Abstract
Background:
Hepatitis-B infection is not commonly perceived as a serious medical problem in Nigeria. However, chronic hepatitis-B infection, which is a subject of global concern, may lead to lethal liver diseases.
Aim:
The study was to determine the sero-epidemiology of hepatitis-B surface antigenaemia among adult Nigerians with clinical features of liver diseases attending a primary-care clinic in a resource-constrained setting of Eastern Nigeria.
Materials and Methods:
A cross-sectional study was carried out on 140 adult Nigerians with clinical features of liver diseases at the primary-care clinic of Federal Medical Centre, Owerri. They made up three groups: 44 patients, 62 patients and 34 patients with clinical features of hepatitis, liver cirrhosis and hepatocellular carcinoma, respectively. Hepatitis-B surface antigen (HBsAg) was assayed using an immunochromatographic method. Demographic variables were collected.
Results:
The overall sero-positivity rate was 50.7%. The sero-positivity rates for these patients were 23.9%, 39.5% and 36.6% for hepatitis, liver cirrhosis and hepatocellular carcinoma, respectively. The age group 40-60 years (P = 0.048) and artisans (P = 0.019) were significantly infected. Abdominal swelling (86.4%) and ascites (67.1%) were the most common symptoms and signs, respectively.
Conclusion:
HBsAg prevalence was high and has significant association with age and occupation.
Keywords: Epidemiology, Hepatitis-B surface antigenaemia marker, hospital, liver diseases, Nigeria, resource-constrained
Introduction
Hepatitis-B surface antigen (HBsAg) has been the subject of research ever since Blumberg and his associates discovered the antigen.[1,2] Globally, hepatitis-B virus (HBV) infection has been reported as one of the aetiological agents for hepatitis, liver cirrhosis and hepatocellular carcinoma.[3,4] However, in sub-Saharan African countries, HBV infection has been one of the treatable and preventable causes of morbidity and mortality, and a threat to socio-economic development in the sub-region.[2,5] The sub-Saharan African countries are also the same nations where a large number of people die from the scourge of treatable and preventable diseases such as HIV/AIDS, malaria and tuberculosis.
The prevalence of HBV infection varies geographically throughout the regions of the world from high (> 8%), intermediate (2-7%) to low (< 2%) prevalence rates.[6] Globally, about 2 billion people (one-third of the global population) have been infected while about 360 million people are chronic carriers, harbouring the virus in their liver and blood.[7] HBV infection is the tenth leading cause of death from communicable diseases worldwide causing 500,000 to 1.2 million deaths per year due to acute hepatitis, chronic hepatitis, liver cirrhosis and hepatocellular carcinoma.[3]
Variable frequencies of HBV-induced liver diseases have been reported throughout the world,[8–11] although higher in developing countries such as Nigeria where it is hyper-endemic and pandemic.[12–16] In Nigeria, about 18 million people (about 15% of the 120 million population) are infected chronically[17] and prevalence of HBsAg has been reported in various parts of the country: 10.3% was reported in the urban community in Jos, Nigeria;[17] 12.6% was reported in rural Nigeria;[18] and 14.5% reported in hospital patients in Port Harcourt, Nigeria.[19] Research findings in Nigeria have shown that HBV infection is one of the aetiological agents of liver diseases[13–15] and liver diseases have also been found to be prevalent in HBV infection endemic areas.[20–23] In Maiduguri, Northern Nigeria, HBsAg prevalence of 49%, 56% and 50% were detected among patients with HBV-related hepatitis, liver cirrhosis and hepatocellular carcinoma, respectively.[21] Similarly, in Lagos, Southern Nigeria, the reported frequencies were 14%, 30% and 56% for HBV related hepatitis, liver cirrhosis and hepatocellular carcinoma, respectively.[22]
HBV infection is therefore an important clinical and public health problem in Nigeria.[23] Of great concern in Nigeria is that HBV infection is not commonly perceived as a serious medical problem[2] despite the fact that HBV and HIV infections share similar mode of transmission and risk factors.[8] There is poverty of data on the magnitude of HBV-related liver diseases in the primary-care clinics in Nigeria. The early recognition of HBV-related liver diseases by clinicians working in primary-care clinics is quintessential to its management, while identifying its basic epidemiological correlates avails great opportunities for prevention and control.[24] This study therefore posits the relevance of screening adult Nigerians with clinical features of liver diseases for HBsAg in primary-care settings. It is against this background that the authors aimed at determining the sero-epidemiology of HBsAg among adult Nigerians with clinical features of liver diseases attending a primary-care clinic in a resource-constrained setting of Eastern Nigeria.
