Abstract
Background: When H1N1 emerged in 2009, institutions of higher education were immediately faced with questions about how best to protect their community from the virus, yet limited information existed to help predict student preventive behaviors. Methods: The authors surveyed students at a large urban university in November 2009 to better understand how students perceived their susceptibility to and the severity of H1N1, which preventive behaviors they engaged in, and if policies impacted their preventive health decisions. Results: Preventive health behavior messaging had a mixed impact on students. Students made simple behavior changes to protect themselves from H1N1, especially if they perceived a high personal risk of contracting H1N1. Although policies were instituted to enable students to avoid classes when ill, almost no student self-isolated for the entire duration of their illness. Conclusions: These findings can help inform future decision making in a university setting to best influence preventive health behaviors.
Keywords: community health, H1N1, health behaviors, health education
When H1N1 emerged in spring 2009, universities and other institutions of higher education (IHE) were immediately faced with questions about how best to protect their students, faculty, and staff from the virus. Many institutions, including our own, convened or reconvened task forces in order to plan for the Fall semester; aiding administrators in decision making around best practices for infection control, emergency management, continuity of operations, and communications.1 Preventive health measures taken by those who were well in an attempt to prevent infection, and also among those who were ill to prevent spread of the virus to others, were critical in addressing this public health emergency. To mitigate the potential consequences of the virus, our university engaged in a broad communication plan to educate students, their parents, faculty, and staff about the virus in an attempt to increase disease prevention behavior. Information was sent out via email, posted on Web sites, and printed on posters displayed throughout the campus. The university offered free seasonal and H1N1 vaccines and put out advisories to students, faculty, and staff encouraging vaccinations, reminders for hand washing, use of hand sanitizer, to “cover your cough,” get rest, eat healthy, and stay hydrated. Hand sanitizer stations were placed throughout campus, masks were made available in certain high-traffic areas and offered to ill students, and phone banks were established to provide medical advice. The university also provided links for alternative dining options for those who were ill and revised the excused absence policy to discourage ill students from attending class.2 Little empirical data existed, however, to help predict student behaviors or to inform policy development for promotion of best practices amongst students for mitigating the effects of the pandemic.
This research attempts to capture student preventive health behaviors during the H1N1 pandemic and provide data to inform future decision making regarding influenza preparedness. For our purposes, preventive health measures include actions taken by those who were well in an attempt to prevent infection, and also among those who were ill to prevent spread of the virus to others. We assessed the preventive health behaviors of the overall student body, and specifically the behaviors of those students in the university population who became ill with influenza-like illness (ILI), determined by self-report and defined for this study as a fever or fever-ishness, with either a cough or sore throat in the absence of another diagnosis. This definition of ILI is consistent with that of the Centers for Disease Control and Prevention (CDC) during the time of the outbreak, but for the purposes of this study it was assumed that many students would not have thermometers, and as such temperature was not specified.
Background
H1N1 emerged in April 2009, was declared a pandemic in June 2009, and although the pandemic was officially declared over in August 2010, the virus continues to circulate around the world.3 The burden of the 2009 H1N1 influenza virus was disproportionate according to age, with many of the cases in the United States occurring among those under 25 years of age.4 The age distribution of H1N1 deviated from typical patterns for seasonal influenza strains, and the 2009–2010 influenza season had higher pediatric mortality (4 times that of the previous 5 seasons) and rates of hospitalizations in children and young adults than in previous years.5 As a result, pandemic response behaviors are of particular interest among school-aged populations given their increased risk of acquiring H1N1 influenza. Close-contact environments characteristic of IHE, where students live, eat, and study together, are ideal for influenza transmission. Consequently, the CDC addressed transmission among students by providing specific clinical and preventive guidance for both the general student population and health care profession students for the 2009–2010 academic year.6 These recommendations focused on pharmaceutical interventions and nonpharmaceutical interventions for reducing transmission of H1N1 and other ILI in a university setting.
