Abstract
Hip prosthesis stems with a short stem length and proximal fixation geometry support a bone-preserving and muscle-sparing implantation and should also allow for revision surgery with a standard hip stem. We present 250 prospectively documented clinical and radiological results from the Metha Short Hip Stem prosthesis (B. Braun-Aesculap, Tuttlingen, Germany) after an average follow-up of 4.9 years. The average patient age at surgery was 60 years. Indication for total hip replacement was primary osteoarthrosis (OA) (78% of patients), OA based on developmental dysplasia of the hip (16%), and other indications (6%). At the last follow-up, the average Harris Hip Score was 97 points. 85% of patients were very satisfied and 14% were satisfied after surgery, whereas 1% were dissatisfied. Pain according to the Visual Analogue Scale improved from 7.4 (min 1.6, max 9.5) pre-operatively to 0.23 (min 0, max 6.6). No joint dislocations occurred when predominantly using 28 mm and 32 mm prosthesis heads. Nine short-stems were revised: three after bacterial infections, two after primary via valsa with penetration of the femoral cortex two and three months after surgery, and three after early aseptic cases of loosening within the first year. A further nine osseously consolidated short-stems had to be replaced due to breakage of the modular titanium cone adapter after an average of 3.1 years (min 1.9, max 4.4). All surgical revisions were performed using primary standard stems. Without taking the material-related adapter failures into account, a five year Kaplan-Meier survival rate of 96.7% (95% confidence interval 93.4–98.3) was determined for the short-stem prostheses. There were no radiological signs of loosening in any of the short-stem prostheses at the last examination. Fine sclerotic lines were detected in Gruen's AP zones 1 (19%) and 2 (10.5%), individual hypertrophies in zone 3 (3.5%), fine seams in zones 4 (5.5%) and 5 (4%), without pedestal formations in zone 4, clear cancellous bone compressions in zone 6 (97.5%), as well as single fine scleroses (1.5%) and atrophies (2.5%) in zone 7. The mid-term clinical results with periprosthetic bone remodeling and without radiological signs of loosening confirm this metaphyseal short-stem treatment and fixation concept and the possibility of revision surgery using standard hip stems. Long-term results must be further observed on a prospective basis as part of this collective study.
Key words: short-stem hip prosthesis, prospective follow-up study, mid-term results.
Introduction
For patients with good bone quality, treatment with a cementless hip prosthesis using a range of successful stem designs (which have not significantly changed over the years) has led to excellent long-term results, and this generally applies for younger patients as well.1 To improve this high quality of treatment with shorter prosthesis stems, a targeted approach is required where the implantation must be increasingly bone-preserving, muscle-sparing, and anatomically correct, and the shape of the femoral neck must support a shorter stem length and implant size.
When attempting to maintain an intact trochanteric musculature and preserve as much femoral bone as possible during the first implantation, the increased life expectancy and therefore increased statistical risk of a surgical revision for younger patients should be taken into account.2 If a standard implant can be used in a surgical revision instead of a longer revision stem, this can be considered as an advantage for the hip arthroplasty treatment concept. However, this only applies if the lifetime of the first treatment with a short-stem is comparable with that of a standard stem. Depending on the model, the short stem is cementless anchored to the femoral neck, the metaphysis or the upper diaphysis whilst keeping the trochanteric structures completely intact.
Up until now, results from short-stem hip prostheses have only been available in a few works. In addition to femoral neck prostheses,3,4 the majority of short-stems currently available are inserted in the femur, in the metaphyseal region,5,6 and are comparable with models which were already being implanted back in the 1990s.7–11 A comparative clinical follow-up study of a short and standard stem with a similar design showed that equivalent lifetimes were essentially possible and that intraoperative complications with shorter stems could be reduced.12 Even the short-stem implants newly developed in recent years follow this hip arthroplasty treatment concept.13
No binding definition on the length of a short-stem can be found in previously published works. In general, the overall shorter implant length inserted in the bone lies within the broad range of between less than 80 mm and up to approx. 120 mm, and the short-stem fixation concept in question must also be taken into account.
In order to prove the comparable lifetimes of standard prostheses and short-stems, clinical follow-up studies need to be carried out on short-stem lifetime and migration behavior, which, in addition to generally encouraging early clinical results and subjectively satisfied patients, are not disassociated from first-time use and the learning curve that comes with a new implant and implantation concept.
A detailed radiological analysis of the periprosthetic bone remodeling is also necessary, as this may present important particularities regarding the short-stem model used.
