Social determinants of health are increasingly being recognized for their relationship to the soaring incidence of Type 2 diabetes in the US. Interventions focus on biologic and behavioral factors, such as symptoms, diet, and physical activity. It is equally important to address the influence of physical and social environments on health outcomes: low income, employment insecurity, low educational attainment, and poor living conditions. The Patient Protection and Affordable Care Act of 2010 offers an opportunity to improve data collection and policy development.
Abstract
Social determinants of health are the conditions in which individuals are born, grow, live, work, and age. Increasingly, they are being recognized for their relationship to the soaring incidence of Type 2 diabetes in the US, as well as the opportunities they present for us to counter it. Many current Type 2 diabetes interventions focus on biologic and behavioral factors, such as symptoms, diet, and physical activity. However, it is equally important to address the influence of physical and social environments, which may include low income, employment insecurity, low educational attainment, and poor living conditions, on health outcomes. Section 4302 of the Patient Protection and Affordable Care Act of 2010 offers an opportunity to improve data collection and policy development to more effectively identify populations at high risk for developing Type 2 diabetes and to proactively refer them to appropriate social support services that may ultimately support reduction of health disparities. Expanding the scope of this legislation to include data that incorporate social determinants would improve the ability of clinicians and health systems to engage and to treat patients with chronic conditions, such as Type 2 diabetes, while expanding policymakers’ ability to conform to the legislation’s intent of shaping efforts to reduce chronic conditions nationwide.
Introduction
Recent health reform efforts offer many segments of the US population at highest risk for developing chronic conditions opportunities for improved and coordinated medical care through new insurance coverage and innovative care arrangements. Yet, with some notable exceptions, health reform measures did not go far enough to systematically identify metrics to support the development of policies and the allocation of resources for populations at risk for chronic conditions. Research has demonstrated that social determinants are associated with the disproportionate development of chronic conditions and challenges encountered when managing them; this is particularly true of Type 2 diabetes, which will be used to illustrate concepts throughout this article.1–12 Clinical interventions have consistently evolved to improve disease management, particularly as a growing number of clinicians recognize the importance of social determinants of health (eg, income, education, housing, and access to nutritious food) and their contribution to health disparities.12–16
However, to further challenge the underlying nonmedical social and environmental contributors to chronic conditions, a focus on the individual within a systems perspective is necessary. On a systems level, this requires two vital building blocks: 1) data that accurately capture social determinants of health, and 2) policies that both intersect public health principles and practice and promote linkage of social determinants to health care delivery. Although part of the structure to fulfill these requirements already exists, the multifactorial complexity of chronic conditions, such as Type 2 diabetes, requires additional targeted activities to further advance efforts to prevent and to manage them.
Diabetes as a Public Health Issue
In 2010, Type 2 diabetes accounted for more than 95% of the 25 million patients with diabetes in the US, and an additional 79 million individuals were estimated to be prediabetic.17,18 In 2007, the annual economic burden of diabetes was estimated at $174 billion, with $116 billion in excess medical expenditures and $58 billion in reduced productivity.17 Diabetes also takes a toll on the health care system, as 1 in 10 health care dollars is attributed to it.18 Average medical expenses for patients with diabetes are nearly twice as high as those for patients who do not have diabetes.18 Additionally, Type 2 diabetes is more prevalent in minority races and ethnicities, as evidenced by Hispanics having a 66% greater risk, and non-Hispanic blacks having a 77% greater risk for developing it than non-Hispanic whites.17,18
As Type 2 diabetes approaches an epidemic level in our country, its increase is typically attributed to biologic characteristics and behavioral influences (further discussed in the Influence of Social Determinants on Type 2 Diabetes section).19 Biologic factors are related to genetic predispositions for the condition or treatment for other medical conditions and include factors such as age, family history, testosterone deficiency, and use of atypical antipsychotics or statins.19–23 Behavioral influences include factors such as physical inactivity and inadequate sleep.1,2,19,24 Although complex, the relationship between Type 2 diabetes and obesity is multifactorial and can further complicate prevention and management.25 Type 2 diabetes is also associated with many other comorbid complications, such as hypertension, cardiovascular disease, stroke, kidney failure, and blindness, further intensifying health care utilization and associated expenditures.17 With nearly 2 million new cases diagnosed annually, Type 2 diabetes is a costly public health issue that challenges our capacity to respond at the patient level in a comprehensive and systemwide manner.17
Current Type 2 Diabetes Interventions
In the absence of a cure for Type 2 diabetes, conventional treatment strategies have typically combined clinical interventions that manage the condition or minimize symptoms with behavioral modifications, including dietary improvements, increased physical activity, and closely monitored medication regimens.12,18,26–28 In the short term, these efforts aim to lower blood glucose levels, while long-term goals are centered on mitigating further complications, morbidity, and premature mortality associated with the condition.19 Research has demonstrated that the contributions of clinical factors and behavioral choices to prevention and management of Type 2 diabetes do not adequately explain poor diabetes-related health outcomes, particularly among those with lower socioeconomic status.28,29
Some approaches to prevention and management of Type 2 diabetes have attempted to address selected barriers that stem from social determinants, such as, culturally adapted interventions, community health workers, and financial assistance for clinical treatment and behavioral changes.12–16 In other notable approaches to care delivery, such as the Chronic Care Model, clinical supports are paired with a more holistic view of chronic condition management, particularly with respect to promoting the use of community resources to meet patient needs.30 Although this model calls for clinical information systems, it does not discuss the importance of collecting and assessing information on the nonmedical factors that contribute to chronic conditions.