Materials and Methods
Ethical certificate was obtained from the Ethics Committee of the hospital. Informed verbal consent was also obtained from the patients included in the study.
This was a clinic-based descriptive, cross-sectional study carried out from June 2006 to June 2007. A total of 140 adult patients with clinical features of liver diseases were screened for HBsAg, a specific serological marker of HBV infection, at the Department of Family Medicine of Federal Medical Centre, Owerri, a tertiary hospital in Imo State, South-Eastern Nigeria. The Federal Medical Centre is located in the municipal city of Owerri. It is a tertiary hospital established with the tripartite mandate of service delivery, training and research, and serves as a referral centre for primary and secondary public health institutions, as well as missionary and private hospitals in Imo State and the neighbouring states of Abia, Ebonyi, Rivers and Akwa Ibom of Nigeria. Department of Family Medicine serves as a primary-care clinic within the tertiary hospital setting of the medical centre. All patients, excluding paediatric patients and antenatal women, are first seen at Department of Family Medicine where diagnoses are made. Patients who need primary care are managed and followed up in the clinic whereas those who need other specialists’ care are referred to the respective core specialist clinics for further management. The clinic is run by consultant family physicians and postgraduate resident doctors in family medicine.
Inclusion and exclusion criteria
The inclusion criteria were patients aged ≥ 15 years who gave informed consent and had clinical features of liver diseases. The exclusion criterion included pregnant patients and critically ill patients.
Sample size determination
A sample size of 140 was used in this study. The sample size (N) was calculated using the formula[25] N = pq/SE2, where N = sample size, P = prevalence of HBV infection, q = 100 − p, SE = sampling error tolerated (%). A prevalence of 38% was used based on a previous study in Maiduguri, Nigeria.[21] The margin of sampling error tolerated was 5%. Therefore N = 38 (100-38)/52 = 94.
The calculated minimum sample size was 94. However, to improve the precision of the study, the estimated sample size (Ns) was determined considering an anticipated response rate of 50% (0.5). The estimated sample size (Ns) was determined by dividing the original calculated sample size (N) by the anticipated response rate[26] as follows, Ns = N/0.5, where N = minimum calculated sample size, Ns = selected sample size, anticipated response rate = 0.5. Thus, the estimated sample size = 94/0.5 = 188. However, a sample size of 140 patients was used based on the proposed duration of the study.
Sampling technique
Sample selection was done consecutively using every adult patient who had clinical features of liver diseases. This sampling technique was judgementally chosen by the authors based on the fact that the researchers believed that those selected were likely to be representative of the study population.[26]
Universal demographic variables
The basic demographic variables collected from the study population included age, sex, marital status, education and occupation. Social classification of patients was into lower, middle and upper occupational classes to suit the Nigerian environment.[27] Artisans refer to manual workers and include masons (bricklayers), fitter mechanics, electricians, tailors, seamstresses, hair dressers and carpenters.
Diagnostic procedures
Patients with clinical features of liver diseases were offered HBsAg test after informed verbal explanation and consent. Two millilitres of venous blood were collected from each patient from the ante-cubital fossa after thorough aseptic cleaning. Whole venous blood was tested for HBsAg using a commercially available rapid sero-diagnostic kit: One-step test strip manufactured by ACON Laboratories Inc. (Sorrento Valley, San Diego, CA, USA). The test strip uses whole blood, serum or plasma. The dipstick test strip is a rapid, qualitative, one-step immunoassay based on the immunochromatographic principle. This method employs unique combinations of a monoclonal dye conjugate (colloidal gold) and polyclonal solid-phase antibodies to selectively identify HBsAg with high specificity and sensitivity. The test kit has a sensitivity of 99.9% and specificity of 100%. The manufacturer's standard operating procedures were strictly followed.