The aim of this study is therefore to prepare a prospective overview of the clinical and radiological results of a modular short-stem hip prosthesis which was first clinically used in 2004.14
Materials and Methods
Patients
The study group comprises 250 consecutive hip arthroplasty treatments using the Metha Short Hip Stem cementless implant with modular titanium adapters (B.Braun-Aesculap, Tuttlingen, Germany). The current prospective follow-up examination was given a positive vote from the ethics committee (FEKI 09/2463; Freiburg) and carried out in two hospitals: 124 treatments were carried out in hospital 1 (from August 2004 until July 2005) and 126 treatments were carried out in hospital 2 (from August 2004 until November 2005).
Those included in the study were patients with indications of primary total hip arthroplasty. The exclusion criteria for the short-stem treatment included poor bone quality or anatomical femur shapes which would exclude the implantation of the short-stem model used. The upper age limit was approximately 70 years and no distinction was made in terms of gender. The patients were informed of the aims of the study and the new development of the femoral implant component.
Technique
The short-stem prosthesis used meets the criteria outlined above for a bone-preserving short-stem implant using cementless proximal fixation in the metaphyseal region. The top two-thirds of the stem are coated with a 0.35 mm micro-porous titanium coating and a 20 μm dicalcium phosphate coating.15,16 The curved stem has a conical design which allows for a high degree of load-stable primary stability on implantation. The femoral neck is largely untouched when the osteomy is performed and the prosthesis is attached above the closed femoral neck stump which offers primary stability. The main support comes from the medial stem placement on the calcar. A proximal bilateral conical stem shape also supports primary stability and the assertion of metaphyseal force. The final stem position is determined by placing the smooth and slightly curved distal tip of the prosthesis on the dorsolateral cortical bone. The anteversion of the femoral neck results in the prosthesis tip being positioned in the direction of the dorsal cortical bone whilst simultaneously ensuring that the head is in an anatomically-correct position.
The study protocol contains no criteria for cup placement, the surgical approach, the number of surgeons involved or the in-patient course of treatment or rehabilitation process.
Follow-up examination
No comparison group was defined for the study. The raw data included the indication, the Harris Hip Score, the subjective sensation of pain according to the visual analogue scale (VAS), as well as surgical treatment data and complications. Follow-up examinations were carried out within the first year and postoperatively after more than two and four years. The Harris Hip Score,17 VAS and subjective patient satisfaction were all recorded.
All X-ray results were examined for osteolysis. Periarticular ossifications were graded according to Brooker.18 An analysis of the stem position was carried out through a planar measurement of the position of the proximal implant surface set at an angle of 50° to the femoral stem axis in terms of a neutral (130–140°), varus (<130°) or valgus (>140°) implant position. Radiologically detectable postoperative stem movements were measured in categories of <5 mm, >5 mm and >10 mm in relation to the images taken directly after the operation. The distance from the trochanter minor to the bone resection height and the medial shoulder of the prosthesis was also determined. The radiological inclination of the cup was graded with values from <40°/40–50°/>50° and the cup anteversion with <5°/5–20°/>20°.
The following periprosthetic changes observed in the X-rays were documented: hypertrophies, atrophies, seam formations and spot welds,19 as well as sclerotic lines in the form of a neocortex.7 These were recorded using a distribution of zones adapted to the short-stem used,20 with zones 1/2 and 6/7 in the coated upper two-thirds of the stem, zones 3/4 in the uncoated distal stem region and the stem tip as zone 5. The radiological results were examined by an interobserver experienced with the short-stem implant being studied.
Statistics
The values in the tables are given as an average value and range (in brackets). Multivariate analyses were carried out with a single multivariate linear regression model. Kaplan-Meier estimators with a 95% confidence interval were used for survival rates. Calculations were carried out using the statistical software SAS (Version 9.2, SAS Inst. Inc. Cary NC, USA).
Results
At the most recent annual examination, 25 patients and seven deceased patients with eight treatments had dropped out of the study. Thirteen patients could not be contacted at their last follow-up examination or refused to participate in the current follow-up examination. There are 204 clinical and 200 radiological data sets for an average follow-up period of 4.9 years (min 2.9, max 7.1). Table 1 contains the general treatment and follow-up data of both participating hospitals as well as the data for the entire group. Figure 1 shows an example of treatment.
