Abstract
Background:
Nowadays, biliary-enteric drainage (BED) is regarded as a last resort or obsolete therapeutic method for common bile duct stone (CBDS) not only because of advances in minimally invasive therapeutic modalities but also due to fears of higher morbidity, cholangitis, and “sump” syndrome.
Aim:
The present study aimed at evaluating the outcome of this procedure for choledocholithiasis.
Materials and Methods:
It is a retrospective review of 51 patients who underwent open choledochoenterostomy for CBDS between January 2005 and December 2009.
Results:
About 40 women (78%) and 11 men underwent open BED (mean age 72 years). Indications were elderly patients (90%), multiple stones (54.9%) and unextractable calculi (15.4%). We performed 49 (96%) side to side choledochoduodenostomies, one end to side choledochoduodenostomy (CDS) and one end to side hepaticojejunostomy. The mortality rate was 3.9%. Overall morbidity was 12% with no biliary leakage. With a decline of 1-6 years, neither sump syndrome nor cholangiocarcinoma occurred.
Conclusions:
Side-to-side CDS is a safe and highly effective therapeutic measure, even when performed on ducts less than 15 mm wide, provided a few technical requirements are respected. Patients experiencing relapsing cholangitis after BED should be closely monitored for the late development of biliary tract malignancies.
Keywords: Cholangiocarcinoma, Cholangitis, Choledochoduodenostomy, Sump syndrome
Introduction
In the past decade, written communications about biliary-enteric drainage (BED) have significantly decreased throughout the world. In fact, the indications for this surgical modality of common bile duct stone (CBDS) have been limited with the advances and increasing experience in laparoscopic and endoscopic procedures.
The advantages offered by this procedure, as well as its risks and disadvantages, also have been well noted in most of the already quoted bibliographic references. However, with three exceptions, the long-term results of choledochoduodenostomy (CDS), particularly in reference to the incidence of complications such as cholangitis, “sump syndrome” and risk of late development of cholangiocarcinoma have not been documented clearly.
This retrospective study reviews the results of 51 consecutive cases of open biliary-enteric bypass carried out for CBDS over a period of 5 years. Our objective was to review the indications and outcome of this procedure in the endoscopic and laparoscopic era.
Materials and Methods
We conducted a descriptive retrospective chart review of all the patients undergoing open BED for CBDS in General Surgery Department at Farhat Hached Hospital of Sousse in Tunisia between January 2005 and December 2009. Data were collected from patient's medical folders with particular attention to perioperative course, symptoms, complications, hospital length of stay, and mortality. Short-term outcomes were assessed through clinical reports at outpatient follow-up and hospital readmissions. Operative death or complications were considered as those occurring within 30 days of surgery.
The main surgical technique used was a side to side CDS after washing systematically the CBD without verifying its clearance by a choledocoscope or a cholangiogram. Kocherization of the duodenum was performed when necessary. The anastomosis was constructed with 4-0 Vicryl suture with small atraumatic needles in a continuous running (anterior and posterior rows) or interrupted fashion: It was left to the surgeon's discretion to select the type of suturing. Its opening was no smaller than 15 mm in diameter. End to side CDS and hepaticojejunostomy (HJS) were scarcely performed.
Results
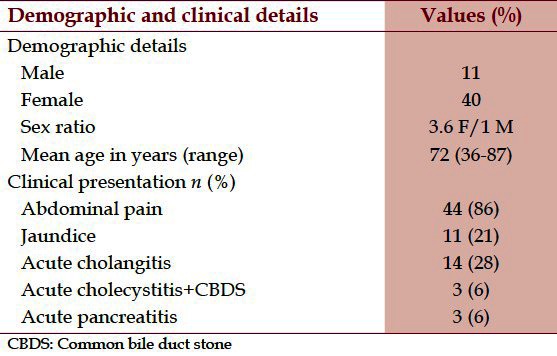
Ninety-three patients were treated for CBDS with several procedures during the 5 years period. Only 51 (40 women [78%] and 11 men) underwent open BED. The age range was 36-87 years with mean age 72 years (standard deviation [SD] 9,7). They presented with acute cholangitis (28%), abdominal pain (86%), jaundice (21%), acute pancreatitis (6%), and acute cholecystitis with asymptomatic CBD stone (6%). Two patients had severe acute cholangitis and hemodynamic failure managed with catecholamines. Table 1 summarizes these demographic and clinical details.