Diagnostic criteria
Patients with clinical features of liver disease present with constitutional, hepatic and extra-hepatic features,[28,29] which were grouped into three. Histopathological examination was not performed. The three groups were:
Group-1 (hepatitis patients): These were patients with hepatitis with clinical features of fever, anorexia, nausea, malaise, fatigue, dark urine, pale stool, pruritus, joint pain, jaundice, right upper quadrant abdominal pain and tender hepatomegaly.
Group-2 (liver cirrhosis patients): This group was made up of patients with liver cirrhosis who had clinical features of fatigue, malaise, weight loss, abdominal swelling, pruritus, jaundice, reduced liver span, ascites, splenomegaly, pedal oedema, muscle wasting, varicel bleeding, spider naevi, gynaecomastia and testicular atrophy in men.
Group-3 (hepatocellular carcinoma patients): This group consisted of patients with hepatocellular carcinoma who had clinical features of anorexia, nausea and vomiting, marked weight loss, marked abdominal swelling, jaundice, marked muscle wasting, irregular and hard liver, a bruit or friction rub over the liver on auscultation, marked ascites, hepatomegaly and marked pedal oedema.
Statistical analysis
Results generated were analyzed using software Statistical Package for Social Sciences (SPSS) version 13.0 (Microsoft Corporation Inc., Chicago, IL, USA) for calculation of percentages for categorical variables and mean for continuous data. χ2-Test was used to assess the significance of differences among groups. In all cases P < 0.05 was considered significant in all statistical comparisons.
Results
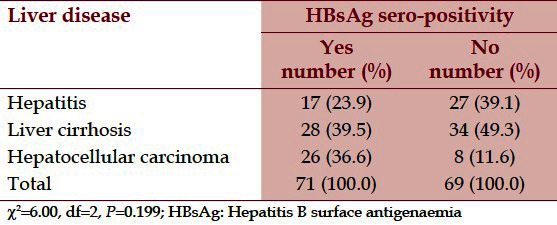
