Abstract
Background
Previous mental health care disparities studies predominantly compare mean mental health care use across racial/ethnic groups, leaving policymakers with little information on disparities among those with a higher level of expenditures.
Aims of the Study
To identify racial/ethnic disparities among individuals at varying quantiles of mental health care expenditures. To assess whether disparities in the upper quantiles of expenditure differ by insurance status, income and education.
Methods
Data were analyzed from a nationally representative sample of white, black and Latino adults 18 years and older (n=83,878). Our dependent variable was total mental health care expenditure. We measured disparities in any mental health care expenditures, disparities in mental health care expenditure at the 95th, 97.5th, and 99th expenditure quantiles of the full population using quantile regression, and at the 50th, 75th, and 95th quantiles for positive users. In the full population, we tested interaction coefficients between race/ethnicity and income, insurance, and education levels to determine whether racial/ethnic disparities in the upper quantiles differed by income, insurance and education.
Results
Significant Black-white and Latino-white disparities were identified in any mental health care expenditures. In the full population, moving up the quantiles of mental health care expenditures, Black-White and Latino-White disparities were reduced but remained statistically significant. No statistically significant disparities were found in analyses of positive users only. The magnitude of black-white disparities was smaller among those enrolled in public insurance programs compared to the privately insured and uninsured in the 97.5th and 99th quantiles. Disparities persist in the upper quantiles among those in higher income categories and after excluding psychiatric inpatient and emergency department (ED) visits.
Discussion
Disparities exist in any mental health care and among those that use the most mental health care resources, but much of disparities seem to be driven by lack of access. The data do not allow us to disentangle whether disparities were related to white respondent’s overuse or underuse as compared to minority groups. The cross-sectional data allow us to make only associational claims about the role of insurance, income, and education in disparities. With these limitations in mind, we identified a persistence of disparities in overall expenditures even among those in the highest income categories, after controlling for mental health status and observable sociodemographic characteristics.
Implications for Health Care Provision and Use
Interventions are needed to equalize resource allocation to racial/ethnic minority patients regardless of their income, with emphasis on outreach interventions to address the disparities in access that are responsible for the no/low expenditures for even Latinos at higher levels of illness severity.
Implications for Health Policies
Increased policy efforts are needed to reduce the gap in health insurance for Latinos and improve outreach programs to enroll those in need into mental health care services.
Implications for Further Research
Future studies that conclusively disentangle overuse and appropriate use in these populations are warranted.
INTRODUCTION
Racial/ethnic disparities in mental health care exceed disparities in many other areas of health care services,1 with blacks and Latinos accessing mental health care at only half the rate of non-Latino whites,1,2 even after adjusting for mental health status.3 Because racial/ethnic minorities respond well to evidence-based care, with results similar to or better than non-Latino whites,4,5 disparities in access and quality of care translate into a greater persistence, severity, and disease burden of mental disorder among blacks and Latinos.2,6–9 Although previous mental health care disparities studies have analyzed mean differences in mental health care use or population average effects,2,6–8 they typically have not examined disparities among those most costly to the mental health care system. Assessing disparities for those in the upper expenditure quantiles is arguably of great importance for policy reasons because of its budgetary implications and for clinical reasons since these individuals have the greatest need for care. Assessing disparities in expenditures among those with the highest need for care determines whether the allocation of resources is being equally spent on the more sickly patients across racial/ethnic groups; and whether the allocation of resources determined to be disparate at the mean, ever equalizes among high utilizers of mental health care.
There is some evidence suggesting that disparities are likely to persist among those in greatest need and the high utilizers of mental health care. Studies measuring quality of care have identified higher rates of attrition from treatment among racial/ethnic minorities,10 with fewer psychotherapy treatment sessions and lack of prescription drug use for individuals diagnosed with depression11,12 and schizophrenia,13 and disparities in receipt of the best available depression treatments.7,14 Racial/ethnic disparities also exist in the use of psychotropic medications, including selective serotonin reuptake inhibitors (SSRIs)11,15,16 for depression, atypical antipsychotics (particularly clozapine) for schizophrenia,17–21 and antipsychotics and mood stabilizers for bipolar disorder.21,22
A recent study identified significant disparities in any mental health care expenditure but no disparities in treatment expenditures among those with greater than zero mental health care expenditures.6 Similarly, in a study of depression treatment, Harman et al.11 identified disparities in initiation, but not in adequacy of treatment conditional on initiation. These studies separate disparities in any use from disparities among positive users, but they do not allow one to investigate whether disparities exist among the highest users of care. The current study differs from these prior studies by measuring expenditures of the patients that receive the most resources from the health care system, and by focusing on whether disparities among positive users that arise from differential access to mental health care are ever eliminated among patients in the upper quantiles of expenditures.
We explore three potential moderators of racial/ethnic disparities at the upper quantiles of expenditures: health insurance, income, and educational level. Restrictions on eligibility, affordability, and scope of health insurance programs could influence mental health care disparities, including some of the disparities among positive users being due to lack of financial access to care or access to providers. Racial/ethnic minorities are more likely to be uninsured, a strong negative predictor of receiving mental health care.3,23,24 Even with insurance coverage, racial/ethnic minorities have greater challenges in effectively navigating health insurance and the medical system.25 We evaluate whether disparities in upper quantiles of expenditures differ among the uninsured compared to individuals with public and private insurance. Lower income and lower educational attainment are two indicators of socioeconomic status that have been linked with poorer mental health and lower use of services when needed.26,27 One study identified a positive association between the percentage of individuals with incomes below the federal poverty level and the magnitude of mental health care disparities.28 Greater education also increases the likelihood of any mental health service use for all racial/ethnic groups, with even greater benefits for Latinos with higher education compared to their white counterparts.3 We investigate whether disparities in upper quantiles of expenditures are equivalent in all income and education categories.
First, we assess disparities in receipt of any mental health care expenditures and identify whether expenditure disparities are ever eliminated among patients in the upper quantiles of expenditures. Second, we use quantile regression to identify racial/ethnic mental health care disparities among the highest users of mental health care resources. Third, we repeat the quantile regression analysis only among those with positive expenditures to identify disparities among those that have accessed care. We also assess to what extent disparities in the overall population differ by insurance status, income, and education. We hypothesize that a smaller percentage of Blacks and Latinos will have any mental health care expenditures (potentially because of lack of access), that Black-white and Latino-white disparities will persist even among those utilizing the most health care resources, and that disparities in the upper quantiles will be narrowed for those with private insurance, greater income and higher education.
