Abstract
Major mental disorders such as schizophrenia and affective disorders are highly disabling illnesses. The cultural factors that influence the diagnosis and treatment of these disorders are of paramount clinical significance. We attempted to critically review the cultural factors in relation to the epidemiology, phenomenology, treatment, and outcome of major mental disorders from an Indian perspective, and tried to compare these with the cultural factors identified in major international studies. The clinical expression of major mental disorders was noted to vary across cultures in the review. In addition, the outcome of major mental disorders is reported to be better in developing nations than in the developed countries. Transcultural variations are also noted to exist in pharmacokinetics, pharmacodynamics, traditional healing practices, and psychotherapeutic approaches. The role of cultural factors in severe mental illnesses needs adequate attention from mental health professionals. Continued research on the cultural aspects is required to understand the interplay of all social, cultural, and biological factors. It is important to consider other cultural, traditional, and folk methods for understanding and management of mental illnesses.
Keywords: Bipolar, culture, schizophrenia
CULTURE AND MAJOR MENTAL DISORDERS
The phenomenology of major mental disorders (schizophrenia and affective disorders) is recognized in all parts of the world. It was previously assumed that culture merely plays a patho-plastic effect on the strong central biological pathogenesis of these disorders.[1] However, current understanding is that culture has multiple roles to play in the expressions of psychopathology. These are as follows:[2]
Pathogenic effects – Culture is a direct causative factor in forming or generating illness
Patho-selective effects – Tendency to select culturally influenced reaction patterns that result in psychopathology
Patho-plastic effect – Culture contributes to modeling or shaping of symptoms
Patho-elaborating effects – Behavioral reactions become exaggerated through cultural reinforcements
Patho-facilitative effects – Cultural factors contribute to frequent occurrence
Patho-reactive effects – Culture influences perception and reaction.
Culture influences the epidemiology, phenomenology, outcome, and treatment of schizophrenia and affective disorders. We review the effects of culture in each of these parameters.
CULTURAL INFLUENCE ON EPIDEMIOLOGY
Schizophrenia
Prevalence
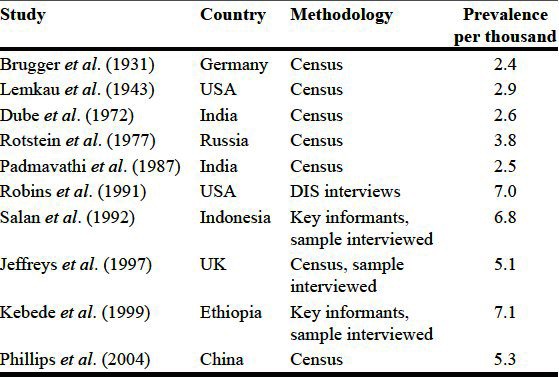
A large number of studies [Table 1] have estimated the prevalence of schizophrenia. Although there are methodological differences, most have found a point prevalence of between 1.5 and 7 per thousand populations at risk. There were pockets of high (e.g., Ireland) and low (e.g., New Guinea) prevalence. Much of the evidence points toward equal prevalence in Asia and the West, although inconclusive. A meta-analysis of 188 studies from 46 countries calculated median lifetime prevalence as 4.0 (1.6-12.1).[3] The prevalence of schizophrenia in “least developed” countries was significantly lower than in the “emerging” and “developed” countries. Indian studies have suggested that the prevalence of schizophrenia is lower in India than in the West.[4] One reason for this difference could be underreporting.[5]
Table 1.