Pharmaceutical Interventions
Pharmaceutical interventions, primarily vaccination, but also the use of antivirals, were and are widely counted upon to mitigate the impact of novel influenza subtypes. These interventions, however, are ultimately only as effective as the resources and behavioral practices behind them, and these interventions can have a limited ability to provide rapid pandemic containment.7–10 Significant challenges accompanied the production and distribution of the H1N1 vaccine with regard to timeliness. Vaccines were initially rationed to priority groups and did not become available to the general public until December 2009 in many US locations.11 Additionally, some polls found trepidation among certain populations to receiving the vaccine.12 Other studies, however, found a willingness among the general population to comply with vaccination recommendations during the pandemic.13,14
Nonpharmaceutical Interventions
Nonpharmaceutical interventions have the benefit of being more accepted among at-risk populations, inexpensive, and readily available, serving as effective primary prevention until other control strategies can be implemented and sustained.8 As limited data exist on the use of behavioral interventions in the context of pandemic preparedness and response, use of generated statistical model predictions and historical evidence demonstrate that nonpharmaceutical interventions can successfully decrease influenza incidence with rapid implementation.15,16 Specifically, school closures and workplace nonattendance during illness are both considered to lower predicted influenza attack rates among populations.17
Hand hygiene is perhaps the most well-documented, effective, and overtly recommended behavioral practice known to protect the individual and mitigate H1N1 transmission.8,9,14,17 However, college students have not always responded to hand-washing campaigns, and an early 2009 study found limited association between hand-washing practices and disease rates, though trends did indicate reductions in upper respiratory symptoms among students who engaged in increased hand washing.18 Unlike hand hygiene, use of personal protective equipment (specifically the use of facemasks) is not overwhelmingly or consistently supported for the general public, and compliance tends to be lower compared to other preventive behaviors.8,16,18 Specifically, young people between the ages of 16 and 24 tend to be the least willing to comply with use of a facemask14
Perceived Risk of H1N1
According to the Health Belief Model (HBM), behavior change, through use of both pharmaceutical and nonpharmaceutical intervention, relies upon students believing they are susceptible to H1N1, that the potential severity of the disease warrants action, and that the benefits of taking actions to reduce susceptibility and outweigh any potential barriers. Once these conditions are met, the students then are influenced by “cues to action,” promoting preventive health behaviors to reduce transmission of H1N1.19 As such, compliance with prevention recommendations is directly associated with higher perceived risk and susceptibility.13,18 Conversely, gaps in health communication and insufficient knowledge conveyed regarding key public health risks strongly hinders the population's overall capacity to respond to a public health emergency.
Outreach and Communication
Beginning in the spring of 2009 and continuing throughout the remaining months of the year, there was intense media attention paid to the H1N1 virus.20 Articles were written, much airtime was devoted to the pandemic on the news, and social media responded in kind with discussion and blogs devoted to the pandemic threat.21,22,∗ The federal government led by the CDC also engaged in outreach and communication strategies, by updating in real time the pandemic Web site (flu.gov). Similarly, local and state health departments created sites to explain local activity and response.23,24,† All of these actions, from media reports to university messaging, worked to influence student perception regarding susceptibility and severity of H1N1, attempted to reduce barriers to action through amended class absentee policies, and provided “cues to action” to encourage students to engage in preventive health behaviors per the HBM.
Study Objectives
The overarching goals of this study was to determine the extent to which the student population at a large urban university followed recommended (by both CDC and the university) H1N1 preventive behavioral practices and to try to discern which precautionary health behaviors were most prominent and why. The primary study aim was to assess student perceived personal risk with regard to susceptibility and severity of H1N1, and if that perceived risk affected preventive health behaviors. The secondary aim was to determine if students with self-reported ILI took preventive measures to reduce transmission of the virus. Third, we tried to determine if university policies and messaging around H1N1 influenced student behavior.
METHODS
Working with the university Office of Academic Planning, Institutional Research and Assessment, 5,000 students at our large research university in the mid-Atlantic region were randomly selected to receive a secure, internet based survey via e-mail.‡ These 5,000 students represented approximately one-quarter of the total student population. The student sample was proportionally selected across graduate and undergraduate enrollments as well as years of study. All student demographics were represented, with the only exclusion criteria being students in the School of Medicine, for which a separate study was conducted.25 All surveys were distributed and completed during the first 3 weeks of November 2009.
Respondents were asked to provide general demographic data, including age, gender, school of study, and living situation. Specific questions were then aimed at determining their perceived susceptibility to H1N1, level of concern about the virus, the specific health behaviors taken in response to the virus, and experience with university policies around the pandemic. Respondents were also asked about whether they had ILI, and what behaviors they engaged in to reduce transmission of the virus to the rest of the university community.
Health behaviors listed and assessed in the survey included self-isolation, hand washing, hand sanitizer use, social distancing, cough etiquette, disinfection/cleaning of surroundings, rearranged furniture to decrease transmission, wearing a facemask, and prophylaxis medication use. Students were asked to identify which behaviors they engaged in, in response to the H1N1 pandemic, and additionally which they engaged in during the Fall 2009 school semester specifically. With regard to risk perception, the survey asked students to indicate their overall concern for H1N1, their individual risk, and risk of family members as low, moderate, high, or extremely high. All students were asked to identify whether they had any preexisting risk factors for influenza complications, specified in the survey as asthma or other pulmonary disorder, cardiovascular disease such as congestive heart failure, neurologic disorder such as multiple sclerosis, diabetes, immunosuppression including human immunodeficiency virus or the use of immune suppressive medications, or pregnancy.
For students who had ILI, an additional set of questions were asked pertaining to the duration of their most recent episode, whether they sought medical care, and if so, where they went and what treatment and recommendations they were given, and if they self-isolated for the recommended period of time to decrease transmission rates.
All respondents were given the opportunity to provide additional comments on the survey. The authors did not have access to any student names or medical records, and no personal health information was obtained or available to the investigators.
RESULTS
Five thousand students were contacted by the university to complete the survey during the first 3 weeks of November 2009. Of these, approximately 100 did not receive the invitation to complete the survey, as they did not have functional e-mail addresses. In total, 819 students submitted responses to the survey (16.7% response rate), although not every student responded to every question.
Demographics of Respondents
The population demographics of survey respondents are described in Table 1. Of the 816 students who identified their living situation, 570 or approximately 70% lived off campus. Of the nearly 30% who lived on campus, 221 (88.4%) lived with roommates, and 6.0% (49) of all respondents lived with children. With regard to health care access, 737 (90.8%) of students responded that they had access to primary care, whereas the remaining 75 (9.2%) who answered this question said no.