The overall sero-positivity rate was 50.7%. The sero-positivity rates for the three groups of patients were 23.9%, 39.5% and 36.6% for hepatitis, liver cirrhosis and hepatocellular carcinoma, respectively. The sero-positivity rates for the three groups of patients were not statistically significant (χ2 = 6.00, df = 2, P = 0.199) [Table 1].
Table 1.
Distribution of patients based on HBsAg sero-positivity
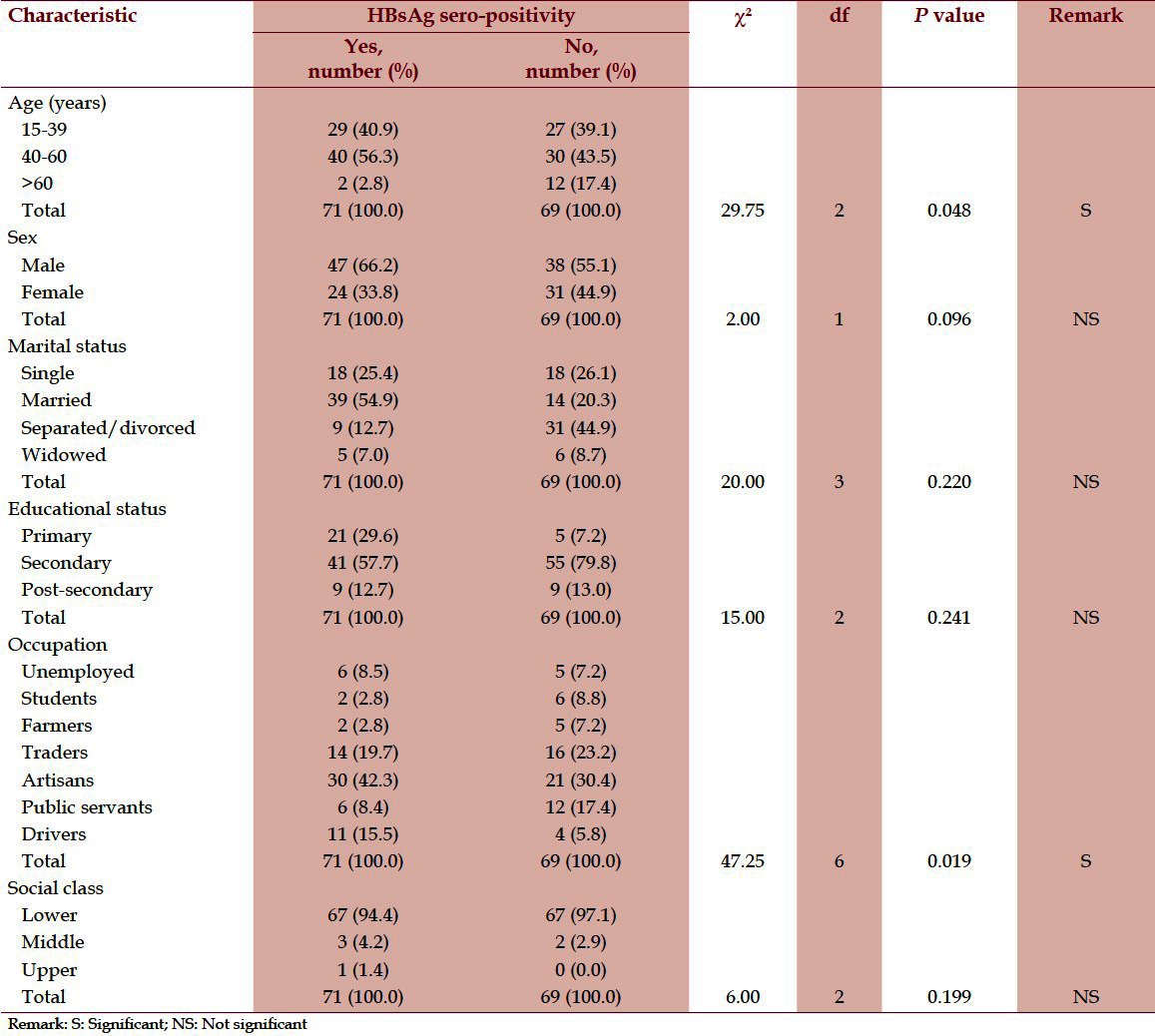
Bivariate analysis of socio-demographic variables as related to HBsAg sero-positivity showed that age (χ2 = 29.7, df = 2, P = 0.048) and occupation (χ2 = 47.2, df = 8, P = 0.019) were statistically significant. The age group 40-60 years and artisans were significantly infected. Socio-economic variables such as sex, marital status, educational attainment and socio-economic class were not statistically significant [Table 2].
Table 2.
Socio-demographic characteristics as related to HBsAg sero-positivity
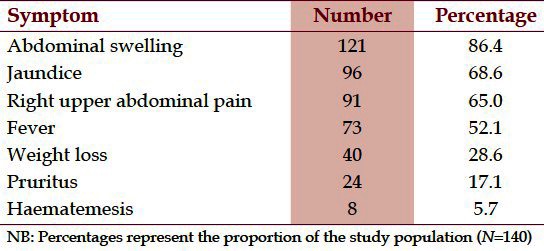
Abdominal swelling constituted the most common symptom and was documented in 86.4% of the patients. Jaundice and right upper quadrant abdominal pain also occurred frequently and were seen in 68.6% and 65.0% of the patients, respectively. Fever and weight loss were present in 52.1% and 28.6% of the study population, respectively. Less common symptoms were pruritus (17.1%) and haematemesis (5.7%) [Table 3].
Table 3.
Distribution of patients based on symptoms of liver diseases
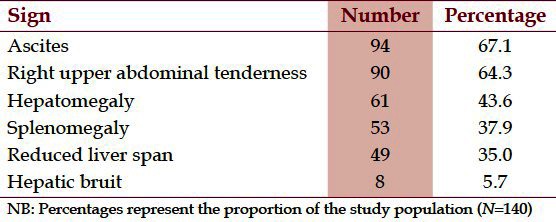
Ascites was the most common sign found in 67.1% of the patients. Right upper quadrant abdominal tenderness and hepatomegaly occurred in 64.3% and 43.6% of the study population, respectively. Less common signs were splenomegaly (37.9%), reduced liver span (35.0%) and hepatic bruit (5.7%) [Table 4].
Table 4.
