnecessary in asymptomatic patients with erosive esophagitis. The patients who are diagnosed incidentally with asymptomatic erosive esophagitis are unlikely to maintain themselves on antireflux treatment because of poor compliance resulting from the lack of disease-related symptoms.13 However, there is currently no guidance about what to do with asymptomatic erosive esophagitis.
Reflux esophagitis results from the combination of excessive gastroesophageal reflux of gastric juice and impaired esophageal clearance of the gastric acid. The treatment of reflux esophagitis should be titrated to disease severity. Minimal therapy for GERD patients is comprised of lifestyle modification, dietary modification, as needed antacid use, H2 receptor antagonists, and PPIs. Lifestyle modifications are aimed at enhancing esophageal acid clearance, minimizing the incidence of reflux events, or both as with cessation of smoking and avoidance of late meals. However, a systematic review of the published literature concluded that weight loss and head of bed elevation are effective lifestyle interventions for GERD but there is no evidence supporting an improvement in GERD measures after cessation of tobacco, alcohol, or other dietary interventions.14 Although their effectiveness has not been extensively evaluated in clinical trials, these approaches have been used clinically. Similarly in this survey, the most common choice for initial management of asymptomatic erosive esophagitis was nonpharmacologic treatment such as lifestyle modification.
Among the respondents who chose pharmacologic treatment, 41.1% chose a PPI (full-dose PPI 35.6%, half-dose PPI 5.5%) and 11.0% chose a prokinetic agent, but none chose a H2 receptor antagonist. Acid-suppressant drugs predominate in the treatment of GERD. Many trials have established the efficacy of the various PPIs and H2 receptor antagonists in the treatment of esophagitis.15,16 PPIs are the first-line of choice in both reflux esophagitis and nonerosive reflux disease. In a meta-analysis, complete relief from heartburn occurred at a rate of 11.5% per week with a PPI compared to 6.4% per week with a H2 receptor antagonist.17 On the other hand, asymptomatic Barrett's esophagus represents no indication for treatment, although recent studies have suggested that potent antireflux treatment (such as PPIs) may retard neoplastic progression in patients with Barrett's esophagus.18,19 Prokinetic drugs such as bethanechol or metoclopramide can be used in the treatment of GERD by increasing lower esophageal sphincter pressure, enhancing gastric emptying, or improving peristalsis. However, the currently available promotility agents are hampered by side effects that limit their use in GERD.20 A guideline on GERD management developed by the American Gastroenterological Association Institute recommends against use of metoclopramide as monotherapy or adjunctive therapy because of these side effects.20
In this survey in Korea, 56.2% of respondents explain to patients that they have GERD, but do not require treatment. And 58.9% chose nonpharmacologic treatment for initial management of asymptomatic erosive esophagitis without medication. In spite of these responses, more than half of respondents survey following endoscopy annually. The need for endoscopy in patients with GERD is unsettled. Some experts advocated an endoscopy in patients who require continuous maintenance medical therapy to rule out Barrett's esophagus.21 In patients without Barrett's esophagus on an initial examination, the cancer risk is too low to justify a follow-up endoscopy. Exceptions are patients who develop bleeding, dysphagia, or a significant change in symptoms while on effective therapy.
Sleep and GERD have a bidirectional relationship in which GERD adversely affects the quality of sleep, and poor quality of sleep worsens GERD.22-24 Unfortunately, the clinical features of sleep disorders including obstructive sleep apnea are nonspecific and the diagnostic accuracy of clinicians' subjective impression is poor.25 Recent studies have shown that, even in patients without nighttime heartburn, gastroesophageal reflux may result in sleep disturbances.26 It suggests that the presence of sleep disturbances and poor quality of sleep could be clinical clues for identifying patients with asymptomatic GERD. However, there is little interest in this area, unlike extraesophageal symptoms such as cough, asthma or laryngitis in Korea. In this survey, only 34% were explaining to the patients about sleep disturbance.
Barrett's esophagus is a metaplastic change of the esophageal mucosa, such that the normal squamous epithelium is replaced by specialized columnar epithelium.27 The condition develops as a consequence of chronic GERD, and predisposes to the development of adenocarcinoma of the esophagus. Estimates of the frequency of Barrett's esophagus in the general population have varied widely ranging from 0.9% to 4.5% depending in part upon the population studied and the definitions used.28,29 To decrease mortality from esophageal adenocarcinoma, it has been proposed that patients with GERD symptoms should be screened endoscopically for Barrett's esophagus.21,30 However, a significant number of patients presenting with adenocarcinoma of the esophagus don't have any GERD-related symptoms such as heartburn or regurgitation during their lifetime.31 In other studies, fewer than 5% were known to have had Barrett's esophagus before they presented with symptoms of esophageal cancer.32 It is not clear that patients who have Barrett's esophagus benefit from surveillance. In addition, there is little evidence that these programs have prevented deaths from esophageal adenocarcinoma. Even more, because the epidemiological study about relationship between GERD and Barrett's esophagus or esophageal adenocarcinoma is insufficient in Korea, explanation of risk like this on the basis of just endoscopic finding of erosive esophagitis is maybe unnecessary. In this survey, only 25% was explaining to the patients about possibility of Barrett's esophagus or esophageal adenocarcinoma.