METHODS
Data
The data were taken from responses to the 2004–2008 Medical Expenditure Panel Surveys (MEPS) containing variables related to individuals’ mental health care expenditures, sociodemographic characteristics, and mental health status from a nationally representative sample of the non-institutionalized civilian population of the United States. We pooled five years of cross-sectional data in order to increase the precision of the estimates, accounting for the non-independence of individuals that span two years of data and the complex sample design of the MEPS.29 Children (age < 18) were excluded because the MEPS did not collect three scales of mental health status important to the analyses. Native Americans and Asian/Pacific Islanders were omitted from the analyses because the sample sizes were inadequate to detect meaningful differences.
We consider mental health services as treatment of a disorder covered by International Classification of Diseases (ICD-9) codes of 291, 292, or 295–314.30 Prices are adjusted to 2008 dollars using the Consumer Price Index (CPI). The dependent variable of interest is mental health care expenditures, the sum of all direct payments in the last year for mental health-related prescription drugs, inpatient care, outpatient care, office-based care (including counseling and social worker visits), and emergency room use. These expenditures include out-of-pocket payments and payments by private insurance, Medicaid, Medicare and other sources, but do not include payments for over-the-counter drugs and exclude premiums paid by individuals or by their employers.
We use Census categories to identify respondents’ racial/ethnic background. Respondents of Hispanic or Latino origin were identified as Latino, independent of race. Other respondents were classified as black or non-Latino white based on responses to the race question.
Covariates that reflect the socioeconomic status, insurance status, and geography of the participants are education level (less than high school, high school graduate, any college, college graduate), income level (below federal poverty level (FPL), near poverty [100–125% FPL], low income [125%–200% FPL], middle income [200%–400% FPL], and high income [≥400%FPL]), insurance coverage (private, Medicare, Medicaid or other public (e.g. military insurance and Tricare), and uninsured), and region of the country (Northeast, South, Midwest, and West). Four items were used to measure mental health status: 1) self-reported mental health score (excellent, very good, good, fair, poor); 2) the mental health component of the Short-Form 12 Version 2 (SF-12v2);31 3) the Patient Health Questionnaire (PHQ-2) scale of depressive symptoms,32 with strong sensitivity (93%) and specificity (74%) for major depressive disorder;32 and 4) the Kessler Index (K-6) scale of non-specific psychological distress,33,34 a scale designed to maximize the ability to discriminate cases of severe mental illness from non-cases.33 Three measures of physical health indicators were also included because of their association with greater severity of mental health status:35–37 self-reported physical health scores (excellent, very good, good, fair, poor), having any functional limitation, and indicators for the following chronic diseases and health conditions: diabetes, asthma, coronary heart disease, angina, myocardial infarction, stroke, emphysema, joint pain, arthritis, and other heart disease. Gender and age category (18–24, 25–34, 35–44, 45–54, 55–64, 54–73, and 75+) are considered as characteristics representing need for mental health care given the large differences in rates of mental illness among these groups.
Approximately 13% of our weighted sample was missing on the SF-12, K-6, and PHQ-2 scales while most other variables were missing in approximately 1% of the sample. To account for differential missingness by race/ethnicity, we reweighted the included individuals to represent their propensity to be like individuals with missing values.38,39
Data Analytic Procedures
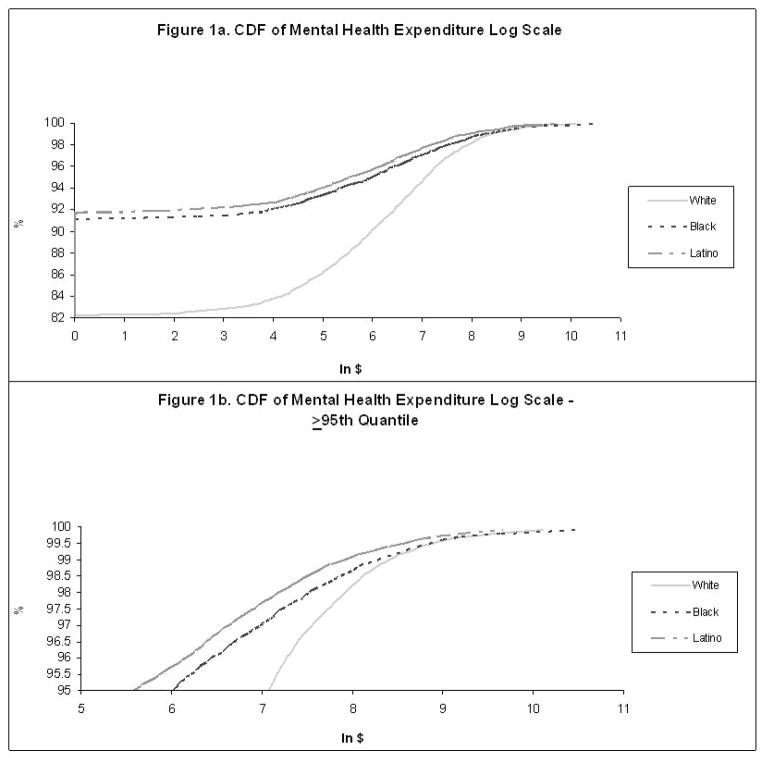
We first report unadjusted total mental health care expenditures for each racial/ethnic group at each quantile of expenditure, and compare the cumulative distribution function for each racial/ethnic group. This analysis assesses whether disparities among positive users that arise from differential access to mental health care are ever eliminated among patients in the upper quantiles of expenditures.
Second, we estimated quantile regression (explained in more detail below) to assess disparities at the 95th, 97.5th, and 99th quantiles of mental health care expenditure. The analysis answers the question: Do Blacks and Hispanics that receive the most mental health care resources (at the top 5th, 2.5th, and 1st quantiles) spend as much as their white counterparts, after adjustment for need and other covariates? In determining quantiles, this analysis uses both users and non-users, setting all non-users to receive $0 expenditures.