TABLE 1.
Demographics of Survey Respondents by Gender and Age, According to Student Year
| Undergraduate |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Freshman |
Sophomore |
Junior |
Senior |
Graduate |
Total |
|||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Gender | ||||||||||||
| Male | 33 | 12.8 | 21 | 8.2 | 20 | 7.8 | 25 | 9.7 | 158 | 61.5 | 257 | 32.0 |
| Female | 61 | 11.2 | 52 | 9.5 | 46 | 8.4 | 53 | 9.7 | 334 | 61.2 | 546 | 68.0 |
| Age | ||||||||||||
| 18–23 | 93 | 43.3 | 73 | 18.0 | 62 | 15.3 | 74 | 18.2 | 104 | 25.6 | 406 | 50.2 |
| 24–29 | 1 | 0.3 | 0 | 0.0 | 4 | 1.3 | 5 | 1.7 | 276 | 96.5 | 286 | 35.4 |
| >29 | 1 | 0.9 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 115 | 99.1 | 116 | 14.4 |
| Total by year | 96 | 11.9 | 73 | 9.0 | 66 | 8.2 | 79 | 9.8 | 495 | 61.2 | ||
Risk Perception for Susceptibility to and Severity of H1N1
Over 80% (668) of all respondents identified themselves as not having any of the documented risk factors for complications of influenza, including severe influenza, pneumonia, and death (listed as asthma or other pulmonary disorder, cardiovascular disease, neurologic disorder, diabetes, immunosuppression, or pregnancy). Those reporting close contact with someone experiencing ILI made up one quarter (201 of the 816 student respondents) of the study population and another 134 (16.4%) identified more than 1 contact with ILI (Figure 1). The 481 (58.9%) students indicating they had no contacts with ILI, however, were almost universally more likely to self-report preventive behaviors compared to the students who had at least 1 contact with ILI. As an unexpected finding, this remained true for all solicited behaviors except self-isolation, which was essentially the same regardless of number of contacts. The most prominent differences in self-reported behaviors were seen in rearranging furniture to decrease transmission, followed by wearing a facemask and social distancing, which were all at least 20% higher among students with no contacts. However, despite both the number of students indicating contacts with ILI and the apparent increase in behaviors among those with no contacts, the majority of respondents indicated low to moderate concern for H1N1 infection and low to moderate risk perception of personal or family member infection. This level of concern was consistent across age groups and categories of students (Table 2).
FIGURE 1.
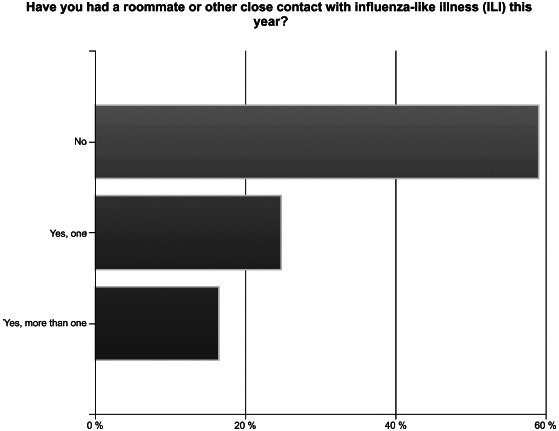
Proportion of students identifying known contacts with influenza like illness (ILI) (color figure available online).
TABLE 2.
Relationship Between Personal Risk Perception of Acquiring H1N1 and Preventive Health Behaviors
| Self-identified risk of personal H1N1 infection |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Extremely high | High | Moderate | Low | None | ||||||
| Have you engaged in any of the following preventive health behaviors in response to H1N1? (Choose all that apply) | n | % | n | % | n | % | n | % | n | % |
| Total | 20 | 95 | 355 | 277 | 58 | |||||
| Isolated | 8 | 40.0 | 30 | 31.6 | 88 | 24.79 | 37 | 13.360 | 12 | 20.69 |
| Washed hands | 17 | 85.0 | 85 | 89.5 | 304 | 85.60 | 221 | 79.800 | 40 | 69.00 |
| Hand sanitizer | 16 | 80.0 | 72 | 75.8 | 251 | 70.70 | 162 | 58.500 | 27 | 46.60 |
| Avoidance | 6 | 30.0 | 24 | 25.3 | 66 | 18.60 | 22 | 7.945 | 7 | 12.10 |
| Covered mouth | 15 | 75.0 | 87 | 91.6 | 303 | 85.40 | 221 | 79.800 | 41 | 70.70 |
| Disinfected | 13 | 65.0 | 60 | 63.2 | 184 | 51.80 | 112 | 40.400 | 18 | 31.00 |
| Rearranged | 4 | 20.0 | 7 | 7.4 | 21 | 5.90 | 9 | 3.300 | 6 | 10.30 |
| Face mask | 1 | 5.0 | 2 | 2.1 | 9 | 2.50 | 6 | 2.200 | 4 | 6.90 |
| Preventive meds | 7 | 35.0 | 16 | 16.8 | 55 | 15.50 | 31 | 11.200 | 5 | 8.60 |
Note. The categories for preventive health behaviors are self-isolation, hand washing, hand sanitizer use, social distancing, covering your mouth when you cough, disinfection/cleaning of surroundings, rearranging furniture to decrease virus transmission, wearing a facemask, and taking preventive medication.
