Abstract
Adherence to a Mediterranean diet (MeD) has recently been shown to protect against cognitive decline and dementia. It remains unclear, however, whether such protection extends to differing ethnic groups and middle-aged individuals, and how it may compare with adherence to the USDA Dietary Guidelines for Americans 2005 (measured with Healthy Eating Index-2005, HEI-2005). This study examined associations between diet quality, as assessed by the MeD and HEI-2005, and cognitive performance in a sample of 1,269 Puerto Rican adults, aged 45–75 years, living in the Greater Boston area, Massachusetts. Dietary intake was assessed with a food-frequency questionnaire specifically designed for and validated with this population. Adherence to the MeD was assessed with a 0 to 9 point scale, and the HEI-2005 score was calculated with a maximum score of 100. Cognitive performance was measured with a battery of seven tests; the Mini Mental State Examination (MMSE) was used for global cognitive function. Greater adherence to the MeD was associated with higher MMSE score (P trend = 0.012) and lower likelihood (OR = 0.87 for each additional point, 95% CI, 0.80–0.94, P <0.001) of cognitive impairment, after adjustment for confounders. Similarly, individuals with higher HEI-2005 score had higher MMSE score (P trend = 0.011) and lower odds of cognitive impairment (OR = 0.86 for each 10 points, 95% CI, 0.74–0.99, P = 0.033). In conclusion, high adherence to either the MeD or the diet recommended by the USDA dietary guidelines may protect cognitive function in middle-aged and older adults.
Keywords: Mediterranean diet, Healthy Eating Index-2005, diet quality, Cognitive impairment
INTRODUCTION
The Mediterranean diet (MeD), characterized by high intake of vegetables, fruit, legumes, nuts, cereals and monounsaturated fat (olive oil); low intake of saturated fat; moderate intake of dairy foods, meat, poultry and fish; and regular moderate intake of alcohol, primarily from wine consumed with meals (1), has been associated with less cognitive decline (2) and lower risk for development of mild cognitive impairment (3) and Alzheimer disease (4, 5). However, available studies have focused mainly on older populations, with baseline age ≥65 years (2-6), and most have examined only the Mediterranean diet. One exception is a recent French study, where higher adherence to a healthy dietary pattern derived from an a posteriori statistical method in middle life was associated with better cognitive function 13 years later (7). To postpone cognitive decline, and, eventually, cognitive impairment and dementia, it is important to understand protective factors at an earlier age. It is also important to understand if there is something particular about the Mediterranean Diet itself in protecting cognitive function, or if other measures of a healthy diet are also protective.
The Healthy Eating Index-2005 (HEI-2005) is a measure of diet quality relative to adherence to the USDA Dietary Guidelines for Americans 2005 (8). Higher HEI-2005 score indicates greater adherence to the dietary guidelines. Higher HEI-2005 scores have been associated with favorable lipid profile (9) and lower risk of obesity (10) but, in one study, they were not associated with cognitive decline in elderly adults (6). Additional investigation is needed to examine the role of dietary quality measured with the HEI-20005 in the preservation of cognitive function. To our knowledge, no study has shown associations between the HEI-2005 and cognitive function with participants aged <65 years.
Relative to non-Hispanic white adults, higher incidence of dementia has been shown in Latinos (11). Food insecurity has been found to be associated with increased risk for cognitive impairment in Puerto Rican adults (12). Puerto Rican adults consume foods in differing frequency and portion size compared with general US population (13). To identify a favorable dietary pattern for cognition could be particularly important for this population. We, therefore, aimed to investigate adherence to the Mediterranean diet and to the HEI-2005, and their associations with cognitive function in a sample of middle-aged and older Puerto Rican adults from the Greater Boston area, Massachusetts.