Prevalence studies of schizophrenia
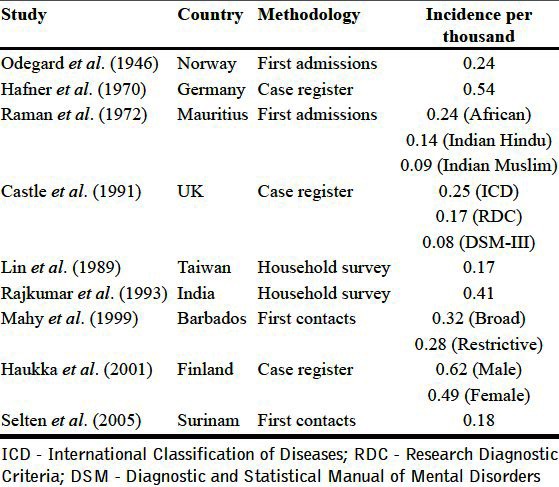
Incidence
The incidence of schizophrenia is comparable across cultures. There are differences based on whether a “narrow” or “broad” definition of schizophrenia is used [Table 2]. Studies that have used broad definition (International Classification of Diseases (ICD)-8, ICD-9) have found incidence rates between 0.17 and 0.54 per thousand populations, whereas studies that have used narrow criteria (ICD-10, Diagnostic and Statistical manual of Mental disorders (DSM)-III) have found incidence rates to be much lower. The WHO 10 country study (DOSMED-Determinants of Outcome of Severe Mental Disorders) was a cross-cultural epidemiological study aimed at determining the incidence of schizophrenia in various cultures.[6,7] The incidence rate in the broad diagnostic group was 0.15-0.42 per 1000 and there was significant difference across areas. The rate for “restrictive” diagnostic group was 0.07-0.14 per thousand and the difference across areas was nonsignificant. These results have been replicated in similar studies.[8,9] In another transcultural study, it was found that late-borns were more prone to develop schizophrenia in West, whereas early-borns were more susceptible in India.[10]
Table 2.
Incidence studies of schizophrenia
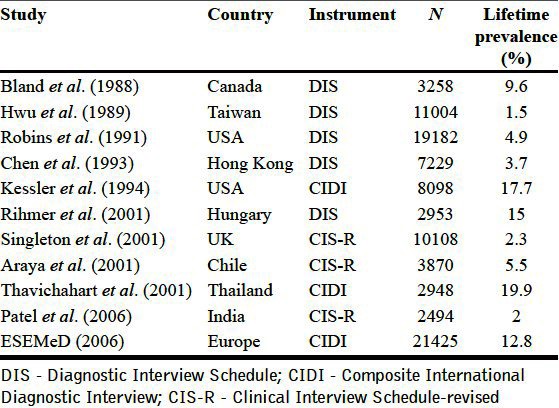
Affective disorders
The WHO collaborative study of mental illness in primary care attendees[11] studied rates of depression in 15 countries. The rates varied greatly from 2.6% to 29.5%. However, this study did not use an unselected community sample. The Diagnostic Interview Schedule (DIS)[12] and the Composite International Diagnostic Interview (CIDI)[13] have been used in large surveys to make case-finding techniques uniform. Using the DIS, 12-month prevalence rates were found to range between 0.8% and 5.8%. European nations had higher rates of depression than the United States (two- to threefold), whereas the rates in East Asian countries were low. Using ICD-10 criteria/Clinical Interview Schedule–Revised (CIS-R), the range was 1.7-5.5%. Lower rates were found in the Goan community survey and higher rates were found in Chile. Also, the prevalence rates were particularly low in African countries. A list of studies using DIS/CIDI/CIS-R is given in Table 3. The prevalence of affective disorders has been found to be lower in most Indian studies than the West.[4]
Table 3.
Prevalence studies of depressive disorder
CULTURAL INFLUENCE ON PHENOMENOLOGY
Schizophrenia
Subtypes
The first systematic examination of schizophrenia subtypes[14] found that catatonic subtype was rare in the West, hebephrenic subtype was common in Japan, and simple subtype was common in Asia. The International Pilot Study of Schizophrenia (IPSS) sheds more light on this issue.[15] Paranoid schizophrenia was the commonest subtype (40%). The hebephrenic subtype (11%) was more prevalent in Cali and Taipei, whereas the catatonic subtype (11%) was more in developing countries (Agra, Cali, and Ibadan). Another transcultural study, International Study on Psychotic Symptoms (ISPS) found the catatonic subtypes to be equally prevalent in all sites; this may be due to the use of DSM-IV criteria for examining catatonic schizophrenia.[16,17]
Symptoms
Delusions: Themes of delusions have been found to be related to patients' social background, cultural beliefs, and expectations.[18] Religious delusions are common in Christian societies, whereas these are rarer in Hindu, Muslim, or Buddhist societies.[18,19] Magical religious delusions have also been found to be greater in rural societies, especially in women >30 years of age.[18] Low rates of religious delusions, grandiose delusions, and delusions of guilt were found in Pakistan, the only pure Islamic country in the study.[20] In contrast, religious grandiosity was more common in African countries. The cultural content of the delusions recurs in future episodes of psychosis.[21]
Hallucinations: The first large-scale cross-cultural evaluation of hallucinations[22] found that visual hallucinations were more common in Africa. Another study found higher occurrence of auditory and visual hallucinations in non-European patients than in European patients.[23] The ISPS showed that auditory hallucinations were commonest in all cultures and that visual hallucinations were the commonest in Africa and the rarest in Pakistan. The cultural content of hallucinations also recurs in future psychotic episodes.[24]
First rank symptoms (FRS): Indian studies have found FRS to be generally culture free.[5] However, there is a lower occurrence of FRS in non-Western countries. FRS were present in 35% in India,[25] 25% in Sri Lanka,[26] and 27% in Malaysia.[27] In contrast, a study from Nigeria reported 60.3% FRS.[28] In the ISPS, Nigeria and Ghana had higher frequency of FRS than the other developing countries.