Distribution of patients based on signs of liver diseases
Discussion
The finding of a HBsAg sero-prevalence of 50.7% in this study is higher than 38.0% reported in Maiduguri,[21] Northern Nigeria. However, the HBsAg sero-prevalence in this study is lower than 54.8% reported in Lagos, South-West Nigeria by Ola et al., in 2007[13] and 58.1% reported in another study in Lagos, South-West Nigeria by Lesi et al., in 2004.[22] This high prevalence of HBsAg in this study and other studies[13,21,22] is a reflection of the fact that these were patients who had clinical features of liver diseases. The findings of this study corroborate previous reports that HBV infection exists in patients with liver diseases and may have a significant relationship with liver diseases.[5,13–15,21,22] However, socio-demographic factors may be contributory.[17–20] This study has buttressed reports that HBV infection is still an issue of clinical and public health importance in Nigeria.[2,5,14] At present in Nigeria, HBV-related liver diseases in adults are not given high priority like HIV/AIDS, but the probability of death from HBV-related liver diseases is high. Of great concern is that HBV infections can be treated or prevented with minimum input of resources.[24] In fact, the developed countries of the world have overcome many of the HBV infections and HBV-related liver diseases through preventive, promotional and risk reduction interventional measures.[9,24] This high prevalence therefore calls for urgent action by government, non-governmental organizations, civil society organizations, faith-based organizations and community-based organizations to embark on interventional measures such as public health information and education to address various factors that promote the spread of the virus. When these issues are not adequately addressed in the resource-constrained Nigerian environment, morbidity and mortality from HBV-related liver diseases may constitute an obstacle to the achievement of the Millennium Development Goals as regards infectious diseases.
The finding of a significantly higher sero-prevalence of HBV infection among patients aged 40-60 years is similar to the reports on the age predilection for HBV infections from the country.[2,17,22] According to these reports, sero-prevalence of HBsAg increases with age, suggesting that most infection occurs predominantly through horizontal transmission.[18,19] However, the pattern of age distribution in this study could be a reflection of the study population who were mainly patients with liver cirrhosis and hepatocellular carcinoma. Chronic HBV infection has been documented to usually precede liver cirrhosis and hepatocellular carcinoma by a decade.[14,17,20,21,23] This high sero-prevalence of HBsAg among this age group paints a gloomy picture in Nigeria, as this age group constitutes the most economically productive years in the Nigerian workforce who are expected to take active manpower responsibilities. Similarly, this age group comprises the most productive age group in Nigerian families who are expected to take up responsible parenthood. Major interventions for HBV-related chronic liver diseases and promotion of appropriate health-seeking behaviour among middle-aged patients with clinical features of liver diseases should be integrated as part of a comprehensive healthcare protocol in primary care.
This study observed that artisans had significantly higher sero-prevalence of HBsAg compared with other occupational groups. This could be attributed to the clustering of risk factors among the artisans, which was reported in previous studies.[21,30] Artisans are a special occupational group and often experience frequent changes in job location and socialization.[17] The artisans are more likely to have clustering of risk factors such as history of multiple unprotected sexual intercourse.[2,17,18] This factor among others may encourage exposure to HBV infection. In addition, the significantly higher sero-prevalence among the artisans in this study could be a reflection of the male predominance of artisan occupation. The reported gender epidemiological pattern of HBV infections in the endemic areas of sub-Sahara Africa was in favour of the male sex.[20–22] Accordingly, there is a rapid decline in HBsAg titres in females resulting in a shorter duration of the carrier state.[29,31] More so, males have poorer handling of HBV infections than females because of the presence of an immune-regulatory gene on the X-chromosome that determines susceptibility to infections.[29,31] This study therefore beckons for health-seeking decision-making by artisans with clinical features of liver such as early presentation to appropriate health facility.