Table 1.
Demographic and clinical details of 51 patients
The main indications for biliary enteric bypass were elderly patients (90% were over 65 years old), multiple (atleast 5) stones (54.9%) and unextractable calculi (15.7%). The remaining patients had different clinical and intra-operative presentation: Congenital biliary cyst (1 case), accidental intra-operative transection of CBD with transversal cholédochotomy (1 case), cholécysto-choledochal fistulas (1 case), suspicious chronic pancreatitis associated with CBD calculi (1 young woman) and a recurrent lithiasis in an old woman with permanent biliary stenting.
We performed side to side CDS in 49 patients (96%) and end to side type in one patient who had iatrogenic transection of CBD. The last patient had end to side HJS after congenital biliary cyst was resected. The CBD diameter was larger than 16 mm in 37.3% of the patients and 10 mm in 98% of the patients. The mean operative time was 174 min (range 80-350).
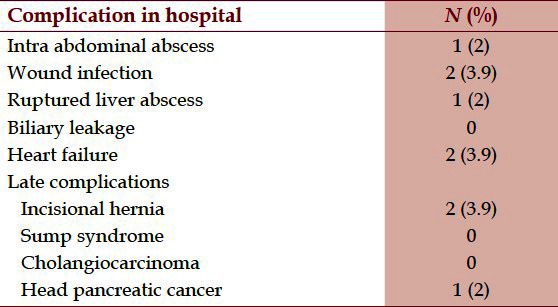
Post-operative complications [Table 2] occurred in 5 (10%) patients, including one case of intra-abdominal abscess (2%) successfully managed by transparietal drainage, wound infection (4%), two cases of heart failure (3.9%) and one patient had post-operative peritonitis subordinate to ruptured liver abscess previously unnoticed, he was re-operated and had successful peritoneal toilet. There was no biliary leakage. Post-operative deaths: Two patients (3.9%) died in the hospital during the same hospitalization for their CDS. The first was an 80-year-old woman with cardiac history admitted for acute cholecystitis associated to asymptomatic CBDS; she died of post-operative heart failure. The second was a 76-year-old woman admitted for severe acute cholangitis with hemodynamic failure. She died of sepsis and multiple organ system failure.
Table 2.
Post-operative complications
The mean hospital stay was 10.9 days (SD 6.5) and the mean post-operative stay was 7 days (SD 3.8). Eight patients left the hospital in good condition and were lost to follow-up, so it is presumed that their intervention was initially successful. They never come to outpatient control.
During the follow-up (1-6 years) of the remaining patients, two had further intervention for right subcostal incisional hernia and one presented non-resectable head pancreatic cancer with multiple liver metastases 1 year after CDS. There was no occurrence of cholangitis, hepatic abscess, and sump syndrome.
Discussion
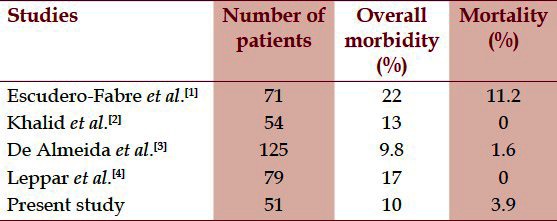
Our data corroborating others, as illustrated in Table 3, indicate that side to side CDS is a very safe procedure with low morbidity and mortality. No long-term complications, as cholangitis, sump syndrome, or cholangiocarcinoma were observed. Nevertheless, we believe that we have to consider a longer follow-up.
Table 3.
Comparison of outcomes of different studies
It should be noticed that we opted for BED because of not only its benefits mentioned further in the text but also the lack of interventional endoscopist and laparoscopic instruments particularly the helical basket in our hospital. Indeed CDS provides a safe and effective biliary drainage when carried out for carefully chosen indications. The procedure may still be required in selected cases, even with all the endoscopic and laparoscopic advances.[2] We performed the side to side type of CDS for 49 patients (96%) including two young women (36- and 38-years-old) as it is technically easier and faster than its end to side variety and HJS. It also permits to avoid the particular problem of residual stone. These criteria are capital when choosing among BED modalities particularly for high risk and elderly patients. Furthermore, the latter with their limited life expectancy should not develop long-term complications.
