Abstract
Background:
Compassion fatigue is a broad term comprising of two components – burnout and secondary traumatic stress. The current study is aimed at identifying ‘burnout’ and ‘compassion fatigue’ among clinicians involved in care of individuals suffering from medical illness.
Materials and Methods:
A total of 60 clinicians were included in the study. A semi-structured questionnaire was administered to gather information related to personal, professional, anthropometric, and metabolic profile of the study participants. Professional Quality of Life Scale (ProQoL Version V) was used to assess burnout, compassion satisfaction and secondary traumatic stress. Analysis was carried out using the SPSS version 19.0.
Results:
The mean age of clinicians was 46.68±11.06 (range 26-67 years). Burnout score was significantly higher in those involved in diabetology practice. Similarly, compassion satisfaction score was greater among those with greater years of practice as well as among those in private practice. Clinicians who reported a poor working condition, as opposed to good, had more burnout and less compassion satisfaction.
Conclusion:
The current study suggests that it is important to find out ways of decreasing burnout and compassion fatigue among clinicians.
Keywords: Burnout, clinicians, compassion fatigue
INTRODUCTION
Compassion fatigue is a broad term comprising of two components – burnout and secondary traumatic stress. The symptoms of this condition are normal displays of chronic stress. In physicians these result from a strong identification with time demanding, helpless, suffering, or traumatized people.[1]
Compassion satisfaction, a related concept, is about the pleasure a clinician derives from being able to do his work well. For example, clinician may feel it be a pleasure to treat patients through his skills. He may feel positive about his colleagues or his ability to contribute to the work setting or even the greater good of society.
A term with related connotations is burnout (BO). It is defined as feeling of hopelessness and difficulties in dealing with work or in carrying out one's job effectively. These negative feelings usually have a gradual onset. They can stem from the feeling that one's efforts make no difference, or they can be associated with a very high workload or a non-supportive work environment.[2]
The second component of compassion fatigue (CF) is secondary traumatic stress (STS). It is work related, secondary exposure to extremely or traumatically stressful events. Developing problems due to exposure to other's trauma is somewhat rare but does happen to many people who care for those who have experienced extreme or traumatically stressful events. The symptoms of STS are usually rapid in onset and associated with a particular event.[2] Up to one third of practicing clinicians could be expected to be suffering from burn out if assessed cross-sectionally.[3] More importantly there has been an increasing trend in the emotional exhaustion of clinicians over the years.[4]
The issue assumes a greater significance in context of clinicians involved in care of individuals diagnosed with medical illness. Although it is expected in clinicians play host to a high level of compassion fatigue, the issues remain relatively under researched.
The research in western settings has clearly established the adverse impact of clinician stress, fatigue, and burnout on quality of patient care.[5–7] Additionally, this could lead to negative affective state among clinicians and is associated with feelings of alienation, helplessness and hopelessness, loss of idealism and spirit, and physical and emotional drain anxiety, and depressive disorders in them.[8,9]
However, there is paucity of literature in this area, especially in the Indian setting. The current study aimed at identifying ‘burnout’ and ‘compassion fatigue’ among clinicians involved in care of individuals suffering from medical illness. A cohort of surgeons and physicians engaged in patient care were studied for this purpose.
MATERIALS AND METHODS
The study was carried out among clinicians practicing at a district headquarter (Karnal) in Haryana, India, working in different clinical settings. The study participants were assessed for compassion satisfaction, burnout and secondary traumatic stress.
A total of 60 clinicians gave an informed verbal consent to participate in the study. The study cohort included 35 medical (medicine, pediatrics, skin, and radiology) and 25 surgical (Obstetrics and Gynecology, General Surgery, Orthopedics, and Otorhinolaryngology) specialty practitioners.
