Abstract
The optimal method of fixation for primary total hip replacements (THR), particularly fixation with or without the use of cement is still controversial. In a systematic review and metaanalysis of all randomized controlled trials comparing cemented versus uncemented THRS available in the published literature, we found that there is no significant difference between cemented and uncemented THRs in terms of implant survival as measured by the revision rate. Better short-term clinical outcome, particularly an improved pain score can be obtained with cemented fixation. However, the results are unclear for the long-term clinical and functional outcome between the two groups. No difference was evident in the mortality and the post operative complication rate. On the other hand, the radiographic findings were variable and do not seem to correlate with clinical findings as differences in the surgical technique and prosthesis design might be associated with the incidence of osteolysis. We concluded in our review that cemented THR is similar if not superior to uncemented THR, and provides better short term clinical outcomes. Further research, improved methodology and longer follow up are necessary to better define specific subgroups of patients in whom the relative benefits of cemented and uncemented implant fixation can be clearly demonstrated.
Key words: cemented, uncemented, total hip arthroplasty, meta analysis.
Introduction
Total hip replacement (THR) is one of the most successful and cost-effective of surgical procedures with the primary goals of pain relief and restoration of function. Since THRs were introduced, there has been steady improvement in the technology associated with it, leading to better functional outcome and implant survivorship.1 The success of THRs and the increasing frequency of its use is largely due to the development of the cemented low-friction arthroplasty with its high survival rate.2,3 However, the outcomes of other cemented THR prostheses were poor with high and early loosening rate, primarily due to the implant designs and cementing techniques in many cases. The cement itself was considered a cause of loosening leading the term cement disease. The uncemented THR was developed to avoid these problems; however the early designs had similarly poor outcomes. The development of circumferentially coated uncemented implants which allow bone to grow into or onto the prosthesis has led to an improved implant survival rate and supported their growing use, despite higher costs.4–6 Published studies comparing cemented to uncemented THRs are rare. The majority of these are retrospective, non-randomised comparisons,7,8 or comparison in the same patient with bilateral THRs.9,10 Various randomized controlled trials (RCTs) have been designed to compare the clinical and radiological outcomes of cemented versus uncemented fixation.11,12 Thus far no one study has been able to draw a decisive conclusion because of inherent limitations. Furthermore, there are no horizontal or longitudinal comparisons of the published RCTs in the literature. Our study aims to determine whether the contemporary hip surgeons should abandon the proven dependability of cemented fixation for the emerging technology of cementless fixation.
Objectives
This review aims to systematically evaluate all RCTs comparing cemented versus uncemented fixation of THRs, with no restriction to the patients age.
Information sources
A comprehensive search across multiple Databases was performed for studies published in English and other languages. Databases included Medline, BIOSYS, Embase, Web of Science, CAB Health, Cumulative Index to Nursing and Allied Health Literature, Science Citation Index/ Current Contents and the Cochrane Library (Issue 4, 2010). The reference list of each study was reviewed to find additional relevant studies. Experts in the field and manufacturers of implants were contacted to identify further studies. The so called grey literature was identified using the Inside Database of the British Library, the System for Information on Grey Literature in Europe, and relevant abstract bands. The studies not published because of negative results or other reasons were identified from online trial registers (UK National Research Register of ongoing health research, information on clinical trials sponsored by the NIH and The International Register of Clinical Trials Registers).
Eligibility criteria
Types of studies
We included reports of only RCTs. In the case of multiple publications of a trial, we included the first published article. Exceptions were made if a more recent publication corroborates the results of a longer follow up or examined a different outcome or both.
Types of participants
Humans aged 18 years or older who underwent a primary THR were eligible.
Types of interventions and comparison
The intervention of interest is the implantation of primary cemented THRs compared to primary uncemented THRs.
Types of outcome measures
The primary outcome is failure of the primary procedure, measured objectively by the revision rate due to aseptic loosening of either the cup or the stem. Secondary outcomes included radiological signs of loosening or osteolysis, mortality, complications, pain score, functional scores mainly Harris Hip Score (HHS) and Merle-D'Aubigne score, follow up duration and radiostereometric analysis (RSA).
Selection criteria
Inclusion criteria were established a priori to minimize selection bias. The objective was to identify all RCTs with comparison of cemented versus uncemented fixation of THRs. Studies that included arthroplasty for trauma, tumor cases, animal studies, studies containing previously published data or poorly randomized trials were excluded.
Data collection and analysis
Initial screening of articles was performed by primary author. Two reviewers then independently assessed each of the studies for eligibility for inclusion. Any disagreements were resolved by consensus.
Statistical analysis
Meta-analyses were computed using Review Manager 5 from the Cochrane collaboration. The impact of sample size was addressed by estimating a weighting factor for each study, and assigning larger effect-weights in studies with bigger samples.
Effect sizes measured were relative risk (RR) for categorical variables and mean difference (MD) for continuous variables. Outcome variables that were reported in a comparable manner among at least three RCTs were included in meta-analyses. Pooled estimation of the RRs and MDs of each RCT and the corresponding 95% Confidence Intervals (CI) were calculated by the random effect model and heterogeneity was described by the I2 statistic. We predefined significant heterogeneity as I2>50%.
An estimate of the potential publication bias was carried out by funnel plot. An asymmetric plot suggested a possible publication bias.
Subgroup analyses for primary outcomes (revision rate, pain and HHS scores) were performed analyzing separately the RCTs with less than 5 year follow up (short term follow-up) and those with more than 5 years (long term follow-up). P value less than 0.05 was considered as statistically significant.
Reporting was carried out in line with PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.13
Results
Study selection
Of the 107 citations identified through literature searches (Figure 1), 16 were assessed for eligibility.12,14–28 Seven studies were excluded, five were reporting previously published data,14,16,18–20 one was not a proper RCT and one was RCT comparing cemented with another cemented implant.15,17 Nine RCTs met all of our inclusion criteria.12,21–28
Figure 1.
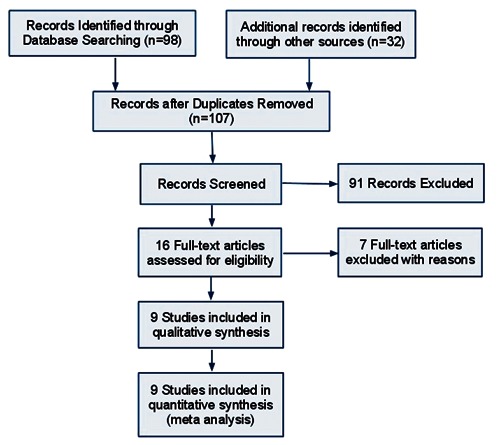
Flow chart of selection process.