Other symptoms: Negative symptoms and neuropsychological deficits are common in most cultures. There are differences in the frequency of types of negative symptoms between patients in India and the United States.[29] Symptoms in schizophrenia such as not eating, not sleeping, and negative symptoms were reported to be more distressing in Indian patients, compared to aggression and positive symptoms among those from UK.[30]
Reasons for cultural differences in psychopathology: Cross-cultural differences in language and thought result in cross-cultural differences in symptoms and subtypes.[31] Greater linguistic competence leads to more elaborate, systematized delusions, and poorer prognosis. Low linguistic competence prevents delusional elaboration and manifests catatonia. Cultural defenses and modal personalities also play a role in the differential expression of psychopathology.
Affective disorders
Culture greatly influences the way in which depressive symptoms are expressed. In the WHO collaborative study on standardized assessment of depressive disorder,[32] 583 patients in five centers (Basel, Montreal, Tehran, Nagasaki, and Tokyo) were assessed for core depressive symptoms. Most of them had in common features of sadness, anhedonia, lack of interest and energy, impaired concentration, and ideas of worthlessness. Feelings of guilt and suicidal ideations were least common in Tehran. Indian studies have also found guilt to be less common among Indian patients than those in the West;[33,34] in addition, they reported guilt of an impersonal nature: The present suffering is attributed to possible bad deeds of previous life (consequence of “Karma”) rather than due to self-failure as in the West.[5,35] Studies in India have reported physical symptoms to be common presenting symptoms in depression.[36,37] A comparison of depression in Western and non-Western societies noted that disorders of conduct and somatic complaints were more common in non-Western cultures.[38]
There have not been many comparisons of the phenomenology of mania between cultures. Indian bipolar patients have preponderance of mania in contrast to patients in Western countries.[39] Indian studies have found higher prevalence of grandiose delusions, delusions of persecution and reference, and those related to sexual and religious themes than in the West.[40] Hostile irritability is the predominant affect in Indian manic subjects.[41] There are reports of seasonal occurrence of mania in summer season, which is not reported in the west.[40,42] Recurrent unipolar mania is commoner in India and tropical countries than in temperate western countries.[42]
CULTURAL INFLUENCES ON OUTCOME
Schizophrenia
The IPSS was a landmark study which identified differences in the course and outcome of schizophrenia between cultures.[7,43–45] This study evaluated 1202 patients from nine countries. At 5-year follow-up, a more favorable outcome was observed in developing countries in comparison with that in developed countries. India and Nigeria had the highest percentage with best outcome (66%) and the lowest percentage with worst outcome (10%), respectively. The major limitation of the study was that the sample was not an epidemiological sample. To circumvent this limitation, the DOSMED study[46] used an epidemiological sample from 12 centers in 10 countries and recruited 1379 subjects in 2 years. As observed in IPSS, there was favorable outcome in developing countries in comparison with that in developed countries. The Madras longitudinal study[47,48] and the study of factors associated with course and outcome of schizophrenia (SOFACOS)[49] again demonstrated that two-thirds of schizophrenia patients in India have partial to full remission of symptoms. However, cognitive function, quality of life, and effect of medication have not been extensively researched in studies from these countries.[50]
Affective disorders
The outcome of affective disorders has been found to be favorable in India than in developed countries. In a 4-year follow-up of first-episode manic patients from Ranchi,[51] 40% of the patients did not have any recurrences and 25% had one recurrence. In the Chandigarh acute psychosis study,[52,53] 17 depressive and 21 manic subjects were followed up for 1 year. Three-fourths of the subjects had no symptoms or social impairment at the end of follow-up. In a follow-up study of 92 depressed patients for 5-10 years, it was found that 36% of the subjects had no recurrence of symptoms.[36]