A semi-structured questionnaire was administered to gather information related to personal, professional, anthropometric, and metabolic profile of the study participants. The personal domain included information about marital status, alcohol consumption, and smoking. Professional domain included information about type of practice, duration of practice, working hours, working conditions, emergencies, chronic care patients, elderly patients, and financial constraints. The anthropometric parameters assessed were height, weight, body mass index (BMI), waist circumference (WC), hip circumference (HC), waist hip ratio (WHR), and WC to height ratio and metabolic parameters recorded were fasting blood glucose, HBA1c, lipid profile, and blood pressure. Professional Quality of Life Scale (ProQoL Version V) - a validated, pre-tested, and structured 30 point questionnaire to assess burnout, compassion satisfaction and secondary traumatic stress - was also used for assessment.[10] An individual with compassion satisfaction score below 40 and a burnout score above 57 was considered to have compassion fatigue.
Anthropometric measurements
Each study participant was examined for height, weight, WC, and hip circumference without footwear with minimal clothing as per cardiovascular survey methods.[4] BMI was calculated by formula of weight in kg/height m2. WHR was calculated by WC/HC in centimeters. WHtR was calculated by WC/height in centimeters. Value of BMI greater than or equal to 23 kg/m2 was used to define overweight and greater than or equal to 25 kg/m2 was used to define obese. Value of waist circumference >90 cm in men and >80 cm in women was defined as abnormal.[11]
Metabolic measurements
Parameters of fasting blood glucose, glycated hemoglobin, triglycerides, total cholesterol, and HDL cholesterol were taken from last routine laboratory blood report available with the clinician. Blood pressure was measured in respective OPDs using a standard mercury sphygmomanometer under standard conditions as mentioned in cardiovascular survey methods.[12]
Diabetes mellitus (DM) was labeled if a subject was a known diabetic or on treatment with any OGLD or if FBG ≥126 mg/dl.[13] Dyslipidemia was defined according to NCEP ATP III guidelines.[14] Hypertension was labeled if blood pressure ≥140 mmHg systolic blood pressure and ≥90 mmHg diastolic blood pressure or known to be hypertensive on treatment with any blood pressure.[12]
Statistical analysis
Analysis was carried out using the SPSS version 19.0. Pearson's correlation coefficient was calculated to find out the correlations between continuous variables. Independent student's t-test was used for in-between group comparisons. For all the tests performed, results were considered statistically significant for P<0.05.
RESULTS
The study cohort comprised of sixty clinicians. Forty four among them were males (73.3%). The mean age of clinicians was 46.68±11.06 (range 26-67 years).
Fifty eight of the clinicians were married (96.6%), 1 single (1.6%), and 1 widowed (1.6%). The spouses of 50 were working (83.3%) and 9 were non-working (15%). Two had no children (3.33%), 11 had a single child (18.33%), 42 had two (70%), and 4 had three or more (6.66%). Fifty three believed in God (88.3%), four were agnostic (6.66%), while three did not believe in God (5%). Thirty seven preferred vegetarian foods (61.6%), while the rest were non-vegetarian (38.3%); 19 consumed alcohol (31.6%), 2 chewed tobacco (3.33%), and 3 were current smokers (5%).
Forty nine of study participants had a private setup (81.6%) and 11 were working in government setup (18.3%). Also, 35 were practicing medical specialties (58.3%) (Medicine, Pediatrics, Skin, and Radiology) and rest were practicing surgical specialties (41.6%) (Obstetrics and Gynecology, General Surgery, Orthopedics, and Otorhinolaryngology) [Table 1].
Table 1.
Socio.demographic and practice related professional parameters
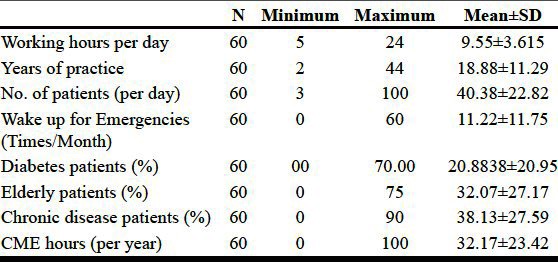
Also, 9 out of 60 had financial constraints (15%), and 48 dealt with their respective hospital paper work (80%).