Having a preexisting risk factor for complications of influenza and more severe illness had little effect on whether students perceived themselves to be at risk for H1N1. Each perceived personal risk group (extremely high, high, moderate, low, and none) had similar percentages of those who identified themselves as having a preexisting risk factor, in relationship to those who did not. Of the students who identified a risk factor for influenza complications, the majority claimed to have a moderate personal risk of developing H1N1 (Figure 2).
FIGURE 2.
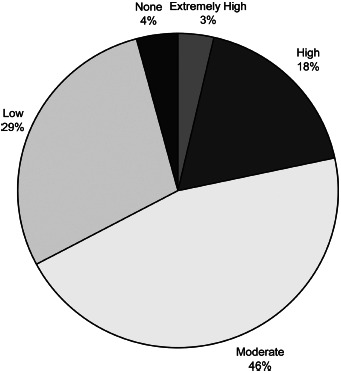
Perceived personal risk of H1N1 infection among students with risk factors for complications of influenza (color figure available online).
Change in Behaviors
The percentage of students who engaged in each preventive health behavior grew progressively as risk perception moved from none to extremely high. This was also true for students engaging in each preventive behavior more in the fall, than in previous times. Students were asked to identify preventive health behaviors they engaged in, as well as to identify whether any of the behaviors were more frequent during the Fall semester as a result of the H1N1 pandemic and associated recommendations from health and university officials. Cough etiquette and hand washing were the 2 most frequently indicated behaviors among the 780 students who responded; compliance with each behavior was reported by 676 students, with 95.9% and 91.7% compliance, respectively, followed by disinfection/cleaning of surroundings by 392 (86.2%), and hand sanitizer use by 538 (84.1%). Wearing a facemask and rearranging furniture to decrease virus transmission were the 2 behaviors least engaged in overall. However, they were the 2 most common behaviors in which students engaged in more often during the Fall semester in response to the H1N1 threat. Furthermore, the proportion of students who specifically indicated they rearranged furniture, wore a mask, and took preventive medications during the fall period was increased compared to the general use of these precautions prior to the Fall semester (Figure 3).
FIGURE 3.
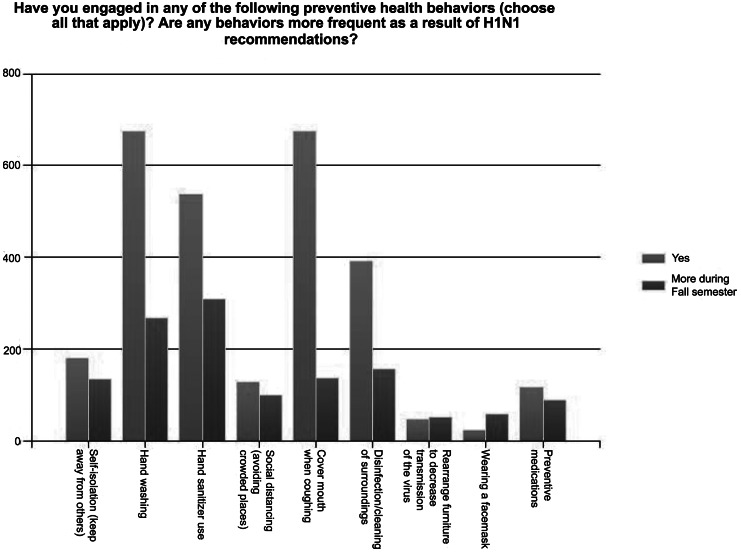
Preventive health behaviors (color figure available online).
Table 3 examines the changes in behavior of students as it related to contact with other sick students or their own illness. For the most part, students who had similar ILI experiences and no direct contact with ILI reported the same preventive behaviors, regardless of whether they said they had changed their behaviors or not. However, there were some inconsistencies among this group. Those who did not feel they made changes self-isolated less and avoided large gatherings less, but they covered their coughs and rearranged furniture more. Students who reported having close contacts with ILI were more likely to report a change in their behavior. Comparing students with no ILI/no direct contacts who did not feel they changed their behaviors versus those who did feel they changed their behaviors—hand washing was 133 (76.9%) versus 96 (89.7%), covering cough was 130 (75.1%) versus 95 (88.8%), and mask use was 8 (4.6%) versus 4(3.7%), respectively. All other behaviors were engaged in by roughly half of those who had ILI (Table 3).
TABLE 3.