A total of 930 THRs were performed in 778 patients in these studies: 330 patients were males and 448 were females; 459 had cemented and 471 had cementless prosthesis. The mean age was 60.5 years. The average post operative follow up was 4.3 (range 2–8) years (Table 1). Mortality and post-operative complications at their last follow up are shown in Table 2 and Table 3 respectively. Two RCTs compared cemented and uncemented sockets, 4 compared cemented and uncemented femoral stems while the rest compared both components. The implant types reported by these studies are listed in Table 4.
Table 1. Patients characteristics of in both groups.
| Study ID | Mean age (years) | Gender (male/female) | Matched variables between cemented and uncemented groups | Follow up (years) |
|---|---|---|---|---|
| P. McCombe 2004 | 67.3 | 76/86 | Age, follow-up, diagnosis | 6.5 |
| Laupacis 2002 | 64 | 33/31 | Age, sex, follow-up, weight, diagnosis | 6.3 |
| S. P. GODSIFF 1992 | 64.5 | 29/29 | Age, follow-up, diagnosis | 2 |
| Håkan Ström 2006 | 54 | 15/30 | Age, follow-up, weight, diagnosis | 8 |
| Reigstad 1993 | 64 | 32/88 | Age, sex, follow-up, weight, diagnosis, right/left ratio, clinical and radiographic assessments of the arthrosis | 5 |
| Wykman et al. 1991 | 66.2 | 57/93 | Age, follow-up, weight | 5 |
| Onsten & Carlsson 1994 | 60.2 | 41/40 | Age, sex, follow-up, weight, diagnosis, right/left ratio | 2 |
| J Karrholm 1994 | 53 | 31/30 | Age, sex, weight, the roentgenographic quality of the bone; and the reason for the operation | 2 |
| Grant 2005 | 51.6 | 16/21 | Age | 2 |
Table 2. Post operative mortality.
| Study | Cemented group | Total | Cementless group | Total |
|---|---|---|---|---|
| P. McCombe 2004 | 19 | 63 | 16 | 52 |
| Laupacis 2002 | 18 | 124 | 17 | 126 |
| S. P. GODSIFF 1992 | 0 | 30 | 0 | 28 |
| Håkan Ström 2006 | 0 | 23 | 0 | 22 |
| Reigstad 1993 | 5 | 60 | 4 | 60 |
| Wykman et al. 1991 | 4 | 90 | 4 | 90 |
| Onsten & Carlsson 1994 | 4 | 30 | 3 | 30 |
| J. Karrholm 1994 | NR | 20 | NR | 44 |
| Grant 2005 | 0 | 19 | 0 | 19 |
| Total | 50 | 44 |
NR, not reported.
Table 3. Summary of post operative complications.
| Study | Complications |
|---|---|
| P. McCombe 2004 thought to | Four acetabular prostheses were revised for recurrent dislocation; these were all Duraloc cups and the dislocations were have been caused by the prominent 10° lip |
| Laupacis 2002 | NR |
| S. P. GODSIFF 1992 | One patient in the cemented group suffered a postoperative pulmonary embolus and subsequent cardiac arrest. She was successfully resuscitated, made a full recovery, and went on to have an excellent result at two years |
| Håkan Ström 2006 | NR |
| Reigstad 1993 | No serious operative or postoperative complications occurred |
| Wykman et al. 1991 | One patient was reoperated at 2 months with a Girdlestone hip because of infection. In the Charnley group 2 patients had their prostheses removed because of deep infection |
| Onsten & Carlsson 1994 | NR |
| J Karrholm 1994 | NR |
| Grant 2005 | One patient had a superficial wound infection, and one a weak abductor function with a Trendelenburg gait |
NR: not reported
Table 4. Implants characteristics.
| Study | Location | Compared components | Non compared components | |
|---|---|---|---|---|
| Cemented implant | Cementless implant | |||
| P. McCombe 2004 | Australia | Polyethylene Exeter cup | Duraloc cup | Cemented double-taper stem (Exeter; Stryker Australia) |
| Laupacis 2002 | Canada | Mallory-Head total hip prosthesis | Mallory-Head total hip prosthesis | Hips with both cemented components were compared to hips with both uncemented components |
| S. P. GODSIFF 1992 | UK | Ring UPM stem | Ring UPM stem | The acetabular components were all implanted without cement |
| Håkan Ström 2006 | Sweden | Bimetric stem | Cone stem | All patients in the randomized study received a cemented Cenator (Corin, Cirencester, UK) acetabular component |
| Reigstad 1993 | Norway | (Landos Titane) total hip prosthesis | (ZweymOller/Endler cup) total hip prosthesis | Hips with both cemented components were compared to hips with both uncemented components |
| Wykman et al. 1991 | Sweden | Charnley total hip prosthesis | Honart Patel-Garches (press fit) | Hips with both cemented components were compared to hips with both uncemented components |
| Onsten & Carlsson 1994 | Sweden | Charnley socket | Harris-Galante socket | Charnley femoral component (head 22 mm) was cemented in all cases |
| J Karrholm 1994 | Sweden | Tifit straight-stem femonal prosthesis of the same basic design made of titaniumaluminum-vanadium alloy implant total hip prosthesis | Tifit straight-stem femonal prosthesis of the same basic design made of titaniumaluminum-vanadium alloy implant total hip prosthesis | A press-fit acetabular cup with titanium-fiber mesh was inserted without cement and was additionally fixed with screws (Harris-Galante I or II; Zimmen, Warsaw, Indiana) in all of the hips |
| Grant 2005 | Norway | Elite Plus stem implant total hip prosthesis | Custom made Unique stem implant total hip prosthesis | Uncemented Duraloc (DePuy) acetabular component in all patients except one |
Results of meta-analyses
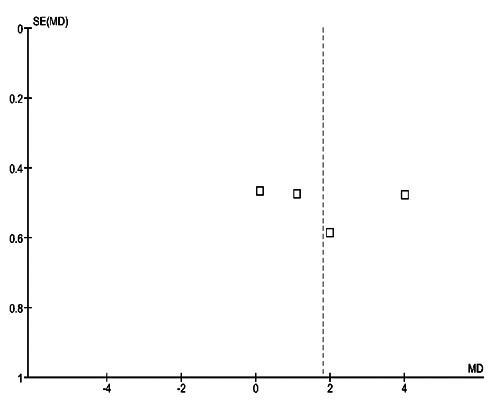
The revision rates were reported in 6 RCTs (719 patients). The cemented THRs had a higher but statistically non significant revision rate (RR=1.44; 95% CI, 0.88 to 2.35; P=0.14) with nonsignificant heterogeneity (I2=3%) for this outcome (Table 5, Figure 2). Subgroup analysis (Figure 3) showed no change in results for RCTs reporting a follow up greater than 5 years (RR=1.43; 95% CI, 0.70 to 2.93; P=0.32). Visual inspection of the funnel plot showed asymmetry (Figure 4).