METHODS
Study sample
The Boston Puerto Rican Health Study is an ongoing study to investigate the sociological, environmental and genetic risk factors for chronic diseases, cognitive impairment and reduced quality of life. The design of the study has been described in detail previously (14). Participants were not included if they had Mini Mental State Examination (MMSE) score ≤10, an indicator of severe cognitive impairment (15) which may affect the quality of their response to questionnaires. A total of 1,500 Puerto Rican adults, aged 45–75 years, completed the baseline visit. Of those, individuals with implausible energy intake (<600 kcal/d or >4800 kcal/d) were excluded from the analysis, as were those with incomplete cognitive tests or blood analyses. Cleaned and complete data were available for 1,269 participants for this analysis. The Institutional Review Board at Tufts Medical Center approved the study protocol, and all participants provided written informed consent.
Development of MeD score and HEI-2005 score
Dietary intake was assessed for the last 12 months with a validated semi-quantitative food frequency questionnaire (FFQ) during home interview (16). Ounce or cup equivalents of each food per day were calculated using the MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003-2004 (17). Food equivalents were then summed within each food group. Similar to the work of Scarmeas et al. (4) and Feart et al. (2), the MeD score was composed following the procedure described by Trichopoulou et al. (1). Food equivalents for each of nine food groups were adjusted for total energy intake using the regression residual method before further analysis (18). A score for adherence to the MeD was created by adding points from the nine food categories, resulting in a possible range of 0 to 9 (Supplemental text). The HEI-2005 score was calculated using an energy density approach according to procedures from the USDA Center for Nutrition Policy and Promotion (8). The HEI-2005 score is a sum of scores from 12 individual components, with maximum score 100 (Supplemental text).
Assessment of cognitive function
A battery of seven neuropsychological tests, with the MMSE as a measure of global cognitive function, was conducted with each participant in their home by a qualified research assistant (supplemental text), before the FFQ was administrated, on the same day (12). Higher scores on each of these exams reflect better cognitive function. To minimize the potential of redundancy in the neuropsychological tests and to reduce the possibility of type I error due to multiple testing (19), a factor analysis was performed with scores from the seven neuropsychological tests (12). Three factors were identified with Kaiser’s criterion (eigenvalue >1) (20). Orthogonal varimax rotation was then conducted to maximize interpretability. The three cognitive function factors were uncorrelated and were interpreted as executive function, memory, and attention, respectively (Supplemental Table 1).
Cognitive impairment was defined as MMSE score <21 for those with less than high school education, <23 for those with high school completion, and <24 for those with at least some college education (14).
Statistical analyses
Participants were placed in quintile categories by scores of MeD and HEI-2005, respectively. Cognitive performance scores for each category of the MeD adherence score were calculated after multivariable adjustment using general linear models. Model 1 was adjusted for age (years), sex, and educational attainment (≤ primary school, secondary school, high school, or ≥ some college). Model 2 was further adjusted for household income below the poverty threshold (yes/no), acculturation score, smoking status (never, past or current smoker), physical activity score, supplement use (yes/no), taking more than 5 types of medications within the past 12 months (yes/no), body mass index (kg/m2), hypertension (yes/no), diabetes (yes/no), total cholesterol (mg/dL), high-density lipoprotein cholesterol (mg/dL) and triglycerides (mg/dL). Original continuous dietary scores were used for trend tests. Finally, possible interactions between age (in three categories: 45-54, 55-64, 65-75 years) and adherence to the MeD were tested by additionally including the product of age and diet score in the models for cognitive function outcomes. In the current study, MMSE scores were treated as the primary outcome, because the MMSE measures global cognitive function. Secondary analyses examined associations between the diet quality scores and the three derived cognitive function factors. Logistic regression models were used to calculate odds ratios for cognitive impairment per point change of continuous MeD scores and for the upper four quintiles of MeD scores, when compared with first quintile.
All analyses were repeated to estimate associations between HEI-2005 score and cognitive performance. All statistical analyses were conducted with SAS version 9.2 (SAS Institute Inc, Cary, NC). A value of P <0.05 (two-sided) was considered statistically significant.