All our patients underwent open surgery. Reports on laparoscopic CDS have been published, but these procedures need considerable experience and expensive technologies.[5,6] The two most notable objections to CDS are the possibility of cholangitis and the presence of the symptoms produced by the so called “sump/blind sac” syndrome. Thus many authors suggested a CBD diameter larger than 16 mm precaution to allow a CDS with an opening no smaller than 14 mm in diameter.[1–7] Our study, with no such complications, disproves this condition (only 37% of patients had CBD diameter larger than 16 mm). Moreover, De Almeida[3] ensured that a wide anastomosis can be constructed even on a duct 10-12 mm wide, and this concur with our results (98% of our patients had CBD ≥ 10 mm). Meticulous and precise suturing is also essential.[1,2] Such well performed CDS prevents bile stasis, avoids the buildup of excessive intra-ductal pressure and permits a free flow of common duct contents including duodenal reflux as well as eventual retained/recurrent lithiasis back in the duodenum. The prevalence of blind sac syndrome is reported between 2.5% and 9.6% in several studies. It presumably derives from stasis and refluxed duodenal contents (food, stones, or debris) in to the terminal common duct, with bacterial overgrowth enhancing bile salt deconjugation. So Factors leading to sump syndrome are a wide distal choledoque, papillary stenosis, retained stones, and anastomosis stricture. This phenomenon leads to diarrhea, as observed in the “blind-loop” syndrome arising anywhere else in the gut, can cause secondary liver abscess and facilitates deposition and reformation of calcium bilirubinate stones which could not be documented in spite of an exhaustive search. A very wide anastomosis could be the explanation.[8–10]
In order to avoid this so feared syndrome, Lasnier[11] recommended end to side CDS for young patient or in case of incomplete clearance of CBD and/or Oddi dysfunction. Otherwise they opted for side to side CDS specially for elderly patients, in case of altered anatomy after Billroth II surgery, and when he faced up to technical difficulties due to inflammation, sclerosis and portal hypertension. Endoscopic sphincterotomy has been recommended as the primary and definitive treatment modality. However, Mavrogiannis[12] reported a considerably high recurrence rate 19% (6 patients/31) of the syndrome (restenosis of the sphincterotomy opening) after initially successful such management. It occurred 31-72 months (median: 58.5 months) after the initial treatment and new endoscopic treatment with a papillotomy was effective. In case of stoma stricture the best treatment is the endoscopic balloon cholangioplasty.[4–13] The blind sac syndrome associated to side to side HJS is extremely rare. Indeed only four cases were reported in the literature.[14] Stricture is the main complication of HJS and rates, in most series, varies from 0% to 12%[15] (with most being around 8%) and from 2.4 to 4.8% in case of biliary lithiasis.[2] Mortality rates vary from 2-7%.[15] Technique requirements for a good anastomosis are good submucosal apposition, single-layer closure, and mucosal inversion.