The most common symptom and sign of liver disease in this study were abdominal swelling (86.4%) and ascites (67.1%), respectively. This finding is similar to reports from previous studies.[15,21,22] Jaundice, which has been described as the hallmark clinical feature of liver diseases, was detected in 68.6% of the patients. This most common clinical feature could be an indication that clinically identified patients with liver diseases had liver cirrhosis and hepatocellular carcinoma, which is probably a reflection of late presentation of cases of liver diseases in the hospital. Accordingly, some cases of chronic liver diseases may be insidious in onset and may remain unrecognized until they reach the advance stage.[28] There are several reasons for the clinical features of liver diseases in this study. First and foremost, the natural history of silent or asymptomatic progression to liver cirrhosis and hepatocellular carcinoma may partly account for this observation. More so, difficult access to available health facilities, poor socio-economic status and prohibitive costs of hospital consultation may influence early presentation to hospitals in symptomatic patients. In addition, poor perception of the nature of the degree of severity of liver diseases, widespread patronage of alternative medical practitioners, patent medicine vendors, and dealers and spiritual healing homes may affect hospital referral even in patients with clinical features of liver diseases. With late presentation to hospital, intervention becomes less successful especially in hepatocellular carcinoma. The health delivery system especially primary care required for early detection and effective management of HBV-related liver diseases should be improved and strengthened in Nigeria.
Study implications
This study has important implications for clinical and public health practice. Human beings are the only reservoir of HBV infection and are of great epidemiological importance due to latent or carrier state and prolonged viraemia. Although the titre of HBsAg bears little relation with the severity of the liver disease, but detection of HBsAg in the serum is clinically relevant and provides direction for further diagnostic workup, comprehensive and continuing care. Patients with clinical features of HBV-related liver diseases need to be identified during clinical encounter in primary-care clinics through dedicated HBV-screening services. It is through this strategy in addition to other diverse preventive interventions that the vicious cycle of maintaining a high hepatitis-B surface antigenaemia in adult Nigerians in the study area can be interrupted. More so, this would expand the existing therapeutic options, and improve prognosis and survival of these patients through early detection and treatment. Screening for the HBsAg serological marker of HBV infection and perception of its implication are very important when attending to patients with clinical features of liver diseases. This study therefore envisaged the challenges of health delivery to adult patients with clinical features of liver diseases with implication for quality improvement in primary care and in line with the attainment of the Millennium Development Goals as regards infectious disease control.
Study limitations
The study had certain constraints that imposed some degree of limitations to the absolute validity of the results. This study was hospital-based, as only patients who presented to the hospital were studied. Some of the patients with HBV-related liver diseases patronise traditional and spiritual healing homes, patent medicine vendor stores and private clinics closer to their homes. However, because of the hospital-based nature of this study, bias might have been introduced and might not be a true representative of what happens in the community; hence extrapolations to the communities should be done with caution.
The limitation imposed by the descriptive nature of the study is recognised by the researchers. However, this study stimulates the need for analytical and longitudinal studies in this area. This would enable a quasi cause–effect relationship to be drawn and also for a reliable and valid conclusion to be ascertained.
The sample size was relatively small, but this was more than the minimum estimated sample size for the study and was the number of patients seen within the study period.
This study was based on testing of sera samples for HBsAg only, which does not fully reflect the epidemiology of HBV-related liver diseases.[10,14] If other serologic markers of HBV infection such as HBeAg, anti-HBs, HBV DNA and anti-HBc were assayed, the actual prevalence would probably be much higher than the present reported figures.
More so, although rapid sero-diagnostic test kits based on immunochromatographic principles are very sensitive, not all infections in the acute phase were probably detected. It was also possible that an infectious individual early in the incubation phase would not have sero-converted when tested. Similarly, several types of immunological tests such as Western blot, the enzyme-linked immunosorbent assay (ELISA) method and polymerase chain reaction (PCR)-DNA-based assays are currently used for detection of HBV infection. In this study, the use of rapid sero-diagnostic tests based on the chromatographic immunoassay technique, although found to be less sensitive than other counter-immunoelectrophoretic principles (CIEPs), can provide prompt epidemiological data for primary-care physicians, community physicians and health authorities. It can also deliver immediate useful feedback to research participants and the outcomes may assist in improving the local understanding of HBV infections in resource-poor settings.
The case selection in this study was based on clinical parameters. However, histopathological studies were not done due to the objectives, setting and scope of the study. Despite this limitation, this study provides valuable information, which can be utilised in primary-care settings, especially in resource-constrained settings, for adopting appropriate interventional measures.