Practice variation in countries other than Korea is yet to be reported. Fass and Dickman1 suggested that the clinical implications of silent GERD are vast, but no specific treatment guideline was recommended. According to Lu33 in Taiwan, whether to treat asymptomatic GERD patients is an open question.
One of the limitations of our study is that the opinions of members of the Korean Society of Neurogastroenterology and Motility do not necessarily reflect the opinions and practices of endoscopists nationwide and that only 18.1% of the group responded to the survey. There are also inherent limitations to a multiple choice survey; however, several of our questions allowed for write-in responses. Additionally, given the anonymity of our survey design, we were unable to characterize differences between respondents and nonrespondents that may affect the survey results.
In summary, there are substantial practice variations in the management of asymptomatic erosive esophagitis in Korea. A majority of our survey respondents prefer nonpharmacologic treatment such as lifestyle modification to pharmacologic treatment such as PPI. Practice patterns of endoscopic surveillance are variable.
ACKNOWLEDGEMENTS
We would like to thank the participating members of the Korean Society of Neurogastroenterology and Motility.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Fass R, Dickman R. Clinical consequences of silent gastroesophageal reflux disease. Curr Gastroenterol Rep. 2006;8:195–201. doi: 10.1007/s11894-006-0075-8. [DOI] [PubMed] [Google Scholar]
- 2.Yi SY, Lee SK, Kim MH, Han DS, Kim JW, Min YI. Epidemiologic study of reflux esophagitis in general health screening people. Korean J Med. 1994;46:514–520. [Google Scholar]
- 3.Jung SA, Jung HY, Kim KR, Min YI. The prevalence of reflux esophagitis of Korean adults for 10 years of 1990's. Korean J Gastrointest Motil. 2001;7:161–167. [Google Scholar]
- 4.Oh JH, Choi MG, Kim HR, et al. Clinical spectrum of endoscopic reflux esophagitis in routine check-up subjects in Korea. Korean J Neurogastroenterol Motil. 2006;12:12–18. [Google Scholar]
- 5.Cho YS, Choi MG, Jeong JJ, et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005;100:747–753. doi: 10.1111/j.1572-0241.2005.41245.x. [DOI] [PubMed] [Google Scholar]
- 6.Yoo SS, Lee WH, Ha J, et al. The prevalence of esophageal disorders in the subjects examined for health screening. Korean J Gastroenterol. 2007;50:306–312. [PubMed] [Google Scholar]
- 7.Kim JH, Hwang JK, Kim J, et al. Endoscopic findings around the gastroesophageal junction: an experience from a tertiary hospital in Korea. Korean J Intern Med. 2008;23:127–133. doi: 10.3904/kjim.2008.23.3.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang JK, Kim J, Hong SG, et al. A prospective multicenter study on the prevalence and symptoms of erosive reflux esophagitis in secondary and tertiary hospitals in Korea. Korean J Gastroenterol. 2009;53:283–291. doi: 10.4166/kjg.2009.53.5.283. [DOI] [PubMed] [Google Scholar]
- 9.Yang SY, Lee OY, Bak YT, et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008;53:188–193. doi: 10.1007/s10620-007-9842-0. [DOI] [PubMed] [Google Scholar]
- 10.Lee JH, Kim N, Chung IK, et al. Clinical significance of minimal change lesions of the esophagus in a healthy Korean population: a nationwide multi-center prospective study. J Gastroenterol Hepatol. 2008;23(7 Pt 1):1153–1157. doi: 10.1111/j.1440-1746.2008.05299.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee SJ, Song CW, Jeen YT, et al. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001;16:373–376. doi: 10.1046/j.1440-1746.2001.02464.x. [DOI] [PubMed] [Google Scholar]
- 12.Son JI, Kim JJ, Park MK, et al. The natural history of asymptomatic reflux esophagitis: a retrospective study from periodic health check-up program. Korean J Neurogastroenterol Motil. 2004;10:100–104. [Google Scholar]
- 13.Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease: where next? Aliment Pharmacol Ther. 2005;22:79–94. doi: 10.1111/j.1365-2036.2005.02531.x. [DOI] [PubMed] [Google Scholar]
- 14.Kaltenbach T, Crockett S, Gerson LB. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965–971. doi: 10.1001/archinte.166.9.965. [DOI] [PubMed] [Google Scholar]