Many Type 2 diabetes interventions are limited in their capacity to account for the influence of physical and social factors (such as low income, employment insecurity, low educational attainment, and poor living conditions) on behavioral practices.1,3,28,31,32 If future interventions neglect to incorporate a broader social lens, they will fail to sustainably address the necessary population-based changes essential to mitigate the incidence and long-term effects of this condition for the patient and for society. To accomplish this, we must capitalize on the current gaps in Type 2 diabetes prevention and management by systematically collecting data on nonmedical factors and using this information to enhance health policies and current interventions.
The Influence of Social Determinants on Type 2 Diabetes
Complex factors in the physical and social environments affect health. These elements, collectively known as the social determinants of health,33 can be viewed as the primary influencers and best predictors of health outcomes at the individual and at the population level.29,34–39 As evidenced by accumulated international and domestic research, social determinants (such as income, education, housing, and access to nutritious food) are central to the development and progression of Type 2 diabetes.1–10 Moreover, the incidence and prevalence of Type 2 diabetes appear to be socially graded, as individuals with lower income and less education are 2 to 4 times more likely to develop diabetes than more advantaged individuals.24,40–44 If the role of social determinants is not sufficiently addressed in chronic condition management, they will continue to be a key barrier to the improvement of population health.3
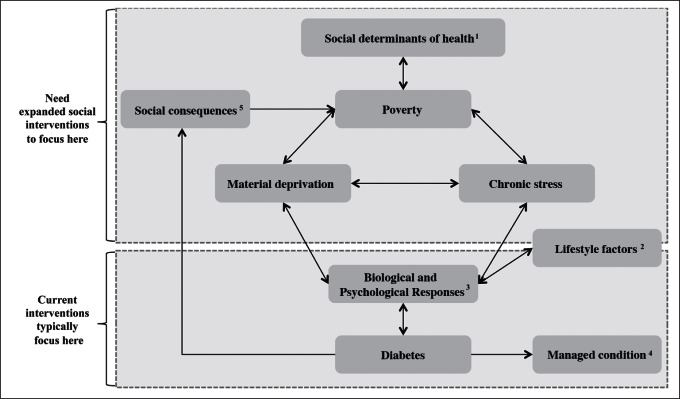
As illustrated in Figure 1, Type 2 diabetes is part of a cyclical process: it both results from and contributes to adverse outcomes. Poverty and material deprivation, defined as a lack of resources to meet the prerequisites for health, may play a key role.3 For disadvantaged individuals, the constant scramble to make ends meet results in high levels of chronic stress, spurring both psychological and biologic responses.33,45 Chronic stress can lead to increased depression and anxiety, reduced self-esteem, and decreased energy and motivation, which amplify the likelihood of self-destructive behaviors and choices (eg, tobacco use, excessive alcohol intake, and consumption of unhealthy foods).34,46 The physical manifestation of chronic stress leads to the negative consequence of allostatic load, which includes increased blood pressure, cortisol, and blood glucose levels, as well as impaired ability to effectively respond to future stressors.35,46,47 Over time, these physiologic reactions, coupled with detrimental psychological responses, and behavioral practices increase the likelihood of obesity and Type 2 diabetes.35
Figure 1.
The sociobiologic cycle of diabetes.
1Social determinants of health encompass factors such as income, education, housing, and access to nutritious food.
2Lifestyle factors incorporate dietary choices, physical activity levels, and access to primary health care services.
3Biologic responses refer to increased allostatic load, cortisol, blood pressure, and blood glucose levels, while psychological responses connote increased depression and anxiety, as well as decreased self-esteem, energy, and motivation.
4Managed condition implies individuals are able to ensure their diabetes is approximately controlled by clinical standards.
5Social consequences include increased health care costs and employment complications, as well as decreased productivity and educational attainment potential.