Table 5. Pooled relative risk (RR) and mean difference (MD).
| Outcome | RCTs | Meta-analyses | Heterogeneity I2 | ||||
|---|---|---|---|---|---|---|---|
| N | Patients | RR | MD | 95% CI | P | ||
| Overall revision | 6 | 719 | 1.44 | 0.88; 2.35 | 0.14 | 3% | |
| Short term follow up of revision | 2 | 220 | NC | NC | NC | NC | |
| Long term follow up of revision | 4 | 595 | 1.43 | 0.70; 2.93 | 0.32 | 27% | |
| Overall pain score | 7 | 695 | 1.13 | 0.03; 2.23 | 0.04 | 93% | |
| Short term follow-up for pain | 4 | 220 | 1.80 | 0.09; 3.51 | 0.04 | 92% | |
| Long term follow-up for pain | 3 | 475 | 0.28 | −1.02; 1.58 | 0.67 | 93% | |
| Overall HHS | 7 | 757 | 1.12 | −1.17; 3.41 | 0.34 | 99% | |
| Short term follow-up for HHS | 3 | 162 | −0.50 | −2.65; 1.65 | 0.65 | 92% | |
| Long term follow-up for HHS | 4 | 595 | 2.31 | −0.74; 5.36 | 0.14 | 99% | |
| Radiological osteolysis | 5 | 710 | 0.54 | 0.19; 1.57 | 0.26 | 85% | |
| Mortality | 5 | 725 | 1.06 | 0.73; 1.52 | 0.77 | 0% | |
| Complications | 4 | 391 | 1.54 | 0.21; 11.03 | 0.67 | 42% | |
HHS, average Harris Hip Score; N, number of RCT included; RR, Relative Risk; MD, mean difference; NC, not calculated because <3 RCTs were available for meta-analysis.
Figure 2.
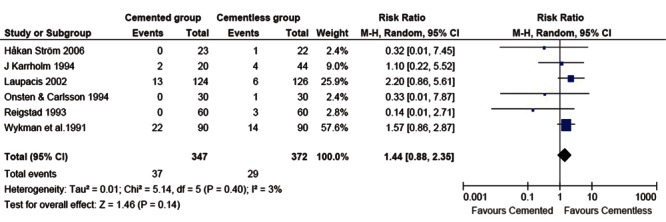
Forest plot of comparison: overall revision.
Figure 3.

Forest plot of comparison: long term follow-up (>5 years) for revision.
Figure 4.

Funnel plot of comparison: overall revision.
Pain scores were reported in 7 RCTs (695 patients). Four RCTs with short term and three with long follow-up evaluated this outcome (Figures 5 and 6). Meta-analysis of all RCTs (Figure 7, Table 5) revealed significantly improved pain score with cemented fixation (MD=1.13; CI: 0.03–2.23; P=0.04) compared with uncemented fixation. Similar results (Figure 5) were obtained for RCTs with short term follow-up (MD=1.80; CI: 0.09-3.51; P=0.04). The effect size was opposite for RCTs with long term follow-up (Figure 6) but not statistically significant (MD=0.28; CI: −1.02 to 1.58; P=0.67). Statistically significant heterogeneity (I2>90%) and symmetric funnel plots were noted (Figure 8).
Figure 5.
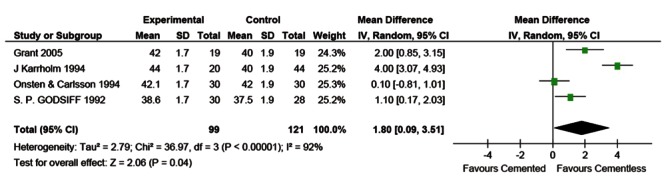
Forest plot of comparison: short term follow-up (<5 years) for pain score.
Figure 6.

Forest plot of comparison: long term follow-up (>5 years) for pain score.
Figure 7.
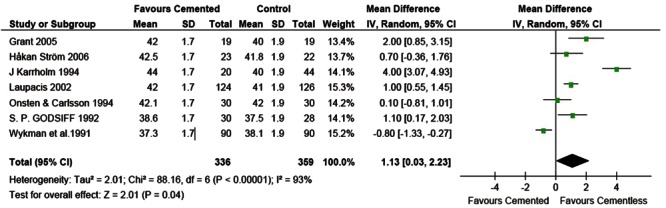
Forest plot of comparison: overall pain score outcome.
Figure 8.
Funnel plot of comparison: hhort term follow-up (<5 years) for pain dcore.
Statistically significant higher average HHS scores were reported in 4 of 7 RCTs in the uncemented group however pooled estimations of the average HHS score MDs did not show statistically significant difference (Table 5, Figure 9).
Figure 9.
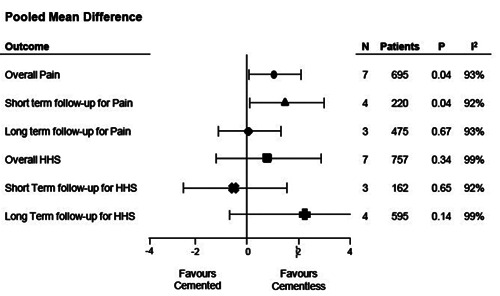
Pooled mean difference for pain score and functional outcome score measured by HHS.
The Relative risk (RR) of outcomes for mortality, complications, and radiological osteolysis were similar between the two groups (Table 5, Figure 10).
Figure 10.