Third, we estimated quantile regression models at the 50th, 75th and 95th quantiles among only those with positive expenditures. This analysis differs from the one described above in that the quantile for each group is determined by only users of the mental health care system. This analysis evaluates disparities in health care system resources spent on individuals within care, a group of individuals that may differ on a number of observed and unobserved factors from the entire population.
Quantile regression 40,41 assesses differences in the response of individuals generally across quantiles as well as the differential response by race and ethnic group. In quantile regression, the intercept and the slopes are both allowed to vary across the quantiles. This is done by differentially weighting positive and negative absolute residuals across the distribution of data.40,42,43 For example, in a 95th quantile regression, residuals are weighted so that the regression “plane” passes through the data so that 95 percent of the observations are below the regression plane and 5 percent are above.
Quantile regression is an alternative to commonly used two-part models that estimate probability of any use with logit regression and positive use with generalized linear models or ordinary least squares (OLS) regression for ln(y)|y>0.44–47 A key difference is that, unlike quantile regression, generalized linear models used in these two-part models implicitly assume that there is a common response to covariates at all levels of positive expenditures but more importantly, they exclude those that have not been able to enter care. The quantile regression method is more ideally suited toward measuring disparities across the distribution because it allows for differential response across levels, making it possible to identify additional differences across the distribution of use given the observable differences in covariates across the groups.
We employed quantile regression on the natural log of expenditures plus a constant. Adding a constant allows us to include zeros in our quantile regression analysis while not changing participants’ membership in the upper quantiles. Moreover, we take the log of expenditures because we expect that the effect of many of the predictor variables on the dependent variable is closer to multiplicative than to additive. From our exploratory analysis of the two-part model’s fit for the overall mean response, we have support for a multiplicative model rather than an additive one.
Model covariates were chosen to assess racial/ethnic disparities in mental health expenditures concordant with the Institute of Medicine (IOM) definition of racial/ethnic healthcare disparities48,49 which states that disparities are all differences except those due to clinical appropriateness, need, and patient preferences.48 In the absence of measures related to clinical appropriateness and patient preferences in the MEPS, we generated predictions based on models that adjust for variables related to need for mental health care (e.g. self-reported mental health, mental health component of the SF-12, K-6, PHQ-2, self-reported physical health, functional limitation, indicators for chronic diseases); and age, sex, and marital status, given large differences across these categories in prevalence of mental illness.50 Interactions between need and race-ethnicity variables were included to allow for the differential return on these variables by race/ethnicity that has been noted in previous work on the MEPS data.51 In a separate analysis, we additionally adjusted for health insurance status, region, and SES characteristics, to view isolated racial/ethnic differences after adjusting for all available covariates.
To improve model fit, we added interactions between race/ethnicity indicators and need and SES variables to account for differential responses, and added the square of the PCS-12 and MCS-12 variables to better match their non-linear association with expenditures. Goodness of fit for quantile regression models was verified using Pregibon’s Link Test on a major percentile basis52 and the modified Hosmer-Lemeshow test.53,54 Both tests adjusted for the complex survey design of the MEPS.
Disparity Predictions
Once models were estimated, predicted disparities were generated using the residual direct effect method (RDE), a method that generates predictions based on the coefficient of interest while adjusting for all other model characteristics.24 In this case, we are interested in transforming the coefficients on Black race and Latino ethnicity indicator variables into a disparity estimate in the scale of interest (expenditure in dollars). To illustrate, for blacks, we fit the quantile regression models on the entire population (including users and non-users), recoded from 0 to 1 all indicators of black race/ethnicity (the black variable and black interaction coefficients when appropriate), and then predicted expenditures in the white population. These predictions were then compared to model-estimated mean predictions for whites at each quantile allowing us to see how the system of care differentially allocates resources among the highest spenders. Previous studies have employed a similar method (often called recycled predictions) of converting regression coefficients into predicted group rates.55,56 The minor difference is that the RDE compares minority individuals with white characteristics with actual whites, whereas the recycled prediction method compares minority individuals with overall population characteristics with white individuals with overall population characteristics. We feel the RDE provides a counterfactual method that more closely aligns with the relevant questions for policy (in this case, what would minority expenditures be if blacks, Latinos and whites all had the same mix of covariates?).
Standard error estimation for predicted expenditures and disparities accounts for the complex sample design of the MEPS in multiple ways. During model estimation, stratum and primary sampling unit (psu) variables were standardized across pooled years29 using publicly available strata and psu variables that specify a common variance structure for MEPS respondents across multiple years of data. The modified balanced repeated replication (BRR) method57 was then used, drawing 128 subsamples of the population, each of which is half of the full sample size, calculating predicted expenditures and disparities on each of the subsamples and calculating the variance of these 128 estimates. The identification of these subsamples is acquired through a publicly available download of BRR dataset indicators that have been randomly generated by AHRQ.29
Assessing Whether Disparities Exist Across Quantiles in all Insurance and SES Groups
We additionally adjusted for interactions between income, education and insurance and race-ethnicity variables, allowing for disparity comparisons within these different subgroups for each quantile. Variables used in interaction terms were centered by subtracting their mean so that main effects results are readily interpretable.58 F-tests between linear combinations of these hypothesized mechanisms’ main effects and interaction coefficients were compared for each of the quantile regression results to assess their differential impact across quantiles, and to assess the differences between adjacent categories within quantiles.
RESULTS
Unadjusted Results
Figure 1a presents the unadjusted cumulative distribution functions of mental health expenditures for non-Latino whites, blacks, and Latinos. Whites were twice as likely as Blacks and Latinos to have any mental health care expenditure (18%, 9%, and 9% respectively). The difference in any use is represented by the y-intercept for each of the racial/ethnic groups, with whites in the 82nd quantile beginning to show use of mental health care, and Blacks and Latinos showing use at the 91st quantile. Black and Latino mental health expenditures do not reach the levels of non-Latino whites until the 99th quantile (Figure 1b).
Figure 1.