Type 2 diabetes can be particularly problematic among less advantaged patients for several reasons. First, the personal financial burden of increased health care costs can further intensify the effects of poverty, particularly because it consumes a greater portion of income (as compared with those who have greater financial resources).48 Second, a disadvantaged individual may not have sufficient access to the resources necessary to manage the condition, such as adequate housing, nutritious food, and health care services.5,9 Third, diabetes can decrease an individual’s productivity at work or limit educational attainment, particularly if left unmanaged, which can lead to further employment-related problems.49 These conditions exacerbate the cycle of inequality, as they lead to further poverty, material deprivation, and social exclusion if disadvantaged individuals are left to fend for themselves.50
Because the interactions between humans and their environment can be reciprocal, such that humans have the ability to both shape and be influenced by their environment, improving prevention and management of chronic conditions requires a coordinated, multilevel approach.51–53 A recent Institute of Medicine (IOM) report entitled “Living Well With Chronic Illness” suggests combining interventions focused on meeting the needs of higher-risk population segments and individual patients to most effectively support strategies for preventing and managing Type 2 diabetes.54 Focusing on the interrelated social causes that are at the root of health inequalities (Type 2 diabetes disproportionately affecting those with low socioeconomic status) is one approach that can be used to mitigate health disparities. By addressing the primary elements that affect individuals and lead to poverty, such as low income and employment insecurity, low educational attainment, and poor living conditions (Figure 1), population-based approaches for the management and prevention of Type 2 diabetes become sustainable.1,32,43,46,48 Reducing these inequalities benefits society, health systems, and clinicians from public health, ethical, and economic standpoints.4 Capitalizing on the central role of data collection in guiding policy to effectively support clinical practice in the allocation of health and social support resources is critical to comprehensively address the nonmedical characteristics affecting human health.55
Systematic Collection of Social Determinants Data
Investing in social support policies that improve income instability, low educational attainment, inadequate housing, and food insecurity is essential to enhance the impact of clinical interventions and overall health outcomes, particularly with regard to Type 2 diabetes.1,32,46,56,57 To guide local, state, and national policies that address health disparities resulting from social determinants, we must first measure the nonmedical factors that contribute to the development of chronic conditions. The Patient Protection and Affordable Care Act of 2010 (PPACA) has further expanded support for those with financial constraints and preexisting conditions through improved access to health care services in the US.58 Additionally, the PPACA has recognized the need for more comprehensively assembled national data to measure and address racial and ethnic health disparities. Section 4302 of the legislation requires the standardized collection of data in five categories of nonmedical factors (race, ethnicity, sex, primary language, and disability status) by all federally funded or federally sponsored population health surveys and health entities, such as Medicare, Medicaid, and the Children’s Health Insurance Program.59 According to the Department of Health and Human Services, the purpose of uniformly gathering and reporting these data is to improve the ability to identify health disparities and ultimately develop interventions to better address them.60
Although these national data standards may prove beneficial in addressing the problem, Section 4302 falls short in the effort to collect the data necessary for adequate and sustainable reduction of health disparities. In addition to the five mandated categories, research supports linking social variables to health disparities associated with the development of chronic conditions, such as Type 2 diabetes.3,6,29 If four additional categories related to social determinants—income, education, housing, and food security—were included as national data standards, both health systems and policymakers could use these data in ways that more fully conform to the intent of the legislation. Questions from these categories, detailed in Table 1, could also be considered prototypes for inclusion in other population-based data survey systems, as they were validated and derived from the American Community Survey and the Food Security Survey component of the Current Population Survey.61,62 Although the US collects some data on social determinants in current population-based health surveys, such as the National Health Interview Survey and the Medical Expenditure Panel Survey, the information is collected as part of a statistical sample. Our suggested additional questions could be used at the individual level and linked with health conditions to make more accurate, real-time clinical and health system decisions. The recommended additional categories and corresponding questions complement current data collection and reporting standards and provide a more comprehensive picture of the extent to which sociodemographic conditions affect health outcomes.
Table 1.
Recommended additional data collection categories and questions for Section 4302 of the Patient Protection and Affordable Care Act
| Category | Question |
|---|---|
| Income1 | Annual household income? |
| Household size? | |
| Unemployment in last 12 months? | |
| Education1 | Highest level of education completed? |
| Attended school/college in last 3 months? | |
| Housing1 | Rent, own, or occupy? |
| Monthly rent or mortgage? | |
| Number of bedrooms in home? | |
| Food security2 | Cut meal size/skip meals because there was not enough money in last 12 months? |
| Afford to eat balanced meals in last 12 months? | |
| Receive government food assistance (eg, food stamps, SNAP)? |
SNAP = Supplemental Nutrition Assistance Program.
The American Community Survey [monograph on the Internet]. US Department of Commerce. United States Census Bureau, Economics and Statistics Administration; 2011 [cited 2011 Nov 6]. Available from: www.census.gov/acs/www/Downloads/questionnaires/2011/Quest11.pdf.
Coleman-Jensen A, Nord M, Andrews M, Carlson S. Household food security in the United States, 2010 [monograph on the Internet]. Economic Research Services Report, 125. Washington, DC: Department of Agriculture; 2011 Sep [cited 2011 Nov 6]. Available from: www.ers.usda.gov/Publications/ERR125/err125.pdf.
With the abundance of research linking social determinants of health to the development of Type 2 diabetes and other chronic conditions, the omission of these recommended variables from Section 4302 is perplexing. There may have been concerns about the validity of self-reported data, the ability to effectively measure data in these additional categories, the cost of mandating collection of data with additional questions, or the slippery slope of asking sensitive questions that could potentially be viewed as intrusive. However, the US has a long tradition of relying on self-reported data, as evidenced by the decennial census.63 The recommended additional categories and questions are derived from current research-validated surveys and can be used in a de-identified format to protect the privacy of respondents and aggregated to analyze effects at the population level.64 Furthermore, by including these socioeconomic variables we will publicly recognize the role that income instability, low educational attainment, inadequate housing, and food insecurity currently play in disease development.
