Abstract
Herein, employing anatomical and dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI), we evaluated non-invasively, the in vivo, chemopreventive efficacy of inositol hexaphosphate (IP6), a major constituent of high fiber diets, against prostate tumor growth and progression in transgenic adenocarcinoma of the mouse prostate (TRAMP) model. Male TRAMP mice, beginning 4 weeks of age, were fed with 1, 2 or 4% (w/v) IP6 in drinking water or only drinking water till 28 weeks of age and monitored using MRI over the course of study. Longitudinal assessment of prostate volumes by conventional MRI and tumor vascularity by gadolinium-based DCE-MRI showed a profound reduction in tumor size partly due to anti-angiogenic effects by IP6 treatment. As potential mechanisms of IP6 efficacy, decrease in the expression of glucose transporter GLUT-4 protein together with an increase in levels of phospho-AMP-activated kinase (AMPKTh172) were observed in prostate tissues of mice from IP6 fed-groups, suggesting that IP6 is interfering with the metabolic events occurring in TRAMP prostate. Investigative metabolomics study utilizing quantitative high-resolution 1H-NMR on prostate tissue extracts showed that IP6 significantly decreased glucose metabolism and membrane phospholipid synthesis, in addition to causing an increase in myo-inositol levels in the prostate. Together, these findings show that oral IP6 supplement blocks PCa growth and angiogenesis in TRAMP model in conjunction with metabolic events involved in tumor sustenance. This results in energy deprivation within the tumor, suggesting a practical and translational potential of IP6 treatment in suppressing growth and progression of prostate cancer in humans.
Keywords: TRAMP, prostate cancer, inositol hexaphosphate, GLUT-4, Magnetic Resonance Imaging
Introduction
Prostate cancer (PCa) is the most frequently diagnosed malignancy in elderly American men; however, its incidence varies dramatically on a global level; both incidence and associated-mortality are lower in Asian compared to Western countries (1). Importantly, the incidence of occult/indolent form of PCa is similar globally despite dramatic difference in the occurrence of clinical malignancy (2). One possible explanation for this enigma could be ageing process, which inadvertently causes slow histopathological changes in the prostate, while environmental/dietary factors serve as a trigger for the progression to more aggressive forms and are thus involved in the promotion rather than initiation of PCa (2–4). In an effort to identify such etiological factors, several studies indicate that one of the possible causes is Western diet that includes highly processed foods (4–6). In the Asian diet, however, one essential component present ubiquitously is inositol hexaphosphate (IP6) or phytic acid which is a naturally-occurring hexaphosphorylated carbohydrate, present abundantly in high fiber content diets, most cereals, legumes, nuts and soybean (5, 7–9). Importantly, IP6 is already marketed as a dietary supplement owing to its anti-oxidant property and known beneficial effects such as prevention against the formation of kidney stone, high cholesterol, and heart and liver diseases (5, 6, 8, 9).
The fact that PCa incidence is lower in Asian men has triggered interest in IP6 as a possible factor in PCa prevention (5, 9). However, due to its metal chelating properties, IP6 is often referred to as an anti-nutrient by the nutritionists; holding its dietary intake responsible for mineral deficiencies (10, 11). Contrary to this, several cancer researchers emphasize that IP6 manifests as an anti-nutrient only when the diet is already poor in trace elements, and strongly recommend IP6 intake for its beneficial anti-cancer properties (6, 9, 12, 13). It is speculated that the anti-cancer effect of IP6 is mediated via its conversion to lower inositol phosphates which play essential roles in cellular signal transduction and regulation of cell growth and differentiation (6). Moreover, exogenously administered IP6 is quickly absorbed by the gastrointestinal tract and rapidly taken up by malignant cells (6, 14), thereby modulating their essential survival pathways; importantly IP6 has no cytostatic or cytotoxic effect on normal cells and tissues (6). In this regard, several research groups, including ours, have demonstrated the in vitro and in vivo anti-cancer efficacy of IP6 against a variety of cancers including PCa (5, 6, 9, 15–22). Earlier mechanistic studies by us have shown that IP6 possesses strong anticancer efficacy against both androgen-dependent and –independent PCa cell types wherein, it inhibits cell growth and causes G1 cell cycle arrest via modulation of cell cycle regulatory molecules, and induces apoptotic death (16, 21). Other studies demonstrated that IP6 impairs erbB1 receptor-associated mitogenic signaling and inhibits constitutive activation of NF-κB in DU145 cells and targets PI3K-AKT pathway in PCa cell lines (5, 15, 17, 18). In terms of its efficacy in pre-clinically PCa models, our recent studies reported the chemopreventive efficacy of IP6 against PCa growth and progression in transgenic adenocarcinoma of the mouse prostate (TRAMP) model (23, 24). However, one limitation of the previous study was that no detailed mechanistic investigations were performed; though preliminary findings showed a pro-apoptotic and an anti-proliferative effect (19).