The average expenditures for each quantile by racial/ethnic group were lower for Latinos and Blacks in all quantiles, with the exception that there is no difference between Blacks and non-Latino whites in the 99th quantile (Table 1). Latino mental health spending remains significantly lower than non-Latino whites through the 99th quantile where Latinos spend $3170 less than non-Latino whites on total mental health care.
Table 1.
Weighted Mental Health Expenditure ($FY 2008) for Blacks, Hispanics and Latinos Age>=18 by Quantile
| Quantile | Total MH Expenditure | ||
|---|---|---|---|
| White (n=49,078) | Black (n=14,139) | Latino (n=20,661) | |
| 1 | 0 | 0 | 0 |
| . | . | . | . |
| . | . | . | . |
| 81 | 0.00 | 0 | 0 |
| 82 | 9.43 | 0 | 0 |
| 83 | 44.72 | 0 | 0 |
| 84 | 79.44 | 0 | 0 |
| 85 | 115.58 | 0 | 0 |
| 86 | 160.63 | 0 | 0 |
| 87 | 212.68 | 0 | 0 |
| 88 | 276.49 | 0 | 0 |
| 89 | 350.96 | 0 | 0 |
| 90 | 436.35 | 0 | 0 |
| 91 | 553.20 | 16.82 ** | 4.15 ** |
| 92 | 684.95 | 79.84 ** | 55.45 ** |
| 93 | 848.16 | 157.75 ** | 122.19 ** |
| 94 | 1051.65 | 291.33 ** | 219.04 ** |
| 95 | 1287.63 | 494.48 ** | 382.03 ** |
| 96 | 1611.39 | 809.35 ** | 619.09 ** |
| 97 | 2234.98 | 1393.88 ** | 1005.03 ** |
| 98 | 3382.58 | 2567.88 ** | 1801.69 ** |
| 99 | 9530.90 | 11221.86 | 6361.35 ** |
Source: 2004–2008 MEPS
Expenditures adjusted for inflation to $2008 dollars using Consumer Price Index (CPI)
significant at α<.05 level
Predicted Mental Health Care Expenditures from Quantile Regressions
We identified significant Black-white and Latino-white disparities at the 95th, 97.5th, and 99th quantiles in the model specification that includes only need variables (mental health status, physical health status, age, sex, and marital status) (Table 2a). Compared to disparities in the 95th quantile, disparities were reduced in relative terms in the 97.5th and 99th quantiles but remained statistically significant. Estimated Black overall expenditures were $334, $843, and $1129 less than whites, respectively, in the 95th, 97.5th, and 99th quantile. Latino expenditures were $322, $836, and $1204 less than whites, respectively in the 95th, 97.5th, and 99th expenditure quantiles.
Table 2a. Racial and ethnic differences in total mental health care expenditures by quantile.
Comparing White Expenditure to Predicted Minority Mental Health Expenditure using Black/Latino Coefficients and White Covariate Distributions
| Quantile Regression | Quantile |
|
|
|||||
|---|---|---|---|---|---|---|---|---|
| White | Black | B-W Disparity | %Disparity | Latino | L-W Disparity | %Disparity | ||
|
|
|
|||||||
| Estimate | Estimate | Estimate | ||||||
| Need covariates only model | 95% | 341.59 | 7.92 | 333.67 | 98% | 19.30 | 322.28 | 94% |
| 97.5% | 996.73 | 153.83 | 842.90 | 85% | 161.10 | 835.63 | 84% | |
| 99% | 2254.13 | 1125.57 | 1128.56 | 50% | 1049.83 | 1204.30 | 53% | |
| Full covariates model | 95% | 318.97 | 10.11 | 308.86 | 97% | 57.75 | 261.23 | 82% |
| 97.5% | 975.27 | 137.21 | 838.06 | 86% | 277.19 | 698.08 | 72% | |
| 99% | 2115.69 | 868.90 | 1246.78 | 59% | 1312.25 | 803.44 | 38% | |
Source: 2004–2008 MEPS (n=83,878)
All disparity results are significant at α<.05
In addition to race/ethnicity indicator variables, quantile regression models using need only covariates adjust for health and mental health status variables (self-reported mental health and health status, mental and physical components of the SF-12 scale, K6 scale of severe psychological distress, PHQ-2 depression scale, list of chronic conditions, BMI, age, gender. Full covariate models additionally include socioeconomic status variables (poverty status, education, and marital status), and interactions between race/ethnicity and education and income.
In the full covariate model, Black-white disparities were similar to those estimated in the need-only covariate model. Latino-white disparities were slightly lower in percentage terms than the need-variable-only model, showing that adjusting for Latinos’ poorer insurance and SES status reduced disparities.
Among the subpopulation of positive mental health care users, we found Latino-white disparities among positive users of borderline significance (p<.10, $395 and $310 for Whites and Latinos, respectively) at the 50th quantile. We found no significant Black-white disparities among positive users at the 50th, 75th, or 95th quantile and no significant Latino-white disparities among positive users at the 75th or 95th quantiles of expenditures (See Table 2b).
Table 2b. Racial and ethnic differences in total mental health care expenditures among those with positive expenditures by quantile.
Comparing White Expenditure to Predicted Minority Mental Health Expenditure using Black/Latino Coefficients and White Covariate Distributions
| Quantile Regression | Quantile |
|
|
|||||
|---|---|---|---|---|---|---|---|---|
| White | Black | B-W Disparity | %Disparity | Latino | L-W Disparity | %Disparity | ||
|
|
|
|||||||
| Estimate | Estimate | Estimate | ||||||
| Full covariates model | 50% | 389.79 | 377.47 | 12.32 | 3% | 372.63 | 17.16 | 4% |
| 75% | 997.81 | 1067.00 | −69.19 | −7% | 1022.37 | −24.56 | −2% | |
| 95% | 3436.47 | 3715.49 | −279.01 | −8% | 3883.02 | −446.55 | −13% | |
| HS covariates only model | 50% | 394.78 | 384.62 | 10.16 | 3% | 310.28 | 84.50 | 21% * |
| 75% | 992.98 | 1207.17 | −214.19 | −22% | 877.76 | 115.22 | 12% | |
| 95% | 3613.39 | 5578.72 | −1965.33 | −54% | 3449.86 | 163.53 | 5% | |
Source: 2004–2008 MEPS (n=83,878)
p<.10
In addition to race/ethnicity indicator variables, quantile regression models using need only covariates adjust for health and mental health status variables (self-reported mental health and health status, mental and physical components of the SF-12 scale, K6 scale of severe psychological distress, PHQ-2 depression scale, list of chronic conditions, BMI, age, gender. Full covariate models additionally include socioeconomic status variables (poverty status, education, and marital status), and interactions between race/ethnicity and education and income.
