Begun in 2005, an 18-month randomized clinical trial, culturally adapted an evidence-based dietary approach and exercise program to fit the female AfricanAmerican population. The study included 223 African-American women (120 in the experimental group). That group received education and instruction at 24 group sessions and recorded their daily food intake and physical activity. Controls received usual care (referral to a dietitian). After 18 months, the treatment group consisted of 12 women (attrition rate of 87%) who had begun the study low in self-efficacy.
Abstract
Introduction
African-American women are more overweight and have greater difficulty maintaining weight loss than do Caucasian women. Evidence suggests that African-American women are more successful with culturally tailored weight-loss programs.
Methods:
Begun in 2005, an 18-month randomized clinical trial, Project Take HEED (Healthy Eating and Exercise Decisions), culturally adapted an evidence-based dietary approach and exercise program to fit the female African-American population in an attempt to improve program attrition rates. The study was conducted with 223 African-American women (120 women in the experimental group; 103 controls), age 35 to 65 years, with a body mass index of 30 kg/m2 or higher. The experimental group received education and instruction at 24 group sessions and were asked to record their daily food intake and physical activity. Cultural adaptation included social and spiritual components. Controls received usual care (referral to a dietitian).
Results:
After 18 months, Project Take HEED demonstrated the following outcomes:
-
Attrition: the treatment group consisted of 12 African-American women at the end of month 18—(an attrition rate of 87%). (It had been 70% at the end of month 15.)
Factors contributing to attrition included: caregiver responsibilities, transportation difficulties, work schedules, and others.
Those clients that did remain, however, provided the impetus for our next study. The remaining participants had, by and large, begun the study as being low in self-efficacy regarding weight loss and weight loss maintenance
Conclusion:
Initial Findings: The high self-efficacy that some women had at the beginning of the intervention did not translate into the desired behavior change. The inverse relationship seen in this study suggests that treatments that improve participants’ self-efficacy may result in greater weight loss.
New Directions: A new study, commencing in 2013, will use at-home Web-based and virtual reality technology (avatars) in an attempt to enhance client motivation to persist in long-term weight management programs. Bandura’s pioneering work on self-efficacy will be the theoretical foundation of the pilot study, also enrolling African-American women.
Introduction
African-American women are more overweight and have greater difficulty maintaining weight loss than do Caucasian women.1–3 Evidence suggests that African-American women are more successful with weight-loss programs that are culturally tailored.4,5 At the same time, this racial group exhibits a higher attrition rate in weight-loss maintenance programs than any other population subset.3
A series of investigations at Kaiser Permanente (KP) Bedford Medical Offices in Ohio focused on the question “Why do African-American women, in particular, display high attrition rates in weight-loss maintenance programs?” Begun in 2005 as a randomized clinical trial, Project Take HEED (Healthy Eating and Exercise Decisions) was a combination of two interventions that had shown success in clinical trials with African Americans. The Therapeutic Lifestyle Changes (TLC) dietary approach from the National Cholesterol Program6 and the CHANGE (Change Habits by Applying New Goals and Experiences) exercise program7 were combined and culturally adapted to fit the population.
In an attempt to combat attrition of African-American women in weight-loss maintenance programs, the study objective was to determine the effectiveness of a culturally adapted intensive lifestyle intervention administered in a health care environment, relative to a control group that was provided standard lifestyle recommendations in producing and maintaining weight loss. Both groups were African-American women, age 35 to 65 years, who had a baseline body mass index (BMI) of 30 kg/m2 or higher.
We posed the following hypotheses: 1) Obese African-American women enrolled in a culturally adapted weight-loss program, consisting of nutrition, exercise, and behavioral interventions, will lose more weight over the 18-month period than those clients participating in a standard weight control program; 2) Self-efficacy among experimental group participants would contribute in a positive fashion from baseline to end of treatment; that is, those participants with an initially high sense of self-efficacy (confidence regarding attainment of desired outcomes) would have less difficulty losing weight than those with an initially low measure of self-efficacy.