RESULTS AND DISCUSSION
The MeD score and cognitive function
In this population-based cross-sectional sample of middle-aged and older Puerto Rican adults, the mean age was 57.3 years (SD 7.6), and the mean MeD score was 4.37 (SD 1.61) with a range of 0 to 9; 45.0% had a score of 4 or 5, and 0.2%, 3.0%, 2.7% and 0.2% had scores of 0, 1, 8, and 9, respectively. The average MeD score in our study was similar to the mean MeD score (4.36, SD: 1.67) in two cohorts of the Washington-Heights-Inwood Columbia Aging Project in New York, NY (3).
Higher adherence to the MeD was associated with better global cognitive function, as measured by higher MMSE score, after adjusting for age, sex and educational attainment (Table 1). These associations remained significant after further adjustment for confounders. Each MeD score point was associated with a 0.14 point higher MMSE score (β = 0.14, SE = 0.05, P = 0.012). This was inversely comparable to a difference in MMSE score associated with 3-years of age (β = −0.14, SE = 0.04, P <0.001) in model 2. MeD adherence was also significantly associated with the attention factor (model 1), but significance was attenuated with full adjustment. MeD score was not associated with executive function or memory factors.
Table 1.
Cognitive performance by quintile of Mediterranean diet score
| Mediterranean diet score |
|||||||
|---|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | Continuous | ||
| (0–2) | (3) | (4) | (5) | (6–9) | |||
| n | 159 | 232 | 278 | 287 | 313 | ||
| Score | 1.74 (0.47)a | 3 (0)a | 4 (0)a | 5 (0)a | 6.48 (0.73)a | ||
| Age (years)b | 56.1 (7.5)a | 57. 3 (7.5)a | 57.5 (7.5)a | 57.4 (7.8)a | 57.7 (7.6)a | ||
|
| |||||||
| Mean (SE) c | β (SE) c | P for trend d | |||||
|
| |||||||
| MMSEe | |||||||
| Model 1f | 23.1 (0.2) | 23.3 (0.2) | 23.6 (0.2) | 23.8 (0.2) | 23.9 (0.2) | 0.19 (0.05) | <0.001 |
| Model 2g | 23.0 (0.3) | 23.3 (0.2) | 23.5 (0.2) | 23.7 (0.2) | 23.7 (0.2) | 0.14 (0.05) | 0.012 |
| Executive function | |||||||
| Model 1f | −0.06 (0.07) | −0.004 (0.06) | 0.002 (0.06) | −0.08 (0.06) | 0.05 (0.05) | 0.02 (0.02) | 0.34 |
| Model 2g | −0.14 (0.08) | −0.03 (0.07) | −0.08 (0.06) | −0.11 (0.06) | −0.02 (0.06) | 0.01 (0.02) | 0.52 |
| Memory | |||||||
| Model 1f | −0.15 (0.08) | −0.16 (0.07) | 0.08 (0.07) | −0.08 (0.07) | −0.06 (0.06) | 0.02 (0.02) | 0.23 |
| Model 2g | −0.13 (0.09) | −0.17 (0.07) | 0.12 (0.07) | −0.07 (0.07) | −0.07 (0.07) | 0.02 (0.02) | 0.39 |
| Attention | |||||||
| Model 1f | −0.03 (0.08) | 0.03 (0.07) | 0.17 (0.06) | 0.09 (0.06) | 0.19 (0.06) | 0.04 (0.02) | 0.017 |
| Model 2g | −0.08 (0.09) | 0.02 (0.07) | 0.15 (0.07) | 0.06 (0.07) | 0.13 (0.07) | 0.03 (0.02) | 0.067 |
Mean (SD).
P = 0.30 for age differences across quintiles of Mediterranean diet score (PROC GLM in SAS 9.2).
Adjusted means (standard error, SE) by quintile category, and β coefficients (SE) for linear scores were calculated using general linear models (PROC GLM in SAS 9.2) after adjustment for covariates.
P values for trend were calculated using the continuous diet score in general linear models (PROC GLM in SAS 9.2).
Mini Mental State Examination (MMSE) score.
Model 1, adjusted for age (years), sex, and educational attainment (≤ primary school, secondary school, high school, or ≥ some college).