Disparities by Insurance Status
Assessing differential outcomes across quantiles of total mental health care expenditure by insurance status in the overall US population (including those that did not enter care), we identified Black-white disparities in all insurance categories at the 95th quantile (Table 3, panel 1). In the 97.5th and 99th quantiles, we identified Black-white disparities among those with private insurance and the uninsured but not among the publicly insured. Across quantiles, Black-white disparities were highest in the privately insured. Latino-white disparities exist in all insurance categories for all quantiles (Table 3, Panel 2). However, the magnitude of Latino-white disparities was significantly greater among the publicly insured compared to the privately uninsured in all quantiles and Latino-white disparities were greater for the uninsured compared to the publicly uninsured in the 97.5th and 99th quantiles.
Table 3.
Quantile regression coefficients from model of mental health care expenditure testing differential response by race, insurance, education, income, and language
| 95th percentile | 97.5 percentile | 99th percentile | ||
|---|---|---|---|---|
| Black-White Difference | ||||
| Insurance | Private₪ | −2.896 ** | −1.603*** | −1.304*** |
| Public | −1.009 ***,††† | 0.112††† | −0.112††† | |
| Uninsured | −0.823 **,††† | −1.798***,††† | −1.752***,†† | |
| Education | < HS Grad₪ | −2.896 ** | −1.603*** | −1.304*** |
| HS Grad | −2.757 ***,††† | −1.007***,††† | −0.531††† | |
| Any College | −3.618 *** | −1.544***,†† | −0.948**,†† | |
| College Grad | −2.833 ***,††† | −0.843**,††† | −0.459††† | |
| Income | <FPL₪ | −2.896 ** | −1.603*** | −1.304*** |
| 100–125% FPL | −3.023 ***,††† | −0.769††† | −0.879††† | |
| 125–200% FPL | −3.199 *** | −1.880***,††† | −0.782 | |
| 200–400% FPL | −2.779 *** | −1.922*** | −1.439*** | |
| 400%+ FPL | −3.367 *** | −1.706***,†† | −1.305*** | |
| Latino-White Difference | ||||
| Insurance | Private₪ | −1.888 *** | −1.352** | −0.819** |
| Public | −2.100 ***,††† | −1.569***,††† | −1.482***,†† | |
| Uninsured | −0.6361 ** | −2.632***,††† | −1.648***,†† | |
| Education | < HS Grad₪ | −1.888 *** | −1.352** | −0.819** |
| HS Grad | −1.547 **,††† | −0.489††† | 0.078††† | |
| Any College | −2.421 *** | −1.026***,††† | −0.181††† | |
| College Grad | −1.724 ***,††† | −0.715 | −0.094††† | |
| Income | <FPL₪ | −1.888 *** | −1.352*** | −0.819** |
| 100–125% FPL | −2.225 ***,††† | −1.393***,††† | −1.141**,††† | |
| 125–200% FPL | −2.054 *** | −1.399*** | −0.973** | |
| 200–400% FPL | −1.733 *** | −1.394*** | −1.193*** | |
| 400%+ FPL | −2.307 *** | −1.580*** | −0.694†† | |
Source: 2004–2008 MEPS (n=83,878)
On log scale - proportional effects (no risk ratios)
In addition to race/ethnicity indicator variables, quantile regression models adjust for age, gender, health and mental health status variables (self-reported mental health and health status, mental and physical components of the SF-12 scale, K6 scale of severe psychological distress, PHQ-2 depression scale, list of chronic conditions, BMI), socioeconomic status variables (poverty status, education, and marital status), and interactions between race/ethnicity and education and income.
Indicates referent group used in the expenditure model. Coefficients presented for these groups are estimated using linear combinations.
Significant disparity at α=0.05 and α=0.01 levels
Significantly different from prior row’s group (same quintile) at α=0.05 and α=0.01 levels
Disparities by Education
Black-white disparities exist within all education categories for the 95th and 97.5th quantiles, and among those with less than a high school education and those with some college education at the 99th quantile. In the 97.5th and 99th quantiles, disparities were generally reduced with greater education. Latino-white disparities exist in all education categories in the 95th quantile, among those with less than a high school education and some college education in the 97.5th quantile, and only among those with less than a high school education in the 99th quantile. As with African-Americans, the magnitude of Latino-white disparities is generally reduced with greater education in the 97.5th and 99th quantiles.
Disparities by Income
Black-white disparities in mental health care expenditure were seen in nearly every income category, and the magnitude of disparities changed very little even when comparing the groups with the greatest income. Latino-white disparities also exist in nearly every income category in all quantiles and there is little variation in the magnitude of these disparities across the income categories (though at times these variations are significant) in each of the quantiles.
DISCUSSION
Our analysis of treatment disparities across the distribution of mental health care expenditures identified that Black-white disparities and Latino-white disparities exist in receipt of any mental health care and in expenditures among those that receive the most mental health care resources, even after adjustment for need and a complete set of covariates. In contrast, among only those in mental health care (18% of whites, 9% of Blacks and 9% of Latinos), no disparities among positive users were identified at the 50th, 75th, and 95th quantile in either unadjusted (not shown), full covariate adjustment or IOM-concordant adjustment estimates with the exception of marginally significant Latino-white disparities at the 50th quantile. This emphasizes that expenditure disparities in the overall population are largely attributable to the inaccessibility of the healthcare system to ethnic/racial minorities even at substantial levels of illness severity. One similarity in results between the overall sample and positive users is that there is no Black-white disparity in expenditures in the highest quantile, suggesting that the Blacks that are most in need are receiving both equitable access and treatment resources.