The anthropometric data, for the clinicians under the study is given in Table 2. The metabolic profile of the clinicians revealed 5 of them having diabetes (8.3%), 12 having hypertension (20%), 19 having dyslipidemia (31.6%), and 2 suffering from heart disease (3.3%). Scores of the study participants on the ProQol Version 5.0 for burnout, compassion satisfaction and secondary traumatic stress score have been provided in Table 3.
Table 2.
Anthropometric parameters of study subjects
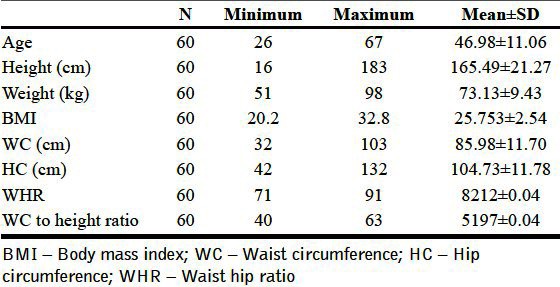
Table 3.
BO/CS/STS values amongst clinicians
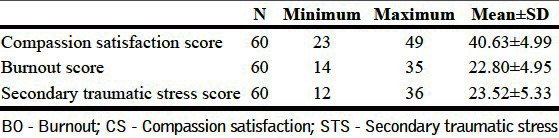
In the professional domain, burnout score was significantly higher in those involved in diabetology practice (t=0.266, P=0.04). Similarly, compassion satisfaction score was greater among those with greater years of practice (t=0.258, P=0.046) as well as among those in private practice (t=0.273, P=0.035) [Table 4]. Therapists who had been into practice for longer duration of time had better satisfaction scores.
Table 4.
Correlates of burnout and compassion satisfaction score
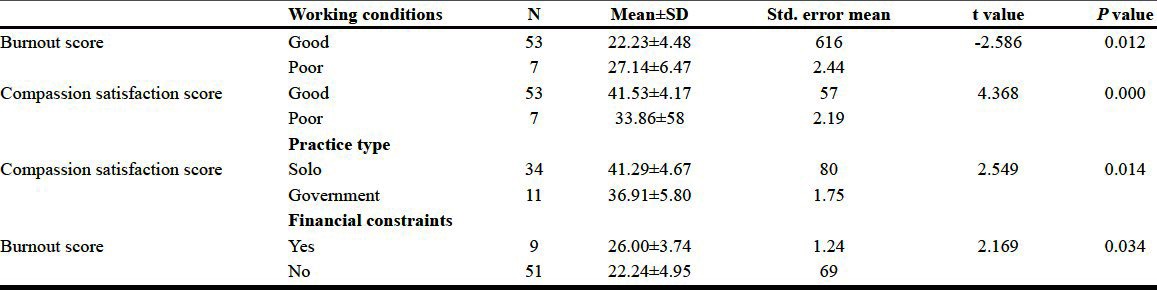
Clinicians who reported a poor working condition, as opposed to good, had more burnout and less compassion satisfaction. Private practitioners as compared to government job had a higher compassion satisfaction score (t=2.549, P=0.014) [Table 4].
On analyzing personal, anthropometric, and metabolic parameters no significant correlation was found with burnout, compassion satisfaction, and secondary traumatic scores. The gender of the clinician also had no significant relation to his/her burnout, compassion satisfaction, and secondary traumatic stress that is the values in male clinicians were fairly comparable to those in female clinicians. The specialty of the clinician, whether medical or surgical, did not significantly affect burnout, and other related parameters. The percentage of elderly patients, and chronic disease patients had a similar insignificant effect.
The ‘work quantity’ that is the hours for which a therapist worked, and the patients he examined per day had no significant correlation with burnout. The times he had to wake up for emergencies, hours of continued medical education per year and hospital paper work also did not relate significantly. Some clinicians with abnormal lipid profiles, fasting glucose, etc. had no burnout while those with normal values reported higher burnout and lack of compassion satisfaction. As against the conventional thought, smoking, consumption of alcohol and tobacco also did not affect burnout, compassion satisfaction, and secondary traumatic stress values.
