Abstract
Background:
India is a country of several diversities and cultures, which may influence the help-seeking behavior of mentally ill patients and families. Only a few Indian studies have focused on help seeking, especially for severe mental disorders.
Objective:
The study aimed to describe and compare the help-seeking behaviors among caregivers of psychotic patients visiting psychiatric clinics at two distinct cities of India.
Materials and Methods:
This was a cross-sectional exploratory study of key caregivers (N=50) of patients with a DSM-IV TR diagnosis of schizophrenia and other psychotic disorders, visiting psychiatric out-patient departments of VIMHANS, New Delhi, and CIMS, Bilaspur, Chhattisgarh. After due informed consent was taken, a semi-structured proforma was administered for socio-demographic profile, illness details, causative beliefs, and information on help seeking.
Results:
Supernatural forces were held responsible by 40% of the Bilaspur sample in contrast to 8% in New Delhi sample. Faith-healers were initial contacts for 56% and 64% of sample, respectively, at New Delhi and Bilaspur. Faith-healers followed by a psychiatrist formed the commonest pathway of care at both centers (32% and 36%, respectively). The sample at New Delhi spent significantly more money (median: $4000 vs. $10) and traveled greater distances (median: 35 km vs. 10 km) for faith-healers during the course of illness. Two-thirds of sample in New Delhi and one-third at Bilaspur were aware of the nearby psychiatrist at the time of initial help seeking; however, only 28% and 12%, respectively, chose psychiatrist as an initial contact. The New Delhi sample reported a fear of medication adverse effects and stigma as perceived disadvantages of psychiatric help. The median time lost at both the centers was 1 month, with a maximum of 8.4 years in New Delhi and 4.9 years in Bilaspur. Of the total, 16% caregivers at New Delhi and 32% at Bilaspur center reported an intention to continue with faith-healing practices alongside psychiatric care.
Conclusion:
In spite of differing causal attributions, the patients and families across these cities may not be as different when it comes to behaviors related to help seeking for mental illness. Future large-scale studies across various regions of India may help in determining sociocultural and regional patterns of help seeking in greater detail.
Keywords: Causative beliefs, India, help seeking, pathways of care, psychotic disorders
INTRODUCTION
India is a country of several diversities and cultures, which may influence the causative beliefs, and consequently, the help-seeking behaviors of the mentally ill patients and families. Nearly 6.5% of Indian population suffers from a serious mental or behavioral disorder.[1] With only 3500 psychiatrists in a country of over a billion, the average national deficit of psychiatrists is estimated to be 77%.[2] Further, there are only 500 clinical psychologists, 400 psychiatric social workers, and 900 psychiatric nurses, against an estimated national requirement of 17,250 clinical psychologists, 23,000 psychiatric social workers, and 3000 psychiatric nurses, pointing to a huge deficit of mental health professionals.[3] The coverage of treatment services is patchy and inadequate. Further, in many parts of India and other developing countries, the medical model of care is considered as external and more faith is put on magico-religious or faith-based healing methods. These healing traditions are typically based on notions of supernatural affliction, such as spirit possession, sorcery, and religious healing.[4]
The pathway of care is the sequence of contacts initiated by the patients or families in their efforts to seek care. The pathway and the associated help-seeking behaviors help us in identifying the possible sources of delay in presentation. An understanding of the way in which people seek help for mental disorders is important for planning mental health services, coordinating the psychiatric referrals, and enhancing the treatment-seeking attitude.[5,6] Goldberg and Huxley proposed a model that people with psychiatric problems initiate care by consulting their general practitioners, who may refer them to psychiatric facilities.[7] While this may be more true for well-resourced western countries, it has been seen that patients from low-resourced developing countries rely more often on non-professional care.[4]
Very few Indian studies have focused on the pathways or help-seeking behaviors of psychiatric patients.[8–11] Further, their samples mostly comprise common mental disorders (e.g. depression, anxiety, somatoform, etc.) presenting to clinics and only limited information is available on help-seeking behaviors for psychotic disorders. It is likely that help-seeking behaviors may have regional differences depending on accessibility to mental health services, prevailing perceptions of mental illness, and other sociocultural factors.