CULTURAL INFLUENCES ON TREATMENT
Pharmacotherapy
Various cultural differences exist in the way drugs are prescribed, the way they are metabolized and excreted, and the way individuals respond to medications. Many of these variations are secondary to genetic mechanisms. In addition, nongenetic factors such as medication acceptance and adherence, drug availability and affordability, and explanatory models about illness also play an important role.[54]
Pharmacokinetics
Every drug taken by a person needs to be absorbed, metabolized, distributed, and excreted. It is the process of metabolism which usually leads to variations between individuals of different backgrounds.[55]
Cytochrome p450 (CYP) enzymes are the most important enzymes for drug metabolism. CYP2C9, CYP2C19, and CYP2D6 account for nearly 40% of human hepatic metabolism phase I. CYP2D6 metabolizes many psychotropic medications, including antidepressants and antipsychotics. Based on how the drugs are metabolized, there are ultra-rapid metabolizers (UM), extensive metabolizers (EM), intermediate metabolizers (IM), and poor metabolizers (PM).[56] These variations are secondary to allelic variations of the CYP2D6 gene.[57] The frequencies of variant alleles differ among ethnic groups. The frequency of PM is much higher in the Asian population than in the Caucasian or African population.[58] Slower drug metabolism leads to poorer drug response and more adverse effects.[59] Nongenetic factors which affect CYP450 enzymes include smoking and diet. For example, a diet rich in cabbage and broccoli can increase the activity of CYP1A2 enzyme.
Pharmacodynamics
Pharmacodynamic mechanisms include transporters, receptors, and key enzymes in neurotransmitter biosynthesis and catabolism. Genetic polymorphisms involving these mechanisms can lead to alterations in drug responses between ethno-cultural groups. For example, Asian subjects with schizophrenia require lower haloperidol dosages and lower plasma concentration for drug responses than Caucasians, possibly mediated by dopamine receptor-related mechanisms;[55,60] they also develop side effects on low doses.[54]
Differences in clinical practice
Physical treatments are used more often used in India and other developing countries (e.g., Electroconvulsive therapy). The roles of family members are very different transculturally. They play a more significant role in treatment in an Indian setting. Communicating with patients and families regarding diagnosis, illness, and care is an art that needs to be attuned to individual cultural frameworks. Follow-up rates were poorer in those whose sociocultural beliefs were contradicted.[61] In addition, the nature of expressed emotions and life events differ between cultures.
Coping with severe mental illnesses
Indian patients with schizophrenia used less number of coping strategies compared to German patients. Indian patients endorsed strategies of avoidance, relaxation, and meditation, and waited for situation to change. German patients sought medical help, counseling and problem solving.[10] The degree of perceived stress was lower among Indian patients, possibly due to better family support.
Stigma associated with severe mental illness
Rural Indians had higher stigma scores and deployed punitive measures to deal with severe mental illness (SMI). Urban Indians and not rural Indians showed more discrimination to work with SMI.[62] Urban Indians hid their illness and illness history; rural Indians felt ridicule, shame, and discrimination.[63]
Traditional healing practices
Motivational factors to follow traditional healing practices include cultural faith, inadequate recovery with allopathic treatment, economic factors, social stigma, and easy approachability.[64] Various diagnoses (e.g., pher, kartab, shaitani aid, jadu tona, and stars positioning) and treatment methods (e.g., tabiz, jhaad, phook, chirag, and jap) have been documented, but treatment effectiveness rates have not been mentioned. It is important to understand the concepts, classification, and management of other health systems to have effective liaisons with them. Concomitant use of traditional therapies may enhance the acceptance and adherence of modern treatments.