DISCUSSION
The current study aimed at identifying ‘burnout’ and ‘compassion fatigue’ among clinicians involved in care of individuals suffering from medical illness. The adverse effects associated with clinician burn out and an increasing trend in emotional exhaustion of clinicians over the years makes it important to study this phenomenon.[4]
Health professionals' quality of life is a vital, yet understudied and less understood aspect of health care. Compassion fatigue and the burnout that the physician faces have not been given any significant importance that they deserve.
Burnout is the most well established measure of stress and distress in clinicians. Burnout among clinician is not an uncommon phenomenon with up to one third expected to be experiencing the same at a given point in time.[3] Clinician burnout has been shown to impact the patient care adversely.[5–7] In an earlier study, burnout has been shown to affect patient care. Emotional exhaustion was included as a potential predictor of personal accomplishment and depersonalization. It was conceptualized as the core element of burnout.[15] Also, it has been demonstrated in another study that organizational measures, specifically, evaluative ratings of workload/scheduling and input/influence are the strongest predictors of emotional exhaustion amongst the physicians.[16] These issues are especially more relevant for clinicians dealing with chronic diseases as they are more prone to get exhausted while treating and counseling the patient.
Various predictors of health care professionals' burn out include patient related, clinician related and work place related factors. Younger age, difficult family dynamics, and uncertain prognosis are important patient related factors predicting the burn out among health care professionals.[17–19] It has been observed that oncologists tend to have relatively higher levels of burn out.[20,21] Burnout has been well observed and studied in oncologists but burnout and compassion fatigue associated with diabetes patients and other endocrinological disorders still remains less researched.[22] Additionally, the available literature on this topic is restricted to western settings. There is paucity of published work on this issue in the Indian setting.
The current study revealed that clinicians having a significant diabetology practice were more prone to burnout. Perhaps this was because patients suffering from diabetes mellitus demand more time and empowerment during shared decision making, to achieve therapeutic goals. The role of the clinician in treating a case of diabetes is vital, as patient education forms a major part of the treatment. Clinicians need to get more involved and spend more time with such patients and thus are more predisposed to burnout and compassion fatigue.
Another significant association of burnout was with the experience of the therapist. Therapists who have been into practice for a longer duration of time have reported less burnout levels. Studies from west have also found young age as a predictor of burn out among clinicians.[20] This may be related as an ‘escape phenomenon’, where experienced clinicians have devised ways to maintain adequate levels of patient satisfaction and simultaneously causing no burnout to them. Work experience definitely supports the patient – clinician relationship and ensures better health care from the clinician's end.
A striking difference of compassion satisfaction was seen amongst clinicians working in private setup versus a government setup. Also, poor working conditions, significantly affected burnout and compassion satisfaction. These two results maybe related. Government setups may have poor working conditions leading to lack of compassion satisfaction in the clinicians. On the other hand, in the private setup, modern equipment, trained staff, and good working conditions, prevent burnout of the clinician and ensure better compassion satisfaction. A Swiss study among physicians also reported higher feelings of low accomplishment among physicians working in public institutions as compared to those working in private settings.[23] Work load, both quantitative as well as qualitative, have been consistently associated with burnout among clinicians (including mental health professionals) across studies.[8,24,25] Isolation from specialist advice, lack of support out of hours, and not having access to or taking adequate leaves have also been established as predictors of burnout in western settings.[20,26]
Lastly, the financial constraints demonstrate significant affect over burnout. Clinicians, who were well off and had no patient treatment cost issues, were less burnt out. This may be of significant importance in government setup where clinicians may be more burnt out due to fewer salaries, and more work load.
Earlier in 2008, a similar study, conducted at a specialist diabetes care centre in the same district showed lesser burnout, higher compassion satisfaction, and lower secondary traumatic stress.[27] This could probably be due to better working conditions, less financial constraints, and inclusion of only trained diabetes care professionals (DCPs) in this cohort. Also, in such a centre the patients were better satisfied as each of them could be given much more time, as compared to per patient time in a general physician OPD or in a government hospital.