The present study aimed to describe and compare the pathway of care, help-seeking behaviors, and causative beliefs among caregivers of schizophrenia and other psychotic patients visiting the psychiatry clinics at two geographically and culturally distinct Indian cities. As the two cities contrasted in several socioeconomic and cultural factors, we hypothesized that the help-seeking behaviors would differ significantly between the two study centers.
MATERIALS AND METHODS
This was a cross-sectional, hospital-based study conducted simultaneously at the out-patient clinics of a neuropsychiatric hospital in New Delhi, India, and the psychiatry department of a Government Medical College in Bilaspur, Chhattisgarh. These settings were chosen as both these centers provide specialized care and mental health services to a large number of mentally ill persons in the catchment area and are located in two distinct cities of North and Central India, which contrast in several social, economic, and cultural parameters, as described below.
Delhi
With the second highest population (17 million) in India, it is a major cultural, political, and commercial center located in northern India.[12] The economy of Delhi has a contribution of 78%, 21%, and 1%, respectively, from tertiary (e.g. service sector), secondary (e.g. manufacturing), and primary (e.g. agriculture) sectors. The average annual per-capita income (66,728 INR/US$1080) is 2.5 times higher than the national average and poverty rates are 8.2% compared to the national average of 26%.[13,14] The state of Delhi has a surplus (13%) of psychiatrists, considering an ideal number of one psychiatrist per lakh population.[2] Over time, the capital city, satellite cities, and adjoining suburban and rural areas have evolved into a pool of various Indian cultural styles with people migrating from other parts, along with influences of westernization and globalization.
Bilaspur, Chhattisgarh
Bilaspur is a city with a population of 0.3 million,[12] located in the central Indian state of Chhattisgarh.[12] It a traditional culture-rich state with low population density, huge biodiversity, and coverage of forests in 44% area.[15,16] Nearly 80% of its population is rural (of which 33% is tribal), and economy is based on agriculture followed by horticulture, animal husbandry, and power or steel industries.[16,17] Certain sociocultural beliefs pertaining to witchcraft and sorcery are widespread, even though it is the only Indian state to introduce a separate legislation for witchery. Various magico-religious and supernatural beliefs related to health and illness are part of the cultural upbringing, especially among rural and tribal areas. The psychiatric services are grossly inadequate, with an average estimated deficit of 92.8% for psychiatrists.[2]
Study settings
Centre I (Vidyasagar Institute of Mental Health and Neurosciences (VIMHANS), New Delhi): Established in 1980s, it is a specialty hospital providing a comprehensive range of mental health services, including out- and in-patient psychiatry, psychological services, rehabilitation, community out-reach, school-based programs, and community awareness activities. It is also a teaching hospital for postgraduate psychiatry and conducts regular training activities for mental health professionals.
Centre II (Chhattisgarh Institute of Medical Sciences (CIMS), Bilaspur): Established in 2001, it is an Medical Council of India (MCI)-approved, state-funded undergraduate teaching institution with an annual intake of 100 medical students. In addition to out-patient and in-patient psychiatric care, the teaching and training activities are conducted for undergraduate medical students and interns in the field of mental health. The institution was established to provide quality medical education and health care, particularly to the tribal, backward, and rural community of Chhattisgarh.
Study criteria and sample
The study sample comprised a total of 50 key caregivers of schizophrenia and other psychotic patients (n=25 for each center). The patients of all age groups and either gender presenting with a psychotic illness for the first time at any of the two study centers during the same month were screened by pre-defined criteria. Patients who fulfilled the DSM-IV TR[18] diagnosis of schizophrenia and other psychotic disorders and were accompanied by the key caregiver were selected. The key caregiver was defined as the family member or relative aged 18 years and above, who accompanied the patient to hospital, had almost a daily regular and uninterrupted contact with the patient, resided in the same family or near to patient's residence, and was actively involved in patient care. Presence of mental subnormality, significant head trauma, substance dependence (other than nicotine) in the patient, and non-availability of the key caregiver were the exclusion criteria.