In this research report, we describe the previously unpublished results of Project Take HEED and address the lessons learned from this 2005–2006 clinical trial. Additionally, we report on a new study that takes advantage of “nonimmersive virtual reality” in the form of commercially available avatars that morph to approximate the participant’s ideal self over time with sustained exercise and prescribed dieting. This technology serves as a potential mechanism to overcome the shortcomings of the original study by addressing long-term motivation to succeed in weight-loss maintenance programs. The new study, the SISTERS Weight Loss Maintenance study, will commence a one-year pilot program in mid-summer 2013. Like the earlier study, it is funded by the Garfield Memorial Foundation and is, in many ways, an extension of the previous work.
Methods
A series of investigations begun in 2005 at KP Bedford Medical Offices focused on the question “Why do African-American women, in particular, display high attrition rates in weight-loss maintenance programs?” First, we attempted a randomized clinical trial for 18 months from July 2005 to December 2006, termed Project Take HEED. The study originally recruited 223 female, adult African-American volunteer participants age 35 to 65 years with a BMI of 30 kg/m2 or higher. Participants were randomly assigned at baseline (T0) to either the experimental group or a statistically matched control group.
The experimental group consisted of 120 African-American women, age 35 to 65 years, with a BMI of 30 kg/m2 or higher, who, we predicted, would benefit from cultural adaptation of a standard weight-loss maintenance program. These clients completed a 3-day food record as grounds for inclusion in the study. The experimental group received education and instruction regarding the evidence-based practices intervention described later at 24 weekly group sessions (first weekly for 6 sessions, then semi-weekly). The control group was composed of 103 African-American women with the same demographic characteristics, who experienced usual care in the Ohio Permanente Medical Group (OPMG) in Northeastern Ohio. Usual care at the KP Bedford facility consisted of self-referral and/or referral by their primary care physician to a registered dietitian’s monthly information sessions.
Circa 2005, there remained a focus on short-term weight-loss programs in both clinical and commercial (nonprescription) settings. However, our research team suspected that sustainable weight loss was strongly associated with changes in lifestyle. Thus, the TLC program from the National Cholesterol Education Program6 was chosen as an instrument of education and change because of its 3-pronged approach consisting of diet, exercise, and weight management. In addition, the CHANGE exercise program7 was chosen to leverage the exercise portion of the overall approach, wherein 60 minutes of moderate exercise (eg, brisk walking) was recommended daily. In addition to these components, cultural adaptations included a spiritual dimension (“spiritual tablescapes”) and group support involving primarily African-American clinicians and staff. Experimental group clients were asked to record their food intake in a diet diary and their daily physical activity in an exercise log.
Dietary goals for the experimental group were to reduce weekly energy (caloric) intake by 3500 kcal/week, to reduce total fat intake to 25% to 30% of calories daily, and to reduce daily saturated fat intake to less than 70 kcal daily, with dietary cholesterol below 200 mg daily. Overall, the desired goal was to reduce body weight by more than 4% by the end of the study.
Exercise goals for the experimental group were to undertake a minimum of 360 minutes of rigorous exercise per week (60 minutes per day for 6 days), selected from a menu of options that included line dancing and brisk walking (supervised by a community-based instructor).
The intervention provided both a setting and a scheduled time for socialization through the formation of interpersonal bonds that would encourage exercise among the participants. In the group sessions, the experimental group was administered the TLC curriculum, which taught, for instance, the TLC diet, an individualized plan to reduce daily energy intake by 500 kcal. Group solidarity was also encouraged by a series of question-and-answer sessions. From the outset and with group consent, a nondenominational spiritual component was a segment of the group meetings. “Tablescapes” were created using various themes incorporating positive affirmations to facilitate a sense of contemplation and relaxation. Although not evidence-based, the inclusion of such a component did serve to enhance group cohesion (self-reported) among the women in the experimental group.
Seven months after initial enrollment (T1), the remaining participants in both groups were asked to return usable three-day food records (all columns completed).
A mix of validated self-efficacy measures was used to assess participants’ self-efficacy at various time points in the study. The three scales used were the Self-Efficacy for Fruit and Vegetable Intake survey,8 the Barriers to Exercise Self-Efficacy Scale,9 and the Weight Efficacy Lifestyle Questionnaire.10
A t test was used to compare groups by their scores on the self-efficacy scales. Repeated measures using a general linear model was performed to determine whether statistically significant differences occurred between the two groups in the mean amount of weight lost.