Accordingly, in the present study, we fed different doses of IP6 in drinking water to four-week old TRAMP mice till 28 weeks of their age, and assessed the inhibitory effect of IP6 on tumor growth, progression and angiogenesis using longitudinal study parameters [employing conventional magnetic resonance imaging (MRI) and gadolinium-based dynamic contrast-enhanced (DCE-MRI)] as a criterion (25, 26) to simultaneously assess IP6 effect on prostate sizes/volume and tumor vascularization as a function of time, and to also elucidate the molecular events involved in IP6 efficacy. Furthermore, the metabolic activity in tumor tissues was also assessed by quantitative 1H-NMR metabolomics at the end of the study.
Materials and Methods
Animals and Treatment
Heterozygous TRAMP (C57BL/6) females were cross-bred with non-transgenic C57BL/6 breeder males, and progeny subjected to genotyping for PB-Tag as previously described (23). The routinely obtained four week-old TRAMP male mice were randomly distributed into positive control and treatment groups. Positive control mice were supplied with regular drinking water and the treatment groups were fed with 1%, 2%, and 4% (w/v) IP6 in regular drinking water for 24 weeks. For additional details on experimental design and drug doses, refer to supplementary information.
Magnetic Resonance Imaging
We employed MRI (27, 28) to (i) assess prostate and tumor sizes in the mouse using fast spin-echo proton density-weighted MRI, and (ii) non-invasively assess changes in tumor vascularization (perfusion and permeability) by gadolinium (Gd)-based DCE-MRI (fast spin echo continuous T1-acquisitions with 60 sec baseline followed by a bolus injection of 0.1 mmol/kg MultiHance via a tail catheter and 10 min of continuous MRI acquisition) (28). Bruker 4.7 Tesla/ 16-cm MRI/MRS PharmaScan (Bruker Medical, Billerica, MA) with a mouse volume transmitter/ receiver coil (36 mm diameter) was used for all MRI studies (at the Animal Imaging Shared Resources, University of Colorado Anschutz Medical Campus). All sequence parameters and image analysis are detailed in Troiani et al (27). Additional details are provided in supplementary materials and methods.
Necropsy and Histopathology
At the time of sacrifice, mice were euthanized by carbon-dioxide asphyxiation followed by exsanguination. Each mouse was weighed and lower urogenital tract (LUT) including bladder, seminal vesicles and prostate, was removed en bloc. LUT wet weight was recorded, and prostate gland/tumor was harvested, microdissected, partly snap-frozen and partly processed for histopathological and immunohistochemical (IHC) analyses as previously described (29).
Quantitative 1H-NMR Analyses
Snap frozen prostate tumor tissues were extracted using 8% perchloric acid (Sigma-Aldrich Co., St. Louis, MO) and analyzed by NMR as previously described (30, 31). All high-resolution 1H-NMR spectra were obtained at a Bruker 500 MHz DRX spectrometer (Bruker BioSpin, Billerica, MA) equipped with a standard 5-mm TXI probe, using 0.6 mmol/L trimethylsilylpropionic acid (TSP) as a chemical shift and concentration standard (30, 31). Absolute concentrations of 36 metabolites (normalized to the wet weights of each sample) were assessed and presented as micromole per mg of tissue (31, 32).
Statistical and Microscopic Analyses
All MRI and 1H-NMR analyses were performed by the MR scientists (NJS and KMH) who were blinded to the group assignment of the animals/samples. For metabolomics, absolute individual concentrations of distinguished biomarkers were analyzed by ANOVA followed by Tukey’s post-hoc test. Fishers’ Exact test was used to compare incidence of pathological lesions in different groups. All other data were analyzed by unpaired two-tailed Student’s t-test. The significance level was set at p<0.05 for all tests (Sigma Plot-version 9.01, Systat Software, CA and SPSS version 14.0, SPSS Inc., Chicago, IL).