Further research direction
Studies in Nigeria have indicated that HBV-related liver disease is common. However, there may be other causes of liver diseases in Nigeria such as hepatitis-C virus infection, alcohol and aflatoxins. The role of HBV infections in the aetiopathogenesis of liver diseases requires further investigation in the study area. This will provide robust clinico-pathological and epidemiological data for comparative purposes.
Conclusion
This study underscores a high prevalence of HBsAg among the study population and its significant relationship with age and occupation. Screening adult Nigerians with clinical features of liver diseases for serological marker of HBV infection should be integrated as part of baseline assessment in primary-care clinics in order to facilitate early detection and institutionalization of appropriate preventive and therapeutic interventions. Vaccination of persons at risk and provision of antiviral and immunostimulatory therapy for the infected when indicated are advocated.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Polesky HF. In: Modern blood banking and transfusion practices. 3rd ed. New York: Plenum Books; 1998. Transfusion transmitted viruses; pp. 375–87. [Google Scholar]
- 2.Emechebe GO, Emodi IJ, Ikefuna AN, Ilechukwu GC, Igwe WC, Ejiofor OS, et al. Hepatitis B virus infection in Nigeria: A review. Niger Med J. 2009;1:18–22. [Google Scholar]
- 3.Shepard CW, Simard EP, Finelli L, Fiore AE, Bell BP. Hepatitis B virus infection: Epidemiology and vaccination. Epidemiol Rev. 2006;28:112–25. doi: 10.1093/epirev/mxj009. [DOI] [PubMed] [Google Scholar]
- 4.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 5.Ola SO. Relief to the scourge of primary hepatocellular carcinoma. Niger J Med. 2002;11:156–60. [PubMed] [Google Scholar]
- 6.Alter MJ. Epidemiology of hepatitis B infection in Europe and worldwide. J Hepatol. 2003;39:64–9. doi: 10.1016/s0168-8278(03)00141-7. [DOI] [PubMed] [Google Scholar]
- 7.Zukerman AJ. More than third of world's population has been infected with hepatitis B virus. BMJ. 1999;318:1213. doi: 10.1136/bmj.318.7192.1213a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das BK, Gayen BK, Aditya S, Chakrovorty SK, Datta PK, Joseph A. Seroprevalence of hepatitis B, hepatitis C, and human immunodeficiency virus among healthy voluntary first-time blood donors in Kolkata. Ann Trop Med Public Health. 2011;4:86–90. [Google Scholar]
- 9.Omata M, Dan Y, Daniele B, Plentz R, Rudolph KL, Manns M, et al. Clinical features, etiology and survival of hepatocellular carcinoma among different countries. J Gastroenterol Hepatol. 2002;17(Suppl):40–9. doi: 10.1046/j.1440-1746.17.s1.14.x. [DOI] [PubMed] [Google Scholar]
- 10.Sakhuja P, Malhotra V, Gondal R, Sarin SK, Guptan R, Thakur V. Histological spectrum of chronic hepatitis in precore mutants and wild type hepatitis B virus infection. Trop Doct. 2004;34:147–9. doi: 10.1177/004947550403400306. [DOI] [PubMed] [Google Scholar]
- 11.Hayashi PH, Di Bisceglie AM. The progression of hepatitis B- and C-infections to chronic liver disease and hepatocellular carcinoma: Epidemiology and pathogenesis. Med Clin North Am. 2005;89:371–89. doi: 10.1016/j.mcna.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Ogunbiyi JO. Hepatocellular carcinoma in developing world. Semin Oncol. 2001;28:179–87. doi: 10.1016/s0093-7754(01)90090-9. [DOI] [PubMed] [Google Scholar]
- 13.Ola SO, Odaibo GN. Alfa-feto protein, HCV and HBV infections in Nigerian patients with primary hepatocellular carcinoma. Niger Med Pract. 2007;51:33–5. [Google Scholar]