In case of hepatolithiasis, BED results in high frequency of reflux cholangitis and thus should be abandoned.[16] In recent years the number of reports of cholangiocarcinoma occurring in patients who previously had BED many years ago, has been increasing, so it has been suggested as a possible long-term complication of these surgical procedures. Its incidence ranges from 2.8-7.4% at interval average of 10 years after choldechoenterostomy.[17–20]
The direct connection between the intestinal tract and biliary tree and reflux of activated pancreatic juice and intestinal bacteria into the biliary tract are considered as the factors causing chronic relapsing cholangitis, the latter has been suspected as a predisposing factor for the late development of cholangiocarcinoma.[21] BED permits free communication between gastro-intestinal and biliary tracts, depriving the anti-reflux function of the sphincter of Oddi. Histologic examination of resected specimens, including cholangiocarcinoma of the biliary tract arising from long-standing cholangitis secondary to a bilioduodenal drainage, has shown, at sites distant from the malignancy, various degrees of hyperplastic lesions occurring in the area of cholangitis.[18] This strengthens the hyperplasia-dysplasia-carcinoma progression hypothesis of a biliary carcinogenesis mechanism.[22,23] The Roux-en-Y technique is the one expected to produce lower rates of cholangitis because it is immune to pancreatic reflux and less prone to intestinal bacterial backflow because of the protective action exerted by the interposed jejunal loop. Tocchi[21] reported a retrospective study of 1003 patients who underwent biliary enteric anastomosis (transduodenal sphincteroplasty, CDS, and HJS) for benign disease with 129.6 years mean follow-up: Univariate and multivariate analysis showed a significantly higher incidence of cholangiocarcinoma in the CDS group (P = 0.02), and cholangitis was confirmed to be the only independent factor affecting its incidence (P = 0.001, odds ratio 35.7). Thus HJS should be considered straightaway for young patients in spite of CDS benefits. Moreover, complicated CDS should be transformed in HJS.[11] Uchiyama, et al.[24] related four gastric cancers (9%) occurring 8-11 years after CDS. They also noted that patients with such anastomosis had higher incidence of gastric lesions when compared to those with T-tube drainage or endoscopic sphincterotomy. The fact that one of our patients presented non-resectable and metastatic head pancreatic cancer 1 year after the CDS, suggests that the tumor was present at the time of BD but was not detected. Large retrospective studies and prospective randomized trials are needed to establish the definitive risk for late biliary carcinogenesis after bilio-intestinal drainage. Thus we suggest that any patient treated with these procedures and experiencing relapsing cholangitis should be monitored for the late development of bile duct cancer.
In case of asymptomatic CBS, we readily opt for minimally invasive techniques (laparoscopy and/or endoscopy) for young patients or fine CBD. Indeed considering CDS inconvenients, it was performed for only old patients with dilated CBD provided that surgery isn’t considered inappropriate.
Conclusions
Open biliary drainage procedures may still indicated in select patients where the facility or expertise for minimally invasive biliary procedures is not available.
Side-to-side CDS is a safe and highly effective therapeutic measure, even when performed on ducts less than 15 mm wide, provided a few technical requirements are respected. It should only be considered as obsolete after extensive, long-term, prospective, randomized assessments of laparoscopic or combined laparo-endoscopic approaches have been shown to be as effective as or superior to CDS even in young population. Patients experiencing relapsing cholangitis after BED should be closely monitored for the late development of biliary tract malignancies. The procedure should be regarded as an essential in the general surgical knowledge and training.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Escudero-Fabre A, Escallon A, Jr, Sack J, Halpern NB, Aldrete JS. Choledochoduodenostomy. Analysis of 71 cases followed for 5 to 15 years. Ann Surg. 1991;213:635–42. doi: 10.1097/00000658-199106000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khalid K, Shafi M, Dar HM, Durrani KM. Choledochoduodenostomy: Reappraisal in the laparoscopic era. ANZ J Surg. 2008;78:495–500. doi: 10.1111/j.1445-2197.2008.04542.x. [DOI] [PubMed] [Google Scholar]