Results
IP6 Feeding Reduces LUT Weight without any Apparent Toxicity
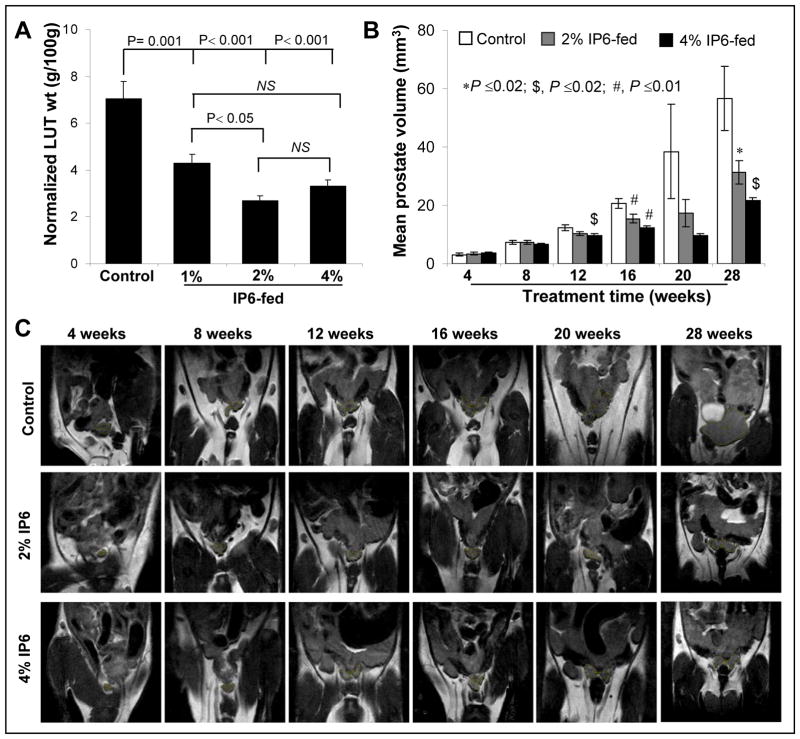
IP6 feeding did not show any significant changes in fluid consumption between positive control and 1% and 2% IP6-fed mice during entire study (data not shown). In 4% IP6-fed group, however, mice showed lower fluid consumption compared to other groups which could be attributed to the taste of the highly concentrated IP6 solution. In addition, IP6 feeding did not show considerable difference in diet consumption and body weight gain profiles between positive control and IP6-fed mice during entire study (data not shown). At necropsy, all animals were examined for gross pathology, and there was no evidence of edema and abnormal organ size or appearance in non-target organs. It is important to emphasize here that since earlier studies have reported that experimental rats fed with pure phytate for their life-time did not show any effect in serum or bone minerals (except for lower zinc concentration in bone of second generation rats) (6, 12, 13), we did not focus our efforts in determining the mineral bioavailability in the TRAMP mice in the present study. There was, however, a significant difference between the LUT weight (normalized to body weight) of positive control mice versus the IP6-fed groups. The normalized LUT weight of 1%, 2% and 4% IP6-fed groups was 39 (P=0.001), 62 (P<0.001) and 53% (P<0.001) lower than that of positive control group (Fig. 1A). In non-transgenic mice, IP6 feeding did not show any change in diet and fluid consumptions, and body weight gain profiles (data not shown). Also, no pathological changes in prostate or other organs were observed in non-transgenic mice in IP6-fed versus control groups (data not shown).
Fig. 1.
(A) Effect of IP6 feeding on the weight of LUT organs normalized to body weight. (B) IP6 feeding reduces prostate volume in TRAMP mice as assessed by MRI, performed as a function of time. Error bars indicate ± SEM. (C) Longitudinal assessment of prostate/tumor volume in TRAMP mice using non-invasive proton density-weighted MRI during IP6 feeding over a time period of 24 weeks, starting from 4 weeks till 28 weeks of mice age. Representative coronal PD MRI images (six TRAMP mice per each group were subjected to MRI) of prostate size are presented for untreated control (top panel), 2% IP6-fed (middle) and 4% IP6-fed mice (bottom). The prostate location and size are depictures as yellow ROI (regions of interest) on each image. NS, Not significant
IP6 Feeding Reduces Prostate Volume in TRAMP Mice (MRI-study)
Longitudinal assessment of prostatic/tumor volumes, from 4 weeks till 28 weeks of mice age, was performed in both positive control (untreated) and IP6-treated TRAMP mice (n=6/group), using non-invasive proton density-weighted MRI (Fig 1B & C). The results indicated that 2–4% IP6 feeding did not affect prostate volumes till 12 weeks of age (an initiation phase of the disease), but significantly decreased prostate volumes at 16 weeks of age till the end of the treatment (28 weeks of age) compared to untreated controls (Fig 1B & C). While both 2% and 4% IP6 doses caused a decrease in prostate/tumor volumes during the progression stages (Fig 1), 1% IP6 dose had no significant effect compared to positive control (data not shown).
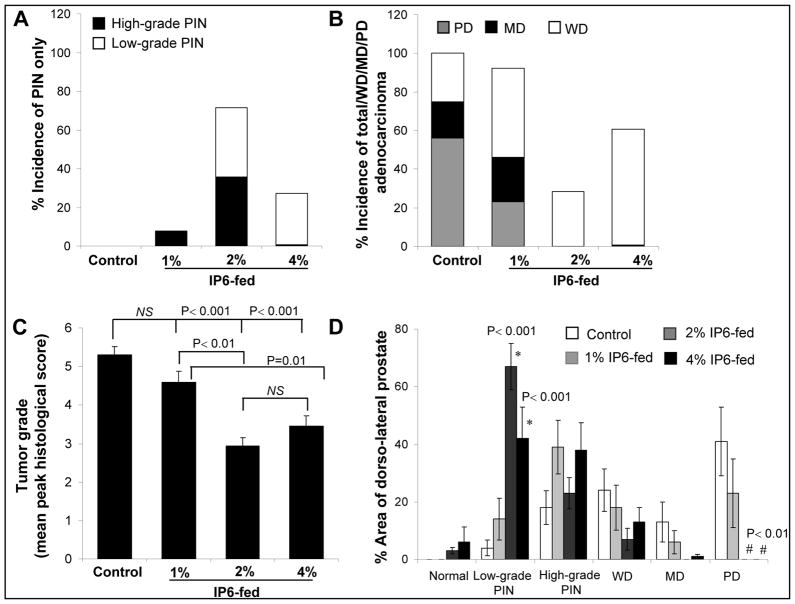
IP6 Feeding Inhibits PCa Progression
Using the classifications previously described (33, 34), the histopathological analysis of the H&E stained dorsolateral prostate showed that there was a marked difference in prostatic intraepithelial neoplasia (PIN) and adenocarcinoma incidences between positive control and IP6-fed groups (Fig. 2A & B). An overall increase in the incidence of more differentiated tumors in IP6-fed groups was also observed compared to positive controls, with a concomitant reduction in the incidence of more aggressive tumors in IP6-treated mice (Fig. 2B). Importantly, there was no incidence of poorly differentiated (PD) adenocarcinoma in both 2% and 4% IP6-fed groups compared to 56% incidence in positive controls. As shown in Figure 2C, there was also a significant reduction in tumor