Study procedure
After a written informed consent was taken, the key caregiver was interviewed in detail using specially designed semi-structured proforma which covered the following areas: (a) socio-demographic profile – age, gender, residence, education, religion, socioeconomic status, relationship to patient; (b) details pertaining to patient's illness, including onset and duration; (c) understanding about the likely causes of patient's illness and behavior; and (d) information on pathway of care and help-seeking behaviors, including the contact person(s), distance to nearest psychiatrist, awareness of nearby mental health services, resources spent in help seeking, and delay in reaching professional care. The study was conducted in accordance with the ethical standards of Declaration of Helsinki. Full confidentiality was ensured in presentation of the results.
The data were analyzed using SPSS version 17.0. Descriptive statistics are presented. Mann–Whitney test was used to compare mean ranks across two groups in case of non-parametric data. Chi-square test was used, wherever suitable, for categorical variables.
RESULTS
There were a total of 50 key caregivers assessed at both the study centers, which comprised mothers (30%), fathers (24%), spouses (14%), brothers (12%), sons (6%), daughters (6%), and other relatives (10%) of the patient.
Socio-demographic characteristics
Table 1 shows the socio-demographic profile of the sample at both the study centers. Nearly two-thirds (76%) of caregivers at New Delhi study center were educated till matriculation or above, while 68% of the caregivers at Bilaspur study center were either illiterate or had <10 years of education. Majority (80%) of the sample at the New Delhi study center belonged to middle socioeconomic status, while the majority (84%) in Bilaspur study center belonged to lower socioeconomic status. Sixty percent of the sample belonged to urban areas at the New Delhi center and to rural areas at the Bilaspur center. Rest of the socio-demographic parameters, including age, gender, marital status, and religion, were similar in distribution across the two study groups.