- 3.De Almeida AC, dos Santos NM, Aldeia FJ. Choledochoduodenostomy in the management of common duct stones or associated pathology: An obsolete method? HPB Surg. 1996;10:27–33. doi: 10.1155/1996/47821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leppard WM, Shary TM, Adams DB, Morgan KA. Choledocho-duodenostomy: Is it really so bad? J Gastrointest Surg. 2011;15:754–7. doi: 10.1007/s11605-011-1465-2. [DOI] [PubMed] [Google Scholar]
- 5.Rhodes M, Nathanson L. Laparoscopic choledochoduodenostomy. Surg Laparosc Endosc. 1996;6:318–21. [PubMed] [Google Scholar]
- 6.Cuschieri A, Adamson GD. Multimedia article Laparoscopic transection choledochoduodenostomy. Surg Endosc. 2005;19:728. doi: 10.1007/s00464-004-6021-7. [DOI] [PubMed] [Google Scholar]
- 7.Aldrete JS. Choledochoduodenostomy. Operative Techniques in General Surgery. 2000;2(4):304–10. [Google Scholar]
- 8.Toshikuni N, Kai K, Sato S, Kitano M, Fujisawa M, Okushin H, et al. Pyogenic liver abscess after choledochoduodenostomy for biliary obstruction caused by autoimmune pancreatitis. World J Gastroenterol. 2006;12:6397–400. doi: 10.3748/wjg.v12.i39.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cetta F. The role of bacteria in pigment gallstone disease. Ann Surg. 1991;213:315–26. doi: 10.1097/00000658-199104000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cetta F. Do Surgical and endoscopic sphincterotomy prevent or facilitate recurrent common duct stones reformation? Arch Surg. 1993;128:329–35. doi: 10.1001/archsurg.1993.01420150085016. [DOI] [PubMed] [Google Scholar]
- 11.Lasnier C, Kohneh-Shahri N, Paineau J. Biliary-enteric anastomosis malfunction: Retrospective study of 20 surgical cases. Review of literature. Annales de chirurgie. 2005;130:566–72. doi: 10.1016/j.anchir.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Mavrogiannis C, Liatsos C, Romanos A, Goulas S, Dourakis S, Nakos A, et al. Sump syndrome: Endoscopic treatment and late recurrence. Am J Gastroenterol. 1999;94:972–5. doi: 10.1111/j.1572-0241.1999.998_t.x. [DOI] [PubMed] [Google Scholar]
- 13.Caroli-Bosc FX, Demarquay JF, Peten EP, Dumas R, Bourgeon A, Rampal P, et al. Endoscopic management of sump syndrome after choledochoduodenostomy: Retrospective analysis of 30 cases. Gastrointest Endosc. 2000;51:180–3. doi: 10.1016/s0016-5107(00)70415-9. [DOI] [PubMed] [Google Scholar]
- 14.Morrissey PE, Burns GA, Cohn SM. Sump syndrome complicating Roux-en-Y hepaticojejunostomy: Case report and review of the literature. Surgery. 1996;119:403–5. doi: 10.1016/s0039-6060(96)80139-5. [DOI] [PubMed] [Google Scholar]
- 15.Sutherland F, Dixon E. Extramucosal hepaticojejunostomy. Am J Surg. 2005;189:667–9. doi: 10.1016/j.amjsurg.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Ling XF, Xu Z, Wang LX, Hou CS, Xiu DR, Zhang TL, et al. Long-term outcomes of choledochoduodenostomy for hepatolithiasis. Chin Med J (Engl) 2010;123:137–41. [PubMed] [Google Scholar]
- 17.Strong RW. Late bile duct cancer complicating biliary-enteric anastomosis for benign disease. Am J Surg. 1999;177:472–4. doi: 10.1016/s0002-9610(99)00087-2. [DOI] [PubMed] [Google Scholar]
- 18.Hakamada K, Sasaki M, Endoh M, Itoh T, Morita T, Konn M. Late development of bile duct cancer after sphincteroplasty: A ten- to twenty-two-year follow-up study. Surgery. 1997;121:488–92. doi: 10.1016/s0039-6060(97)90101-x. [DOI] [PubMed] [Google Scholar]
- 19.Chijiiwa K, Ichimiya H, Kuroki S, Koga A, Nakayama F. Late development of cholangiocarcinoma after the treatment of hepatolithiasis. Surg Gynecol Obstet. 1993;177:279–82. [PubMed] [Google Scholar]
- 20.Bettschart V, Clayton RA, Parks RW, Garden OJ, Bellamy CO. Cholangiocarcinoma arising after biliary-enteric drainage procedures for benign disease. Gut. 2002;51:128–9. doi: 10.1136/gut.51.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: A follow-up study of more than 1,000 patients. Ann Surg. 2001;234:210–4. doi: 10.1097/00000658-200108000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrén-Sandberg A. Diagnosis and management of gallbladder polyps. N Am J Med Sci. 2012;4:203–11. doi: 10.4103/1947-2714.95897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrén-Sandberg A. Diagnosis and management of gallbladder cancer. N Am J Med Sci. 2012;4:293–9. doi: 10.4103/1947-2714.98586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uchiyama K, Onishi H, Tani M, Kinoshita H, Kawai M, Ueno M, et al. Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg. 2003;238:97–102. doi: 10.1097/01.sla.0000077923.38307.84. [DOI] [PMC free article] [PubMed] [Google Scholar]