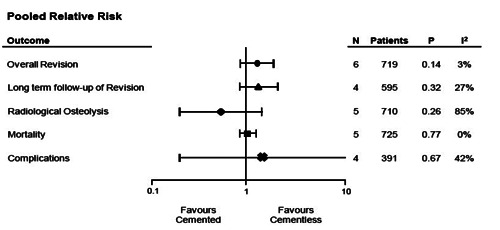
Pooled Relative Risk for all outcomes.
Summary of evidence
A meta-analysis is a useful tool as the results of cemented and uncemented components can be compared together as a package. There were several different components used in these selected studies, the influence of these variables (implant shape, material, etc) could be evaluated with a meta-analysis. Only 9 RCTs met our inclusion criteria. Our study did not demonstrate an overall superiority of either fixation method as measured by implant survival. Comparison of the studies with relatively short follow up versus studies with longer follow up without restriction to the patient's age demonstrated statistically significant differences, in particular better pain scores in the cemented groups. The difference in pain decreases with longer follow up though the cemented implant group still reported better pain scores overall.
Definitions of failure in hip replacement
A careful approach must be taken when analyzing each study for their definitions of success and failure. Criteria for failure can include revision rates, radiographic observations (demarcation, migration and cement fracture), and clinical failure (pain, reduced function and limited motion). Wejkner and Stenport showed that if only revision surgery was considered failure, their failure rate was 4% but taking other parameters into consideration the rate of clinical failure was 8%.29 Radiographic failure generally occurs first, followed by clinical failure with pain, loss of function, and finally, revision surgery. The lowest rate of failure will generally be the reoperation rate. Definition of failure in implant survival studies is fraught with inconsistencies. While we attempted to use estimates based on revisions undertaken for any reason, as this is less subjective than aseptic loosening or mechanical failure, the propensity for differential misclassification and resulting bias is present. This is because the decision to undertake a revision is influenced by the opinions of the surgeon and the patient.
Moreover, revisions are occasionally performed on well-fixed implants without evidence of infection or mechanical failure, and many radiographically loose or symptomatic implants are not revised.
Cemented versus uncemented fixation
Under the broad category of cement disease, investigators include a variety of deleterious processes that occur in conjunction with mechanical loosening of cemented implants. Despite the absence of a precise pathophysiology, it is apparent that a pernicious granulomatous response to cement and polyethylene particles, leading to the erosion of bone.30 It may occur in the presence or absence of loosening.31 The advantage of biologic fixation is very clear as every major survivorship analysis of cemented fixation demonstrates a progressive time dependent loss of fixation.32,33 It has been implied that once stable fixation occurs in the cementless implant, it does not deteriorate with time.34 Further independent, unbiased studies are required to validate this. Cementless femoral components are more expensive than uncemented components.35
Another potential advantage in uncemented fixation is that bone loss will not occur despite loosening, in contrast to the dramatic osteolysis seen in loose cemented implants. However there is evidence to contradict this, with bone loss demonstrated in loose uncemented implants.36 A much lower rate of thromboembolism has been shown in uncemented THRs in one study.37 This observation requires further studies to validate it.
Roder et al.38 found in their study of 4420 matched case controlled THAs that women had a significantly reduce odds ratio of acetabular component failure compared to men and was lower still for women with cemented compared to those with uncemented acetabular component. The study also found that obesity a significant risk factor for failure of the acetabular component with the uncemented cups having a higher odds ratio. Furthermore they found that in patients with dysplastic hips there was a significant decrease in the risk of failure in the cemented group.
In a recent literature review Clement et al.39 concluded that cemented fixation remains gold standard for the acetabulum as the overall and all cause reoperation risk was lower for cemented fixation. Pavkis et al. showed no difference e in the complications, wear, osteolysis, migration and clinical scores when they looked at only RCTs in their systematic review of literature. Non RCT studies revealed better osteolysis, migration properties and aseptic loosening survival for uncemented acetabular components. However in terms of wear and overall survival favored the cemented acetabular components.40 In a RCT involving 240 THRs Bjørgul et al.41 found that at 10-years follow up that there was no clinical and radiological difference between the cemented Charnley cup and the uncemented Duraloc cup. All had received a cemented Charnley stem. There was similarly no difference in the implant survival at 12–14 yeas follow up. A more recent RCT involving 250 patients with a minimum 17 year follow-up showed lower survival rates of cemented compared with cementless THA with Kaplan-Meier survivorship analysis at 20 years.42 Age less than 65years and male gender were significantly predictive for risk of revision surgery.
In a direct comparison study of 92 patients Bjerkholt et al.43 found that there was higher wear in those that had an uncemented acetabular component at 9–10 years follow-up, however the difference was not significant. Patients over 70 yrs of age received a cemented acetabular component and those under 60 years of age received an uncemented acetabular component.
Clinical and functional evaluation
Cemented femoral component provides an immediate postoperative advantage in terms of better integration between bone, cement and the prosthesis, which permits dramatic early relief of pain and early weight-bearing. In the short term outcome, our study shows almost all the relevant studies reported superiority of the cemented fixation to the uncemented in terms of pain reduction. Therefore, we conclude that for the clinical and functional outcome, the cemented group tends to be equal, if not superior, to the uncemented group.
Radiological evaluation
A poor correlation between radiographic and clinical findings with intraoperative findings during revision surgery has demonstrated in either component.44,45 Our finding supports that most radiographic differences were variable and did not seem to correlate with clinical findings.
Osteolysis is the leading concern for surgeons performing THRs and its incidence is influenced by many factors such as cementing techniques and prosthesis type. Only 4 studies examined RSA and in general there was no difference in migration or rotation of the compared implants.22,23,25,27 There was no correlation between weight, age or sex. These observations cannot be generalized and are limited to the few implants compared.