Results
At 7 months (T1), there were 108 remaining participants in both groups, with 45 of those in the control group. The experimental group consisted of 63 participants adhering to the weight-loss maintenance program, for an attrition rate of 48%. These remaining participants in the experimental group attended an average of 56% of the group sessions. At the end of month 15 (T4), the attrition rate in the experimental group was 70% (84 of 120 women had dropped out of the program).
After 18 months, Project Take HEED exhibited the following outcomes:
Attrition: The experimental group consisted of 12 African-American women at the end of month 18, an attrition rate of 90%. Factors contributing to attrition included caregiver responsibilities; transportation difficulties; work schedules; and, sporadically, lack of family support, especially from the significant other, regarding changes in lifestyle and appearance.
Self-Efficacy: The remaining participants, by and large, had begun the study as being low in self-efficacy regarding weight loss and weight-loss maintenance. That is, on the three scales used (Self-Efficacy for Fruit and Vegetable Intake survey, the Barriers to Exercise Self-Efficacy Scale, and the Weight Efficacy Lifestyle Questionnaire) the remaining participants had scored initially lower than did those “high-confidence” participants who later dropped out in large numbers (Table 1).
Table 1.
Project Take HEED results at various time pointsa
| Measure | T0 (controls: n = 103, experimental: n = 120) | T1 (controls: n = 45, experimental: n = 63) | T4 (controls: n = 37, experimental: n = 36) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fruit and veggie SE | Exercise efficacy barriers | WEL total | BMI (kg/m2) | Fruit and veggie SE | Exercise efficacy barriers | WEL total | BMI (kg/m2) | Fruit and veggie SE | Exercise efficacy barriers | WEL total | BMI (kg/m2) | |
| Controls, mean | NA | NA | 6.15 | 37.25 | 2.11 | 45.03 | 6.06 | 37.55 | 2.33 | 41.51 | 5.72 | NA |
| Experimental group, mean | 2.24 | NA | 6.03 | 38.06 | 2.19 | 50.12 | 6.41 | 38.53 | 2.13 | 49.12 | 6.63 | 38.16 |
| t test | 0.5 | 1.18 | 1.15 | 0.9 | 1.15 | 2.59 | ||||||
| p value | 0.62 | 0.24 | 0.26 | 0.37 | 0.13 | 0.01 | ||||||
In the Take HEED study, a mix of validated self-efficacy measures was used, with results noted at baseline (T0), 7 months (T1), and 15 months (T4). Body mass index (BMI) measures were inconclusive and not statistically significant. On the 3 scales used, Self-Efficacy for Fruit and Vegetable Intake Survey (Fruit and veggie SE), the Barriers to Exercise Self-Efficacy Scale (Exercise efficacy barriers), and the Weight Efficacy Lifestyle (WEL) Questionnaire, the remaining participants at T4 had scored initially lower than those “high-confidence” participants, who later dropped out in large numbers.
BMI = body mass index; HEED = Healthy Eating and Exercise Decisions: NA = not applicable; SE = self-efficacy; WEL = weight efficacy lifestyle.
Repeated measures using a general linear model showed no statistically significant difference in the mean amount of weight lost between the two groups over time. Any further statistical analysis (multivariate analysis) would have produced statistically insignificant results because of the high attrition rate among both groups and the resultant small sample size.
Discussion
There was an initial outpouring of interest in the weight management program; all 120 persons in the experimental group attended the general information session. However, attendance rapidly dropped off so that by the end of month 18, there remained only 12 persons in the experimental group who were completing usable 3-day food records.
The counter-intuitive results of Project Take HEED regarding self-efficacy were similar to the later findings of other researchers, who concluded that “high self-efficacy for weight loss before treatment may be detrimental to success … whereas the treatments that improve participants’ self-efficacy may result in greater weight loss.”11
The intervention in this study used an education and information approach, which subsequent researchers (eg, Annesi12) also found to be insufficient in changing ingrained behavior.
Lessons Learned
We arrived at the following lessons learned from this trial:
A sustainable weight-loss program for African-American women must account for realistic goal setting and expectations, particularly among those with initially high self-esteem.
Although social cohesiveness was added to the standard obesity weight management curriculum in our intervention, more emphasis on this aspect should be added at the outset of any future weight-loss maintenance program.
Dietary and exercise education is insufficient; behavioral change and lifestyle interventions are important components of any successful weight-loss management program.