grade in IP6-fed groups; calculated on the basis of criterion described previously (33). The distribution of PIN lesions also indicated that there was a significant increase in the area covered by LGPIN lesions in the mice fed with 2% and 4% IP6 (Fig. 2D). More importantly, in 2% and 4% IP6-fed groups, about 3–6% area of prostate also displayed normal histology which was not the case in both 1% IP6 dose and positive control groups (Fig. 2D). In non-transgenic mice, prostate histopathology did not show any difference in control and IP6-fed group (data not shown). Together, these results suggest that IP6-feeding is effective in decreasing the progression of pre-malignant neoplastic lesions in the prostate of TRAMP mice to more aggressive forms of adenocarcinoma; however, these chemopreventive effects of IP6 do not seem to be dose-dependent; with 2% IP6 dose fairing better than the highest dose. Since the lowest dose of IP6 (1% IP6-fed group) was unable to decrease incidence and severity of prostatic lesions better than other two higher doses, we chose to limit our further mechanistic investigations to the groups that were fed with higher doses of IP6.
Fig. 2.
Inhibitory effect of different doses of IP6 on prostate tumor progression in TRAMP mice. Effect of IP6 feeding on, (A) incidence of low and high grade PIN; (B) adenocarcinoma lesions in dorsolateral prostate of TRAMP mice; (C) tumor grade of dorsolateral prostate in TRAMP mice. (D) Percent area of dorsolateral prostate of positive control and IP6-fed groups having histologically diagnosed PIN, WD, MD, and PD adenocarcinoma characteristics. Error bars indicate ± SEM. NS, Not significant
IP6 Feeding Reduces Proliferation Index and Increases Apoptosis in the Prostate of TRAMP Mice
The in vivo anti-proliferative effect in both 2% and 4% IP6-fed groups was significantly higher than untreated mice, though the effect of 2% IP6 feeding was relatively better (P=0.01) than 4% IP6 dose (Supplementary Figure 1A). Regarding in vivo apoptotic effect, whereas both doses of IP6 increased apoptotic cells in TRAMP prostate tissue, it was again 2% IP6-fed group that showed a statistically significant pro-apoptotic effect as evidenced by a 4-fold (P=0.01) increase in apoptotic cells (Supplementary Figure 1B).
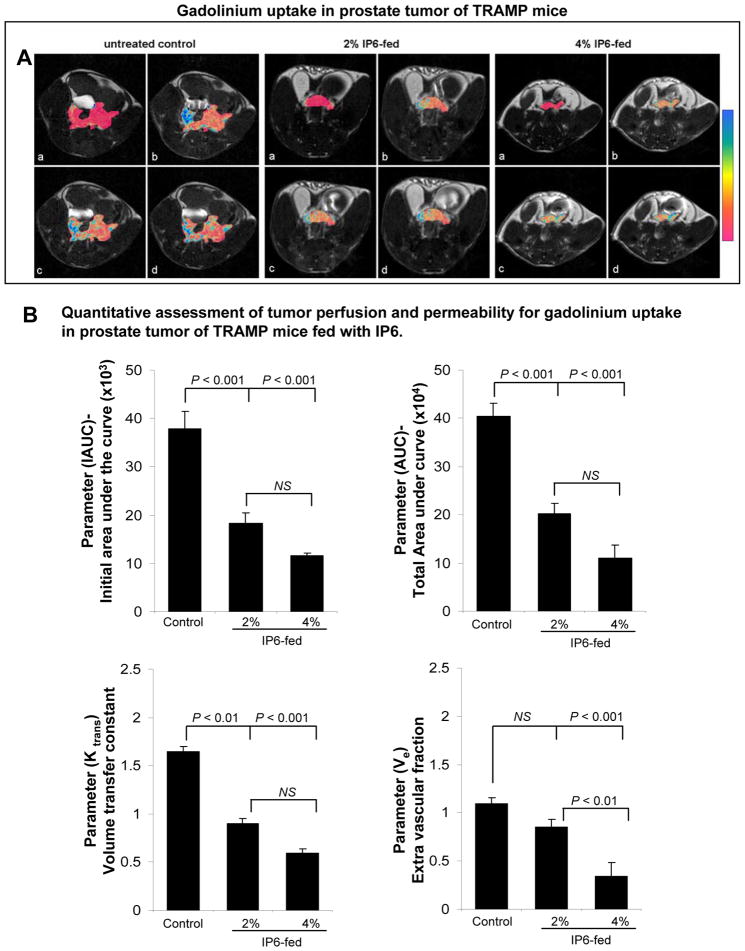
IP6 Feeding Inhibits Angiogenesis in TRAMP Mice (DCE-MRI and IHC study)
Since the ability of localized carcinoma to advance to invasive stages is dependant upon its ability to recruit new vasculature via angiogenesis (35), we also determined the effect of IP6 on tumor vasculature. In TRAMP mice, prostate vasculature undergoes a pro-angiogenic switch with increase in tumor grade leading to higher expression of pro-angiogenic factors resulting in increased microvessel density (MVD) which further promotes progression to invasive stages (35, 36). In this regard, we observed that IP6 feeding significantly decreased tumor perfusion/ permeability and MVD as indicated by DCE-MRI studies (based on gadolinium uptake and kinetics in prostate tissues as an indicator of angiogenesis) (Fig. 3A & B) and IHC staining for CD-31 (Supplementary Figure 1C), respectively. IP6 treatment led to a dose-dependent decrease (up to 3-fold by 4% IP6) in gadolinium IAUCs (initial gadolinium uptake in first 90 sec after gadolinium injection) which is an indicative for decreased tumor perfusion. The universal parameters for tumor vascularity (total AUC, the volume transfer constants Ktrans and the extravascular fractions Ve) were similarly decreased in IP6-fed groups. These results indicated that IP6 might be exerting its anti-angiogenic effect by affecting the expression of pro-angiogenic factors. IHC studies were done to support this assumption and to corroborate imaging results, where the expression of pro-angiogenic factor VEGF (35, 37) was significantly decreased in IP6-fed mice compared to controls (P<0.001, for both doses; Fig. 4A). Additional IHC studies were also carried to determine whether IP6 feeding also affects the expression of inducible nitric oxide synthase (iNOS), an enzyme involved in the production of nitric oxide (NO) which facilitates