Self-reported Health Behaviors Based on ILI Status, Identification of Close Contacts With ILI, and Reported Changes in Behavior
| Have you engaged in any of the following preventive health behaviors? (Choose all that apply) | Isolated |
Washed hands |
Sanitizer |
Avoidance |
Covered mouth |
Disinfected |
Rearranged |
Mask |
Meds |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| No ILI | 107 | 19 | 17.8 | 96 | 89.7 | 50 | 46.7 | 19 | 17.8 | 95 | 88.8 | 59 | 55.1 | 9 | 8.4 | 4 | 3.7 | 18 | 16.8 |
| No contacts | |||||||||||||||||||
| Changes in behavior | |||||||||||||||||||
| No ILI | 173 | 30 | 17.3 | 133 | 76.9 | 97 | 56.1 | 23 | 13.3 | 130 | 75.1 | 64 | 37.0 | 14 | 8.1 | 8 | 4.6 | 20 | 11.6 |
| No contacts | |||||||||||||||||||
| No changes in behavior | |||||||||||||||||||
| Had ILI | 34 | 6 | 17.7 | 27 | 79.4 | 22 | 64.7 | 7 | 20.6 | 25 | 73.5 | 19 | 55.9 | 1 | 2.9 | 2 | 5.9 | 4 | 11.8 |
| No contacts | |||||||||||||||||||
| Changes in behavior | |||||||||||||||||||
| Had ILI | 32 | 6 | 18.8 | 28 | 87.5 | 25 | 78.1 | 4 | 12.5 | 30 | 93.8 | 15 | 46.9 | 4 | 12.5 | 1 | 3.1 | 5 | 15.6 |
| No contacts | |||||||||||||||||||
| No changes in behavior | |||||||||||||||||||
| No ILI | 101 | 27 | 23.7 | 93 | 92.1 | 76 | 75.3 | 14 | 13.9 | 88 | 87.1 | 58 | 57.4 | 6 | 5.9 | 2 | 2.0 | 17 | 16.8 |
| Had contacts | |||||||||||||||||||
| Changes in behavior | |||||||||||||||||||
| No ILI | 63 | 7 | 11.1 | 41 | 65.1 | 34 | 54.0 | 3 | 4.8 | 49 | 77.8 | 19 | 30.2 | 1 | 1.6 | 1 | 1.6 | 2 | 3.2 |
| Had contacts | |||||||||||||||||||
| No changes in behavior | |||||||||||||||||||
| Had ILI | 119 | 50 | 42.0 | 105 | 88.2 | 93 | 78.2 | 28 | 23.5 | 108 | 90.8 | 74 | 62.2 | 8 | 6.7 | 4 | 3.4 | 28 | 23.5 |
| Had contacts | |||||||||||||||||||
| Changes in behavior | |||||||||||||||||||
| Had ILI | 51 | 8 | 15.7 | 38 | 74.5 | 25 | 49.0 | 6 | 11.8 | 37 | 72.6 | 22 | 43.1 | 2 | 3.9 | 2 | 3.9 | 8 | 15.7 |
| Had contacts | |||||||||||||||||||
| No changes in behavior | |||||||||||||||||||
Note. ILI = influenza-like illness.
Vaccination Behaviors
Among students who received either the 2008–2009 or 2009–2010 seasonal flu vaccines, most stated it was because the vaccine was free and/or easily available. (The university offered the vaccine to students during both seasons, but charged a fee during 2008–2009.) Similar rates of vaccination were reported by students for the 2009–2010 vaccine compared to the previous year, with 305 (38.8%) receiving vaccine in 2009–2010 and 279 (35.8%) in 2008–2009. The primary reason given for not receiving either of the last two seasonal vaccines was “not wanting to get the flu from the vaccine.” With regard to the ongoing H1N1 pandemic, 212 or approximately 30%, of student respondents indicated that although the H1N1 vaccine was not yet available (at the time of the survey), they did intend to get it.
A small number of students, 127 (15.8%), identified themselves as being at either at high or very high personal risk of H1N1 infection. With respect to seasonal vaccination behaviors within this high/very high risk group, 60 (47.2%) reported getting the 2009–2010 seasonal flu vaccine, of which 8 (6.6%) identified the primary reason for receiving the 2009–2010 vaccine as health recommendations, 31 (25.4%) received it because it was free and/or easily available, and 21 (17.2%) received it to protect themselves. Similarly, for the H1N1 vaccine, 60 (47.2%) of these 127 high-risk students either received the H1N1 vaccine or indicated they planned to once it became available.
Information and Communication
Most students among the 819 respondents identified newspapers and other media to be their source of information in reference to H1N1 (679, 84.8%). Discussions with friends and family were also prominent with 573 students (71.5%), indicating this as a mode of information and communication along with awareness of public health recommendations (482, 60.2%). In addition, 207 (25.8%) and 180 (22.5%) responded that their professors and physicians respectively acted as a source of information regarding H1N1. Approximately 70% (548) of respondents were aware of the university's H1N1 communication and policy efforts.
Self-reported ILI and Associated Behaviors
Out of 789 students who indicated how many times they had ILI within the year, 527 (66.8%) self-reported that they did not have an ILI episode. Of the remaining students, 200 (25.3%) had 1 episode, 49 (6.2%) had 2 episodes, 6 (0.8%) had 3 episodes, and 7 (0.9%) had more than 3 episodes of ILI. Table 4 outlines the illness duration and absenteeism from school/work as it relates to the illness among the 200 (25.3%) students who reported only 1 ILI episode. Just over a third of students reporting a single episode of ILI also reported missing no work or school (66, 33%), among which 57 (68.6%) indicated they had been ill for 3 days or more, with 10 (12.0%) reporting an illness duration of 7 days or longer (Table 4).