Table 1. General treatment and follow-up data per hospital and as an entire group.
| Hospital 1 | Hospital 2 | Total | |
|---|---|---|---|
| Number of cases | n=124 | n=126 | n=250 |
| Time period | Aug. 2004 - July 2005 | Aug. 2004 - Nov. 2005 | Aug. 2004 - Nov. 2005 |
| Dropped out | 8 | 25 | 33 |
| Could not be contacted | 6 | 7 | 13 |
| Follow-up examination | 110 | 94 | 204 |
| Follow-up examination time | 4.9 (2.9-6.5) years | 4.8 (3.2-7.1) years | 4.9 (2.9-7.1) years |
| Age | 61 (38-71) years | 59 (27-73) years | 60 (27-73) years |
| ♂/♀ | 42%/58% | 42%/58% | 42%/58% |
| BMI | 28 (16-47) | 27 (18-41) | 27 (16-47) |
| HHS pre-op | 47 (22-70) | 53 (22-86) | 50 (22-86) |
| HHS at last follow-up ex. | 98 (60-100) | 97 (46-100) | 97 (46-100) |
| VAS-10 pain pre-op | 8.0 (4.9-9.5) | 6.9 (1.6-9.4) | 7.4 (1.6-9.5) |
| VAS-10 pain follow-up ex. | 0.1 (0-6.6) | 0.35 (0-6) | 0.23 (0-6.6) |
| Primary coxarthrosis | 75% | 80% | 78% |
| Dysplasia coxarthrosis | 17% | 15% | 16% |
| Femoral head necrosis | 2% | 2% | 2% |
| Other sec. coxarthrosis | 4% | 3% | 4% |
| Other diagnoses | 2% | 0% | 1% |
Figure 1.
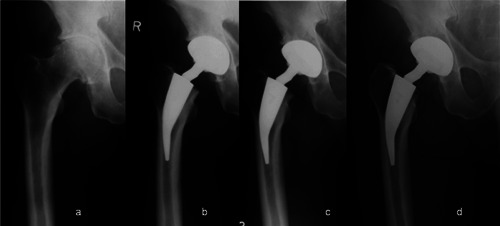
Example of treatment pre-op (a), post-op (b), at 3 months (c) and at 61 months (d).
During the recruitment period, the aforementioned short-stem was implanted in 12 patients on both sides. All patients received cementless cup arthroplasty treatments with ceramic-ceramic (n=109), ceramic-PE (n=137) or metal-PE (n=4) pairings. The polyethylene implants were conventionally sterilized in a nitrogen atmosphere and were not highly cross-linked. Small prosthesis head diameters of 28 mm (40%) and 32 mm (59%) were used predominantly, and 36 mm heads were only used in three cases. The cup inclination (<40°/40–50°/>50°) was determined to be 3%/89%/8%, and the cup anteversion (<5°/5–20°/>20°) as 7%/90%/3%. The procedures were performed by 14 surgeons in total. All surgical incisions were made using a muscle-preserving anterolateral approach.
The CCD angle distribution of the modular 130°/135°/140° femoral neck adapter was 32%/63%/6%, of which 67% was neutral, 22% was in relative 7.5° antetorsion and 11% was in relative 7.5° retrotorsion.
Clinical results
At the last follow-up examination, 85% of patients were very satisfied with the results of the treatment, 14% were satisfied and 1% were dissatisfied. No patients indicated that they were very dissatisfied. For one of the dissatisfied patients, no reason could be deduced from the results of the treatment; for the second patient, revision surgery took place after 64 months due to joint noises and cup complications.
At the last follow-up examination, the average Harris Hip Score was 97 points. 92% of patients scored over 95 points, 4% scored between 85 and 95 points, and 4% scored less than 85 points. One patient with the lowest score of 42 points complained about considerable discomfort in both hip joints; a short-stem had been implanted in one side as part of this study whilst the other side had been treated with a standard stem implant. Pain in the femoral stem region was not observed.
Table 2 gives a summary of complications that were not followed by replacement of the short-stem implant, together with notes on the course of treatment.
Table 2. List of complications without revision of the short-stem.
| Patient | Implantation | Complication | Time | Notes |
|---|---|---|---|---|
| ♀70 | 09/2005 | Femoral nerve lesion | Intra-op | Completely healed, HHS = 94; follow-up ex. at 4.2 years |
| ♀59 | 11/2004 | Stem fissure, left without cerclage | Intra-op | Healed without complication, HHS = 100; follow-up ex. at 6 years |
| ♀55 | 01/2005 | Ceramic head breakage | 12 months | After a considerable fall, replacement of adapter and head, HHS = 96; follow-up ex. at 5 years |
| ♀69 | 09/2005 | Replacement of cup | 9 days | Without subsequent complications, HHS = 96; follow-up ex. at 4.2 years |
| ♀57 | 09/2004 | Femoral fissure | Intra-op | Cerclage, without post-op complications, HHS = 100; follow-up ex. at 6.5 years |
| ♂66 | 01/2005 | Very deep neck resection | Intra-op | No abnormalities, well-integrated, HHS = 100; follow-up ex. at 3.3 years |
| ♂68 | 04/2005 | Stem subsidence of 9 mm post-op; stable after 1-year follow-up ex. | Post-op | No abnormalities, well-integrated, HHS = 100; follow-up ex. at 5.8 years |
HHS, Harris Hip Score.