Policies to Address the Social Determinants of Type 2 Diabetes
Expansion of standardized data collection under recent PPACA legislation can result in more effectively realizing the effect socioeconomic disparities have on the development of chronic conditions in the US. Future sustainable Type 2 diabetes interventions must incorporate horizontal and vertical polices anchored in integrated data, such as the recommended data categories described here, to address the complex relationship between Type 2 diabetes and social determinants of health. Horizontal policies, which seek to improve health through condition-specific interventions, should incorporate this enhanced data in the health system to more comprehensively address the multiple social risks individuals with Type 2 diabetes experience. Vertical policies that aim to improve social and economic standing should be rooted in this integrated data to advance understanding of the link between social factors and chronic conditions, ideally leading to systemic modifications to mitigate adverse effects of chronic conditions.65 Past Type 2 diabetes interventions have primarily focused on horizontal policies; however, the swiftly growing public health problem of diabetes necessitates additional investment of resources and research in vertical policies.
Current horizontal policies could expand upon condition-specific interventions by first gathering the recommended data for use in health care organizations and clinical settings. In terms of Type 2 diabetes management, this additional data could ideally be systematically collected for each patient and incorporated into electronic medical records. Health care organizations could use these data to strategically connect information about the social environment and health conditions of patients, thereby enabling longitudinal analyses linking social determinants to the development of Type 2 diabetes and other chronic conditions. Similarly, clinicians could begin to tailor self-management recommendations to individual patients’ needs, particularly in terms of income, education, housing, and access to nutritious food. For example, understanding the extent to which an individual’s income is sufficient to provide for household members, or whether an individual can afford to eat or has access to balanced meals can be important information for the clinician. Such information would also be critical to developing an appropriate referral and decision-support system necessary to manage chronic conditions and reduce poor health outcomes at the population level.
Vertical policies should connect clinical resources with broader social support services and would ideally originate with concerted data collection efforts by health systems and state and federal governments. It can be difficult for clinicians to factor the effect of these services into their treatment decisions without added guidance from health systems and policymakers, who have the ability to develop the broader approaches needed to mitigate adverse health effects of social determinants. By building upon the “health in all policies” approach endorsed by the IOM, vertical policies rooted in the recommended integrated data also recognize the important interrelationships between health and government policies.54 These data could be critical to connect vulnerable populations with the necessary resources that have the potential to alter detrimental sociobiologic processes that foster complex chronic conditions, such as Type 2 diabetes. Health systems and governments could also use these comprehensive data to guide the development of system policies, resource allocation, referral processes, and partnerships with community organizations and social support programs.
The greatest impact of horizontal and vertical policies can be realized when both types of policies are used to complement one another. For example, at the clinic and health care organization level, horizontal policies could initiate collection of the recommended data for each patient and incorporate it into electronic medical records. Innovative managed care organizations could then develop vertical policies that use this information to proactively identify patient populations that may particularly benefit from strategically placed resources to better manage their health. These efforts could conceptually align with integrated care models (such as patient-centered medical homes, community-oriented primary care centers, and accountable care organizations) that seek to integrate health and social services for patients who are at higher risk for developing Type 2 diabetes or who are having difficulty managing the condition.
These patient-centered models of care delivery use a team-based approach focused on the needs of patients and, when appropriate, their families. Depending on the practice, this team could include primary care physicians, nurse practitioners, physician assistants, mental health practitioners or behavioral health specialists, social workers, care coordinators, pharmacists, palliative care clinicians, physical and occupational therapists, community health workers, and other professionals offering support services in the broader community.66 Because the care team is diverse and extends into the community, readily available data about patients’ income, education, housing, and food security could be used by clinicians and health systems to proactively refer patients and their families to appropriate resources. This includes, but is not limited to, social workers who can assist in obtaining subsidized health insurance for those with low income, health educators who can provide assistance to those with low health literacy, social support services to help find adequate housing for those who need more stable home environments, and local public health or community resources to assist in ensuring adequate access to healthy and nutritious food.
Discussion
To assess which health and social policies are ultimately the most successful in mitigating Type 2 diabetes, data collection and research capacity in the US should be strengthened to collectively analyze social, economic, and biologic factors more effectively.32 Collection of standardized and comprehensive sociodemographic and health data allows clinicians, health systems, researchers, and policymakers to better understand the effects of these factors on US health outcomes, particularly with regard to Type 2 diabetes. Integrated data can inform health systems and policymakers about the considerable extent to which these factors ultimately influence poor health status, particularly with regard to chronic conditions.
Most significantly, these data will enable more effective and proactive identification of levers of change to guide the allocation of limited resources, set objectives and targets for interventions, plan effective treatment, refer patients to appropriate social resources, and comprehensively evaluate the effectiveness of health and social policy interventions at both patient and systemwide levels. Integrating these recommended data categories into a seamless data collection effort at the individual clinic and health system level through expanded horizontal policies can promote greater recognition of the influence of social determinants on health conditions such as Type 2 diabetes. Additionally, these data serve as an impetus for developing vertical policies that foster broader, more integrated interventions affecting both clinical outcomes and patient well-being on a more concerted basis.