TABLE 4.
Number of Students Reporting a Single Episode of ILI by Illness Duration and Number of Days Absent
| Number of days absent from work/school |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None |
1–2 |
3–4 |
5–6 |
7 or more |
Total |
|||||||
| Illness duration | n | % | n | % | n | % | n | % | n | % | n | % |
| 1 day | 7 | 2 | 9 | 4.8 | ||||||||
| 2 days | 14 | 9 | 1 | 24 | 12.9 | |||||||
| 3 days | 20 | 12 | 4 | 36 | 19.4 | |||||||
| 4 days | 10 | 20 | 4 | 34 | 18.3 | |||||||
| 5 days | 8 | 15 | 12 | 4 | 39 | 21.0 | ||||||
| 6 days | 1 | 5 | 8 | 4 | 18 | 9.7 | ||||||
| 7 days | 6 | 8 | 3 | 5 | 4 | 26 | 14.0 | |||||
| Total | 66 | 35.5 | 71 | 38.2 | 32 | 17.2 | 13 | 7.0 | 4 | 2.2 | 186 | |
Note. ILI = influenza-like illness. A total of 262 students reported having ILI at least once, but only students who also answered the question about number of days absent from school were included in this analysis.
Of the more than one-third of students who reported at least 1 episode of ILI, 85 (38.6% of respondents) sought medical care, primarily due to symptom severity or fear of having H1N1 infection. Of the students self-reporting ILI, 167 (63.7% of respondents) had symptoms that lasted at least 4 or more days. Most who sought medical care were told to rest, drink fluids, or take over-the-counter medicine. Some received antibiotics, but only those who had been ill for more than 5 days, which is consistent with treatment of a secondary bacterial infection.
Among those who reported having ILI, 107 (43.1%) were told by their physicians, professors, or through university guidance Web sites, to stay at home as a result of their illness; 96 of those students (89.7%) followed the advice, at least partially. Of the 239 students with ILI who indicated the extent of professor support with regards to their illness, 119 (49.8%) did not ask their professors for extra time on assignments or help with missed classes, although those who did ask for help found the professors to be supportive. Only 13 students (5.4%) reported that they were unable to make up work missed from being sick.
COMMENT
Our first aim was to assess student perceived personal risk with regard to susceptibility and severity of H1N1. Risk perception has been widely established as a significant predictor of engaging in preventive health behaviors.13,18,26 In support of this, as students in this study felt themselves to be more at risk for developing H1N1, they were more likely to engage in preventive health behaviors, including self-isolation and social distancing. These results are consistent with the online survey conducted by Holland Jones and Salathe, assessing behavioral response to novel H1N1 implemented during the first few days of widespread media coverage among alumni and current students at a large university.27 Though approximately one-third of student respondents reported at least 1 episode of ILI or more, the overwhelming majority of students generally did not perceive themselves to be at high risk of personal infection with the H1N1 virus and similarly did not have a high overall concern of H1N1.
The university, as well as outside sources such as CDC, delivered a preventive measure message upon which policies were put in place to reduce barriers to recommended behaviors, including offering free vaccinations, making items such as hand sanitizer readily available, and ensuring that professors made provisions so that students who were sick did not feel pressured to come to class.
Young people approximately 16 to 24 are known to be more receptive to and compliant with recommended behavior changes, being more likely to change the way they live their lives in order to follow these behaviors.27–29 These messages and policies, though, had a mixed impact on the students in this sample.
Students appeared to be responsive to H1N1 messaging by engaging in preventive behaviors, as long as those behaviors were relatively easy to institute. With respect to pharmaceutical interventions, studies predicting behavior have found an overall willingness among the general population to comply with vaccination during an anticipated pandemic.13,14 Seasonal vaccine compliance did not increase in light of co-circulation of the novel H1N1 influenza virus, despite the university offering the 2009–2010 vaccine free of charge and thus lowering the barriers to access.
Generally, low perceptions of personal risk for H1N1 infection may have played a role in counteracting the impact of providing free seasonal vaccine may have otherwise had on increased compliance. Students who identified themselves as having a high personal risk of H1N1 infection reported similar rates of concurrent seasonal and H1N1 vaccine compliance. Thus despite efforts to make both the 2009–2010 seasonal and H1N1 vaccines more easily available, vaccine rates remained flat overall. It should be noted that at the time of the survey, the H1N1 vaccine was not yet readily available, and the university held H1N1 vaccination clinics after the survey period ended.
In the context of nonpharmaceutical behavior promotion, washing hands, using cough etiquette, and using hand sanitizer were easy to do in that they did not require major changes in daily routine, and therefore students did them. Wearing facemasks and keeping away from other students had more of an impact on students’ lives, and as a result occurred less often. These behavioral trends are consistent with the HBM, as well as findings by Holland Jones and Salathe.27 Interestingly, this study's findings further support those of the Holland Jones and Salathe survey in that students identifying no close contacts with ILI were more likely to report almost all solicited preventive health behaviors compared to those with at least 1 contact with ILI. They proposed 2 possible reasons why people with fewer contacts would have higher protection indices: the first noting that individuals with small social support networks are more anxious and thus more likely to take preventive actions; the second noting that people taking increased protective actions may intentionally decrease the number of contacts they have. This curious behavioral trend raises an interesting question specifically in the context of a student population. The increased proportions of rearranging furniture and engaging in social distancing among students without contacts found in this study may substantiate this second theory, though the temporality of any association would be difficult to establish without further study.