Model 2, further adjusted for household income below threshold (yes/no), acculturation score (continuous), smoking status (never, past smoker or current smoker), physical activity score (continuous), supplement use (yes/no), taking more than 5 types of medications within the last 12 months (yes/no), body mass index (kg/m2), hypertension (yes/no), diabetes (yes/no), total cholesterol (mg/dL), high-density lipoprotein cholesterol (mg/dL) and triglycerides (mg/dL).
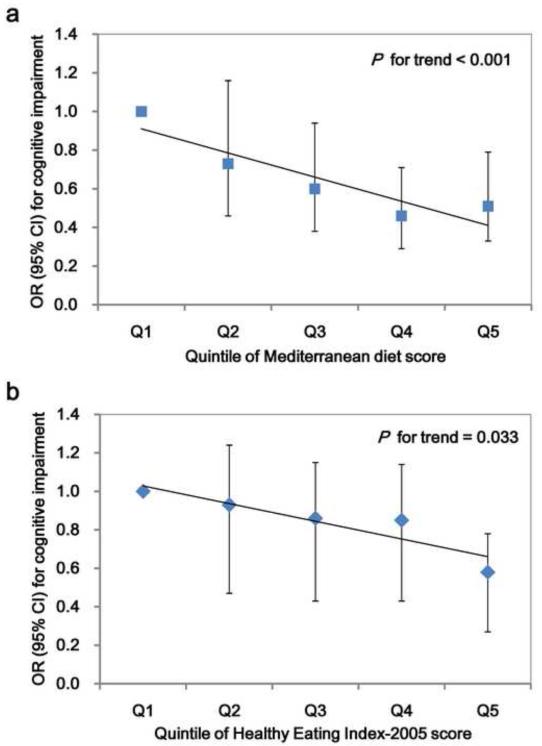
Higher adherence to the MeD was also associated with lower likelihood of cognitive impairment, defined by MMSE cutoff points, after adjustment for potential confounders (Figure 1a). Those in the highest (vs. lowest) quintile of MeD score had about 50% lower odds (odds ratio [OR]: 0.51, 95% confidence interval [CI]: 0.33-0.79) of cognitive impairment. Using continuous MeD score as the independent variable, each additional point of MeD score was associated with 13% lower odds of cognitive impairment after multivariable adjustment (OR: 0.87, 95% CI: 0.80 - 0.94, P trend <0.001).
Figure 1. Odds of cognitive impairment by quintile category of diet score.
Cognitive impairment was defined as: Mini Mental State Examination score <21 for those with less than high school education, <23 for those with high school completion, or <24 for those with at least some college education (14). Logistic regression was used to calculate odds ratios (OR) and 95% confidence interval (CI) for cognitive impairment with PROC LOGISTIC in SAS 9.2, adjusting for age (years), sex, educational attainment (≤ primary school, secondary school, high school, or ≥ some college), household income below threshold (yes/no), acculturation score (continuous), smoking status (never, past smoker or current smoker), physical activity score (continuous), supplement use (yes/no), taking more than 5 types of medications within the last 12 months (yes/no), body mass index (kg/m2), hypertension (yes/no), diabetes (yes/no), total cholesterol (mg/dL), high-density lipoprotein cholesterol (mg/dL), and triglycerides (mg/dL). P for trend was the P value for continuous dietary scores.
Analyses were repeated in three subgroups, stratified by age (45–54, 55–64, and >64 years), to explore whether associations were limited to groups within specific age ranges. In general, similar positive associations between MeD scores and MMSE were observed across each of the three age groups (P for interaction >0.35) after multivariable adjustment (Supplemental Table 2).
The positive association between adherence to the MeD and MMSE score seen in the current study is consistent with findings from previous reports in diverse populations (2, 3, 5, 6). In the Three-city cohort from France, with a total of 1,410 adults aged ≥65 years, higher adherence to the MeD score was associated with less MMSE decline over time (2). Greater adherence to the MeD score was also associated with lower risk of developing mild cognitive impairment (3), and with reduced risk of mild cognitive impairment conversion to Alzheimer’s disease (5) in the Washington-Heights-Inwood Columbia Aging Project, with recruited participants aged ≥65 years at baseline (11). Higher MeD score, measured in a different way, was also associated with slower rates of cognitive decline in the Chicago Health and Aging Project (CHAP) (6). Importantly, the association between adherence to MeD and MMSE score was also observed among individuals aged <65 years in the current study.