Table 1.
Caregivers' socio-demographic profile and patients' illness characteristics
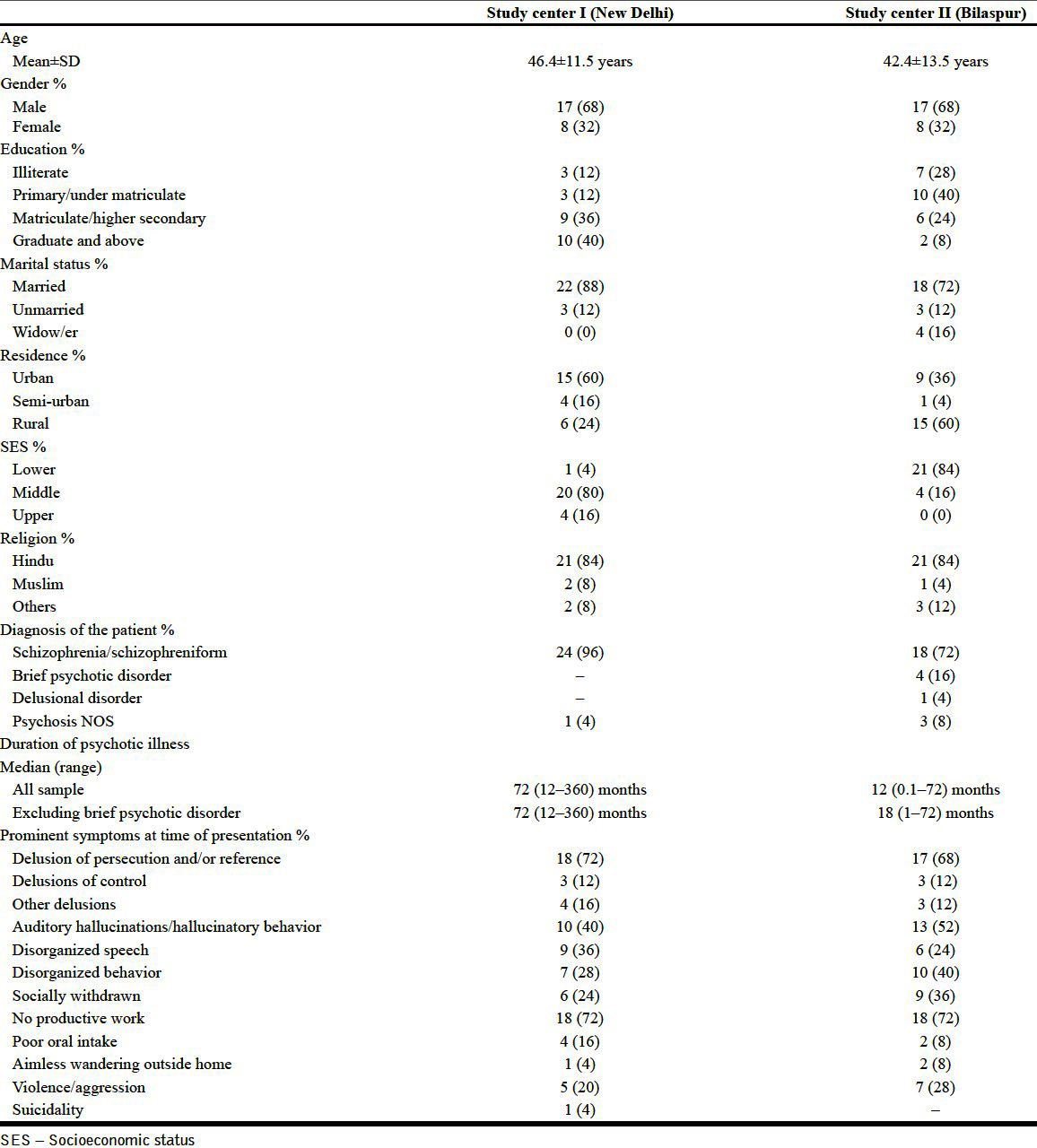
Patient illness characteristics
Table 1 shows the patient illness characteristics at both the study centers. Schizophrenia was the diagnosis in all but one patient in study center I, while schizophrenia and schizophreniform disorder were present in 56% and 16%, respectively, in study center II. The mean duration of psychotic illness was 98.0±76.9 months at study center I and 19.4±20.6 months at study center II. The median duration of psychotic illness is shown in Table 1. The illness duration was significantly longer for patients seen at study center I compared to study center II (Mann-Whitney U=60.00; Z=4.82; P<0.01).
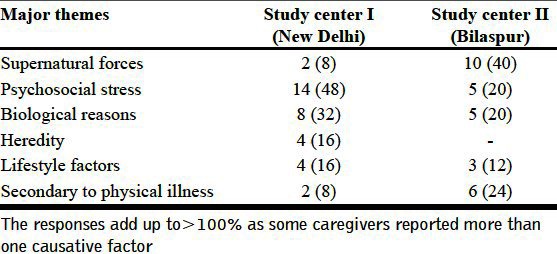
Caregivers' understanding of illness causation
Table 2 shows the frequency of major themes reflected in caregivers' responses. The commonest theme in study center I was psychosocial stress (48%) and the commonest theme in study center II was supernatural forces (40%) as the possible causation of patient's illness.
Table 2.
Caregivers' understanding of illness causation - Major themes
Pathway of care and help-seeking behaviors
The help-seeking behaviors for both the study centers are shown in Table 3. Faith-healers were the initial contact persons for a majority of patients in study center I (56%) and study center II (64%), as seen in Table 3. The common pathways to first psychiatric care in study sample I were: (a) faith-healing followed by a psychiatrist (32%; 8), (b) seeking a psychiatrist's consultation directly (28%, 7), and (c) physician followed by a psychiatrist (16%; 4). The common pathways to initial psychiatric care in study sample II were: (a) faith-healing followed by a psychiatrist (36%; 9), (b) faith-healing followed by a physician followed by a psychiatrist (24%; 6), and (c) physician followed by a psychiatrist (20%; 5).
Table 3.