As the IOM suggests, addressing health-related socioeconomic factors increases both the sustainability and impact on overall health of efforts to prevent and manage chronic conditions, particularly Type 2 diabetes (Figure 1). According to the IOM, “an aligned system with a strong interface among public health, health care, and the community and nonhealth sectors could produce better prevention and treatment outcomes for populations living with chronic illness.”54 Measurement of population health and socioeconomic influences on health outcomes has traditionally been the role of public health agencies. However, innovative models of care delivery (such as patient-centered medical homes and accountable care organizations) recognize the importance of measuring and improving community health outcomes as integral to prevention and management of chronic conditions. The rapid expansion of Type 2 diabetes and other chronic conditions in the US increases society’s need for reliable data, beginning with standardized data collection that incorporates patient-level measures of social determinants of health. In turn, these data can be analyzed to ensure policies and practices at both organizational and system levels are allocating limited resources to mitigate the impact socioeconomic disparities have on the development and management of chronic conditions in the US.
Acknowledgments
Leslie Parker, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Bryant T, Daiski I, Lines E, et al. Type 2 diabetes: poverty, priorities and policy: the social determinants of the incidence and management of Type 2 diabetes [monograph on the Internet] Toronto, Ontario, Canada: York University School of Health Policy and Management; 2010. Mar 16, [cited 2011 Sep 20]. Available from: www.hpclearinghouse.ca/pdf/Diabetes%20Fact%20Sheet%202010%20-%20March%2016%20-%20final%20.pdf. [Google Scholar]
- 2.Touma C, Pannain S. Does lack of sleep cause diabetes? Cleve Clin J Med. 2011 Aug;78(8):549–58. doi: 10.3949/ccjm.78a.10165. DOI: http://dx.doi.org/10.3949/ccjm.78a.10165. [DOI] [PubMed] [Google Scholar]
- 3.Raphael D, Anstice S, Raine K, McGannon KR, Rizvi SK, Yu V. The social determinants of the incidence and management of type 2 diabetes mellitus: are we prepared to rethink our questions and redirect our research activities? Leadersh Health Serv. 2003;16(3):10–20. DOI: http://dx.doi.org/10.1108/13660750310486730. [Google Scholar]
- 4.National Advisory Committee on Health and Disability. The social, cultural and economic determinants of health in New Zealand: action to improve health [monograph on the Internet] Wellington, New Zealand: National Health Committee; 1998. Jun, [cited 2011 Oct 4]. Available from: www.moh.govt.nz/notebook/nbbooks.nsf/0/e2ab5dc750a0e3c04c256635007267d4/$FILE/det-health.pdf. [Google Scholar]
- 5.Pilkington FB, Daiski I, Bryant T, Dinca-Panaitescu M, Dinca-Panaitescu S, Raphael D. The experience of living with diabetes for low-income Canadians. Canadian Journal of Diabetes. 2010 Jun;34(2):119–26. [Google Scholar]
- 6.Chaufan C, Weitz R. The elephant in the room: the invisibility of poverty in research on type 2 diabetes. Humanity Soc. 2009 Feb;(1–2):33. 74–98. DOI: http://dx.doi.org/10.1177/016059760903300106. [Google Scholar]
- 7.Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77. doi: 10.1093/epirev/mxh002. DOI: http://dx.doi.org/10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 8.Smith J. Diabetes and the rise of the SES health gradient NBER Working Paper No 12905 [monograph on the Internet] Cambridge, MA: The National Bureau of Economic Research; 2007. Feb, [cited 2011 Sep 30]. Available from: www.nber.org/papers/w12905. [Google Scholar]
- 9.Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009 May;67(Suppl 1):S36–9. doi: 10.1111/j.1753-4887.2009.00157.x. DOI: http://dx.doi.org/10.1111/j.1753-4887.2009.00157.x. [DOI] [PubMed] [Google Scholar]
- 10.California Center for Public Health Advocacy, PolicyLink, UCLA Center for Health Policy Research. Designed for disease: the link between local food environments and obesity and diabetes [monograph on the Internet] Los Angeles, CA: California Center for Public Health Advocacy; 2008. Apr, [cited 2011 Oct 6]. Available from: www.policylink.org/site/apps/nlnet/content2.aspx?c=lkIXLbMNJrE&b=5136581&ct=6997183. [Google Scholar]
- 11.Lutfey K, Freese J. Toward some fundamentals of fundamental causality: socioeconomic status and health in the routine clinic visit for diabetes. Am J Sociol. 2005 Mar;110(5):1326–72. DOI: http://dx.doi.org/10.1086/428914. [Google Scholar]
- 12.Blas E, Sommerfeld J, Kurup AS, editors. Social determinants approaches to public health: from concept to practice [monograph on the Internet] Geneva, Switzerland: World Health Organization; 2012. [cited 2012 Nov 13]. Available from: www.who.int/sdhconference/resources/SDapproachestopublichealth_eng.pdf. [Google Scholar]