The short-stem had to be revised in nine cases (3.6%): three (1.2%) femoral short-stem components after septic progression, three (1.2%) due to early aseptic loosening (two after 9 months and one after 11 months), one (0.4%) after cup complications with joint noises and breakage of the ceramic inlay after 64 months and two (0.8%) primary implantation failures due to a via Valsa mal-positioning after two and three months respectively (Table 3). Figure 2 shows the progression of a case of early loosening after nine months followed by replacement with a cementless standard stem.
Table 3. List of complications with revision of the short-stem.
| Patient | Implantation | Complication | Time | Revision |
| ♂62 | 07/2005 | Aseptic stem loosening | 9 months | 03/2006 to standard stem |
| ♀56 | 06/2005 | Infection | 36 months | 08/2008 to standard stem |
| ♀58 | 08/2005 | Infection | 12 months | 06/2006 to standard stem |
| ♀60 | 09/2005 | Via valsa, replacement of stem | 2 months | 11/2005 to standard stem |
| ♂54 | 09/2005 | Aseptic stem loosening | 9 months | 06/2006 to standard stem |
| ♂70 | 10/2004 | Replacement of stem after breakage of ceramic insert | 64 months | 02/2009 to standard stem |
| ♀44 | 02/2005 | Infection | 12 months | 02/2006 to standard stem |
| ♂63 | 09/2004 | Perforation of the dorsal femoral cortical bone, stem replacement | 3 months | 12/2004 to standard stem |
| ♀44 | 08/2004 | Aseptic stem loosening | 11 months | 07/2005 to standard stem |
Figure 2.

Early loosening after 9 months followed by replacement with a cementless standard stem (a) post-op (b,c) at 4 and 9 months and (d) after 2 years.
In addition, nine (3.6%) osseously consolidated stems had to be revised after a breakage of the modular titanium cone adapter. Such breakages took place after 3.1 years on average (min 1.9, max 4.4). One patient reported breakages on both sides after 1.9 years and 2.5 years respectively. All revision procedures were performed using primary standard stems whilst retaining the cup components. At the last follow-up examination, the Harris Hip Score was 100 for seven patients and 96 for one patient. The stems had ingrown very tight in the bone and could only be removed through a careful proximal chiselling procedure.
The 5-year Kaplan-Meier survival curve of the short-stems was 92% (95%, CI 87.3–95.0) and 96.7% (95%, CI 93.4–98.3) without taking the adapter failures into consideration, as these are analyzed separately.
Radiological results
For the analysis of the results, 200 prospective series of images were available at the last follow-up. No femoral stem components were shown to be loose and there were no seam formations >1 mm or femoral osteolysis. Ossifications of Brooker class I and II were observed in 6.9% and 1.3% of cases respectively. The stem position was neutral (130–140°) in 74.6% of cases, valgus (>140°) in 5.6% of cases, and varus (<130°) in 19.8% of cases. In comparison to the postoperative images, eight cases of secondary stem movements were observed on the X-ray images of the patients remaining in the study at the last follow-up. Seven of these were under 5 mm and one was between 5–10 mm. Two factors which were likely to influence postoperative subsidence of the stem were the resection height and male gender. However, this was not significant due to the low number of migration cases.
The resection height, which is measured as the relation of the distance from the trochanter minor to the bone resection height and the medial shoulder of the prosthesis, was an average of 86.5%. This figure was significantly lower in hospital 1 at 81.1% (min 60.7%, max 100%) (P<0.02) than in hospital 2 where it was 90.8 % (min 67.2%, max 100%).
This was the only significantly deviating result parameter according to the multivariate analysis (multivariate linear model). Further significant correlations between patient parameters, indications, stem positions, resection heights and radiological findings were not determined.
Typical manifestations of the periprosthetic radiological findings have been summarized in Figure 3.
Figure 3.

Typical radiological findings after 5 years: (a) sclerotic line < 1mm in zones 1+2, (b) spot weld in zone 2/3 at the coating interface, (c) hypertrophy in zone 3, (d) atrophy in zone 7 and fine sclerotic lines in zones 4 and 5.
The X-ray results have been summarized in Table 4. The review performed by an interobserver revealed in 1.4% of Gruen's AP zones assessed (Figure 4) maximum deviations ranging from –2.0% to +2.5% in zones 4 and 5, as well as ±0.5% in the other AP zones.