Help-seeking behaviors for patients with schizophrenia and other psychotic disorders
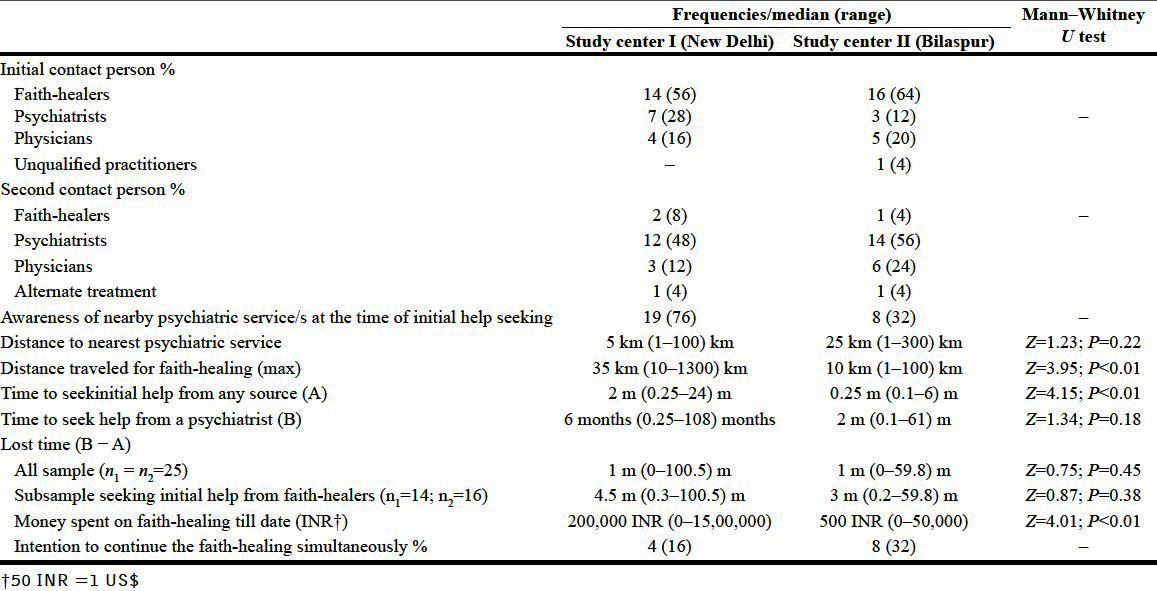
The awareness of a nearby psychiatric service/s at the time of initial help seeking was present in 76% and 32% of the sample, respectively. The median time lost in the subsample which sought faith-healing was 4.5 months (10 days to 8.4 years) in study center I and 3 months (6 days to 4.9 years) in study center II (Z=0.87; P=0.38). Of the total caregivers, 16% of study center I and 32% of study center II reported an intention to continue with faith-healing practices alongside the psychiatric care.
On exploring the perceived reasons for seeking faith-healing and perceived disadvantages of psychiatric help, the prominent themes to emerge in study center I were as follows: (a) fear of possible adverse effects of medications, e.g. medications are sedating or addictive; (b) medical treatment is often too lengthy in duration; and (c) psychiatric help perceived as stigmatizing. In contrast, the sample at study center II did not per se report any disadvantages of medical care, and the main themes to emerge were: (a) prior positive outcomes with faith-healing in self and others; (b) causation was perceived to be supernatural, which needed a religious person rather than a doctor; and (c) as there was no physical problem, a medical doctor was not considered. The most common reason reported by almost all the caregivers for switching from faith-healing to a medical treatment was non-improvement or only a temporary short-lasting improvement with the faith-healing.
DISCUSSION
The study describes and compares the help-seeking behaviors adopted by the caregivers of psychotic patients presenting to psychiatric clinics at two geographically apart cities of India. The cities are contrast to each other in several social, cultural, and economic parameters, as well as availability of mental health services.
The caregivers at both the centers were comparable in age, gender, marital status, and religion. The educational and socioeconomic status was relatively higher in New Delhi sample compared to Bilaspur sample, which is representative of average population profile across the two cities.[13,17] Nearly 60% of New Delhi sample and 36% of Bilaspur sample was from urban areas, while the rest were from adjoining suburban or rural areas. The psychiatrists are generally available at the more central or city locations and patients often travel from surrounding rural areas to the nearest city for seeking treatment. There were no major differences in the clinical symptomatology and patient behaviors at both the centers, though the median duration of psychotic illness was significantly longer in patients presenting at New Delhi study center.
The supernatural forces were held responsible for patient's behavior in nearly 40% of the Bilaspur sample in contrast to only 8% in New Delhi sample. Earlier studies from India[19,20] have shown magico-religious phenomenon (black magic) as a frequent causal belief, which was reported by over 70% of clinic sample in Vellore, a city with a population of nearly 0.3 million in South India. A separate study from the metropolitan city of Chennai (a state capital with population over 5 million) found that only 12% of families reported a supernatural causation for schizophrenia.[21] It is of interest to note that the findings from Vellore and Chennai centers were in remarkable contrast to each other, and draw a parallel to the causal attributions seen in the present study.