The high self-efficacy that some women had at the beginning of the intervention did not translate into the desired behavior change. Although self-efficacy is important, the inverse relationship described here must be accounted for in future weight-loss management programs involving this population.
Looking Forward
On the basis of findings of Project Take HEED, we reviewed other researchers’ work related to self-efficacy and behavior change. Martin et al13 reported: “For subjects in the [experimental group] intervention, baseline self-efficacy was predictive of subsequent weight change [in an inverse manner] … . Because increased self-efficacy was associated with greater weight loss, it is possible that treatments that attempt to improve patient’s self-efficacy may prove beneficial for treatment outcomes.” In related research, Bandura14 showed that a self-efficacy enhancement program proved markedly beneficial in clients with substance abuse or smoking behaviors.
Dietary and exercise education is insufficient; behavioral change and lifestyle interventions are important components of any successful weight-loss management program.
At KP Bedford, we theorize that if we could find the staff and/or the behavioral mechanism to help us to improve self-efficacy among African-American women enrolled in a weight-loss program, we might be able to demonstrate long-term successful results. Fortunately, with emergent technologies, we may have found just such a mechanism in the form of nonimmersive virtual reality technologies. If properly engineered, these technologies will enable our clients to perceive their “Ideal Selves” in such a way as to encourage adherence to a weight management program—the focus of our next effort, a funded 12-month pilot study.
Thus, we will employ commercially available avatars, customized in such a way as to enhance motivation of the client in her own home setting and encourage her to adhere to the regimen she had initially agreed to through a behavioral contract. The approved pilot study envisions the use of weight management interventions—particularly the use of Web-based and virtual reality technology—to help supply the “missing link” of enhanced client motivation to engage in long-term weight management programs and thus sustain weight loss over the long term. (It is known how to produce short-term weight loss.) The specific purpose of the research project is to evaluate the effectiveness of a technology-based, virtual reality lifestyle intervention for obese primary care clients: African-American women age 35 to 65 years, with an elevated BMI of at least 30 kg/m2.
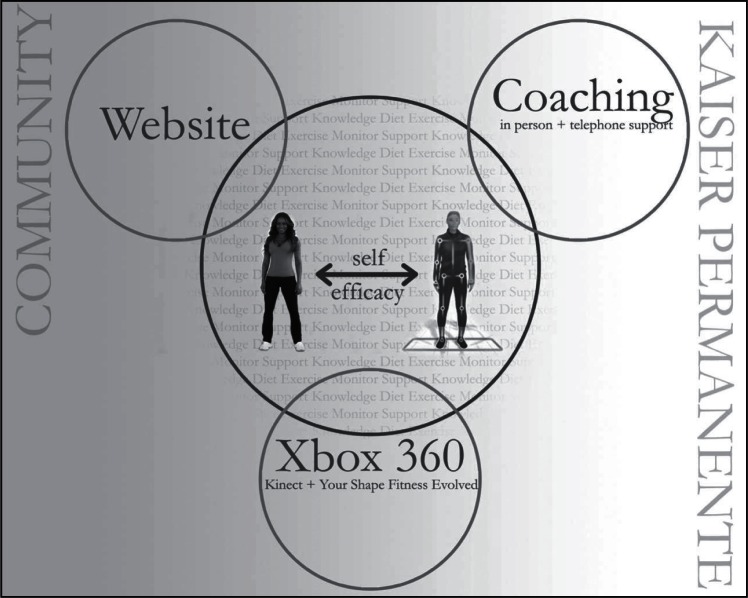
We will do this by combining several aspects of weight management intervention: for instance, computer-tailored nutrition and exercise education, coaches/monitors, and the use of customized, commercially available, nonimmersive virtual reality products such as “Your Shape Fitness Evolved 2012,” “Just Dance” (both from Ubisoft, Inc, San Francisco, CA), and Xbox 360 Kinect (interactive device from Microsoft, Redmond, WA) (Figure 1). This systematic approach to weight-loss management uses what is known from research about primary care obesity treatment and what can be hypothesized from the available technology, as demonstrated in Figure 2. Because this technology is nonimmersive virtual reality, the participant is aware that, in some respects, she is entering a virtual world, a world that in our experience and that of others reported in the research literature15 is quite enjoyable and engaging for the participant.
Figure 1.
The user experience: hardware (Xbox Kinect 360) and software (Ubisoft’s “Your Shape Fitness Evolved”).