This study also sought to determine if students with ILI took preventive measures to reduce transmission of the virus to the rest of the university community. Students with ILI reported staying home from work or school while they were sick; however, the number of days absent does not correspond with the duration of ILI symptoms, with illness duration largely exceeding number of days absent from work or school. So, although some students engaged in social distancing, it may very well have been insufficient when taking into account how long they remained symptomatic. Furthermore, half of all students with ILI did not notify their professors or ask to be excused, but 61% who did not stay home specified it was because they did not want to miss class, even though the university had put policies in place to enable sick students to stay home.
Although university policies were necessary for raising awareness regarding the risk of H1N1, lowering barriers to preventive action, and enabling ill students to take care of themselves and reduce transmission of the disease, these policies were not sufficient to translate into universal adherence to preventive health behaviors. It is clear that some students responded to messaging and increased preventive behaviors, but the majority of students did not self isolate as long as was recommended.
Limitations
A number of limitations should be considered in the context of this study. First, all data collected were self-reported and as such were subjective in nature and could not be verified. Additionally, not all students answered all questions, and so inaccurate or incomplete responses could have potentially impacted comparability across questions during the study analyses. There are also limitations with the external validity or generalizability of study results; this study may not be representative of other IHE, as only 1 university was surveyed. Furthermore, the response rate for this survey was 16.7% (819/4,900) and thus may not apply to preventive behavior assessments in other population settings.
Conclusions
It is hard to say what exactly influenced the behaviors of students this fall in response to H1N1. Further study should be conducted to determine the impact on student preventive behaviors, university policy, the effectiveness of those policies, peer pressure, sense of vulnerability (or lack thereof), or level of deference to authority figures including medical professionals, as students made a series of decisions that affected their risk of infection from H1N1 and their risk of infecting others if sick.
Teasing out the rationale behind student choices around H1N1 is a difficult task. In this study, we attempted to capture some of the decisions students made around H1N1 and how they behaved if they felt they were at risk for becoming ill or were ill themselves (as self-reported). We believe these findings can help inform future decision-making in a university setting, to best influence preventive health behaviors that will protect the overall health of the student body.
NOTE
For comments and further information, address correspondence to Rebecca Katz, PhD, MPH, Assistant Professor of Health Policy and Emergency Medicine, School of Public Health and Health Services, George Washington University, 2021 K Street, NW Suite 800, Washington, DC 20006, USA (e-mail: rlkatz@gwu.edu).
Blogs include: www.spreadofh1n1.com/h1n1-blog; h1n1blog.org; swinefluh1n1.com; www.riskofswineflu.com/h1n1-blog.
For example: District of Columbia Department of Health H1N1 Web page. Available at: Doh.dc.gov/doh/cwp/view,a,1370,q,604320.asp.
Study design approved with Exempt Status by the George Washington University Medical Center Institutional Review Board. IRB Approval No. 100930. Informed consent provided by agreement within the survey itself.
REFERENCES
- 1.Petinaux B, May L, Katz R, Luk J, Goldenberg I. Clinical and public health decisions in preparing for 2009 influenza A (H1N1) in institutions of higher education. Am J Disaster Med. 2009;4:287–296. [PubMed] [Google Scholar]
- 2. George Washington University policy Web site. Available at: www.gwu.edu/∼gwalert/viewarchived.cfm?id=585. Accessed October 25, 2011.
- 3.World Health Organization. H1N1 in post-pandemic period. Opening statement by the Director-General. Available at: http://www.who.int/mediacentre/news/statements/2010/h1n1_vpc_20100810/en/index.html. Published August 10, 2010. Accessed October 5, 2010.
- 4.Centers for Disease Control and Prevention. CDC Estimates of 2009 Influenza cases, hospitalizations and deaths. 2009. April-December 12, Available at: http://cdc.gov/h1n1flu/estimates 2009 h1n1.htm. Accessed January 15, 2010.
- 5.Update: Influenza activity—United States 2009–2010 season. MMWR Morb Mort Wkly Rep. 2010;59:901–908. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Technical report on CDC guidance for responses to influenza for institutions of higher education during the 2009–2010 academic year. Available at: http://www.cdc.gov/H1N1flu/institutions/guidance/technical.htm. Updated 2009. Accessed January 10, 2010.