- 15.Kahrilas PJ, Shaheen NJ, Vaezi MF, et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease. Gastroenterology. 2008;135:1383–1391. doi: 10.1053/j.gastro.2008.08.045. [DOI] [PubMed] [Google Scholar]
- 16.Bell NJ, Hunt RH. Role of gastric acid suppression in the treatment of gastro-oesophageal reflux disease. Gut. 1992;33:118–124. doi: 10.1136/gut.33.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chiba N, De Gara CJ, Wilkinson JM, Hunt RH. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology. 1997;112:1798–1810. doi: 10.1053/gast.1997.v112.pm9178669. [DOI] [PubMed] [Google Scholar]
- 18.El-Serag HB, Garewel H, Kuebeler M, Sampliner RE. Is the length of newly diagnosed Barrett's esophagus decreasing? The experience of a VA Health Care System. Clin Gastroenterol Hepatol. 2004;2:296–300. doi: 10.1016/s1542-3565(04)00058-8. [DOI] [PubMed] [Google Scholar]
- 19.Koop H. An evidence-based look at pharmacotherapy for gastroesophageal reflux. Chirurg. 2005;76:353–358. doi: 10.1007/s00104-004-0906-9. [DOI] [PubMed] [Google Scholar]
- 20.Kahrilas PJ, Shaheen NJ, Vaezi MF American Gastroenterological Association Institute; Clinical Practice and Quality Management Committee. American Gastroenterological Association Institute technical review on the management of gastroesophageal reflux disease. Gastroenterology. 2008;135:1392–1413. doi: 10.1053/j.gastro.2008.08.044. [DOI] [PubMed] [Google Scholar]
- 21.DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:1434–1442. doi: 10.1111/j.1572-0241.1999.1123_a.x. [DOI] [PubMed] [Google Scholar]
- 22.Schey R, Dickman R, Parthasarathy S, et al. Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease. Gastroenterology. 2007;133:1787–1795. doi: 10.1053/j.gastro.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 23.Dickman R, Green C, Fass SS, et al. Relationships between sleep quality and pH monitoring findings in persons with gastroesophageal reflux disease. J Clin Sleep Med. 2007;3:505–513. [PMC free article] [PubMed] [Google Scholar]
- 24.Chen CL, Robert JJ, Orr WC. Sleep symptoms and gastroesophageal reflux. J Clin Gastroenterol. 2008;42:13–17. doi: 10.1097/MCG.0b013e31802fc1bc. [DOI] [PubMed] [Google Scholar]
- 25.Hoffstein V, Szalai JP. Predictive value of clinical features in diagnosing obstructive sleep apnea. Sleep. 1993;16:118–122. [PubMed] [Google Scholar]
- 26.Orr WC. Heartburn: another danger in the night? Chest. 2005;127:1486–1488. doi: 10.1378/chest.127.5.1486. [DOI] [PubMed] [Google Scholar]
- 27.Lee JH. Barrett's esophagus-with emphasis on endoscopic disgnosis. Korean J Gastrointest Endosc. 2009;39:185–198. [Google Scholar]
- 28.Hirota WK, Loughney TM, Lazas DJ, Maydonovitch CL, Rholl V, Wong RK. Specialized intestinal metaplasia, dysplasia, and cancer of the esophagus and esophagogastric junction: prevalence and clinical data. Gastroenterology. 1999;116:277–285. doi: 10.1016/s0016-5085(99)70123-x. [DOI] [PubMed] [Google Scholar]
- 29.Cameron AJ, Zinsmeister AR, Ballard DJ, Carney JA. Prevalence of columnar-lined (Barrett's) esophagus. Comparison of population-based clinical and autopsy findings. Gastroenterology. 1990;99:918–922. doi: 10.1016/0016-5085(90)90607-3. [DOI] [PubMed] [Google Scholar]
- 30.Inadomi JM, Sampliner R, Lagergren J, Lieberman D, Fendrick AM, Vakil N. Screening and surveillance for Barrett esophagus in high-risk groups: a cost-utility analysis. Ann Intern Med. 2003;138:176–186. doi: 10.7326/0003-4819-138-3-200302040-00009. [DOI] [PubMed] [Google Scholar]
- 31.Lagergren J, Bergström R, Lindgren A, Nyrén O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–831. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- 32.Dulai GS, Guha S, Kahn KL, Gornbein J, Weinstein WM. Preoperative prevalence of Barrett's esophagus in esophageal adenocarcinoma: a systematic review. Gastroenterology. 2002;122:26–33. doi: 10.1053/gast.2002.30297. [DOI] [PubMed] [Google Scholar]
- 33.Lu CL. Silent gastroesophageal reflux disease. J Neurogastroenterol Motil. 2012;18:236–238. doi: 10.5056/jnm.2012.18.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]