These two analyses provide distinct snapshots of disparities in the U.S. mental health care system. The overall quantile regression results can be considered to be a comparison of expenditures in a community sample. Results demonstrate that the Blacks and Latinos in the highest quantiles of expenditures spend significantly less than their White counterparts. Individuals in the highest quantiles of expenditures are likely to be those with the greatest severity of mental illness and need for care in the population. Identifying persistent disparities in the upper quantiles, even after equalizing the racial/ethnic groups on their high levels of severity and need, suggests that we are not providing equitable treatment to the population requiring the most care.
In contrast, the conditional quantile regression results can be considered to represent a comparison of a clinical population that was able to access care, and in this comparison we found no significant disparities in expenditures. The lack of disparities in the conditional analysis supports prior evidence finding no disparities in expenditures among positive users as has been found in other studies.6,11 Racial/ethnic minority individuals in the mental health care system appear to be receiving the same amount of resources as whites once in care. This is promising and points to the possible success of system-wide efforts to increase cultural and language competency59 and improve the racial/ethnic concordance of clinic staff.60,61
It is clear from our analysis that there are disparities in access to mental health care, with 18% of whites using mental health care compared to only 9% of Blacks and Latinos. Unobserved characteristics that may account for these access disparities are poorer recognition for depression and anxiety in the PCP settings where racial/ethnic minorities disproportionately seek care.7,62 Our results are consistent to other studies showing that Latinos with depression appear to exhibit a decreased likelihood of recognizing that they have a mental health problem as compared to non-Latinos whites with depression (36.3% of Latinos with depression vs. 60% of non-Latino whites)7 and fail to identify symptoms of mental distress as mental illness worthy of treatment.63 In addition, Blacks and Latinos have been found to be more likely than whites to indicate embarrassment when discussing mental health problems and concern for losing pay or employment as barriers to mental health treatment.64 Furthermore, racial/ethnic minorities may hold cultural value differences related to mental illness that influence care-seeking behaviors (e.g., collectivist values may conflict with the individual orientation of psychotherapy).65 Research has also shown that religious leaders are an important source of support for addressing mental health needs for minority populations.66–68 Continued efforts at initiating and strengthening connections between mental health care systems and alternative/ complementary care settings, improving translation and interpretation services in locations of mental health care, and enhancing bilingual/bicultural outreach programs to enroll those in need into mental health care services, will potentially further serve to reduce disparities among the Latino population.7
Not verifiable in the current cross-sectional dataset is how disparities in access and treatment are inter-related. Past experiences of bias while in mental health care treatment69 and racial/ethnic minorities’ greater likelihood of early drop out from care70 may contribute to present-day access disparities. Relatedly, future studies should investigate the health status and socio-economic characteristics of minorities on the margins of treatment, compare them to white counterparts that are in treatment, and consider targeting these populations for access interventions.
One potential explanation for persistent disparities at the upper end of the expenditure distribution of the overall sample, besides differences in access to care, is that Blacks and Latinos use more expensive outpatient specialty mental health care half as much as whites, even after adjusting for demographics, insurance status, and psychiatric comorbidity.71,72 Their reluctance to use specialty care is concerning given that there are significant disparities in the adequacy of depression and anxiety treatment in PCP settings,7,62,73 and physicians in PCP settings have been less likely to identify mental illness in racial/ethnic minorities compared to whites. The lack of referral to specialty providers may be in part due to mental health screening and diagnostic instruments that are inadequate in minority populations74 or because physicians are more prone to making diagnostic errors because of communication problems.75
Given the lack of detail on the timing of treatment and severity of these patients, we were unable to rule out that disparities in the upper quantiles in the overall sample were due to overuse by whites rather than underuse by minority groups. Studies showing disparities in adequate care among severely mentally ill allay this concern, but future studies that conclusively disentangle overuse and appropriate use in these populations are warranted. We do not believe the disparities at the higher end of the distribution to be caused by greater use of costly inpatient mental health care by whites in comparison to Blacks and Latinos. Removing psychiatric inpatient and emergency department (ED) expenditures (analysis not shown) does not impact the direction and significance of results of the study likely because urgent mental health care in the MEPS sample (and in the U.S.) was extremely rare. We were also limited by the cross-sectional data to making only associational, not causal, claims about the role of insurance, income, and education in disparities.
In the overall sample, the magnitude of Black-white disparities was smaller (less disparity) among those enrolled in public insurance programs compared to the privately insured and uninsured in the 97.5th and 99th quantiles of expenditures. This greater parity in public health insurance programs may be due to the generosity of Medicaid agencies in terms of mental health care benefits in comparison to private insurance and free care insurance programs. The significance of insurance status in regression models combined with significant differences on these factors in Table 1 suggest increased policy efforts at reducing the gap in health insurance for Latinos are needed. The implementation of health care reform stands to reduce Black-white disparities. Some gains will be achieved under health care reform for Latinos although undocumented and recent legal immigrants will remain ineligible for public health insurance in a number of states.
Acknowledgments
Source of Funding:
This study was supported by grants from the National Institute of Mental Health (R01 MH091042: PI Cook, and P50 MHO 73469: PI Alegría). This study was approved by the Cambridge Health Alliance Institutional Review Board.
Contributor Information
Benjamin Lê Cook, Department of Psychiatry, Harvard Medical School, Senior Scientist, Center for Multicultural Mental Health Research.
Willard Manning, Harris School and the Department of Health Studies of the Biological Sciences Division, University of Chicago.
Margarita Alegría, Department of Psychiatry, Harvard Medical School, Director, Center for Multicultural Mental Health Research.