In agreement with previous studies (2, 3), the association between MeD adherence and cognitive function remained unchanged after adjustment for several vascular risk factors, suggesting that the benefits of MeD may be, in part, through non-vascular mechanisms. The MeD usually captures a composition of high intakes of monounsaturated fatty acids, B vitamins, and antioxidants such as complex phenols, vitamins C and E, and carotenoids (2). Higher intake of monounsaturated fatty acids has been associated with better cognitive function or lower risk for cognitive decline (21). B vitamins including folate, vitamins B-6 and B-12 have also been related to cognitive performance (22). In addition, cumulative evidence suggests that oxidative damage contributes to the pathogenesis of mild cognitive impairment and Alzheimer disease (23, 24), and that antioxidants in fruit, vegetables and wine may improve the antioxidative defense system (25). Further, greater adherence to the MeD has been associated with lower concentrations of several inflammatory factors including C-reactive protein, interleukin 6 and white blood cell counts (26-28). Available data suggest that inflammation is involved in the pathogenesis of cognitive impairment and Alzheimer’s disease (24). Therefore, the MeD may protect cognitive function through effects on inflammation and oxidative stress.
The HEI-2005 score and cognitive function
The question remains as to whether it is the Mediterranean diet per se or a healthy diet in general that is protective. Importantly, in the present study, adherence to the USDA Dietary Guidelines for Americans 2005 (measured by the HEI-2005) was also associated with MMSE score (Table 2), and these associations remained after multivariable adjustment. Each 10 points of HEI-2005 score (β = 0.25, SE = 0.10, P = 0.011) was inversely similar to 5 years of age (β = −0.25, SE = 0.07, P <0.001) on MMSE scores, after multivariable adjustment. As with the MeD, the HEI-2005 was not significantly associated with executive function. In contrast, however, the HEI-2005 was associated with memory (rather than attention) in the initial model, but this was attenuated after further adjustment for covariates.
Table 2.
Cognitive performance by quintile of Healthy Eating Index-2005 score
| Healthy Eating Index-2005 score |
|||||||
|---|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | Continuous | ||
| (<64.5) | (64.5–70.5) | (70.6–75.5) | (75.6–80.0) | (>80.0) | |||
| n | 253 | 254 | 254 | 254 | 254 | ||
| Score | 57.4 (5.1)a | 67.2 (1.8)a | 72.6 (1.4)a | 77.3 (1.3)a | 83.9 (3.3)a | ||
| Age (year) b | 55.1 (7.0)a | 56.4 (7.5)a | 56.5 (7.6)a | 59.1 (7.6)*** a | 59.3 (7.4)*** a | ||
|
| |||||||
| Mean (SE) c | β (SE) c d | P for trend e | |||||
|
| |||||||
| MMSEf | |||||||
| Model 1g | 23.4 (0.2) | 23.3 (0.2) | 23.6 (0.2) | 23.7 (0.2) | 24.2 (0.2) | 0.27 (0.09) | 0.004 |
| Model 2h | 23.4 (0.2) | 23.2 (0.2) | 23.4 (0.2) | 23.6 (0.2) | 24.1 (0.3) | 0.25 (0.10) | 0.011 |
| Executive function | |||||||
| Model 1g | −0.04 (0.06) | −0.05 (0.06) | −0.03 (0.06) | 0.02 (0.06) | 0.04 (0.06) | 0.03 (0.03) | 0.27 |
| Model 2h | −0.09 (0.06) | −0.14 (0.06) | −0.08 (0.06) | −0.04 (0.06) | 0.001 (0.07) | 0.04 (0.03) | 0.23 |
| Memory | |||||||
| Model 1g | −0.15 (0.07) | −0.08 (0.07) | −0.04 (0.07) | −0.05 (0.07) | 0.01 (0.07) | 0.07 (0.03) | 0.025 |
| Model 2h | −0.11 (0.07) | −0.13 (0.07) | −0.03 (0.07) | −0.02 (0.07) | −0.002 (0.08) | 0.06 (0.03) | 0.059 |
| Attention | |||||||
| Model 1g | 0.13 (0.06) | −0.01 (0.06) | 0.08 (0.07) | 0.13 (0.07) | 0.22 (0.07) | 0.03 (0.03) | 0.32 |
| Model 2h | 0.05 (0.07) | −0.04 (0.07) | 0.03 (0.07) | 0.12 (0.07) | 0.18 (0.08) | 0.05 (0.03) | 0.10 |
Mean (SD).