- 7.Davey VJ, Glass RJ. Rescinding community mitigation strategies in an influenza pandemic. Emerg Infect Dis. 2008;14:365–372. doi: 10.3201/eid1403.070673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aledort JE, Lurie N, Wasserman J, Bozzette SA. Nonpharmaceutical public health interventions for pandemic influenza: an evaluation of the evidence base. BMC Public Health. 2007;7:208. doi: 10.1186/1471-2458-7-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Writing Group. Nonpharmaceutical interventions for pandemic influenza, national and community measures. Emerg Infect Dis. 2006;12:88–94. doi: 10.3201/eid1201.051371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartley DM, Nelson NP, Perencevich EN. Antiviral drugs for treatment of patients with pandemic (H1N1) 2009 virus [letter] Emerg Infect Dis. 2009;15:1851–1852. doi: 10.3201/eid1511.090720. Available at: http://www.cdc.gov/EID/content/15/11/1851.htm. Accessed January 10, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruiz R. Behind the H1N1 vaccine shortage. Forbes.com. Available at: http://www.forbes.com/2009/10/27/swine-fluvaccine-lifestyle-health-h1n1-shortage.html. Published October 30, 2009. Accessed January 10, 2010.
- 12.Associated Press. Poll: one-third of parents oppose H1N1 vaccines. USA Today. Available at: www.usatoday.com/news/health/2009-10-07-swine-flu-poll N.htm. Published October 7, 2009. Accessed January 10, 2010.
- 13.Brug J, Aro AR, Richardus JH. Risk perceptions and behaviour: towards pandemic control of emerging infectious diseases. Int J Behav Med. 2009;16:3–6. doi: 10.1007/s12529-008-9000-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor M, Raphael B, Barr M, Agho K, Stevens G, Jorm L. Public health measures during an anticipated influenza pandemic: factors influencing willingness to comply. Risk Manage Health Care Policy. 2009;2:9–20. doi: 10.2147/RMHP.S4810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finkelstein S, Prakash S, Nigmatulina K, Klaiman T, Larson R. Pandemic Influenza: Non-pharmaceutical Interventions and Behavioral Changes That May Save Lives. Cambridge, MA: Harvard School of Public Health and MIT; 2009. Available at: http://blossoms.mit.edu/video/larson2/larson2-state-plans.pdf. Accessed January 10, 2010. [Google Scholar]
- 16.Kelso JK, Milne GJ, Kelly M. Simulation suggests that rapid activation of social distancing can arrest epidemic development due to a novel strain of influenza. BMC Public Health. 2009;9:117. doi: 10.1186/1471-2458-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Milne GJ, Kelso JK, Kelly HA, Huband ST, McVernon J. A small community model for the transmission of infectious diseases: comparison of school closure as an intervention in individual-based models of an influenza pandemic. PLoS One. 2008;3(12):e4005. doi: 10.1371/journal.pone.0004005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lau JTF, Griffiths S, Choi KC, Tsui HY. Widespread public misconception in the early phase of H1N1 influenza epidemic. J Infect. 2009;59:122–127. doi: 10.1016/j.jinf.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research and Practice. San Francisco, CA: Wiley and Sons; 2002. Cited by: University of Twente. Health Belief Model. Available at: http://www.utwente.nl/cw/theorieenoverzicht/Theory%20clusters/Health%20 Communication/Health Belief Model.doc/. Accessed October 6, 2010. [Google Scholar]
- 20.Hayward A. Influenza A(H1N1) pandemic: true or false alarm. J Epidemiol Community Health. 2009;63:775–776. doi: 10.1136/jech.2009.096628. [DOI] [PubMed] [Google Scholar]
- 21.Coach K. Forget H1N1, the real pandemic is hysterical media coverage. Media Coach Blog. Available at: http:///www.mediacoachblog.wordpress.com/2009/11/08/forget-h1n1-the-real-pandemic-is-hysterical-media-coverage/. Updated November 8, 2009. Accessed January 10, 2010.
- 22.Dykstra P. Media mayhem: bad news, and news done badly. Mother Nature Network. Available at: http://www.mnn. com/technology/research-innovations/stories/media-mayhem-bad-news-and-news-done-badly. Published May 11, 2009. Accessed January 10, 2010.
- 23.The HHS Interagency Public Affairs Group on Influenza Preparedness and Response, Centers for Disease Control and Prevention. Know what to do about the flu. Flu.gov. Available at: http://www.flu.gov. Updated 2010. Accessed January 10, 2010.
- 24.National Center for Health Marketing, Coordinating Center for Health Information and Service, Centers for Disease Control and Prevention. H1N1 Flu. 2009. Available at: http://www.cdc.gov/h1n1flu. Updated 2010. Accessed January 10, 2010.
- 25.May L, Katz R, Johnston L, Sanza M, Petinaux B. Assessing physicians’ in training attitudes and behaviors during the 2009 H1N1 influenza season: a cross-sectional survey of medical students and residents in an urban academic setting. Influenza Other Respir Viruses. 2010;4:267–275. doi: 10.1111/j.1750-2659.2010.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brewed NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26:136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 27.Holland Jones J, Salathe M. Early assessment of anxiety and behavioral response to novel swine-origin influenza A(H1N1) PLoS ONE. 2009;4(12):e8032. doi: 10.1371/journal.pone.0008032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacobs J, Taylor M, Agho K, Stevens G, Barr M, Raphael B. Factors associated with increased risk perception of pandemic influenza in Australia. Influenza Res Treat. 2010. Article 947906. doi: 10.1155/2010/947906. [DOI] [PMC free article] [PubMed]
- 29.Rubin GJ, Amlot R, Page L, Wessely S. Public perceptions, anxiety, and behavior change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339:b2651. doi: 10.1136/bmj.b2651. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]