References
- 1.AHRQ. National Healthcare Quality Report 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 2.Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse and mental health care. Am J Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 3.Cook B, McGuire T, Miranda J. Measuring Trends in Mental Health Care Disparities, 2000–2004. Psychiatr Serv. 2007;58:1533–1539. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- 4.Miranda J, Bernal G, Lau A, Kohn L, Hwang W, LaFromboise T. State of the Science on Psychosocial Interventions for Ethnic Minorities. Annual Review of Clinical Psychology. 2005:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schraufnagel TJ, Wagner AW, Miranda J, Roy-Byrne PP. Treating minority patients with depression and anxiety: What does the evidence tell us? Gen Hosp Psychiatry. 2006;28:27–36. doi: 10.1016/j.genhosppsych.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Cook BL, McGuire T, Lock K, Zaslavsky A. Comparing Methods of Racial and Ethnic Disparities Measurement across Different Settings of Mental Health Care. Health Serv Res. 2010;45:825–847. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alegria M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Jackson J, Meng XL. Disparity in Depression Treatment Among Racial and Ethnic Minority Populations in the United States. Psychiatr Serv. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanco C, Patel SR, Liu L, Jiang H, Lewis-Fernández R, Schmidt AB, Liebowitz MR, Olfson M. National Trends in Ethnic Disparities in Mental Health Care. Med Care. 2007;45:1012. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 9.Sue S, Zane N, Young K. Handbook of psychotherapy and behavior change. New York: Wiley; 1994. Research on psychotherapy on culturally diverse populations; pp. 783–817. [Google Scholar]
- 10.Sue S, Zane N, Young K. Research on psychotherapy with culturally diverse populations. Handbook of psychotherapy and behavior change. 1994;4:783–820. [Google Scholar]
- 11.Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatr Serv. 2004;55:1379. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- 12.Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatric Quarterly. 2007;78:3–14. doi: 10.1007/s11126-006-9022-y. [DOI] [PubMed] [Google Scholar]
- 13.Busch AB, Lehman AF, Goldman H, Frank RG. Changes over time and disparities in schizophrenia treatment quality. Med Care. 2009;47:199. doi: 10.1097/MLR.0b013e31818475b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the united states. J Gen Intern Med. 2000;15:284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gonzalez HM, Croghan T, West B, Williams D, Nesse R, Tarraf W, Taylor R, Hinton L, Neighbors H, Jackson J. Antidepressant Use in Black and White Populations in the United States. Psychiatr Serv. 2008;59:1131–1138. doi: 10.1176/appi.ps.59.10.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melfi CA, Croghan TW, Hanna MP, Robinson RL. Racial variation in antidepressant treatment in a Medicaid population. J Clin Psychiatry. 2000;61:16–21. doi: 10.4088/jcp.v61n0105. [DOI] [PubMed] [Google Scholar]
- 17.Daumit GL, Crum RM, Guallar E, Powe NR, Primm AB, Steinwachs DM, Ford DE. Outpatient prescriptions for atypical antipsychotics for African Americans, Hispanics, and whites in the United States. Arch Gen Psychiatry. 2003;60:121–128. doi: 10.1001/archpsyc.60.2.121. [DOI] [PubMed] [Google Scholar]
- 18.Herbeck DM, West JC, Ruditis I, Duffy FF, Fitek DJ, Bell CC, Snowden LR. Variations in use of second-generation antipsychotic medication by race among adult psychiatric patients. Psychiatr Serv. 2004;55:677–684. doi: 10.1176/appi.ps.55.6.677. [DOI] [PubMed] [Google Scholar]
- 19.Copeland LA, Zeber JE, Valenstein M, Blow FC. Racial disparity in the use of atypical antipsychotic medications among veterans. Am J Psychiatry. 2003;160:1817–1822. doi: 10.1176/appi.ajp.160.10.1817. [DOI] [PubMed] [Google Scholar]
- 20.Kuno E, Rothbard A. Racial disparities in antipsychotic prescription patterns for patients with schizophrenia. Am J Psychiatry. 2002;159:567–572. doi: 10.1176/appi.ajp.159.4.567. [DOI] [PubMed] [Google Scholar]
- 21.Domino ME, Swartz MS. Who Are the New Users of Antipsychotic Medications? Psychiatr Serv. 2008;59:507. doi: 10.1176/appi.ps.59.5.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Depp C, Ojeda VD, Mastin W, Unutzer J, Gilmer TP. Trends in Use of Antipsychotics and Mood Stabilizers Among Medicaid Beneficiaries With Bipolar Disorder, 2001–2004. Psychiatr Serv. 2008;59:1169. doi: 10.1176/ps.2008.59.10.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuvekas S, Taliaferro G. Pathways to Access: Health Insurance, the Health Care Delivery System, and Racial/Ethnic Disparities, 1996–1999. Health Aff (Millwood) 2003;22:139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 24.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feld P, Power B. Immigrants’ Access to Health Care after Welfare Reform: Findings from Focus Groups in Four Cities. Washington, D.C: Kaiser Commission on Medicaid and the Uninsured; 2000. [Google Scholar]
- 26.Holzer CE, Shea BM, Swanson JM, Leaf PJ, Myers JK, George L, Weissman MM, Bednarski P. The increased risk for specific psychiatric disorders among persons of low socioeconomic status. Am J Psychiatry. 1986 [Google Scholar]
- 27.Muntaner C, Eaton WW, Diala C, Kessler RC, Sorlie PD. Social class, assets, organizational control and the prevalence of common groups of psychiatric disorders. Soc Sci Med. 1998;47:2043–2053. doi: 10.1016/s0277-9536(98)00309-8. [DOI] [PubMed] [Google Scholar]
- 28.Chow J, Jaffee K, Snowden L. Racial/Ethnic Disparities in the Use of Mental Health Services in Poverty Areas. Am J Public Health. 2003;93:792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.AHRQ. MEPS HC-036BRR: 1996–2006 Replicates for Calculating Variances File. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 30.Zuvekas SH. Trends in mental health services use and spending, 1987–1996. Health Aff (Millwood) 2001;20:214–224. doi: 10.1377/hlthaff.20.2.214. [DOI] [PubMed] [Google Scholar]
- 31.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 34.Kessler R, Andrews G, Colpe L, Hiripi E, Mroczek D, Normand S, Walters E, Zaslavsky A. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 35.Ludman EJ, Katon W, Russo J, Von Korff M, Simon G, Ciechanowski P, Lin E, Bush T, Walker E, Young B. Depression and diabetes symptom burden. Gen Hosp Psychiatry. 2004;26:430–436. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Ciechanowski PS, Katon WJ, Russo JE. Depression and Diabetes Impact of Depressive Symptoms on Adherence, Function, and Costs. Arch Intern Med. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 37.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25:246–252. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 38.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res. 1996;5:215–238. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- 39.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, Massachusetts: The MIT press; 2002. Sample selection, attrition, and stratified sampling; pp. 587–590. [Google Scholar]