Role of randomized controlled trials and registry data
This review illustrates the advantages and limitations of RCT in assessing the effectiveness of new orthopedic devices. The RCT is considered the gold standard for the design of clinical research however, there are several drawbacks with this study design, such as the risk of performance bias between centers of excellence and routine surgery,46 RCTs are expensive, labor intensive and has a late feedback because of the demand for long-term follow-up.47 The performance of a RCT might be of limited value if the prosthesis used may have been redesigned during or soon after the study is completed and this adds to the cost, logistical difficulty, and potentially rendering the study irrelevant.8,12 Another disadvantage of many RCTs is that strict inclusion and exclusion criteria lead to a highly selected group of patients who are operated on by a small number of surgeons. This makes the generalizability of the results to the real world uncertain. Among the RCTs in our review, a sample size calculation was conducted in only one study.12 A total of 300 subjects were needed to ensure the statistical significance. However, due to slower-than-expected recruitment rate, the recruitment was stopped when 250 patients had been randomized. Insignificant differences are likely to result from the smaller sample size. Due to the obvious disadvantages of performing randomized studies, there is debate as to whether RCTs can be replaced by observational studies such as register studies which can document long-term performance and safety of the prosthesis in the real world. RCTs will, however, continue to be valuable. Garellick et al.48 compared the long-term survival results of two different hip implants with the results from the Swedish National Hip Registry. They concluded that despite the enormous amount of data, the registries can never replace a prospective, randomized trial.
Currently the data from the several national arthroplasty registries (Tables 6–8) show that cemented implants have a favorable outcome when revision of the implants is taken as the endpoint. The Norwegian registry data shows survivorship of cemented implants to be better but not significantly different.49 When Malchau et al.50 looked at the Swedish arthroplasty register and Lutch looked at the Danish arthroplasty register their findings suggested that cemented implants had a similar lower revision rate.51 However the uncemented implants did better in the less than 55 age group in both registers.
Table 6. Demographic of registry studies.
| Study | Country | Age (years) | Gender | THR (number) | Cemented | Cementless | Hybrid |
|---|---|---|---|---|---|---|---|
| Hailer et al. 2010 | Sweden | 60-75 | 56.532 M | 170.413 | 161.460 | 8953 | N/A |
| 88.805 F | |||||||
| Weiss et al. 2011 | Sweden | 72 (SD 11) | 987 M | 1885 | 812 | 1073 | N/A |
| 898 F | |||||||
| Mäkelä et al. 2010 | Finland | >55 | N/A | 10.310 | 9549 | 30.112 | N/A |
| Bordini et al. 2007 | Italy | <40 (408) | 1799 M | 4750 | (12.1%) | (51.5%) | (36.4%) |
| 40-69 (2965) | 2951 F | ||||||
| >70 (1377) | |||||||
| NJR 2011 | UK | 72.8 (cemented) | 32.843 F | 71.672 | 25.789 | 31.307 | 12.794 |
| 65.4 (cementless) | 21.647 M | ||||||
| Hooper et al. 2009 | New Zealand | <55 (6430) | N/A | 42.665 | 16.005 | 10.898 | 15.189 |
| 55-64 (10467) | |||||||
| 65-74 (13973) | Reverse hybrid 573 | ||||||
| >75 (11222) |
N/A: not available.
Table 8. Summary of registry study's findings.
| Study | Outcome |
|---|---|
| Hailer et al. 2010 | Uncemented THA had a higher risk of revision for any reason. Uncemented cup had a higher risk of cup revision due to aseptic loosening. Uncemented stem had a lower risk of stem revision due to aseptic loosening. No significant difference in the risk of revision due to infection between cemented and uncemented THA. |
| Weiss et al. 2011 | Survival was better for the cemented stems with up to 3 years of follow-up. Decreasing age, multiple previous revisions, short stem length, standard neck offset and short head-neck length were risk factors for reoperation. |
| Mäkelä et al. 2010 | Cementless stem had a higher survival rate at 15 years in patients aged >55 years. Polyethylene wear and osteolysis remain a serious problem for cementless cup designs with unplugged screw holes and low-quality liners. |
| Bordini et al. 2007 | Cemented cups and stems have a higher risk of failure compared with uncemented ones. Worst survival of the prosthesis are associated with male patients, younger than 40 years, affected by sequelae of congenital diseases, operated by a surgeon who performed less than 400 total hip artroplasty. |
| NJR 2011 | Revision rate for uncemented THRs is twice that of the cemented THRs at five years. The rate for hybrid THRs tends to lie between the rates for cemented and uncemented THRs. |
| Hooper et al. 2009 | Fully-cemented THRs had a lower rate of revision while uncemented THRs had a lower rate <65 years. The rate of revision of the acetabular component was less in the uncemented and hybrid groups. The rate of revision of cemented and uncemented femoral components was similar, except in patients >75 years of age in whom revision of cemented femoral components was significantly less frequent. Revision for infection was more common in patients aged <65 years and in cemented and hybrid THRs. Dislocation was the most common cause of revision for all types of fixation and was more frequent in both uncemented acetabular groups. The experience of the surgeon did not affect the findings. |
Table 7. Implants characteristics for registry studies.
| Study | Cemented implant | Cementless implant |
|---|---|---|
| Hailer et al. 2010 | Five most common cups (Lubinus, Charnley, Exeter Duration, Charnley Elite, and Reflection); Five most common stems (Lubinus SP2, Exeter polished, Charnley, Spectron EF Primary, and Scan Hip Collar) |
Five most common cups (Trilogy HA, CLS Spotorno, Trilogy, Trident HA, and Allofit); Five most common stems (CLS, Bi-Metric HA, ABG, Omnifit, and Wagner Cone) |
| Weiss et al. 2011 | Three most common (Lubinus, Exeter, and Spectron). | MP hip reconstruction prosthesis (Waldemar Link, Germany) |
| Makela et al. 2010 | Exeter Universal stem combined with the All-poly cup (Stryker, Mahwah, NJ); Müller Straight stem combined with the Müller Standard cup (Zimmer, Warsaw, IN); Lubinus SP II stem combined with the Lubinus IP cup (Waldemer Link, Hamburg, Germany) |
Anatomic Mesh/HG-II PCA Std/PCA Pegged Bi-Metric/PFU Bi-Metric/Mallory Bi-Metric/Vision ABG I/ABG I ABG I/ABG II ABG II/ABG II |
| Bordini et al. 2007 | Cemented all polyethylene Contemporary howmedica (Mahwah, New Jersey, USA) Muller Cremascoli (Milano, Italy), Muller Sulzer (Geneve,Switzerland), Exeter Howmedica, STEMS LC Samo AHS Cremascoli Definition Howmedica Exeter Howmedica Gemini De Puy self-locking Sulzer Elite De Puy Lubinus SP 2 Link |
Press fit, ceramic or metal liner AnCA Fit Cremascoli, Duofit PSF Samo, Fitek Sulzer, Standard Cup Protek Press fit, polyethylene liner Duraloc De Puy (Warsaw, Indiana, USA) Fitek Sulzer, Duofit PSF Samo (Bologna, Italy), ABG Howmedica, Vitalock Talon Howmedica, PCA Howmedica, STEMS Cone prosthesis Sulzer, Meridian Howmedica, CLS Sulzer, Metabloc Sulzer, Anca Cremascoli Duofit RKT Samo PCA Howmedica Citation Howmedica AML Depuy stems Anca Fit Cremascoli Dual fit Cremascoli stems |
| NJR 2011 | STEMS Exeter V40 CPT C-Stem AMT Cemented Stem C-Stem Cemented Stem Charnley Cemented Stem CUPS Contemporary Elite Plus Ogee Elite Plus Cemented Cup Marathon Exeter Rimt |
STEMS Corail Furlong HAC Stem Accolade Taperloc Cementless Stem Versys Cementless Stem CUPS Pinnacle Trident Trilogy Exceed ABT CSF Plus |
| Cooper et al. 2009 | N/A | N/A |
HG-II, Harris-Galante II; PCA Std, porous-coated Anatomic Standard; PFU, Press-Fit Universal; ABG, Anatomique Benoist Girard; N/A, not available.