Table 4. Radiological results in the AP projection.
| Radiological results AP zones | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| No abnormalities | 80.5% | 89.5% | 96.5% | 93.0% | 95.0% | 2.5% | 94.0% |
| Seam formations/sclerosis up to 1 mm | 19.0% | 10.5% | 0% | 5.5% | 4.0% | 0% | 1.5% |
| Radiolucent lines 1 mm to 2 mm | 0.5% | 0% | 0% | 0.5% | 0.0% | 0% | 0% |
| Radiolucent lines >2 mm/radiolysis | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| Resorption/atrophy | 0% | 0% | 0% | 0% | 0% | 0% | 2.5% |
| Hypertrophy | 0% | 0% | 3.5% | 0% | 1.0% | 97.5% | 2.0% |
Figure 4.

Metha Short Hip Stem prosthesis and definition of Gruen's periprosthetic zones.
With a figure of 97.5% (interobserver = IO 97.0%), zone 6 showed hypertrophy of the trabecular structures in the direction of the medial distal coating interface of zone 6/5 in almost all cases. Similarly, poorly pronounced lateral spot weld bone structures were observed in the direction of the distal lateral coating interface of zone 2/3 in 61% (IO 60%) of cases. Hypertrophies in the lateral distal zone 3 occurred in 3.5% (IO±0.0%) of cases.
Fine seams <1 mm and findings classed as sclerotic lines or neocortex were found in Gruen's surface-coated AP zones 1 and 2 in 19% (IO -0.5%) and 10.5% (IO ± 0.0%) of cases respectively.7
Atrophies on the calcar femorale in zone 7 were observed in 2.5% (−0.5%) of cases. Fine seam formations of the same size were also found around the distal uncoated stem tip of zones 3 and 5. No pedestal formations under the stem tip in zone 4 were found. In one case, a stem tip located inside the cortical bone did not cause a hypertrophic reaction. In 69% of cases, the prosthesis tip was positioned dorsolaterally on the cortical bone; in all other cases, direct contact with the cortical bone was not radiologically detectable in the AP or lateral X-ray projection.
Discussion
The two hospitals participating in this study have extensive experience working with the Metha Short Hip Stem model. This collective study focuses on treatments performed in two of the authors' hospitals. An independent assessment of the radiological results was taken into account by means of an interobserver review.
The prospectively documented clinical and radiological results for a short hip stem first implanted in 2004 are being presented after an average follow-up of 4.9 years.
The study has been designed to focus on the quality of results from the femoral short-stem treatment. The average patient age of 60 years represents an age group for which the use of cementless standard implants has already been tried and tested.
In the Australian national joint replacement register,21 survival rates for cementless hip arthroplasty treatments after five years for patients with primary coxarthrosis up to 65 years are between 96% and 97%. These figures also include early interventions to replace cup or head components, as well as septic complications. In the Swedish hip arthroplasty register,22 the figure for interventions to replace established cementless standard stems in the first five years for patients below 60 years is 2%, not taking into account interventions to replace cup components due to primary instabilities. The demand for the short-term, low revision frequency of new short-stem designs is therefore very high. The effect that a higher prevalence of secondary coxarthrosis has on younger patients and their activity seems to play a less significant role in the first few years than the quality of surgical treatment and correct indication for the implant system used.
Survival rates without aseptic loosening and revision of a femoral short-stem component have been published as 98% after 6.8 years in 162 treatments,7 99% in 155 cases after 6.2 years,9 and 100% after 5.2 years.6 Studies also describe the different periprosthetic bone reactions characteristic for the short-stems used and which, depending on the stem design, are usually found in the upper,6,9 middle and lower parts of the short-stem.8,10
One strength of this particular study is the relatively high total number of 250 prospectively and consecutively documented treatments. The recruitment was carried out for all treatments using the newly developed short-stem model, including a learning curve, for a total of 14 participating surgeons as part of normal clinical routine.
The clinical results revealed a high average Harris Hip Score of 97 points. The subjective patient satisfaction level was also high, with 85% of patients reporting that they were very satisfied and 14% as being satisfied. Studies with the same short-stem type over a short-term period revealed a HHS of 95 points and a total of 96% satisfied patients.5 In studies focusing on the patients' physical activity, a Harris Hip Score of 94 points was achieved after 2.7 years (2.0–4.2) in 68 patients with the same type of short-stem prostheses.23 With an indication of femoral head necrosis,24 a HHS of just 90.6 points was determined in one collective study of 72 Metha Short Hip Stem treatments after 2.8 years. The starting score in this study was 41.4 points, which was 8.5 points lower than our overall starting figure.