The study, additionally, brings to attention the concept of ‘Physician, Heal Thyself’.[3] This positive health psychology concept aims at reducing the ongoing stress and compassion fatigue of the physicians. Clinician stress, fatigue, and burnout not only interfere with their job satisfaction, they also impact their health adversely.[6,28] Psychiatric disorders among clinicians have been found to be independently associated with the stress of feeling overloaded, dealing with treatment toxicity/errors, and deriving little satisfaction from professional status.[29] It is equally important for clinicians to take care of themselves while they take care of their patients. Coping strategies such as ‘painful problem solving’ and ‘positive reappraisal’ have been associated with lower levels of burnout in hospice nurses.[30] Similarly, clinicians who have received communication training are less likely to experience burnout.[20] Additionally, number of hours spent for continuing education is known to have a positive influence on self-esteem and work-related satisfaction among clinicians.[16,31,32]
The current study suggests that ensuring better working conditions can help reduce burnout and improve compassion satisfaction in the medical practitioners. These include the staff working at the centre, the ambience, and the latest equipment. Better and effective ways of dealing with chronic care patients also play a role. Also, financial satisfaction is necessary along with quality health care to prevent early burnout and maintain the enthusiasm of the clinicians. The study had certain limitations. The study sample comprised of a heterogonous group of clinicians from both medical and surgical specialties. The burn our scores were found to differ between clinicians form different specialties. Future studies among clinicians from specific specialty would be more informative.
The current study suggests that it is important to find out ways of decreasing burnout and compassion fatigue among clinicians. Stress management and coping skills training can be considered as a measure to decrease significant burnout and compassion fatigue.[27] Clinicians should try and practice ‘safe stress’ or ‘eu-stress’ which in no way harms them, rather is creative, beneficial and improves their work efficiency. The phrase “Physician, heal thyself” if extrapolated to “Physician, love thyself”, may not be narcissistic, but give us an compassionate health care provider, and an invaluable asset to the society.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Figley CR. Compassion fatigue: Psychotherapists' chronic lack of self care. J Clin Psychol. 2002;58:1433–41. doi: 10.1002/jclp.10090. [DOI] [PubMed] [Google Scholar]
- 2.Soderfelt M, Soderfelt B. Burnout in social work. Social Work. 1995;40:638–47. [Google Scholar]
- 3.West CP, Huschka MM, Novotny PJ, Soan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA. 2006;296:1071–8. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 4.Taylor C, Graham J, Potts HW, Richards MA, Ramirez AJ. Changes in mental health of UK hospital consultants since the mid-1990s. Lancet. 2005;366:742–4. doi: 10.1016/S0140-6736(05)67178-4. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt TD. Enhancing meaning in work: A prescription for preventing physician burnout and promoting patient-centered care. JAMA. 2009;302:1338–40. doi: 10.1001/jama.2009.1385. [DOI] [PubMed] [Google Scholar]
- 6.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: A missing quality indicator. Lancet. 2009;74:1714–21. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 7.Lemaire JB, Wallace JE, Dinsmore K, Lewiin AM, Ghali WA, Roberts D. Physician nutrition and cognition during work hours: Effect of a nutrition based intervention. BMC Health Serv Res. 2010;10:241. doi: 10.1186/1472-6963-10-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 9.Zellmer DD. Teaching to prevent burnout in the helping professions. Analytic Teaching. 2005;24:20–5. [Google Scholar]
- 10.Hudnall Stamm B. ProQoL Version 5. www.proqol.org .