Psychotherapy
Cultural values are important to determine psychotherapeutic needs and interventions. There are cross-cultural differences in personality configurations which have to be taken into account. The Western-model psychotherapy in its usual form may not be suited for a diverse culture like India.
In addition to these modifications in Western psychotherapy, indigenous models of psychotherapy may be needed. For example, the guru–chela relationship might be a particularly useful paradigm in India.
Some proposed modifications to suit the need of Indian patients are as follows:
Use of religion or spirituality – Religious beliefs can be used for the benefit of the patient if used carefully
Family involvement – Unlike in the West, many Indian subjects might want active family involvement. The need for confidentiality may not be as high
Lower emphasis on individual responsibility and autonomy – Indian culture fosters dependence and dependability
Superior class of the therapist and paternalistic approach – In Indian societies, the doctor is considered superior and the patient becomes submissive. This may be used for patients' benefit[54]
Greater active participation by the therapist – Unlike the Western-style therapist, the Indian therapist has to be more active and direct suggestions might be particularly useful
Single session therapy may be useful for the poor and underprivileged.[65]
CONCLUSIONS
The role of cultural factors in SMI needs adequate attention from mental health professionals. Cultural sensitivity and competence in assessment, and management are as important as other aspects. Continued research on cultural aspects along with biological aspects is required to understand the interplay of all factors. The use of cultural factors in a positive way will improve coping with symptoms and illness, as well as recovery. It is also important to consider other cultural, traditional, and folk methods for understanding and management of mental illnesses.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Yap PM. Comparative Psychiatry: A Theoretical Framework. In: Lau MP, Stokes AB, editors. Toronto: University of Toronto; 1974. pp. 45–46. [Google Scholar]
- 2.Tseng W. Handbook of Cultural Psychiatry. San Diego, CA, USA: Academic Press; 2001. Culture and Psychopathology; pp. 175–433. [Google Scholar]
- 3.Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Math SB, Chandrashekar CR, Bhugra D. Psychiatric epidemiology in India. Indian J Med Res. 2007;126:183–92. [PubMed] [Google Scholar]
- 5.Avasthi A. Indianizing psychiatry – Is there a case enough? Indian J Psychiatry. 2012;53:111–20. doi: 10.4103/0019-5545.82534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, et al. Schizophrenia: Manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl. 1992;20:1–97. doi: 10.1017/s0264180100000904. [DOI] [PubMed] [Google Scholar]
- 7.Sartorius N, Jablensky A, Korten A, Ernberg G, Anker M, Cooper JE, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. A preliminary report on the initial evaluation phase of the WHO collaborative study on determinants of outcome of severe mental disorders. Psychol Med. 1986;16:909–28. doi: 10.1017/s0033291700011910. [DOI] [PubMed] [Google Scholar]
- 8.McNaught AS, Jeffreys SE, Harvey CA, Quayle AS, King MB, Bird AS. The Hampstead Schizophrenia Survey 1991.II: Incidence and migration in inner London. Br J Psychiatry. 1997;170:307–11. doi: 10.1192/bjp.170.4.307. [DOI] [PubMed] [Google Scholar]
- 9.Rajkumar S, Padmavathy R, Thara R. Incidence of schizophrenia in an urban community in Madras. Indian J Psychiatry. 1993;35:18–21. [PMC free article] [PubMed] [Google Scholar]