neo-vascularization and invasion (38). The data indicated that IP6 significantly decreases (31–34%, P<0.001 for both doses) iNOS immunoreactivity scores (Fig. 4B). As transcription factor NF-κB mediates transcription of genes which are associated with cancer initiation and progression, including those encoding for VEGF and iNOS (39), we next assessed whether IP6 interferes with the expression of these proteins via down-regulation of NF-κB activity. IHC analysis showed that IP6 does inhibit NF-κB activity as evidenced by a significant decrease in the nuclear expression of phospho NF-κB/p65 in the TRAMP prostate of both doses of IP6-fed mice compared to controls (Fig. 4C). Additional mechanistic studies delineating the anti-angiogenic effect of IP6 revealed that its activity was transduced by an upstream molecule, AKT, which is known to regulate NF-κB (40). Specifically, both 2% and 4% IP6-fed groups of mice showed a significantly reduced phospho AKT ser 473 levels in IHC staining in the TRAMP prostate (Fig. 4D). Together, these results suggested that IP6 feeding inhibits the recruitment of new vascular network during angiogenesis, by down regulating the expression of pro-angiogenic factors via a series of molecular events which in totality acted as a limiting factor that in turn restricted the ability of localized PIN/carcinoma to advance to more invasive stage.
Fig. 3.
Dose dependant effect of IP6 feeding on angiogenesis in prostate of TRAMP mice. (A) Representative DCE-MRI images in axial plane of TRAMP prostate/tumor. There are 4 panes per image: (a) top left, baseline (prior to Gd-injection); (b) top right, 4 min post-; (c) bottom left, 7 min post-; and (d) bottom right, 10 min post-gadolinium injection. The color scale represents incremental increase in signal intensity in the prostate. (B) Quantitative assessment of tumor perfusion and permeability for gadolinium uptake in prostate of TRAMP mice fed with IP6. Quantification of parameters is shown as mean and ± SEM (error bars) in each group. NS, Not significant
Fig. 4.
Dose dependant effect of IP6 feeding on biomarkers associated with survival and angiogenesis in dorsolateral prostate of TRAMP mice. IHC staining for (A) VEGF, (B) i-NOS, (C) pP65Ser536, and (D) pAKTSer473. Representative pictographs are depicted at ×400. Columns represent mean and ± SEM (error bars) in each group. NS, Not significant
IP6 Feeding Interferes with the Expression of Molecules Associated with Tumor Sustenance and Glucose Transportation in TRAMP Prostate
Additional IHC studies were next performed to examine IP6 effect on the expression of transmembrane glucose transporter (GLUT) proteins which mediate glucose uptake in the cells and thereby play an essential role in the first step of the glucose utilization cascade (41). Whereas there was no change in GLUT-1 (data not shown), the expression of GLUT-4 protein (both membrane and cytoplasmic) was significantly decreased (57% and 34%, P<0.001, for both doses) in the prostate of 2% and 4% IP6-fed mice compared to positive control (Fig. 5A); 2% IP6 dose produced significantly (P<0.01) stronger effect than 4%. The observed decrease in GLUT-4 protein levels suggested the potential of IP6 to decrease/limit the amount of glucose being pumped into the cells, which led us to predict that this decreased glucose uptake in the prostate of IP6-fed mice could result in a cellular stress associated with decreased ATP levels and increased AMP levels in the prostate (42). Further IHC studies were carried out to confirm this mechanistic assumption, which revealed that indeed there was an increase in the phosphorylated levels of AMP-activated kinase (AMPKTh172) (Fig. 5B). Specifically, the immunoreactivity scores for phospho-AMPKTh172 and its down streamtarget, phospho ACC (42, 43), were increased by ~2-folds (P<0.05- P<0.001, and P<0.01, for both doses, respectively) in the prostate of IP6-fed mice compared to positive controls (Fig. 5). Together, these findings suggested that IP6 was interfering with the metabolic events occurring in the TRAMP prostate tumor tissue, which might have an important role in its observed chemopreventive efficacy.