Eighteen short-stems had to be revised in our study group, nine of which were due to a breakage of the modular titanium adapter. There were also three cases of septic progression, two implantation failures due to cortical bone perforation (malpositioning) which required revision after a few weeks, and one revision was carried out of a firmly integrated stem after cup complications. These revision procedures are not attributable to the short-stem implant. The remaining three cases involved aseptic loosening of the implant and were all reported within a period of up to one year after surgery. These cases displayed undersizing and clear radiological signs of loosening with seam formations >2 mm in zones 1 and 2 and were accompanied by clinical pain symptoms.
In 50 prospectively reviewed treatments with the short-stem implant used in this study after 2.4 years (1.9–2.8), Braun et al.5 reported one case of aseptic loosening of the stem, one case of breakage of the titanium adapter and one case of early periprosthetic fracture after a fall during rehabilitation.
These data for early aseptic complications correspond to those of our study which, excluding the titanium adapter failures, results in a 5-year Kaplan-Meier revision rate of 96.7% (Figure 5). The various different reasons for revision of the short-stem model of our study is also determined by the first implantation phase of the short-stem design in question. The fact that all revision procedures could be performed using standard hip stems confirms the fundamental aim of using a short prosthesis stem to improve the potential revision situation. This applies in particular for the nine cases of short-stems which were firmly integrated with the bone and showed no clinical or radiological abnormalities before the breakage of the implant component. The causes of the failures have already been examined and the procedure for explanting the stem and treating patients has also already been described.25,26 Since 2007, the short-stem adapter material has been changed to a cobalt chromium alloy and the stem product range has been supplemented with three non-modular stem versions with CCD angles of 120°, 130° and 135°.
Figure 5.
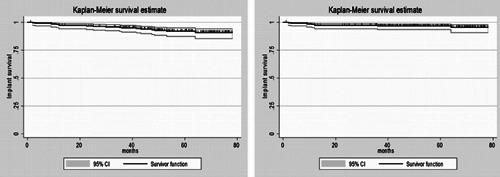
Kaplan-Meier survival curves. On the left: all stem revisions, on the right: stem revisions without titanium neck adapter breakages.
At the last follow-up, no evident radiological signs of femoral loosening were detected and there were no clinically abnormal progressions attributable to the short-stem implant.
The radiological examination of cementless implanted prosthetic hip stems is an important assessment criterion for newly developed stem designs. In this study, a particular focus was placed on obtaining a detailed radiological analysis - the results of which provide valuable data for the assessment of the periprosthetic bone remodelling for the cementlessly implanted short-stem prosthesis being studied. The criteria for the qualitative assessment of the radiological findings stipulate that the assessor must have appropriate experience and deal systematically with the findings. This was implemented by means of an interobserver assessment, of which the radiological assessment criteria deviated from the radiological results of the two centers in just 1.4% of the individual zone values.
The manifestation of a neocortex as described by Morrey et al.7 in the predominately proximal-lateral region of the short-stem was recorded as a radiologically detectable, implant-adjacent sclerotic line <1 mm around the coated region of the short-stem in zones 1 and 2 and was also detected in the medial region of zone 7 in individual cases.
In general, a sclerotic line in the fixation area can be differentiated from the direct contact and visible alignment of trabecular structures on the fixation surfaces of the implant. The total percentage for these sclerotic lines of 19% and 10.5% in zones 1 and 2 respectively after an average of 4.9 years corresponds to the data published by Morrey et al.,7 which gives a percentage of 17% in Gruen's AP zone 1 (defined in an equivalent way) after an average follow-up period of 6.2 years.
In the distal short-stem region, functionally different, fine sclerotic lines are visible, which occur as a result of relative movements of the uncoated implant tip in the deformed bone-implant compound. It is also worth noting that the implant tip generally moves in a medial direction if force is applied to the bone-implant compound, as well as the fact that no pedestal formation was observed in a single case. For the interobserver assessment, there was a relatively high deviation of 2.5% in zones 4 and 5 in terms of the number of absolute case assessments for this specific radiological manifestation. We view this as being irrelevant as the prosthesis tip does not have a load-transferring function in these zones. The interobserver assessment showed a very good correlation of ±0.5% in all other periprosthetic zones.
For the assessment of short prosthesis stems, the hypertrophy induced by the prosthesis tip, found in the distal-lateral region of cortical zone 3, must be taken into consideration, as this could potentially cause problems for a secondary distal implant fixation and lead to associated pain.27
In this study, cortical hypertrophies were detected in seven cases (3.5%) in zone 3, and did not correlate to clinically-symptomatic pain symptoms. In two of these cases, a low-grade sclerotic zone was found in zones 1 or 2, which, in one case, was combined with a significant and otherwise rare hypertrophy in zone 5, which was very deeply resected (resection value of 67.7%) and was in the valgus position. Morrey et al.7 also observed hypertrophies in the distal lateral stem region but did not indicate a percentage value. Briem et al.9 reported a figure of 68% for sclerotic bone reactions in zone 3 without clinical abnormalities.