- 10.Kulhara P, Shah R, Aarya KR. An overview of Indian research in schizophrenia. Indian J Psychiatry. 2010;52:S159–72. doi: 10.4103/0019-5545.69229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ustun TB, Sartorius N. Chichester: Wiley; 1995. Mental Illness in General Health Care: An International Study; pp. 79–98. [Google Scholar]
- 12.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–9. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 13.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The composite international diagnostic interview. An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 14.Murphy HB. Comparative psychiatry. The international and intercultural distribution of mental illness. Monogr Gesamtgeb Psychiatr Psychiatry Ser. 1982;28:1–327. [PubMed] [Google Scholar]
- 15.Geneva: World Health Organization; 1973. WHO. Report of the International Pilot Study of Schizophrenia; pp. 386–397. [Google Scholar]
- 16.Stompe T, Ortwein-Swoboda G, Ritter K, Marquart B, Schanda H. The impact of diagnostic criteria on the prevalence of schizophrenic subtypes. Compr Psychiatry. 2005;46:433–9. doi: 10.1016/j.comppsych.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Stompe T, Ortwein-Swoboda G, Ritter K, Schanda H, Friedmann A. Are we witnessing the disappearance of catatonic schizophrenia? Compr Psychiatry. 2002;43:167–74. doi: 10.1053/comp.2002.32352. [DOI] [PubMed] [Google Scholar]
- 18.Kala AK, Wig NN. Delusion across cultures. Int J Soc Psychiatry. 1982;28:185–93. doi: 10.1177/002076408202800304. [DOI] [PubMed] [Google Scholar]
- 19.Tateyama M, Asai M, Hashimoto M, Bartels M, Kasper S. Transcultural study of schizophrenic delusions. Tokyo versus Vienna and Tübingen (Germany) Psychopathology. 1998;31:59–68. doi: 10.1159/000029025. [DOI] [PubMed] [Google Scholar]
- 20.Stompe T, Bauer S, Ortwein-Swoboda G. Delusions of guilt: The attitude of Christian and Islamic confessions towards Good and Evil and the responsibility of men. J Muslim Ment Health. 2006;1:43–56. [Google Scholar]
- 21.Sinha VK, Chaturvedi SK. Consistency of delusions in schizophrenia and affective disorder. Schizophr Res. 1990;3:347–50. doi: 10.1016/0920-9964(90)90020-8. [DOI] [PubMed] [Google Scholar]
- 22.Murphy HB, Wittkower ED, Fried J, Ellenberger H. A cross-cultural survey of schizophrenic symptomatology. Int J Soc Psychiatry. 1963;9:237–49. doi: 10.1177/002076406300900401. [DOI] [PubMed] [Google Scholar]
- 23.Ndetei DM, Vadher A. A comparative cross-cultural study of the frequencies of hallucination in schizophrenia. Acta Psychiatr Scand. 1984;70:545–9. doi: 10.1111/j.1600-0447.1984.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 24.Chaturvedi SK, Sinha VK. Recurrence of hallucinations in consecutive episodes of schizophrenia and affective disorder. Schizophr Res. 1990;3:103–6. doi: 10.1016/0920-9964(90)90042-6. [DOI] [PubMed] [Google Scholar]
- 25.Radhakrishnan J, Mathew K, Richard J, Verghese A. Schneider's first rank symptoms – Prevalence, diagnostic use and prognostic implications. Br J Psychiatry. 1983;142:557–9. doi: 10.1192/bjp.142.6.557. [DOI] [PubMed] [Google Scholar]
- 26.Pela OA. Cultural relativety of first rank symptoms in schizophrenia. Int J Soc Psychiatry. 1982;28:91–5. doi: 10.1177/002076408202800202. [DOI] [PubMed] [Google Scholar]
- 27.Salleh MR. Specificity of Schneider's first rank symptoms for schizophrenia in Malay patients. Psychopathology. 1992;25:199–203. doi: 10.1159/000284772. [DOI] [PubMed] [Google Scholar]
- 28.Gureje O, Bamgboye EA. A study of Schneider's first-rank symptoms of schizophrenia in Nigerian patients. Br J Psychiatry. 1987;150:867–9. doi: 10.1192/bjp.150.6.867. [DOI] [PubMed] [Google Scholar]
- 29.Chaturvedi SK. Negative symptoms in schizophrenia: Cross-cultural differences. Indian J Psychiatry. 1986;2:59–65. [Google Scholar]