P < 0.001 for age differences across quintiles of Healthy Eating Index-2005 score (PROC GLM in SAS 9.2).
Adjusted means (standard error, SE) by quintile category, and β coefficients (SE) for linear scores were calculated using general linear models (PROC GLM in SAS 9.2) after adjustment for covariates.
β coefficients per 10 points of Healthy Eating Index-2005.
P values for trend were calculated using continuous Healthy Eating Index-2005 score (PROC GLM in SAS 9.2).
Mini Mental State Examination (MMSE) score.
Model 1, adjusted for age (years), sex, and educational attainment (≤ primary school, secondary school, high school, or ≥ some college).
Model 2, further adjusted for household income below threshold (yes/no), acculturation score (continuous), smoking status (never, past smoker or current smoker), physical activity score (continuous), supplement use (yes/no), taking more than 5 types of medications within the last 12 months (yes/no), body mass index (kg/m2), hypertension (yes/no), diabetes (yes/no), total cholesterol (mg/dL), high-density lipoprotein cholesterol (mg/dL) and triglycerides (mg/dL).
P <0.05
P <0.001 compared with the lowest category with Tukey’s adjustment for multiple comparisons.
Those in the highest (vs. lowest) quartile of the HEI-2005 score had about 40% lower odds (OR: 0.58, 95% CI: 0.38 - 0.89) of cognitive impairment (Figure 1b). Similarly, each 10 HEI-2005 point increase in score was associated with 14% lower odds of cognitive impairment (OR: 0.86, 95% CI: 0.74 - 0.99, P trend = 0.033). In general, positive associations between the HEI-2005 and MMSE scores were observed across the three age groups (45–54, 55–64, and >64 years; P for interaction >0.35) after multivariable adjustment (Supplemental Table 2).
In contrast to these findings, the HEI-2005 score was not associated with cognitive function in the CHAP study (6). There are several plausible explanations for this inconsistency. The FFQ used here has many more food items compared with the one used in the CHAP (246 vs. 139 food items). Greater detail on the FFQ may improve the calculation of the HEI-2005 score, which was originally designed from 24-hour dietary recalls. Further, the participants in the present study were much younger than those in the CHAP (mean age, 75.4 years), and the HEI-2005 score was higher in our study (72.8 for women and 68.9 for men) than in the CHAP (61.6 for women and 60.5 for men). All these features in our study may increase power to detect potential associations between HEI-2005 scores and cognitive function. Indeed, Wengreen et al. reported that adherence to a diet with higher quality, reflected by higher recommended food score, was associated with lower 11 year cognitive decline among elderly men and women aged ≥65 years at baseline (29). More studies with prospective designs are warranted to examine associations between adherence to the USDA Dietary Guidelines for Americans 2005 and cognitive function.
Strengths and limitations
Because of the cross-sectional nature of this analysis, a causal direction between MeD score or HEI-2005 score and cognitive function cannot be assumed. However, significant dose-response associations were observed between these diet quality scores with cognitive measures, which are unlikely to be due to reverse causation, as it is unlikely that those with more cognitive impairment would choose lower quality of overall diet in a dose-response manner. Strengths of our study include a population-based design, a high proportion of middle-age, as well as older, participants, and careful control for confounders, although residual confounding may still exist.