Hailer et al.52 looked at data from the Swedish registry involving over a 170,413 THAs. Uncemented THAs (85%) had a significantly lower 10 year survival rate compared to the cemented THA (94%). This was largely due to the poorer performance of the uncemented acetabular components. While uncemented stems had a lower revision rate due to loosening they had a higher revision rate due to periprosthetic fracture in the first two postoperative years. Weiss et al.53 on the other hand reviewed the Survival of uncemented acetabular monoblock cups which represent a subtype of uncemented cups with the polyethylene liner molded into the metal shell and compared their survival to the modular designs in 210 hips from the Swedish Hip Arthroplasty Register. They concluded that both cups showed good survival rates at 11 years of follow up.
The data from the Finnish arthroplasty registry regarding THAs in the under 55-year age group showed higher revision rates for aseptic loosening in the cemented group compared to the proximally coated uncemented femoral components. The cemented all-polyethelyne acetabular components had a revision rate three times as high as the porous coated uncemented acetabular components. However there was no difference between cemented and uncemented implants when the end point was revision for any cause.54 The Finnish arthroplasty registry data regarding the 55-year and older age group suggests that there is no significant difference in overall implant survival between the two groups. Uncemented porous coated femoral components survived better in the 55-year to 74-year age group while in the 75-year and older age group there was no significant difference.55
The New Zealand registry show similar results. THAs with cemented acetabular and femoral components had a higher survival rate when all revision for all causes is taken into consideration. Uncemented THAs had a lower revision rate in the less than 65 years age group. Revision for aseptic loosening of the acetabular component was considerably lower in the uncemented and hybrid THA group with the exception of those aged over 75 years where the cemented acetabular components did better.56 Data from the Rizolli Institute registry in Italy shows that uncemented implants generally outperformed the cemented implants. They suggest that as experience with uncemented implants is increasing the results are improving, particularly in the younger THA patient. Interestingly they noted that the more expensive the prosthesis, the longer it survived.57 The 2011 National Joint registry data for England and Wales shows that the revision rate at five years for uncemented THRs is twice that of the cemented THRs.58 The rate for hybrid THRs tends to lie between the rates for cemented and uncemented THRs. These registry data suggest that cemented implants seem to have an overall better survival rates.
A met-analysis of previously published studies up to 2005 by Morshed et al.59 found that there was no difference in failure when defined as revision of one or both components of a THR. They found superior survival rates for cemented fixation for all age groups. Cemented titanium stems and threaded acetabular components had a poor survival rate. They noted a difference in the implant survival and the year of publication of studies with uncemented implant survival improving with time. While overall revision rates were higher in uncemented acetabular components in a study by Hartofilakidis et al.,60 they found that revision rates for aseptic loosening for the cemented acetabular component (28%) was more than twice that of uncemented components (12%). However they noted aggressive expansile osteolysis with the uncemented acetabular components, thought to be due to a combination of polyethylene and metal wear debris from the uncemented metal backed components.
The revision rate for infection is overall similar between the uncemented THA and the cemented THA with antibiotic cement. Revision rate was due to infection was 1.8 times higher in the cemented THAs where antibiotic cement was not used.61
Bias and confounders
While all included studies were randomized the potential for bias and confounders were not absent. Of the 9 RCTs, only one study documented proper randomization techniques, concealment of allocation, and discussed reasons for exclusion or non-participation.12
Losses to follow-up or non-response during data collection are sources of selection bias and were not addressed in most RCTs in this review. Of the 3 RCTs that mentioned the reasons for their exclusion and censoring, only one study accounted for withdrawals that the CONSORT statement requires.12,62
Review limitations
Several limitations in our work are important to note. In any systematic review or meta-analysis, there may be publication bias, incomplete ascertainment of studies and errors in data extraction. By restricting our analysis to RCTs, all factors that might affect outcomes are similarly distributed between the groups. We attempted to minimize errors in data extraction through cross-checking of all quantitative information by two authors. We used all available sources of data identified from a comprehensive literature search, without language restriction. Given the limitations in the published literature on this topic, the methods used in this study had limited bias and explored sources of heterogeneity to the greatest degree possible.
Conclusions
Although there are some limitations in the selected studies, our review showed no significant difference between cemented and cementless group in terms of implant survival as measured by the revision rate, mortality or the complication rate. Radiographic differences were variable and do not seem to correlate with clinical findings. It is almost certain that better shortterm clinical outcomes mainly improved pain score can be obtained from cemented fixation; this is still unclear for the long-term clinical and functional outcome. We strongly emphasize the need for more uniform standards in the selection of control groups in future trials.