The socio-demographic as well as local cultural factors of a city are likely to influence the illness-related beliefs and perceptions.[4] The New Delhi sample appeared to favor biopsychosocial causation more often compared to Bilaspur sample. It could be due to more access to information, higher level of awareness, growing western influences, and a trend of moving away from indigenous concepts toward the gradual adoption of biomedical model. Nearly 36% caregivers in New Delhi and 16% Bilaspur center held more than one kind of belief to explain the abnormal behavior of patient. This is in accordance with previous studies from India and other developing countries which have found patients to hold multiple beliefs about causation.[20,22]
Another main finding of the study is that the pathways and initial help seeking at New Delhi center were not remarkably different from the Bilaspur sample. The caregivers in New Delhi and Bilaspur showed a similarly high reliance on faith-healers (56% and 64%, respectively) and similar delays in time to reach psychiatric care. The sample at New Delhi was rather found to spend significantly more money (median of $4000 vs. $10; P<0.01) and traveled significantly greater distances (median of 35 km vs. 10 km; P<0.01) to seek help from faith-healers. This could be due to better socioeconomic status or a longer duration of psychosis. Nonetheless, it points to a similar pattern of help-seeking behaviors across two cities despite an obvious difference in causal attributions. It seems that the traditional methods of help seeking which have been passed across generations may be deeply ingrained in people. These socioculturally sanctioned methods of help seeking may not show an immediate and drastic change with an increasing affluence, socioeconomic progress, or exposure to a globalized culture of a metropolitan city.
Nearly one in two psychotic patients at both the centers was initially taken to faith-healers for help. A previous study from Gwalior, India, found that faith-healers were sought by 68% of patients mostly suffering from severe mental disorders.[9] Another multicenter study which focused on general psychiatric (mostly neurotic) patients across five different hospitals of India found that samples from Delhi (42%) and Kerala (74%) had higher frequency of psychiatrists as initial contacts and samples at Ranchi (43.4%) had the highest frequency of faith-healers as initial contacts. Earlier studies from Delhi[8,11] have also found psychiatrists to be the most common initial contacts; however, nearly 90% of their sample comprised common mental disorders. It is possible that help-seeking process may differ for psychotic patients whose behaviors are clearly odd and disorganized, coupled with a reluctance to visit a doctor.
Interestingly, two-thirds of sample in New Delhi were aware of the nearby psychiatrist at the time of initial help seeking; however, only 28% sought psychiatrist as an initial contact. The reasons for choosing faith-healers over a psychiatrist could be multifold and appeared to differ across the two centers. The sample at Bilaspur reported prior positive outcomes with faith-healing, supernatural causation, and a lower awareness of mental illness and its treatment, while the sample at New Delhi reported the fear of adverse effects of medication, length of psychiatric treatment, and perceived stigma of visiting a psychiatrist. The sample at New Delhi appeared to harbor misconceptions and stigma pertaining to psychiatric treatment in spite of having higher education and resources. It appears that even though Delhi has a surplus of 13% psychiatrists,[2] mere availability of mental health services may not be enough to change the attitude and behaviors of people. Active efforts must be made to reduce the stigma and enhance the acceptability and perceived safety of psychiatric treatment. There is a need for a greater sensitization and awareness to get professional help early in the course of schizophrenia and other psychotic disorders, especially as an early diagnosis and treatment is known to influence patient's outcome.
Even though India, like other developing countries, has made considerable progress with regard to mental healthcare, faith-healers are frequent care providers for majority of psychiatric patients, and in some instances, caregivers may revert back to faith-healers or simultaneously seek help from modern as well as traditional methods of therapy.[6,23,24] Nearly 32% of Bilaspur sample and 16% of New Delhi sample reported an intention to continue the faith-healing alongside the medical treatment. This pluralistic approach to medical treatment has been reported from India[19,25] as well as from other developing countries.[26,27] It emphasizes the importance of socioculturally sanctioned pathways in the help-seeking process. From a clinical perspective, it is important for psychiatrists to take into account the individual's perceptions and attitudes toward illness and not be overtly dismissive of their efforts at seeking simultaneous help from traditional sources.