Fig. 5.
Dose dependant effect of IP6 feeding on molecules associated with tumor sustenance and glucose transportation in dorsolateral prostate of TRAMP mice. IHC staining for (A) GLUT-4, (B) pAMPKTh172 and (C) pACC Ser79. Representative pictographs are depicted at ×400. Columns represent mean and ± SEM (error bars) in each group. NS, Not significant.
IP6 Feeding Causes Metabolic Alterations in the TRAMP Prostate as Assessed by 1H-NMRS
To further confirm that IP6 feeding was indeed interfering with the metabolic events involved in TRAMP prostate malignancy (31), we subjected the prostate tissues to a metabolomics study utilizing 1H-NMRS (Table 1). A variety of cancerous tissues including that of prostate exhibit altered metabolic profile of choline containing metabolites; specifically, phosphatidylcholine (PtdCho) - the major phospholipid in the cell membrane- is reported to be increased in a variety of tumors (44, 45). Our results indicated that IP6 feeding decreased the levels of all membrane phospholipids including PtdCho and phosphatidylinositol (PtdIns, both p=0.04) indicating a specific inhibition of cell membrane biosynthesis in the prostate (Table. 1). Interestingly, the phospholipid precursors for PtdCho and PtdIns in the aqueous fraction were increased after IP6 feeding (phosphocholine and glycerophosphocholine, p=0.001, as well as myo-inositol, p=0.02). One of the most striking differences between positive control and IP6-fed group was the accumulation of fatty acids (especially mono-unsaturated fatty acids) and a decrease in cholesterol. Accumulation of lipids, while accompanied by a significant decrease in phospholipid levels, is another confirmation for deterioration in cell membranes. While normal prostate glands express relatively high concentrations of polyols compared to PCa lesions (46), it was interesting to observe increased concentrations of osmolyte myo-inositol and other polyols and sugars in IP6-fed group, which are significantly decreased during prostate tumor progression (Table 1). Furthermore, though glucose was present in prostate tissues, the levels were quite low, below NMR limit of quantification, in both IP6-fed and positive control mice. In our study, a decrease in lactate and alanine (end-products of glycolysis) was also observed in IP6-fed group compared to controls (Table 1). Furthermore, IP6 feeding caused an increase in the levels of glutathione (the antioxidant glutathione serves as a free radical scavenger) and decreased [PUFA/MUFA] ratios indicating an overall improved anti-oxidant defense and decreased necrotic fraction (32, 45) by IP6 feeding (Table 1).
Table 1.
Quantitative metabolic profile of prostatic tumor tissues of two study groups (i) positive control (untreated) TRAMP mice, and (ii) IP6-treated TRAMP mice (2% w/v IP6 in regular drinking water given for 24 weeks).*
| Metabolite
|
1H-NMRS
|
Untreated [μmol/g] | 2% IP6 [μmol/g]
|
|---|---|---|---|
| 1. Aromatic Acids | hydrophilic | 12.12±2.37 | 14.94±1.88 |
| 2. Adenosines | hydrophilic | 3.39±0.89 | 4.05±0.2 |
| 3. Nucleotides | hydrophilic | 1.18±0.77 | 1.11±0.07 |
| 4. Myo-Inositol | hydrophilic | 1.17±0.74 | 4.48±0.65 P=0.02 |
| 5. Polyols+Sugars | hydrophilic | 15.71±4.9 | 53.07±14.64 P=0.03 |
| 6. Taurine | hydrophilic | 11.90±3.17 | 13.15±0.28 |
| 7. PC+GPC | hydrophilic | 2.65±0.47 | 7.82±0.44 P<0.001 |
| 8. Total Choline | hydrophilic | 0.09±0.03 | 0.06±0.03 |
| 9. Total Creatine | hydrophilic | 3.50±0.47 | 6.27±1.8 |
| 10. GSH | hydrophilic | 0.53±0.17 | 0.58±0.05 |
| 11. Citrate | hydrophilic | 0.43±0.23 | 0.32±0.01 |
| 12. Methionine | hydrophilic | 1.86±0.73 | 3.53±0.61 P<0.001 |
| 13. Total Glutathione | hydrophilic | 0.88±0.21 | 2.91±0.60 P=0.01 |
| 14. Glutamine | hydrophilic | 0.60±0.09 | 0.99±0.14 P=0.01 |
| 15. Succinate | hydrophilic | 0.83±0.22 | 2.07±0.39 P=0.01 |
| 16. Glutamate | hydrophilic | 3.34±0.56 | 2.58±0.32 P=0.04 |
| 17. Ketone Bodies | hydrophilic | 1.01±0.18 | 0.58±0.28 P=0.02 |
| 18. Total CH2-, CH3 | hydrophilic | 7.71±1.62 | 9.11±0.42 |
| 19. Acetate | hydrophilic | 0.02±0.02 | 1.91±0.36 P=0.01 |
| 20. Lysine+Arginine | hydrophilic | 2.26±0.31 | 2.10±0.17 |