References
- 1.Rothman RH, Cohn JC. Cemented versus cementless total hip arthroplasty. A critical review. Clin Orthop Relat Res. 1990:153–69. [PubMed] [Google Scholar]
- 2.Charnley J. Surgery of the hip-joint: present and future developments. Br Med J. 1960;1:821–6. doi: 10.1136/bmj.1.5176.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84A:171–7. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Sinha RK, Dungy DS, Yeon HB. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg Am. 2004;86A:1254–61. doi: 10.2106/00004623-200406000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995;77:432–9. doi: 10.2106/00004623-199503000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Clark CR. Cost containment: total joint implants. J Bone Joint Surg Am. 1994;76:799–800. doi: 10.2106/00004623-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Kirk PG, Rorabeck CH, Bourne RB, Burkart B. Total hip arthroplasty in rheumatoid arthritis: comparison of cemented and uncemented implants. Can J Surg. 1993;36:229–32. [PubMed] [Google Scholar]
- 8.Maloney WJ. National joint replacement registries: has the time come? J Bone Joint Surg Am. 2001;83A:1582–5. doi: 10.2106/00004623-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Hearn SL, Bicalho PS, Eng K, et al. Comparison of cemented and cementless total hip arthroplasty in patients with bilateral hip arthroplasties. J Arthroplasty. 1995;10:603–8. doi: 10.1016/s0883-5403(05)80203-7. [DOI] [PubMed] [Google Scholar]
- 10.Kim YH. Bilateral cemented and cementless total hip arthroplasty. J Arthroplasty. 2002;17:434–40. doi: 10.1054/arth.2002.31073. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Oh SH, Kim JS. Incidence and natural history of deep-vein thrombosis after total hip arthroplasty. A prospective and randomised clinical study. J Bone Joint Surg Br. 2003;85:661–5. [PubMed] [Google Scholar]
- 12.Laupacis A, Bourne R, Rorabeck C, et al. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. J Bone Joint Surg Am. 2002;84A:1823–8. doi: 10.2106/00004623-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Bourne RB, Rorabeck CH, Laupacis A, et al. A randomized clinical trial comparing cemented to cementless total hip replacement in 250 osteoarthritic patients: the impact on health related quality of life and cost effectiveness. Iowa Orthop J. 1994;14:108–14. [PMC free article] [PubMed] [Google Scholar]
- 15.Chandran P, Azzabi M, Miles J, et al. Furlong hydroxyapatite-coated hip prosthesis vs the Charnley cemented hip prosthesis. J Arthroplasty. 2010;25:52–7. doi: 10.1016/j.arth.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Devane PA, Robinson EJ, Bourne RB, et al. Measurement of polyethylene wear in acetabular components inserted with and without cement. A randomized trial. J Bone Joint Surg Am. 1997;79:682–9. doi: 10.2106/00004623-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Marston RA, Cobb AG, Bentley G. Stanmore compared with Charnley total hip replacement. A prospective study of 413 arthroplasties. J Bone Joint Surg Br. 1996;78:178–84. [PubMed] [Google Scholar]
- 18.Mulliken B, Nayak N, Bourne R, et al. Early radiographic results comparing cemented and cementless total hip arthroplasty. J Arthroplasty. 1996;11:24–33. doi: 10.1016/s0883-5403(96)80158-6. [DOI] [PubMed] [Google Scholar]
- 19.Rorabeck CH, Bourne RB, Laupacis A, et al. A double-blind study of 250 cases comparing cemented with cementless total hip arthroplasty. Cost-effectiveness and its impact on health-related quality of life. Clin Orthop Relat Res. 1994:156–64. [PubMed] [Google Scholar]
- 20.Rorabeck CH, Bourne RB, Mulliken BD, et al. The Nicolas Andry award: comparative results of cemented and cementless total hip arthroplasty. Clin Orthop Relat Res. 1996:330–44. [PubMed] [Google Scholar]
- 21.Godsiff SP, Emery RJ, Heywood-Waddington MB, Thomas TL. Cemented versus uncemented femoral components in the ring hip prosthesis. J Bone Joint Surg Br. 1992;74:822–4. doi: 10.1302/0301-620X.74B6.1447241. [DOI] [PubMed] [Google Scholar]
- 22.Grant P, Aamodt A, Falch J, Nordsletten L. Differences in stability and bone remodeling between a customized uncemented hydrox-yapatite coated and a standard cemented femoral stem. A randomized study with use of radiostereometry and bone densitometry. J Orthop Res. 2005;23:1280–5. doi: 10.1016/j.orthres.2005.03.016.1100230607. [DOI] [PubMed] [Google Scholar]
- 23.Karrholm J, Malchau H, Snorrason F, Herberts P. Micromotion of femoral stems in total hip arthroplasty. A randomized study of cemented, hydroxyapatite-coated, and porous-coated stems with roentgen stereo-photogrammetric analysis. J Bone Joint Surg Am. 1994;76:1692–705. doi: 10.2106/00004623-199411000-00013. [DOI] [PubMed] [Google Scholar]
- 24.McCombe P, Williams SA. A comparison of polyethylene wear rates between cemented and cementless cups. A prospective, randomised trial. J Bone Joint Surg Br. 2004;86:344–9. doi: 10.1302/0301-620x.86b3.14567. [DOI] [PubMed] [Google Scholar]
- 25.Onsten I, Carlsson AS. Cemented versus uncemented socket in hip arthroplasty. A radiostereometric study of 60 randomized hips followed for 2 years. Acta Orthop Scand. 1994;65:517–21. doi: 10.3109/17453679409000904. [DOI] [PubMed] [Google Scholar]
- 26.Reigstad A, Rokkum M, Bye K, Brandt M. Femoral remodeling after arthroplasty of the hip. Prospective randomized 5-year comparison of 120 cemented/uncemented cases of arthrosis. Acta Orthop Scand. 1993;64:411–6. doi: 10.3109/17453679308993656. [DOI] [PubMed] [Google Scholar]
- 27.Strom Hk, Kolstad K, Mallmin H, Sahlstedt B, Milbrink J. Comparison of the uncemented Cone and the cemented Bimetric hip prosthesis in young patients with osteoarthritis: an RSA, clinical and radiographic study. Acta Orthop. 2006;77:71–8. doi: 10.1080/17453670610045713. [DOI] [PubMed] [Google Scholar]
- 28.Wykman A, Olsson E, Axdorph G, Goldie I. Total hip arthroplasty. A comparison between cemented and press-fit noncemented fixation. J Arthroplasty. 1991;6:19–29. doi: 10.1016/s0883-5403(06)80153-1. [DOI] [PubMed] [Google Scholar]
- 29.Wejkner B, Stenport J. Charnley total hip arthroplasty. A ten- to 14-year follow-up study. Clin Orthop Relat Res. 1988:113–9. [PubMed] [Google Scholar]
- 30.Huddleston HD. Femoral lysis after cemented hip arthroplasty. J Arthroplasty. 1988;3:285–97. doi: 10.1016/s0883-5403(88)80027-5. [DOI] [PubMed] [Google Scholar]