- 14.Lesi OA, Kehinde MO, Omilabu SA. Prevalence of the HBeAg in Nigerian patients with chronic liver disease. Niger Qt Hosp Med. 2004;14:1–4. [Google Scholar]
- 15.Ndububa DA, Ojo OS, Adetiloye VA, Durosnmi MA, Olasode BJ, Famurewa OC, et al. Chronic hepatitis in Nigerian patients: A study of 70 biopsy-proven cases. West Afr J Med. 2005;24:107–11. doi: 10.4314/wajm.v24i2.28177. [DOI] [PubMed] [Google Scholar]
- 16.Adeniji KA, Anjorin AS. The pattern of malignant tumors of the liver in a tertiary health institution in Nigeria. Afr J Med Sci. 2004;33:27–30. [PubMed] [Google Scholar]
- 17.Sirisena ND, Njoku MO, Idoko JA, Isamade E, Barau C, Jelpe D, et al. Carriage rate of hepatitis-B surface antigen (HBsAg) in an urban community in Jos, Plateau State, Nigeria. Niger Postgrad Med J. 2002;9:7–10. [PubMed] [Google Scholar]
- 18.Jumbo GT, Egah DZ, Banwat EB. Hepatitis B virus infection in a rural settlement of Northern Nigeria. Niger J Med. 2005;14:425–8. [PubMed] [Google Scholar]
- 19.Ejele OA, Ojule AC. Hepatitis B antigenaemia (HBsAg): Risk of occupational exposure in a chemical pathology laboratory in Nigeria. Niger J Clin Pract. 2003;6:99–101. [Google Scholar]
- 20.Abdulkareem FB, Banjo AA, Elesha SO, Daramola AO. Histopathological study of liver diseases at the Lagos University teaching hospital, Nigeria (1989-2000) Niger Postgrad Med J. 2006;13:41–6. [PubMed] [Google Scholar]
- 21.Baba MM, Ajayi BB, Ekanem LA. Prevalence of hepatitis B surface antigen among patients suspected of liver diseases in a Nigerian hospital. Niger Postgrad Med J. 2000;7:91–5. [PubMed] [Google Scholar]
- 22.Lesi OA, Kehinde MO, Anomneze EE. Chronic liver disease in Lagos: A clinicopathological study. Niger Postgrad Med J. 2004;11:91–6. [PubMed] [Google Scholar]
- 23.Ola SO, Otagbeyo JA, Odaibo GN, Olaleye OD, Olubuyide OL. Serum hepatitis C virus and hepatitis B surface antigenaemia in Nigerian patients with acute icteric hepatitis. West Afr J Med. 2002;21:215–7. doi: 10.4314/wajm.v21i3.28033. [DOI] [PubMed] [Google Scholar]
- 24.Hoofnagle JH. Hepatitis B-preventable and now treatable. N Engl J Med. 2006;354:1074–6. doi: 10.1056/NEJMe058309. [DOI] [PubMed] [Google Scholar]
- 25.Okey A. Faculty of Business Administration. Enugu campus: University of Nigeria; 1994. Epidemiological Research: A Practical approach for the Medical and Nursing Sciences; pp. 57–65. [Google Scholar]
- 26.Araoye MO. Research Methodology with Statistics for Health and Social Sciences. Ilorin: Nathadex Publishers; 2004. Sample size determination; pp. 115–21. [Google Scholar]
- 27.Omoigberale AI, Airauhi LU. Aspects of the epidemiology of intestinal parasitoses (IP) in children: Knowledge, practices and perceptions of mothers. Niger J Clin Pract. 2006;9:109–13. [PubMed] [Google Scholar]
- 28.Dienstag JL, Isselbacker KJ. Viral hepatitis. In: Braunwald E, Fauci AS, editors. Harrison's Principle of Internal Medicine. 16th ed. New York: W.B. Saunders Company; 2005. pp. 1808–40. [Google Scholar]
- 29.Sherlock S, Dooley J. Oxford: Blackwell Publishers; 2002. Diseases of the Liver and Biliary System; p. 294. [Google Scholar]
- 30.Ola SO, Jaiyesimi AE, Olusanya OO. Co-infection of human immunodeficiency virus and hepatitis B virus among Nigerian patients and blood donors at Sagamu. Niger Med J. 2005;46:64–7. [Google Scholar]
- 31.Hyams KC. Risk of chronicity following acute hepatitis B virus infection: A review. Clin Infect Dis. 1995;20:992–1000. doi: 10.1093/clinids/20.4.992. [DOI] [PubMed] [Google Scholar]