- 13.Glazier RH, Bajcar J, Kennie N, Wilson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006 Jul;29(7):1675–88. doi: 10.2337/dc05-1942. DOI: http://dx.doi.org/10.2337/dc05-1942. [DOI] [PubMed] [Google Scholar]
- 14.Eakin EG, Bull SS, Glasgow RE, Mason M.Reaching those most in need: a review of diabetes self-management interventions in disadvantaged populations Diabetes Metab Res Rev 2002January–Feb18126–35.DOI: http://dx.doi.org/10.1002/dmrr.266 [DOI] [PubMed] [Google Scholar]
- 15.Comprehensive, culturally sensitive care and self-management support improves health-related behaviors, clinical outcomes, and emotional health in Native Americans with diabetes [monograph on the Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2011. Aug 3, [cited 2012 Nov 13]. Available from: www.innovations.ahrq.gov/content.aspx?id=3200. [Google Scholar]
- 16.Racial and Ethnic Approaches to Community Health (REACH) [monograph on the Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2012. Nov 6, [cited 2012 Nov 13] Available from: www.cdc.gov/reach/about.htm. [Google Scholar]
- 17.National diabetes statistics, 2011 [monograph on the Internet] Bethesda, MD: US Department of Health and Human Services: National Institutes of Health; 2011. Feb, [cited 2011 Sep 20]. Available from: http://diabetes.niddk.nih.gov/dm/pubs/statistics/ [Google Scholar]
- 18.Diabetes: successes and opportunities for population-based prevention and control: at a glance 2011 [monograph on the Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2011. Aug 1, [cited 2011 Sep 22] Available from: www.cdc.gov/chronicdisease/resources/publications/AAG/ddt.htm. [Google Scholar]
- 19.Diabetes overview [monograph on the Internet] Bethesda, MD: US Department of Health and Human Services: National Institutes of Health; 2008. Nov, [cited 2011 Sep 20]. Available from: http://diabetes.niddk.nih.gov/dm/pubs/overview/ [Google Scholar]
- 20.Saad F, Gooren L. The role of testosterone in the metabolic syndrome: a review. J Steroid Biochem Mol Biol. 2009 Mar;114(1–2):40–3. doi: 10.1016/j.jsbmb.2008.12.022. DOI: http://dx.doi.org/10.1016/j.jsbmb.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 21.Farrell JB, Deshmukh A, Baghaie AA.Low testosterone and the association with type 2 diabetes Diabetes Educ 2008September–Oct345799–806.DOI: http://dx.doi.org/10.1177/0145721708323100 [DOI] [PubMed] [Google Scholar]
- 22.Sampson UK, Linton MF, Fazio S. Are statins diabetogenic? Curr Opin Cardiol. 2011 Jul;26(4):342–7. doi: 10.1097/HCO.0b013e3283470359. DOI: http://dx.doi.org/10.1097/HCO.0b013e3283470359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Izzedine H, Launay-Vacher V, Deybach C, Bourry E, Barrou B, Deray G. Drug-induced diabetes mellitus. Expert Opin Drug Saf. 2005 Nov;4(6):1097–109. doi: 10.1517/14740338.4.6.1097. DOI: http://dx.doi.org/10.1517/14740338.4.6.1097. [DOI] [PubMed] [Google Scholar]
- 24.Dinca-Panaitescu S, Dinca-Panaitescu M, Bryant T, Daiski I, Pilkington B, Raphael D. Diabetes prevalence and income: results of the Canadian Community Health Survey. Health Policy. 2011 Feb;99(2):116–23. doi: 10.1016/j.healthpol.2010.07.018. DOI: http://dx.doi.org/10.1016/j.healthpol.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Candib LM.Obesity and diabetes in vulnerable populations: reflection on proximal and distal causes Ann Fam Med 2007November–Dec56547–56.DOI: http://dx.doi.org/10.1370/afm.754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liburd LC, Jack L, Jr, Williams S, Tucker P. Intervening on the social determinants of cardiovascular disease and diabetes. Am J Prev Med. 2005 Dec;29(5 Suppl 1):18–24. doi: 10.1016/j.amepre.2005.07.013. DOI: http://dx.doi.org/10.1016/j.amepre.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 27.Williamson DF, Vinicor F, Bowman BA, Centers for Disease Control and Prevention Primary Prevention Working Group Primary prevention of type 2 diabetes mellitus by lifestyle intervention: implications for health policy. Ann Intern Med. 2004 Jun 1;140(11):951–7. doi: 10.7326/0003-4819-140-11-200406010-00036. [DOI] [PubMed] [Google Scholar]
- 28.Jack L, Jr, Liburd L, Spencer T, Airhihenbuwa CO. Understanding the environmental issues in diabetes self-management education research: a reexamination of 8 studies in community-based settings. Ann Intern Med. 2004 Jun 1;140(11):964–71. doi: 10.7326/0003-4819-140-11-200406010-00038. [DOI] [PubMed] [Google Scholar]
- 29.Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants—and why current policies may make matters worse. Health Aff (Millwood) 2011 Oct;30(10):1852–9. doi: 10.1377/hlthaff.2011.0685. DOI: http://dx.doi.org/10.1377/hlthaff.2011.0685. [DOI] [PubMed] [Google Scholar]