The SISTERS Weight-Loss Management program will develop a behavioral management system for managing obesity that incorporates active use and monitoring of motion detection-based fitness coaching and training tools. The motion detection technology is comprised of two components: the hardware and the software. The hardware is made up of the Xbox and the Kinect, which detects and tracks participant movement. The software component is the Xbox game “Your Shape Fitness Evolved,” from Ubisoft, Inc, which uses the hardware to place the participant’s full likeness (avatar) into a virtual gym class.
© 2012 Ubisoft Entertainment. All Rights Reserved. Your Shape logo, Ubisoft, and the Ubisoft logo are trademarks of Ubisoft Entertainment in the US and/or other countries.
Figure 2.
User’s experience regarding the Web site, the avatar-Xbox device, and the resultant impact on self-efficacy are displayed. Also displayed is the role of the coach/mentor in the home setting.
In addition to the principal investigator from the original Project Take HEED study (Pamala Murphy, MD), our research team includes the University of Pittsburgh Medical School, a national leader in the field of obesity treatment, and, specifically, the Diabetes Prevention Program (Chief Investigator, Kathleen M McTigue, MD, MPH, MS). This diabetes prevention program will be delivered to study participants by means of a Web site and mediated by coaches, mentors, and group study sessions, as described earlier. Laurey R Simkin-Silverman, PhD, also of the University of Pittsburgh, is an expert in both behavior modification techniques and external evaluation mechanisms.
Regarding Self-Efficacy: there are two hypothesized conditions in the proposed study:
For those who start out low in self-efficacy, they can build self-efficacy, both internally (“Your Shape Fitness Evolved” program) and externally, by belonging to a group of like-minded individuals aided and facilitated by health care professionals and an evidence-based curriculum (the Diabetes Prevention Program).16,17
For those high in initial confidence that they can succeed, their interest will be enhanced by the avatar, and their overconfidence will be kept in check by the on-board metrics of both the Web-based Diabetes Prevention Program and the metrics provided by the Xbox Kinect portion of “Your Shape Fitness Evolved” (BMI changes, calories burned, food intake portions, etc).
Thus, we believe that both groups, those high in initial self-confidence and those who are not, will realize an overall increased motivation to persist in the program via the mechanisms just described. In terms of social networking, also a critical element of program success, both devices, the Diabetes Prevention Program Web site and the Xbox controller, contain social networking capabilities, which we plan to use.
The short-term goals of the SISTERS Weight-loss Maintenance pilot study, to commence in May 2013, are as follows:
Assess the usability of the non-immersive technology with participants and caregivers.
Examine the impact on self-efficacy with respect to weight loss in the pilot study’s population.
Begin to examine (through focus groups, etc), the impact of culture, race, and home environment as inhibiting or enabling variables in weight-loss maintenance among this population.
Demonstrate, ideally, a drop of 8% or greater in participants’ BMI, with a corresponding decrease in waist circumference, over the full 12 months of the project.
After completion of this pilot study, we believe we can demonstrate both experience with the customized technology/intervention package (“off the shelf” and ready to go) and the expertise of the team assembled to work on the project. This should position us well for an R01 grant application to the National Institutes of Health under the National Heart, Lung and Blood Institute’s Funding Opportunity Program Announcement (PA 11-211), “Virtual Reality Technologies for Research and Education in Obesity and Diabetes.” This research, in turn, could be followed by additional study funding applications extending the project to 7 or 8 years total and involving other KP Regions and coinvestigators (also followed by newer applications of the technology, as they become available).
Acknowledgments
We would like to acknowledge the Garfield Memorial Fund, both in providing original funding for Project Take HEED, and for funding the soon-to-commence SISTERS Weight Loss Management study, as above.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
This research was funded and supported by the Kaiser Permanente Garfield Memorial Fund.