- 30.Gopinath PS, Chaturvedi SK. Distressing behaviour of schizophrenics at home. Acta Psychiatr Scand. 1992;86:185–8. doi: 10.1111/j.1600-0447.1992.tb03249.x. [DOI] [PubMed] [Google Scholar]
- 31.Varma VK. Present status of psychotherapy in India. Indian J Psychiatry. 1982;24:209–26. [PMC free article] [PubMed] [Google Scholar]
- 32.Geneva: World Health Organization; 1983. WHO. Depressive Disorders in Different Cultures; pp. 120–131. [Google Scholar]
- 33.Sethi BB, Dube S. Guilt in India (social, cultural and psychological perspectives) Indian J Psychiatry. 1982;24:101–6. [PMC free article] [PubMed] [Google Scholar]
- 34.Venkoba Rao A. Depression – A psychiatric analysis of 30 cases. Indian J Psychiatry. 1966;8:143–54. [Google Scholar]
- 35.Ananth J, Engelsman F, Ghadirian AM, Wohl M, Shamasundara P, Narayanan HS. Depression and guilt in Indian and north American patients: A comparative study. Indian J Psychiatry. 1993;35:36–9. [PMC free article] [PubMed] [Google Scholar]
- 36.Gada M. The course of depressive illness: A follow-up investigation of 92 cases. Indian J Psychiatry. 1989;31:196–200. [PMC free article] [PubMed] [Google Scholar]
- 37.Teja JS, Narang RL, Agarwal AK. Depression across cultures. Br J Psychiatry. 1971;119:253–60. doi: 10.1192/bjp.119.550.253. [DOI] [PubMed] [Google Scholar]
- 38.Aichberger MC, Schouler-Ocak M, Rapp MA, Heinz A. Transcultural aspects of depression. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2008;51:436–42. doi: 10.1007/s00103-008-0512-y. [DOI] [PubMed] [Google Scholar]
- 39.Chopra MP, Kishore Kumar KV, Subbakrishna DK, Jain S, Murthy RS. The course of bipolar disorder in rural India. Indian J Psychiatry. 2006;48:254–7. doi: 10.4103/0019-5545.31559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sethi S, Khanna R. Phenomenology of mania in eastern India. Psychopathology. 1993;26:274–8. doi: 10.1159/000284833. [DOI] [PubMed] [Google Scholar]
- 41.Chatterjee S, Kulhara P. Symptomatology, symptom resolution and short term course in mania. Indian J Psychiatry. 1989;31:213–8. [PMC free article] [PubMed] [Google Scholar]
- 42.Avashthi A, Sharma A, Gupta N, Kulhara P, Varma VK. Seasonality and unipolar recurrent mania: Preliminary findings from a retrospective study. Indian J Psychiatry. 1996;38:236–9. [PMC free article] [PubMed] [Google Scholar]
- 43.Jablensky A. Multicultural studies and the nature schizophrenia: A review. J R Soc Med. 1987;80:162–7. doi: 10.1177/014107688708000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jablensky A. Epidemiology of schizophrenia: The global burden of disease and disability. Eur Arch Psychiatry Clin Neurosci. 2000;250:274–85. doi: 10.1007/s004060070002. [DOI] [PubMed] [Google Scholar]
- 45.Leff J, Sartorius N, Jablensky A, Korten A, Ernberg G. The international pilot study of schizophrenia: Five-year follow-up findings. Psychol Med. 1992;22:131–45. doi: 10.1017/s0033291700032797. [DOI] [PubMed] [Google Scholar]
- 46.Edgerton RB, Cohen A. Culture and schizophrenia: The DOSMD challenge. Br J Psychiatry. 1994;164:222–31. doi: 10.1192/bjp.164.2.222. [DOI] [PubMed] [Google Scholar]
- 47.Thara R. Twenty-year course of schizophrenia: The Madras longitudinal study. Can J Psychiatry. 2004;49:564–9. doi: 10.1177/070674370404900808. [DOI] [PubMed] [Google Scholar]
- 48.Thara R, Henrietta M, Joseph A, Rajkumar S, Eaton WW. Ten-year course of schizophrenia – The Madras longitudinal study. Acta Psychiatr Scand. 1994;90:329–36. doi: 10.1111/j.1600-0447.1994.tb01602.x. [DOI] [PubMed] [Google Scholar]
- 49.Verghese A, John JK, Rajkumar S, Richard J, Sethi BB, Trivedi JK. Factors associated with the course and outcome of schizophrenia in India. Results of a two-year multicentre follow-up study. Br J Psychiatry. 1989;154:499–503. doi: 10.1192/bjp.154.4.499. [DOI] [PubMed] [Google Scholar]