In previous follow-up examinations of our patients up to three years after the procedure, we did not detect any hypertrophies in zone 3. In their DEXA analyses, Lerch et al.28 even reported a significant reduction of the bone density in the corresponding AP zone 3 after two years. This should be explored in further detail as the formation of distal hypertrophies in cementless standard hip stems is known and this aspect appears to be important for the long-term radiological assessment of short-stems.
Lerch et al.28 also confirmed a significant increase of the bone density in zone 6. This had a radiological value of 97.5% in our collective study.
The initial movements of the short-stem under 5 mm, observed in seven cases in our collective study, have undergone secondary stabilization. The same applies for one case of significant subsidence of 9 mm, which was stabile after one year. This observation is also confirmed by the EBRA-FCA study with the same short-stem implant in a follow-up observation of 80 cases after an average of 2.7 years.29 We were unable to gather data for predicting the risk of potential subsidence, e.g. whether the resection height has an influence on this. The case analyses conducted by Braun et al.5 are consistent with the assessment that the stem size selected intraoperatively and the proximal-lateral support situation can affect the primary stability if the stem is implanted too deeply.
The absence of dislocations following predominate use of small 28 mm and 32 mm standard prosthesis heads in our study falls considerably below the average value of 3.2% which D'Angelo et al.30 determined in a review of published. After assessing the cup inclination, with inclinations over 50° in 9% of cases and anteversions over 20° in 3% of cases, we put the low number of dislocations down to the use of an anterolateral approach and the little iatrogenic muscle damage caused by this approach and stem implantation method. Good joint stability could be further promoted by ensuring that the stem anteversion and head position are anatomically correct and are not easily manipulated.
The short-stem treatment concept is described by most of the aforementioned authors as a less invasive and muscle-preserving procedure, although there has not yet been any clear evidence of these advantages in relation to standard stems.31
Conclusions
The positive mid-term clinical and radiological results, which do not show signs of loosening, generally confirm the metaphyseal fixation concept of the short-stem model being investigated in this study.
All necessary revision procedures could be performed with a standard hip stem.
Long-term results must be further observed on a prospective basis as part of this collective study.
References
- 1.Hallan G, Lie SA, Furnes O, et al. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br. 2007;89:1574–80. doi: 10.1302/0301-620X.89B12.18969. [DOI] [PubMed] [Google Scholar]
- 2.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish hip arthroplasty register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas W, Lucente L, Mantegna N, Grundei H. [ESKA (CUT) endoprosthesis] Orthopäde. 2004;33:1243–8. doi: 10.1007/s00132-004-0717-1. [Article in German] [DOI] [PubMed] [Google Scholar]
- 4.Ender SA, Machner A, Pap G, et al. Cementless CUT femoral neck prosthesis: increased rate of aseptic loosening after 5 years. Acta Orthop. 2007;78:616–21. doi: 10.1080/17453670710014301. [DOI] [PubMed] [Google Scholar]
- 5.Braun A, Sabah A. [Two-year results of a modular short hip stem prosthesis--a prospective study] Z Orthop Unfall. 2009;147:700–6. doi: 10.1055/s-0029-1185899. [Article in German] [DOI] [PubMed] [Google Scholar]
- 6.Ettinger M, Ettinger P, Lerch M, et al. The NANOS short-stem in total hip arthroplasty: a mid term follow-up. Hip Int. 2011;21:583–6. doi: 10.5301/HIP.2011.8658. [DOI] [PubMed] [Google Scholar]
- 7.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82:952–8. doi: 10.1302/0301-620x.82b7.10420. [DOI] [PubMed] [Google Scholar]
- 8.Gill IR, Gill K, Jayasekera N, Miller J. Medium term results of the collum femoris preserving hydroxyapatite coated total hip replacement. Hip Int. 2008;18:75–80. doi: 10.1177/112070000801800202. [DOI] [PubMed] [Google Scholar]
- 9.Briem D, Schneider M, Bogner N, et al. Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short-stem prosthesis. Int Orthop. 2011;35:655–60. doi: 10.1007/s00264-010-1020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Götze C, Ehrenbrink J, Ehrenbrink H. [Is there a bone-preserving bone remodelling in short-stem prosthesis? DEXA analysis with the Nanos total hip arthroplasty] Z Orthop Unfall. 2010;148:398–405. doi: 10.1055/s-0030-1250151. [Article in German] [DOI] [PubMed] [Google Scholar]