- 11.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 12.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetic Association. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 14.Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 15.Boucher JL. Clinician burnout: How do clinicians take care of themselves? Diabetes Spectrum. 2011;24:59–60. [Google Scholar]
- 16.Graham J, Potts HW, Ramirez AJ. Stress and burnout in doctors. Lancet. 2002;360:1975–6. doi: 10.1016/s0140-6736(02)11871-x. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd-Williams M. Senior house officers' experience of a six month post in a hospice. Med Educ. 2002;36:45–8. doi: 10.1046/j.1365-2923.2002.01103.x. [DOI] [PubMed] [Google Scholar]
- 18.Wilkes LM, Beale B. Palliative care at home: Stress for nurses in urban and rural New South Wales, Australia. Int J Nurs Pract. 2001;7:306–13. doi: 10.1046/j.1440-172x.2001.00267.x. [DOI] [PubMed] [Google Scholar]
- 19.Kirchhoff KT, Spuhler V, Walker L, Hutton A, Cole BV, Clemmer T. Intensive care nurses' experiences with end-of-life care. Am J Crit Care. 2000;9:36–42. [PubMed] [Google Scholar]
- 20.Girgis A, Hansen V. Newcastle, NSW: Centre for Health research and Psycho-oncology (CHeRP), University of Newcastle; 2007. Prevalence and predictors of burnout in the COSA oncology workforce. [Google Scholar]
- 21.Trufelli DC, Bensi CG, Garcia JB, Narahara JL, Abrão MN, Diniz RW, et al. Burnout in cancer professionals: A systematic review and meta-analysis. Eur J Cancer Care (Engl) 2008;17:524–31. doi: 10.1111/j.1365-2354.2008.00927.x. [DOI] [PubMed] [Google Scholar]
- 22.Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: Results of a random survey of 1,000 oncologists. J Clin Oncol. 1991;9:1916–20. doi: 10.1200/JCO.1991.9.10.1916. [DOI] [PubMed] [Google Scholar]
- 23.Arigoni F, Bovier PA, Mermillod B, Waltz P, Sappino AP. Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: Who are most at risk? Support Care Cancer. 2009;17:75–81. doi: 10.1007/s00520-008-0465-6. [DOI] [PubMed] [Google Scholar]
- 24.Renzi C, Tabolli S, Ianni A, Di Pietro C, Puddu P. Burnout and job satisfaction comparing healthcare staff of a dermatological hospital and a general hospital. J Eur Acad Dermatol Venereol. 2005;19:153–7. doi: 10.1111/j.1468-3083.2005.01029.x. [DOI] [PubMed] [Google Scholar]
- 25.Thomsen S, Soares J, Nolan P, Dallender J, Arnetz B. Feelings of professional fulfilment and exhaustion in mental health personnel: The importance of organisational and individual factors. Psychother Psychosom. 1999;68:157–64. doi: 10.1159/000012325. [DOI] [PubMed] [Google Scholar]
- 26.Taubert M, Nelson A. 'Oh God, not a palliative': Out-of-hours general practitioners within the domain of palliative care. Palliat Med. 2010;24:501–9. doi: 10.1177/0269216310368580. [DOI] [PubMed] [Google Scholar]
- 27.Sanjay K, Komal C, Bharti K. Compassion fatigue in diabetes care professionals: Effect of cognitive therapy. Indian J Endocrinol Metab. 2008;12:7–10. [Google Scholar]
- 28.Rosenstein AH, Mudge-Riley M. The impact of stress and burnout on physician satisfaction and behaviors. Physician Exec. 2010;36:16–8. [PubMed] [Google Scholar]
- 29.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM, Leaning MS, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–9. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Payne N. Occupational stressors and coping as determinants of burnout in female hospice nurses. J Adv Nurs. 2001;33:396–405. doi: 10.1046/j.1365-2648.2001.01677.x. [DOI] [PubMed] [Google Scholar]
- 31.Travado L, Grassi L, Gil F, Ventura C, Martins C. Southern European Psycho-Oncology Study Group. Physician–patient communication among Southern European cancer physicians: The influence of psychosocial orientation and burnout. Psychooncology. 2005;14:661–70. doi: 10.1002/pon.890. [DOI] [PubMed] [Google Scholar]
- 32.Libert Y, Merckaert I, Reynaert C, Delvaux N, Marchal S, Etienne AM, et al. Does psychological characteristic influence physicians' communication styles? Impact of physicians' locus of control on interviews with a cancer patient and a relative. Support Care Cancer. 2006;14:230–42. doi: 10.1007/s00520-005-0871-y. [DOI] [PubMed] [Google Scholar]