CONCLUSIONS
Diets with higher quality, measured either by the MeD score or HEI-2005 score, were associated with greater cognitive function and lower likelihood of cognitive impairment in middle-aged and older Puerto Rican adults. Further studies, including intervention trials, will be useful to determine whether the whole-diet approach is effective in slowing the progress of cognitive impairment and delaying onset of dementia in this and other ethnic groups.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Xingwang Ye, Institute for Nutritional Sciences Shanghai Institute for Biological Sciences Chinese Academy of Sciences Taiyuan Road 294, Shanghai, China, 200031 TEL: +86-21-54920902 FAX: +86-21-54920291 xwye@sibs.ac.cnAt time research was finished: Postdoctoral Associate Department of Health Sciences Northeastern University 312 Robinson Hall 360 Huntington Avenue Boston, MA 02115.
Tammy Scott, Department of Psychiatry Tufts Medical Center Boston, MA 02111 Tel: 617-636-3751; tscott@tuftsmedicalcenter.org.
Xiang Gao, Department of Nutrition, Harvard University School of Public Health The Channing Laboratory, Department of Medicine, Brigham and Women’s Hospital, Boston, MA 02115 Tel: 617-432-5080; Fax: 617-432-2435; hpgao@channing.harvard.edu.
Janice E. Maras, Department of Health Sciences Northeastern University 208 Robinson Hall 360 Huntington Avenue Boston, MA 02115 Tel: 617- 373-3665, Fax: 617-373-2968, j.maras@neu.edu
Peter J. Bakun, Dietary Assessment and Epidemiology Research Program Jean Mayer USDA Human Nutrition Research Center on Aging Tufts University Boston, MA, 02111 Tel: 617-556-3354, Fax: 617-556-3344, peter.bakun@tufts.edu
Katherine L. Tucker, Department of Health Sciences 316 Robinson Hall Northeastern University 360 Huntington Avenue Boston, MA 02115 Phone: 617-373-7952, Fax: 617-373-2968, kl.tucker@neu.edu.
REFERENCES
- 1.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 2.Feart C, Samieri C, Rondeau V, et al. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302(6):638–648. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66(2):216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer’s disease. Ann Neurol. 2006;59(6):912–921. doi: 10.1002/ana.20854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scarmeas N, Stern Y, Mayeux R, Luchsinger JA. Mediterranean diet, Alzheimer disease, and vascular mediation. Arch Neurol. 2006;63(12):1709–1717. doi: 10.1001/archneur.63.12.noc60109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, Morris MC. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011;93(3):601–607. doi: 10.3945/ajcn.110.007369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kesse-Guyot E, Andreeva VA, Jeandel C, Ferry M, Hercberg S, Galan P. A healthy dietary pattern at midlife is associated with subsequent cognitive performance. J Nutr. 2012;142(5):909–915. doi: 10.3945/jn.111.156257. [DOI] [PubMed] [Google Scholar]
- 8.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Shah BS, Freeland-Graves JH, Cahill JM, Lu H, Graves GR. Diet quality as measured by the healthy eating index and the association with lipid profile in low-income women in early postpartum. J Am Diet Assoc. 2010;110(2):274–279. doi: 10.1016/j.jada.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 10.Gao SK, Beresford SA, Frank LL, Schreiner PJ, Burke GL, Fitzpatrick AL. Modifications to the Healthy Eating Index and its ability to predict obesity: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2008;88(1):64–69. doi: 10.1093/ajcn/88.1.64. [DOI] [PubMed] [Google Scholar]
- 11.Tang MX, Cross P, Andrews H, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56(1):49–56. doi: 10.1212/wnl.56.1.49. [DOI] [PubMed] [Google Scholar]