| 21. Alanine | hydrophilic | 3.19±0.22 | 1.60±0.27 P<0.001 |
| 22. Lactate | hydrophilic | 9.86±0.87 | 7.84±1.09 |
| 23. Hydroxybutyrate | hydrophilic | 0.51±0.17 | 1.32±0.34 |
| 24. Essential Amino Acids | hydrophilic | 4.59±0.72 | 4.82±0.04 |
| 25. MUFA | lipids | 5.44±3.56 | 36.84±18.77 P=0.04 |
| 26. TAG | lipids | 6.07±0.3 | 18.55±5.61 P=0.03 |
| 27. Glycerol-Plipids | lipids | 14.57±1.69 | 14.04±0.31 |
| 28. PtdCho | lipids | 8.07±1.55 | 5.67±0.34 P=0.04 |
| 29. PtdIns | lipids | 2.32±1.0 | 0.94±0.28 P=0.04 |
| 30. Total Colines (Lipids) | lipids | 7.74±1.3 | 4.68±0.44 P=0.04 |
| 31. PtdEth | lipids | 1.95±0.22 | 1.17±0.63 |
| 32. PUFA | lipids | 27.32±2.93 | 27.97±7.45 |
| 33. Fatty Acids | lipids | 34.73±7.77 | 108.03±34.58 P=0.02 |
| 34. (CH2)n Lipids | lipids | 323.06±65.82 | 777.87±210.28 P=0.02 |
| 35. Total Lipids | lipids | 67.30±14.38 | 97.88±19.64 P=0.05 |
| 36. Cholesterol | lipids | 5.82±0.45 | 3.56±0.35 P=0.02 |
| 37. [PUFA/MUFA] | lipids | 6.20±2.83 | 0.88±0.35 P=0.03 |
All data are given in μmol of metabolite normalized to prostate tissue weight [μmol/g] and presented as mean ± S.D (n=4 for each group). Cho, choline; GPC, glycerophosphocholine; GSH, reduced glutathione; MUFA, mono-unsaturated fatty acids; PC, phosphocholine; PtdCho, phosphatidylcholine; PtdEth, phosphatidylethanolamine; PUFA, poly-unsaturated fatty acids.
Discussion
Herein, we applied multi-parametric MRI on TRAMP mouse prostate consisting of a combination of anatomical proton density-weighted imaging for longitudinal tumor growth and DCE-MRI for tumor perfusion and permeability, to evaluate IP6 effect on prostate tumorigenesis as a function of time. This non-invasive imaging technique showed that 1% IP6 dose was not significantly effective, but 2% and 4% IP6 doses showed a significant decrease in prostate volume after 16 weeks of mouse age, though they were ineffective in inhibiting tumorigenesis before this time point. These results suggest that IP6 does not interfere with PIN development; an initial stage of prostate tumorigenesis (23, 24). However, our results highlight the potential of IP6 to interfere with the events involved in transformation of neoplastic lesions to more advanced forms of the disease that are initiated with increasing age of TRAMP mice (3, 29, 35) and cause the prostate to endure an insult of pro-angiogenic events (24, 29, 35). Histopathological evaluation further corroborated MRI imaging findings where IP6 had no inhibitory effect on PIN formation but decreased adenocarcinoma lesions. In fact, a higher incidence of PIN lesions and more differentiated tumors were observed in TRAMP prostate fed with 2% and 4% IP6. Overall, while we expected IP6 to display a dose-dependant efficacy at 1, 2 and 4% doses, the results showed that 2% IP6 was an optimum dose executing significant anti-tumor efficacy. Notably, 4% IP6 dose, though non-toxic, was less effective than 2% dose. To address this discrepancy, since IP6 feeding was done in drinking water, first we analyzed the fluid consumption data of different treatment groups, and found that the mice in 4% IP6 group consumed the least water (data not shown). Once corrected for water consumption and IP6 concentration, the 4% IP6-fed group of mice actually consumed IP6 that was even less than 2% IP6-fed group, which supports the IP6 efficacy outcomes as optimum at 2% dose observed by us in this study.
Regarding our imaging approach, while volumetric assessment by MRI has been used as a “gold-standard” for treatment response to chemotherapeutic agents, it falls short in explaining the mechanisms of action of novel targeted therapies. A novel functional imaging DCE-MRI technique was applied in this study for non-invasive assessment of tumor angiogenesis. This analysis showed that IP6 feeding inhibits the development of new vasculature in TRAMP prostate which was later corroborated by IHC staining for CD-31. As a pertinent mechanism, IP6 was found to decrease the transcriptional activity of NFκB, possibly resulting in decreased expression of its downstream targets, such as VEGF and iNOS. These effects of IP6 were consistent with our earlier findings in PCa cell lines in culture and xenografts (5, 18).