- 30.The chronic care model [monograph on the Internet] Seattle, WA: Group Health Research Institute: Improving Chronic Illness Care; 2006–2012. [cited 2012 Nov 13]. Available from: www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2. [Google Scholar]
- 31.Bell J, Standish M.Communities and health policy: a pathway for change Health Aff (Millwood) 2005March–Apr242339–42.DOI: http://dx.doi.org/10.1377/hlthaff.24.2.339 [DOI] [PubMed] [Google Scholar]
- 32.Isaacs SL, Schroeder SA. Class—the ignored determinant of the nation’s health. N Engl J Med. 2004 Sep 9;351(11):1137–42. doi: 10.1056/NEJMsb040329. DOI: http://dx.doi.org/10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- 33.Social determinants of health [monograph on the Internet] Geneva, Switzerland: World Health Organization; 2011. [cited 2011 Sep 10]. Available from: www.who.int/social_determinants/en/ [Google Scholar]
- 34.Mikkonen J, Raphael D. Social determinants of health: the Canadian facts. Toronto, Ontario, Canada: York University School of Health Policy and Management; 2010. May, [Google Scholar]
- 35.Wilkinson R, Marmot M, editors. Social determinants of health: the solid facts. 2nd ed. Copenhagen, Denmark: World Health Organization; 2003. [monograph on the Internet] [cited 2013 Jan 18]. Available from: www.euro.who.int/document/e81384.pdf. [Google Scholar]
- 36.Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991 Jun 8;337(8754):1387–93. doi: 10.1016/0140-6736(91)93068-k. DOI: http://dx.doi.org/10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- 37.Pincus T, Esther R, DeWalt DA, Callahan LF. Social conditions and self-management are more powerful determinants of health than access to care. Ann Intern Med. 1998 Sep 1;129(5):406–11. doi: 10.7326/0003-4819-129-5-199809010-00011. [DOI] [PubMed] [Google Scholar]
- 38.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of socioeconomic lifecourse. Soc Sci Med. 1997 Mar;44(6):809–19. doi: 10.1016/s0277-9536(96)00191-8. DOI: http://dx.doi.org/10.1016/S0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 39.Determinants of health [monograph on the Internet] Washington, DC: Department of Health and Human Services: Healthy People 2020; updated 2012 Sep 20 [cited 2013 Jan 30]. Available from: http://healthypeople.gov/2020/about/DOHAbout.aspx. [Google Scholar]
- 40.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011 Jun;40(3):804–18. doi: 10.1093/ije/dyr029. DOI: http://dx.doi.org/10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 41.Saydah S, Lochner K.Socioeconomic status and risk of diabetes-related mortality in the US Public Health Rep 2010May–Jun1253377–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilkins R, Berthelot JM, Ng E. Trend in mortality by neighbourhood income in urban Canada from 1971 to 1996. Health Reports (Statistics Canada, Catalog 82-003) 2002;13(Suppl):45–71. [Google Scholar]
- 43.Overcoming obstacles to health: report from the Robert Wood Johnson Foundation to the Commission to Build a Healthier America [monograph on the Internet] Princeton, NJ: Robert Wood Johnson Foundation; 2008. Feb 1, [cited 2011 Sep 31]. Available from: www.rwjf.org/en/research-publications/find-rwjf-research/2008/02/overcoming-obstacles-to-health.html. [Google Scholar]
- 44.Reither EN, Fedor TM, Abel KM, Hatch DJ. Associations between education attainment and diabetes in Utah: The Behavioral Risk Factor Surveillance System, 1996–2007. Utah’s Health: An Annual Review. 2009;14:42–51. [Google Scholar]
- 45.Lupien SJ, King S, Meaney MJ, McEwen BS. Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biol Psychiatry. 2000 Nov 15;48(10):976–80. doi: 10.1016/s0006-3223(00)00965-3. DOI: http://dx.doi.org/10.1016/S0006-3223(00)00965-3. [DOI] [PubMed] [Google Scholar]
- 46.Adler N, Stewart J, Cohen S, et al. Reaching for a healthier life: facts on socioeconomic status and health in the US [monograph on the Internet] Chicago, IL: John D and Catherine T MacArthur Foundation Research Network on Socioeconomic Status and Health; 2008. [cited 2011 Oct 5]. Available from: www.macses.ucsf.edu/downloads/Reaching_for_a_Healthier_Life.pdf. [Google Scholar]
- 47.McEwen BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann NY Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. DOI: http://dx.doi.org/10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 48.Raphael D, Daiski I, Pilkington B, Bryant T, Dinca-Panaitescu M, Dinca-Panaitescu S. A toxic combination of poor social policies and programmes, unfair economic arrangements, and bad politics: the experiences of poor Canadians with type 2 diabetes. Crit Public Health. 2012;22(2):127–45. DOI: http://dx.doi.org/10.1080/09581596.2011.607797. [Google Scholar]