- 31.Harris WH, McGann WA. Loosening of the femoral component after use of the medullary-plug cementing technique. Follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am. 1986;68:1064–6. [PubMed] [Google Scholar]
- 32.Amstutz HC, Yao J, Dorey FJ, Nugent JP. Survival analysis of T-28 hip arthroplasty with clinical implications. Orthop Clin North Am. 1988;19:491–503. [PubMed] [Google Scholar]
- 33.Hozack WJ, Rothman RH, Booth RE, Jr, et al. Survivorship analysis of 1,041 Charnley total hip arthroplasties. J Arthroplasty. 1990;5:41–7. doi: 10.1016/s0883-5403(06)80008-2. [DOI] [PubMed] [Google Scholar]
- 34.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 35.Unnanuntana A, Dimitroulias A, Bolognesi MP, et al. Cementless femoral prostheses cost more to implant than cemented femoral prostheses. Clin Orthop Relat Res. 2009;467:1546–51. doi: 10.1007/s11999-008-0485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zweymuller K. A cementless titanium hip endoprosthesis system based on press-fit fixation: basic research and clinical results. Instr Course Lect. 1986;35:203–25. [PubMed] [Google Scholar]
- 37.Kim YH, Suh JS. Low incidence of deep-vein thrombosis after cementless total hip replacement. J Bone Joint Surg Am. 1988;70:878–82. [PubMed] [Google Scholar]
- 38.Roder C, Bach B, Berry DJ, et al. Obesity, age, sex, diagnosis, and fixation mode differently affect early cup failure in total hip arthroplasty: a matched case-control study of 4420 patients. J Bone Joint Surg Am. 2010;92:1954–63. doi: 10.2106/JBJS.F.01184. [DOI] [PubMed] [Google Scholar]
- 39.Clement ND, Biant LC, Breusch SJ. Total hip arthroplasty: to cement or not to cement the acetabular socket? A critical review of the literature. Arch Orthop Trauma Surg. 2012;132:411–27. doi: 10.1007/s00402-011-1422-2. [DOI] [PubMed] [Google Scholar]
- 40.Pakvis D, van Hellemondt G, de Visser E, et al. Is there evidence for a superior method of socket fixation in hip arthroplasty? A systematic review. Int Orthop. 2011;35:1109–18. doi: 10.1007/s00264-011-1234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bjorgul K, Novicoff WM, Andersen ST, et al. No differences in outcomes between cemented and uncemented acetabular components after 12-14 years: results from a randomized controlled trial comparing Duraloc with Charnley cups. J Orthop Traumatol. 2010;11:37–45. doi: 10.1007/s10195-010-0082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Corten K, Bourne RB, Charron KD, et al. What works best, a cemented or cementless primary total hip arthroplasty?: minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011;469:209–17. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bjerkholt H, Hovik O, Reikeras O. Direct comparison of polyethylene wear in cemented and uncemented acetabular cups. J Orthop Traumatol. 2010;11:155–8. doi: 10.1007/s10195-010-0104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carlsson AS, Gentz CF. Radiographic versus clinical loosening of the acetabular component in noninfected total hip arthroplasty. Clin Orthop Relat Res. 1984:145–50. [PubMed] [Google Scholar]
- 45.Cook SD, Thomas KA, Haddad RJ., Jr Histologic analysis of retrieved human porous-coated total joint components. Clin Orthop Relat Res. 1988:90–101. [PubMed] [Google Scholar]
- 46.Crowninshield RD, Brand RA, Johnston RC, Milroy JC. An analysis of femoral component stem design in total hip arthroplasty. J Bone Joint Surg Am. 1980;62:68–78. [PubMed] [Google Scholar]
- 47.Dorey F, Grigoris P, Amstutz H. Making do without randomised trials. J Bone Joint Surg Br. 1994;76:1–3. [PubMed] [Google Scholar]
- 48.Garellick G, Malchau H, Herberts P. Survival of hip replacements. A comparison of a randomized trial and a registry. Clin Orthop Relat Res. 2000:157–67. [PubMed] [Google Scholar]
- 49.Havelin LI, Engesaeter LB, Espehaug B, et al. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000;71:337–53. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 50.Malchau H, Herberts P, Eisler T, et al. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84A(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 51.Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand. 2000;71:433–9. doi: 10.1080/000164700317381081. [DOI] [PubMed] [Google Scholar]
- 52.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weiss RJ, Hailer NP, Stark A, Karrholm J. Survival of uncemented acetabular monoblock cups: evaluation of 210 hips in the Swedish Hip Arthroplasty Register. Acta Orthop. 2012;83:214–9. doi: 10.3109/17453674.2012.688726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eskelinen A, Remes V, Helenius I, et al. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0–22 years. Acta Orthop. 2005;76:28–41. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 55.Makela KT, Eskelinen A, Pulkkinen P, et al. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–70. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 56.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–8. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 57.Bordini B, Stea S, De Clerico M, et al. Factors affecting aseptic loosening of 4750 total hip arthroplasties: multivariate survival analysis. BMC Musculoskelet Disord. 2007;8:69. doi: 10.1186/1471-2474-8-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.National Joint Registry. The 2011 National Joint registry data for England and Wales. [Accessed: January 2013]; Available from: http://www.njrcentre.org.uk.
- 59.Morshed S, Bozic KJ, Ries MD, et al. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78:315–26. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 60.Hartofilakidis G, Georgiades G, Babis GC. A comparison of the outcome of cemented all-polyethylene and cementless metal-backed acetabular sockets in primary total hip arthroplasty. J Arthroplasty. 2009;24:217–25. doi: 10.1016/j.arth.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 61.Engesaeter LB, Espehaug B, Lie SA, et al. Does cement increase the risk of infection in primary total hip arthroplasty? Revision rates in 56,275 cemented and uncemented primary THAs followed for 0–16 years in the Norwegian Arthroplasty Register. Acta Orthop. 2006;77:351–8. doi: 10.1080/17453670610046253. [DOI] [PubMed] [Google Scholar]
- 62.Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ. 1996;313:570–1. doi: 10.1136/bmj.313.7057.570. [DOI] [PMC free article] [PubMed] [Google Scholar]