- 12.Gao X, Scott T, Falcon LM, Wilde PE, Tucker KL. Food insecurity and cognitive function in Puerto Rican adults. Am J Clin Nutr. 2009;89(4):1197–1203. doi: 10.3945/ajcn.2008.26941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tucker KL, Bianchi LA, Maras J, Bermudez OI. Adaptation of a food frequency questionnaire to assess diets of Puerto Rican and non-Hispanic adults. Am J Epidemiol. 1998;148(5):507–518. doi: 10.1093/oxfordjournals.aje.a009676. [DOI] [PubMed] [Google Scholar]
- 14.Tucker K, Mattei J, Noel S, et al. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health. 2010;10(1):107. doi: 10.1186/1471-2458-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perneczky R, Wagenpfeil S, Komossa K, Grimmer T, Diehl J, Kurz A. Mapping scores onto stages: mini-mental state examination and clinical dementia rating. Am J Geriatr Psychiatry. 2006;14(2):139–144. doi: 10.1097/01.JGP.0000192478.82189.a8. [DOI] [PubMed] [Google Scholar]
- 16.Ye X, Maras JE, Bakun PJ, Tucker KL. Dietary intake of vitamin b-6, plasma pyridoxal 5′-phosphate and homocysteine in Puerto Rican adults. J Am Diet Assoc. 2010;11(110):1160–1168. doi: 10.1016/j.jada.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bowman SA, Friday JE, Moshfegh A. MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003-2004 [Online] Food Surveys Research Group. Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture; Beltsville, MD: [Accessed August 25, 2010]. 2008. Web site: http://www.ars.usda.gov/ba/bhnrc/fsrg. [Google Scholar]
- 18.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4 Suppl):1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. discussion 1229S-1231S. [DOI] [PubMed] [Google Scholar]
- 19.Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 20.Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141–151. [Google Scholar]
- 21.Solfrizzi V, Panza F, Torres F, et al. High monounsaturated fatty acids intake protects against age-related cognitive decline. Neurology. 1999;52(8):1563–1569. doi: 10.1212/wnl.52.8.1563. [DOI] [PubMed] [Google Scholar]
- 22.Tucker KL, Qiao N, Scott T, Rosenberg I, Spiro A., 3rd High homocysteine and low B vitamins predict cognitive decline in aging men: the Veterans Affairs Normative Aging Study. Am J Clin Nutr. 2005;82(3):627–635. doi: 10.1093/ajcn.82.3.627. [DOI] [PubMed] [Google Scholar]
- 23.Pratico D. Alzheimer’s disease and oxygen radicals: new insights. Biochem Pharmacol. 2002;63(4):563–567. doi: 10.1016/s0006-2952(01)00919-4. [DOI] [PubMed] [Google Scholar]
- 24.Galasko D, Montine TJ. Biomarkers of oxidative damage and inflammation in Alzheimer’s disease. Biomark Med. 2010;4(1):27–36. doi: 10.2217/bmm.09.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joseph JA, Shukitt-Hale B, Willis LM. Grape juice, berries, and walnuts affect brain aging and behavior. J Nutr. 2009;139(9):1813S–1817. doi: 10.3945/jn.109.108266. [DOI] [PubMed] [Google Scholar]
- 26.Esposito K, Ciotola M, Giugliano D. Mediterranean diet, endothelial function and vascular inflammatory markers. Public Health Nutr. 2006;9(8A):1073–1076. doi: 10.1017/S1368980007668529. [DOI] [PubMed] [Google Scholar]
- 27.Dai J, Miller AH, Bremner JD, et al. Adherence to the mediterranean diet is inversely associated with circulating interleukin-6 among middle-aged men: a twin study. Circulation. 2008;117(2):169–175. doi: 10.1161/CIRCULATIONAHA.107.710699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dedoussis GV, Kanoni S, Mariani E, et al. Mediterranean diet and plasma concentration of inflammatory markers in old and very old subjects in the ZINCAGE population study. Clin Chem Lab Med. 2008;46(7):990–996. doi: 10.1515/CCLM.2008.191. [DOI] [PubMed] [Google Scholar]
- 29.Wengreen HJ, Neilson C, Munger R, Corcoran C. Diet quality is associated with better cognitive test performance among aging men and women. J Nutr. 2009;139(10):1944–1949. doi: 10.3945/jn.109.106427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.