- 49.Currie J, Madrian BC. Health, health insurance and the labor market. In: Ashenfelter A, Card D, editors. Handbook of labor economics. 3C. Amsterdam, The Netherlands: Elsevier BV; 1999. pp. 3309–416. [Google Scholar]
- 50.Corcoran M, Adams T. Race, sex, and the intergenerational transmission of poverty. In: Duncan GJ, Brooks-Gunn J, editors. Consequences of growing up poor. New York, NY: Russell Sage Foundation; 1997. Jun, pp. 461–517. [Google Scholar]
- 51.Caprio S, Daniels SR, Drewnowski A, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment. Obesity (Silver Spring) 2008 Dec;16(12):2566–77. doi: 10.1038/oby.2008.398. DOI: http://dx.doi.org/10.1038/oby.2008.398. [DOI] [PubMed] [Google Scholar]
- 52.Liburd LC. Diabetes and health disparities: community-based approaches for racial and ethnic populations. New York, NY: Springer Publishing Company; 2009. Sep 14, [Google Scholar]
- 53.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1998 Winter;15(4):351–77. doi: 10.1177/109019818801500401. DOI: http://dx.doi.org/10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 54.Committee on Living Well with Chronic Disease: Public Health Action to Reduce Disability and Improve Functioning and Quality of Life; Board on Population Health and Public Health Practice; Institute of Medicine Living well with chronic illness: a call for public health action. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- 55.Raphael D. Social determinants of health: present status, unanswered questions, and future directions. Int J Health Serv. 2006;36(4):651–77. doi: 10.2190/3MW4-1EK3-DGRQ-2CRF. DOI: http://dx.doi.org/10.2190/3MW4-1EK3-DGRQ-2CRF. [DOI] [PubMed] [Google Scholar]
- 56.Commission on Social Determinants of Health final report: closing the gap in a generation: health equity through action on the social determinants of health [monograph on the Internet] Geneva, Switzerland: World Health Organization; 2008. [cited 2013 Jan 18]. Available from: www.who.int/social_determinants/thecommission/finalreport/en/index.html. [Google Scholar]
- 57.Syme SL, Lefkowitz B, Krimgold BK.Incorporating socioeconomic factors into US health policy: addressing the barriers Health Aff (Millwood) 2002March–Apr212113–8.DOI: http://dx.doi.org/10.1377/hlthaff.21.2.113 [DOI] [PubMed] [Google Scholar]
- 58.The Patient Protection and Affordable Care Act of 2010.Public Law 111-148, 111th Congress, 124 Stat 119, HR 3590, enacted 2010 Mar 23.
- 59.US Department of Health and Human Services implementation guidance on data collection standards for race, ethnicity, sex, primary language, and disability status [monograph on the Internet] Washington, DC: US Department of Health and Human Services; 2011. Oct, [cited 2011 Oct 25]. Available from: http://aspe.hhs.gov/datacncl/standards/ACA/4302/index.shtml. [Google Scholar]
- 60.Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the Department of Health and Human Services. Health Aff (Millwood) 2011 Oct;30(10):1822–9. doi: 10.1377/hlthaff.2011.0673. DOI: http://dx.doi.org/10.1377/hlthaff.2011.0673. [DOI] [PubMed] [Google Scholar]
- 61.The American Community Survey [survey on the Internet] Washington, DC: US Department of Commerce, Economics and Statistics Administration; US Census Bureau; 2011. [cited 2011 Nov 6] Available from: www.census.gov/acs/www/Downloads/questionnaires/2011/Quest11.pdf. [Google Scholar]
- 62.Coleman-Jensen A, Nord M, Andrews M, Carlson S. Household food security in the United States in 2010. Economic Research Services Report No 125 [monograph on the Internet] Washington, DC: US Department of Agriculture; 2011. Sep, [cited 2011 Nov 6]. Available from: www.ers.usda.gov/Publications/ERR125/err125.pdf. [Google Scholar]
- 63.History: Index of questions [monograph on the Internet] Washington, DC: US Department of Commerce: United States Census Bureau; last revised 2012 Oct 18 [cited 2013 Feb 6]. Available from: www.census.gov/history/www/through_the_decades/index_of_questions/ [Google Scholar]
- 64.Ramanayake A, Zayatz L. Research report series (statistics #2010-04): balancing disclosure risk with data quality [monograph on the Internet] Washington, DC: Statistical Research Division, US Census Bureau; 2010. Feb 22, [cited 2011 Oct 25]. Available from: www.census.gov/srd/papers/pdf/rrs2010-04.pdf. [Google Scholar]
- 65.Ruger JP. Ethics of the social determinants of health. Lancet. 2004 Sep 18–24;364(9439):1092–7. doi: 10.1016/S0140-6736(04)17067-0. DOI: http://dx.doi.org/10.1016/S0140-6736(04)17067-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pcmh.ahrq.gov [homepage on the Internet] Rockville, MD: Agency for Healthcare Research and Quality; updated 2010 Jul 31 [cited 2012 Nov 13]. Available from: http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/what_is_pcmh. [Google Scholar]