Preventable
Except for smoking, obesity is now the number one preventable cause of death in this country. Three hundred thousand people die of obesity every year …
—C Everett Koop, MD, 1916 – 2013, American pediatric surgeon and public health administration, former US Surgeon General
References
- 1.Flegal KM, Carroll MD, Kucmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1999 Jan;22(1):39–47. doi: 10.1038/sj.ijo.0800541. DOI: http://dx.doi.org/10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 2.Kumanyika SK, Obarzanek E, Stevens VJ, Hebert PR, Whelton PK. Weight-loss experience of black and white participants in NHLBI-sponsored clinical trials. Am J Clin Nutr. 1991 Jun;53(6 suppl):1631S–38S. doi: 10.1093/ajcn/53.6.1631S. Erratum in: Am J Clin Nutr 2003 May; 77(5):1342. Kumanyaka SK [Corrected to Kumanyika SK]) [DOI] [PubMed] [Google Scholar]
- 3.Kumanyika SK. Obesity treatment in minorities. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. Guilford, NY: Guilford Press; 2002. pp. 416–46. [Google Scholar]
- 4.Davis Martin P, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American Women. Obesity (Silver Spring) 2006 Aug;14(8):1412–20. doi: 10.1038/oby.2006.160. DOI: http://dx.doi.org/10.1038/oby.2006.160. [DOI] [PubMed] [Google Scholar]
- 5.Noar S, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007 Jul;133(4):673–93. doi: 10.1037/0033-2909.133.4.673. DOI: http://dx.doi.org/10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 6.Expert Panel on Detection, Evaluation Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001 May 16;285(19):2486–97. doi: 10.1001/jama.285.19.2486. DOI: http://dx.doi.org/10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 7.Moore SM, Charvat JM, Gordon NH, et al. Effects of a CHANGE intervention to increase exercise maintenance following cardiac events. Ann Behav Med. 2006 Feb;31(1):53–62. doi: 10.1207/s15324796abm3101_9. DOI: http://dx.doi.org/10.1207/s15324796abm3101_9. [DOI] [PubMed] [Google Scholar]
- 8.Ma J, Betts NM, Horacek T, Georgiou C, White A, Nitzke S.The importance of decisional balance and self-efficacy in relation to stages of change for fruit and vegetable intakes by young adults Am J Health Promot 2002January–Feb163157–66.DOI: http://dx.doi.org/10.4278/0890-1171-16.3.157 [DOI] [PubMed] [Google Scholar]
- 9.McAuley E, Katula J, Mihalko SL, et al. Mode of physical activity and self-efficacy in older adults: a latent growth curve analysis. J Gerontol B Psychol Sci Soc Sci. 1999 Sep;54(5):P283–92. doi: 10.1093/geronb/54b.5.p283. DOI: http://dx.doi.org/10.1093/geronb/54B.5.P283. [DOI] [PubMed] [Google Scholar]
- 10.Dutton GR, Martin PD, Rhode PC, Brantley PJ. Use of the weight efficacy lifestyle questionnaire with African American women: validation and extension of previous findings. Eat Behav. 2004 Nov;5(4):376–84. doi: 10.1016/j.eatbeh.2004.04.005. DOI: http://dx.doi.org/10.1016/j.eatbeh.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res. 2004 Apr;12(4):646–51. doi: 10.1038/oby.2004.74. DOI: http://dx.doi.org/10.1038/oby.2004.74. [DOI] [PubMed] [Google Scholar]
- 12.Annesi JJ. Supported exercise improves controlled eating and weight through its effects on psychosocial factors: extending a systematic research program toward treatment development. Perm J. 2012 Winter;16(1):7–18. doi: 10.7812/11-136. DOI: http://dx.doi.org/10.7812/TPP/11-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res. 2004 Apr;12(4):646–51. doi: 10.1038/oby.2004.74. DOI: http://dx.doi.org/10.1038/oby.2004.74. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Self-efficacy: the exercise of control. New York, NY: W H Freeman and Company; 1997. p. 21. [Google Scholar]
- 15.Riva G. The key to unlocking the virtual body: virtual reality in the treatment of obesity and eating disorders. J Diabetes Sci Technol. 2011 Mar 1;5(2):283–92. doi: 10.1177/193229681100500213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diabetes Prevention Program Outcomes Study (DPPOS) questions and answers [monograph on the Internet] Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2009. Oct, [cited 2012 Nov 27] Available from: www2.niddk.nih.gov/Research/ClinicalResearch/DPPOS/QA.htm. [Google Scholar]
- 17.McTigue KM, Conroy MB, Hess R, et al. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemed J E Health. 2009 Nov;15(9):851–8. doi: 10.1089/tmj.2009.0036. DOI: http://dx.doi.org/10.1089/tmj.2009.0036. [DOI] [PubMed] [Google Scholar]