The factors causing delay in help seeking may vary from region to region depending on sociocultural profile, education, societal attitude toward mental illness, perceptions, myths, beliefs, stigma, availability/accessibility of psychiatric services, and previous experience of receiving psychiatric help.[6] There is a need to delineate help-seeking behaviors and pathways of care as well as their determinants in the developing countries. The awareness of mental disorders in general population could address cultural myths and stigma related to psychiatric disorders, consequently enhancing the treatment-seeking attitude from mental health professionals. It is important that the interventions to enhance awareness and treatment seeking from mental health care facilities be provided in a culturally appropriate and socially acceptable fashion.
The study has several limitations. It was a pilot study with relatively small sample size. Findings across two cities may be different in larger samples. It was a hospital-based sample, and the help-seeking process and beliefs may be different in community populations. The recall bias may have been introduced while obtaining help-seeking information from the caregivers. The role of various socio-demographic variables, e.g. education, rural-urban residence, etc., in help seeking was not explored in view of the small sample size. Future large-scale studies across various regions of India may help in determining sociocultural and regional patterns of help seeking and pathways of care.
To conclude, the caregivers at New Delhi study center attributed the illness to biological and psychosocial reasons more often in contrast to Bilaspur with a preponderance of supernatural causative beliefs. The caregivers at both the centers displayed broadly similar help-seeking behaviors for mental illness, with a higher reliance on faith-healers as initial contacts. In spite of several socioeconomic differences across the two city samples, the patients and families may not be as different, when it comes to behaviors related to mental illness.
‡Findings from this study were presented as poster at IV International Conference on Schizophrenia, Schizophrenia Research Foundation-SCARF (co-sponsored by WPA, WHO IPS, Douglas Hospital Research Centre and RCP) held at Chennai, India, from 20 to 22 Oct, 2010.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.NCMH background papers-Burden of disease in India, National Commission of Macroeconomics and Health 2005. [Accessed Dec 1, 2011]. Available from: http://www.whoindia.org/en/Section102/Section201_888.htm .
- 2.Thirunavukarasu M, Thirunavukarasu P. Training and National deficit of psychiatrists in India-A critical analysis. Indian J Psychiatry. 2010;52:S83–8. doi: 10.4103/0019-5545.69218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinha SK, Kaur J. National mental health programme: Manpower development scheme of eleventh five-year plan. Indian J Psychiatry. 2011;53:261–5. doi: 10.4103/0019-5545.86821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gater R, de Almeida e Sousa B, Barrientos G, Caraveo J, Chandrashekar CR, Dhadphale M, et al. The pathways to psychiatric care: a cross-cultural study. Psychol Med. 1991;21:761–74. doi: 10.1017/s003329170002239x. [DOI] [PubMed] [Google Scholar]
- 5.Rogler LH, Cortes DE. Help-seeking pathways: A unifying concept in mental health care. Am J Psychiatry. 1993;150:554–61. doi: 10.1176/ajp.150.4.554. [DOI] [PubMed] [Google Scholar]
- 6.Trivedi JK, Jilani AQ. Pathway of psychiatric care. Indian J Psychiatry. 2011;53:97–8. doi: 10.4103/0019-5545.82530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldberg DP, Huxley P. London: Tavistock Press; 1980. Mental illness in the community: The pathway to psychiatric care. [Google Scholar]
- 8.Chadda RK, Agarwal V, Singh MC, Raheja D. Help seeking behaviour of psychiatric patients before seeking care at a mental hospital. Int J Soc Psychiatry. 2001;47:71–8. doi: 10.1177/002076400104700406. [DOI] [PubMed] [Google Scholar]
- 9.Lahariya C, Singhal S, Gupta S, Mishra A. Pathway of care among psychiatric patients attending a mental health institution in central India. Indian J Psychiatry. 2010;52:333–8. doi: 10.4103/0019-5545.74308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pradhan SC, Singh MM, Singh RA, Das J, Ram D, Patil B, et al. First care givers of mentally ill patients: A multicenter study. Indian J Med Sci. 2001;55:203–8. [PubMed] [Google Scholar]
- 11.Mishra N, Nagpal SS, Chadda RK, Sood M. Help-seeking behavior of patients with mental health problems visiting a tertiary care center in north India. Indian J Psychiatry. 2011;53:234–8. doi: 10.4103/0019-5545.86814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Census of India. Office of the Registrar General and Census Commissioner, Ministry of Home Affairs, Government of India. [Accessed Dec 25, 2011]. Available from http://censusindia.gov.in .