- 40.Koenker R. Quantile Regression. Cambridge University Press; 2005. [Google Scholar]
- 41.Koenker R, Hallock KF. Quantile Regression. J Econ Perspect. 2001;15:143–156. [Google Scholar]
- 42.Buchinsky M. Recent Advances in Quantile Regression Models: A Practical Guideline for Empirical Research. J Hum Resour. 1998;33:88–126. [Google Scholar]
- 43.Koenker R, Bassett G., Jr Regression quantiles. Econometrica. 1978;46:33–50. [Google Scholar]
- 44.Buntin M, Zaslavsky A. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23:525–542. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Manning W, Mullahy J. Estimating log models: To transform or not to transform. J Health Econ. 2001;20:461–495. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 46.Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20:897–916. doi: 10.1002/hec.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mullahy J. Econometric modeling of health care costs and expenditures: a survey of analytical issues and related policy considerations. Med Care. 2009;47:S104–S108. doi: 10.1097/MLR.0b013e31819c9593. [DOI] [PubMed] [Google Scholar]
- 48.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 49.Cook B, McGuire TG, Zaslavsky AM. Measuring Racial/Ethnic Disparities in Health Care: Methods and Practical Issues. Health Serv Res. 2012;47:1232–1254. doi: 10.1111/j.1475-6773.2012.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He J, Koretz D, McLaughlin KA, Petukhova M. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. 2012;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cook BL, Manning WG. Measuring racial/ethnic disparities across the distribution of health care expenditures. Health Serv Res. 2009;44:1603–1621. doi: 10.1111/j.1475-6773.2009.01004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pregibon D. Goodness of link tests for generalized linear models. Applied Statistics. 1980;29:15–24. [Google Scholar]
- 53.Archer KJ, Lemeshow S. Goodness-of-fit test for a logistic regression model fitted using survey sample data. Stata Journal. 2009;6:97–105. [Google Scholar]
- 54.Hosmer DW, Lemeshow S. Applied logistic regression analysis. New York: John Wiley & Sons; 1989. [Google Scholar]
- 55.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 56.Wells KB, Tang L, Miranda J, Benjamin B, Duan N, Sherbourne CD. The Effects of Quality Improvement for Depression in Primary Care at Nine Years: Results from a Randomized, Controlled Group-Level Trial. Health Serv Res. 2008;43:1952. doi: 10.1111/j.1475-6773.2008.00871.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rao J, Shao J. Modified balanced repeated replication for complex survey data. Biometrika. 1999;86:403–415. [Google Scholar]
- 58.Kraemer HC, Blasey CM. Centring in Regression Analyses: A Strategy to Prevent Errors in Statistical Inference. International Journal of Methods in Psychiatric Research. 2004;13:141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. J Gen Intern Med. 2007;22:289–293. doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Takeuchi DT, Sue S, Yeh M. Return rates and outcomes from ethnicity-specific mental health programs in Los Angeles. Am J Public Health. 1995;85:638–643. doi: 10.2105/ajph.85.5.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sue S, Dhindsa MK. Ethnic and racial health disparities research: Issues and problems. Health Educ Behav. 2006;33:459–469. doi: 10.1177/1090198106287922. [DOI] [PubMed] [Google Scholar]
- 62.Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Med Care. 2008;46:668–677. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zuvekas SH, Fleishman JA. Self-rated mental health and racial/ethnic disparities in mental health service use. Med Care. 2008;46:915–923. doi: 10.1097/MLR.0b013e31817919e5. [DOI] [PubMed] [Google Scholar]
- 64.Ojeda V, McGuire T. Gender and racial/ethnic differences in use of outpatient mental health and substance use services by depressed adults. Psychiatr Q. 2006;77:211–222. doi: 10.1007/s11126-006-9008-9. [DOI] [PubMed] [Google Scholar]
- 65.Leong F, Lau A. Barriers to providing effective mental health services to Asian Americans. Ment Health Serv Res. 2001;3:201–214. doi: 10.1023/a:1013177014788. [DOI] [PubMed] [Google Scholar]
- 66.Blank MB, Mahmood M, Fox JC, Guterbock T. Alternative mental health services: The role of the Black church in the South. Am J Public Health. 2002;92:1668–1672. doi: 10.2105/ajph.92.10.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Taylor RJ, Ellison CG, Chatters LM, Levin JS, Lincoln KD. Mental health services in faith communities: The role of clergy in black churches. Soc Work. 2000;45:73–87. doi: 10.1093/sw/45.1.73. [DOI] [PubMed] [Google Scholar]
- 68.Vega WA, Kolody B, Aguilar-Gaxiola S. Help seeking for mental health problems among Mexican Americans. Journal of Immigrant Health. 2001;3:133–140. doi: 10.1023/A:1011385004913. [DOI] [PubMed] [Google Scholar]
- 69.Snowden L. Bias in mental health assessment and intervention: theory and evidence. Am J Public Health. 2003;93:239–243. doi: 10.2105/ajph.93.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Atdjian S, Vega W. Disparities in mental health treatment in U. S. racial and ethnic minority groups: implications for psychiatrists. Psychiatr Serv. 2005;56:1600–1602. doi: 10.1176/appi.ps.56.12.1600. [DOI] [PubMed] [Google Scholar]
- 71.Scheffler R, Miller A. Demand analysis of mental health service use among ethnical sub populations. Inquiry. 1989;26:202–215. [PubMed] [Google Scholar]
- 72.Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega A. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr Serv. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- 73.Wang P, Lane M, Olfson M, Pincus H, Wells K, Kessler R. Twelve- Month Use of Mental Health Services in the United States. Arch Gen Psychiatry. 2005;629–640:629. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 74.Ryu H, Young WB, Kwak H. Differences in Health Insurance and Health Service Utilization Among Asian Americans: Method for Using the NHIS to Identify Unique Patterns Between Ethnic Groups. Int J Health Plann Manage. 2002;17:55–68. doi: 10.1002/hpm.652. [DOI] [PubMed] [Google Scholar]
- 75.Balsa A, McGuire T. Statistical discrimination in health care. J Health Econ. 2001;20:881–907. doi: 10.1016/s0167-6296(01)00101-1. [DOI] [PubMed] [Google Scholar]