- 11.Zeh A, Weise A, Vasarhelyi A, et al. [Medium-term results of the Mayo™ short-stem hip prosthesis after avascular necrosis of the femoral head] Z Orthop Unfall. 2011;149:200–5. doi: 10.1055/s-0030-1270710. [Article in German] [DOI] [PubMed] [Google Scholar]
- 12.Molli RG, Lombardi AV, Jr, Berend KR, et al. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res. 2012;470:450–61. doi: 10.1007/s11999-011-2068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jerosch J. [Is shorter really better? Philosophy of short-stem prosthesis designs] Orthopäde. 2011;40:1075–83. doi: 10.1007/s00132-011-1848-9. [Article in German] [DOI] [PubMed] [Google Scholar]
- 14.Bücking PK, Feldmann PH, Wittenberg RH. [Metha - modular short-stem prosthesis] Orthopädische Praxis. 2006;42:474–8. [Article in German] [Google Scholar]
- 15.Fink U. Plasmapore: a plasma-sprayed micorporous titanium coating to improve the long term stability. In: Mainard D, editor. Acutalités en Biomatériaux. Vol. III. Paris: Romillat Edit; 1996. pp. 97–104. [Google Scholar]
- 16.Reigstad O, Franke-Stenport V, Johansson CB, et al. Improved bone ingrowth and fixation with a thin calcium phosphate coating intended for complete resorption. J Biomed Mater Res B Appl Biomater. 2007;83:9–15. doi: 10.1002/jbm.b.30762. [DOI] [PubMed] [Google Scholar]
- 17.Harris W. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by arthroplasty. An end-result study using an new method of result-evaluation. J Bone Joint Surg. 1969;51:737–55. [PubMed] [Google Scholar]
- 18.Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossifications following total hip replacement, incidence and a method of classification. J Bone Joint Surg. 1973;55:1629–32. [PubMed] [Google Scholar]
- 19.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990:107–28. [PubMed] [Google Scholar]
- 20.Gruen TA, McNeice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components. Clin Orthop. 1979;141:17–27. [PubMed] [Google Scholar]
- 21.Australian orthopaedic association national joint replacement registry annual report 2011, published online October 2011. Available from: http://www.dmac.adelaide.edu.au/aoanjrr/documents/AnnualReports2011/AnnualReport_2011_WebVersion.pdf.
- 22.Swedish hip arthroplasty register, annual report 2010. Available from: http://www.shpr.se/Libraries/Documents/AnnualReport-2010-eng.sflb.ashx.
- 23.Schmidutz F, Grote S, Pietschmann M, et al. Sports activity after short-stem hip arthroplasty. Am J Sports Med. 2012;40:425–32. doi: 10.1177/0363546511424386. [DOI] [PubMed] [Google Scholar]
- 24.Floerkemeier T, Tscheuschner N, Calliess T, et al. Cementless short-stem hip arthroplasty METHA® as an encouraging option in adults with osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2012;132:1125–31. doi: 10.1007/s00402-012-1524-5. [DOI] [PubMed] [Google Scholar]
- 25.Grupp TM, Weik T, Bloemer W, Knaebel HP. Modular titanium alloy neck adapter failures in hip replacement, failure mode analysis and influence of implant material. BMC Musculoskelet Disord. 2010;11:3. doi: 10.1186/1471-2474-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohler S, Ratayski H, Zacher J. [Implant-related fractures of the femoral neck cone adapter of a modular short-stem hip prosthesis-patient management and operative technique] Z Orthop Unfall. 2010;149:185–190. doi: 10.1055/s-0030-1250358. [Article in German] [DOI] [PubMed] [Google Scholar]
- 27.Ritter MA, Fechtman RW. Distal cortical hypertrophy following total hip arthroplasty. Arthroplasty. 1988;3:117–21. doi: 10.1016/s0883-5403(88)80076-7. [DOI] [PubMed] [Google Scholar]
- 28.Lerch M, von der Haar-Tran A, Windhagen H, et al. Bone remodelling around the Metha short-stem in total hip arthroplasty: a prospective dual-energy x-ray absorptiometry study. Int Orthop. 2012;36:533–38. doi: 10.1007/s00264-011-1361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmidutz F, Graf T, Mazoochian F, et al. Migration analysis of a metaphyseal anchored short-stem hip prosthesis. Acta Orthop. 2012;83:360–5. doi: 10.3109/17453674.2012.712891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.D'Angelo F, Murena L, Zatti G, Cherubino P. The unstable total hip replacement. Indian J Orthop. 2008;42:252–9. doi: 10.4103/0019-5413.39667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McElroy MJ, Johnson AJ, Mont MA, Bonutti PM. Short and standard stem prostheses are both viable options for minimally invasive total hip arthroplasty. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S68–76. [PubMed] [Google Scholar]