- 13.State Income. Economic Survey of Delhi, 2007-2008. Planning Department, Government of National Capital Territory of Delhi. [Accessed Dec 25, 2011]. pp. 10–17. Available from: http://delhiplanning.nic.in/Economic%20Survey/ES2007-08/C2.PDF .
- 14.Poverty line in Delhi. Economic Survey of Delhi, 2007–2008. Planning Department, Government of National Capital Territory of Delhi. [Accessed Dec 25, 2011]. pp. 241–244. Available from: http://delhiplanning.nic.in/Economic%20Survey/ES2007-08/C21.PDF .
- 15.Chhattisgarh at a glance. Department of Finance and Planning, Government of Chhattisgarh. [Accessed Dec 25, 2011]. Available from: http://www.descg.gov.in/publications.aspx .
- 16.Chhattisgarh@2022, Vision document, Confederation of Indian Industries, Chhatisgarh. [Accessed Dec 25, 2011]. Available from: http://www.indiaat75.in/vision-statewise-pdf%27 s/Chattisgarh_Vision Document.pdf .
- 17.Chhattisgarh: Socio-economic analysis. Department of Finance and Planning, Government of Chhattisgarh. [Accessed Dec 25, 2011]. Available from: http://www.descg.gov.in/publications.aspx .
- 18.Text revision (DSM-IV TR) 4th ed. Washington DC: American Psychiatric Association; 2000. American psychiatric association. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 19.Saravanan B, Jacob KS, Deepak MG, Prince M, David A, Bhugra D. Perceptions about psychosis and psychiatric services: A qualitative study from Vellore, India. Soc Psychiatry Psychiatr Epidemiol. 2008;43:231–8. doi: 10.1007/s00127-007-0292-y. [DOI] [PubMed] [Google Scholar]
- 20.Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Belief models in first episode schizophrenia in South India. Soc Psychiatry Psychiatr Epidemiol. 2007;42:446–51. doi: 10.1007/s00127-007-0186-z. [DOI] [PubMed] [Google Scholar]
- 21.Srinivasan TR, Thara R. Beliefs about causation of schizophrenia: Do Indian families believe in supernatural causes? SOC Psychiatry Psychiatr Epidemiol. 2001;36:134–40. doi: 10.1007/s001270050302. [DOI] [PubMed] [Google Scholar]
- 22.Phillips MR, Li Y, Stroup TS, Xin L. Causes of schizophrenia reported by patients' family members in China. Br J Psychiatry. 2000;177:20–5. doi: 10.1192/bjp.177.1.20. [DOI] [PubMed] [Google Scholar]
- 23.Saravanan B, Jacob KS, Prince M, Bhugra D, David AS. Culture and insightrevisited. Br J Psychiatry. 2004;184:107–9. doi: 10.1192/bjp.184.2.107. [DOI] [PubMed] [Google Scholar]
- 24.Raguram R, Venkateswaran A, Ramakrishna J, Weiss MG. Traditional community resources for mental health: A report of temple healing from India. BMJ. 2002;325:38–40. doi: 10.1136/bmj.325.7354.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joel D, Sathyaseelan M, Jayakaran R, Vijayakumar C, Muthurathnam S, Jacob KS. Explanatory models of psychosis among community health workers in South India. Acta Psychiatr Scand. 2003;108:66–9. doi: 10.1034/j.1600-0447.2003.01327.x. [DOI] [PubMed] [Google Scholar]
- 26.Leslie C. The ambiguities of medical revivalism in modern India. In: Leslie C, editor. Asian medical systems: A comparative study. Berkeley: University of California Press; 1976. pp. 356–67. [Google Scholar]
- 27.Patel V, Musara T, Butau T, Maramba P, Fuyane S. Concepts of mental illness and medical pluralism in Harare. Psychol Med. 1995;25:485–93. doi: 10.1017/s0033291700033407. [DOI] [PubMed] [Google Scholar]