- 50.Isaac M, Chand P, Murthy P. Schizophrenia outcome measures in the wider international community. Br J Psychiatry Suppl. 2007;50:s71–7. doi: 10.1192/bjp.191.50.s71. [DOI] [PubMed] [Google Scholar]
- 51.Khess CR, Das J, Akhtar S. Four year follow-up of first episode manic patients. Indian J Psychiatry. 1997;39:160–5. [PMC free article] [PubMed] [Google Scholar]
- 52.Susser E, Fennig S, Jandorf L, Amador X, Bromet E. Epidemiology, diagnosis, and course of brief psychoses. Am J Psychiatry. 1995;152:1743–8. doi: 10.1176/ajp.152.12.1743. [DOI] [PubMed] [Google Scholar]
- 53.Susser E, Varma VK, Malhotra S, Conover S, Amador XF. Delineation of acute and transient psychotic disorders in a developing country setting. Br J Psychiatry. 1995;167:216–9. doi: 10.1192/bjp.167.2.216. [DOI] [PubMed] [Google Scholar]
- 54.Kuruvilla A, Kuruvilla K. Incidence of adverse reactions to commonly prescribed psychopharmacological agents during early phase of therapy. Indian J Psychiatry. 1995;37:113–8. [PMC free article] [PubMed] [Google Scholar]
- 55.Lin KM, Poland RE, Nakasaki G. Psychopharmacology and Psychobiology of Ethnicity. Washington, DC: American Psychiatric Press; 1993. Ethnicity and Psychopharmacology; pp. 59–61. [Google Scholar]
- 56.Kinnear CJ, Niehaus DJ, Moolman-Smook JC, du Toit PL, van Kradenberg J, Weyers JB, et al. Obsessive-compulsive disorder and the promoter region polymorphism (5-HTTLPR) in the serotonin transporter gene (SLC6A4): A negative association study in the Afrikaner population. Int J Neuropsychopharmacol. 2000;3:327–31. doi: 10.1017/S1461145700002054. [DOI] [PubMed] [Google Scholar]
- 57.Aitchison KJ, Jordan BD, Sharma T. The relevance of ethnic influences on pharmacogenetics to the treatment of psychosis. Drug Metabol Drug Interact. 2000;16:15–38. doi: 10.1515/dmdi.2000.16.1.15. [DOI] [PubMed] [Google Scholar]
- 58.Yokota H, Tamura S, Furuya H, Kimura S, Watanabe M, Kanazawa I, et al. Evidence for a new variant CYP2D6 allele CYP2D6J in a Japanese population associated with lower in vivo rates of sparteine metabolism. Pharmacogenetics. 1993;3:256–63. doi: 10.1097/00008571-199310000-00005. [DOI] [PubMed] [Google Scholar]
- 59.Chou WH, Yan FX, de Leon J, Barnhill J, Rogers T, Cronin M, et al. Extension of a pilot study: Impact from the cytochrome P450 2D6 polymorphism on outcome and costs associated with severe mental illness. J Clin Psychopharmacol. 2000;20:246–51. doi: 10.1097/00004714-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 60.Lin KM, Poland RE, Nuccio I, Matsuda K, Hathuc N, Su TP, et al. A longitudinal assessment of haloperidol doses and serum concentrations in Asian and Caucasian schizophrenic patients. Am J Psychiatry. 1989;146:1307–11. doi: 10.1176/ajp.146.10.1307. [DOI] [PubMed] [Google Scholar]
- 61.Pandey RS, Sreenivas KN, Muralidhar D. Sociocultural beliefs and treatment acceptance. Indian J Psychiatry. 1980;22:161–6. [PMC free article] [PubMed] [Google Scholar]
- 62.Jadhav S, Littlewood R, Ryder AG, Chakraborty A, Jain S, Barua M. Stigmatization of severe mental illness in India: Against the simple industrialization hypothesis. Indian J Psychiatry. 2007;49:189–94. doi: 10.4103/0019-5545.37320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Loganathan S, Murthy SR. Experiences of stigma and discrimination endured by people suffering from schizophrenia. Indian J Psychiatry. 2008;50:39–46. doi: 10.4103/0019-5545.39758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sethi BB, Manchanda R. Socio-economic and cultural correlates of psychiatric disorders with special reference to India. Indian J Psychiatry. 1978;20:199–211. [Google Scholar]
- 65.Hoch EM. Experiences with psychotherapy training in India. Psychother Psychosom. 1990;53:14–20. doi: 10.1159/000288334. [DOI] [PubMed] [Google Scholar]