Rapid cellular proliferation during tumorigenesis is associated with enhanced glucose uptake and increased metabolism (45), and we presumed that IP6 feeding interferes with the overall metabolism of the prostate tissue/tumor as one of the mechanisms of its prostate cancer chemopreventive efficacy. Notably, our results indicated that IP6 has a significant effect on the glucose transport by the prostatic cells which resulted in energy restrictions within the tumor. To meet bioenergy requirements, tumor cells display deregulation of the transporter GLUT proteins, which aids in the incorporation of higher amounts of glucose within these tumor cells, compared to normal cells (41). Recent studies have shown that both GLUT-1 and GLUT-4 are aberrantly expressed in many tumors and thus provide the cancer cells with a metabolic advantage (41). Importantly, GLUT-4 is expressed in IGF-I-responsive tissues (41) and therefore, increased levels of IGF-I receptor, as in certain cancer states (47), could lead to aberrant expression of GLUT-4 which in turn could alter glucose metabolism. While previous studies by us and others have reported the over expression of IGF-1 related receptor, IGF1-Rβ, in TRAMP tumor tissue (33, 47), our present study further identifies the over expression of GLUT-4 protein in the TRAMP prostate. Importantly, in line with our recently studies showing inhibition of IGF-1/PI3K-AKT signaling pathway by IP6 in human PCa cell lines (17), in present study, we observed a decrease in phospho Akt ser 473 and GLUT-4 protein in the prostate of TRAMP mice fed with IP6. Whereas a decrease in the expression of phospho Akt ser 473 by IP6 could be a result of inhibition of PI3K-Akt signaling (5, 48, 49), a decrease in GLUT-4 expression (both membrane/cytoplasmic) indicated decreased glucose consumption by prostatic tissue in IP6-fed mice. Importantly, 1H-NMRS results showed that there were very low levels of glucose in the prostates of both positive control and IP6-fed mice. Considering GLUT-4 expression in our study, one interpretation could be that a decrease in glucose levels in the prostate of positive control group of mice is due to increased consumption of this sugar by the tumor cells, which are highly proliferative and consume more glucose to meet their increased bioenergy requirements. However, in IP6-fed mice, the low levels of glucose are related to overall decrease in glucose uptake by the prostatic tissue via a decreased expression of GLUT-4. Indeed, in support of this assumption, the levels of lactate and alanine (end products of glycolysis) were reduced in IP6-treated prostatic tissues compared to untreated positive control group.
Limited source of metabolic energy activates AMPK due to altered AMP to ATP ratio, which could alter the activity of ACC; a precursor for fatty acid synthesis (42). We observed increased levels of both phospho-AMPK (activated AMPK) and phospho-ACC by IP6 feeding in the prostatic tissues. These results are important, as in vitro studies by different research, translating the effect of limited glucose supply on normal and malignant cells, have shown that glucose withdrawal leads to cellular death in tumors through distinct mechanisms (50). Specifically, in some tumors, the mechanism of cell death seems to be ATP depletion, which in turn activates the mitochondrial death cascade leading to apoptotic death (50). Interestingly, IP6 feeding showed a statistically significant pro-apoptotic effect in TRAMP prostate tissue. Furthermore, the NMR metabolomics study revealed that though the levels of fatty acids were increased in the prostate tissue from IP6-fed mice (possibly due to an increase in cell membrane degradation and accumulation of fatty acids and lipids), a significant decrease was evident in cell membrane phospholipds (PtdCho and PtdIns) as an indicator of decreased cell membrane biosynthesis (decreased proliferation rates). Also, a significant increase in total glutathione levels in the prostatic tissue of IP6-fed mice was observed suggesting that IP6 inhibits PCa progression also in part by increasing antioxidant glutathione levels, which serves as a free radical scavenger. Another, striking effect of IP6-feeding was increased levels of myo-inositol; its decreased expression is reported with increased malignancy in prostate (46).
In summary, our results are both novel and highly significant in establishing that IP6 suppresses growth and progression of PCa via its ability to alter tumor vascularity and the energy generating metabolic events in the tumor cells. Since, these mechanistic events eventually result in an arrest of tumor grade at neoplastic stages; the observed chemopreventive effect of IP6 against PCa could have translational potential in controlling the clinical progression of PCa in the patients diagnosed early at the PIN stage of the disease.
Supplementary Material
Acknowledgments
Grant support: NCI RO1 grant CA116636; NCI Cancer Center P30 CA046934; NCRR CTSA UL1 RR025780.
Footnotes
Disclosure of potential conflicts of interest: No potential conflicts of interest were identified by any authors of this manuscript.
References
- 1.Gronberg H. Prostate cancer epidemiology. Lancet. 2003;361:859–64. doi: 10.1016/S0140-6736(03)12713-4. [DOI] [PubMed] [Google Scholar]
- 2.Ko YJ, Bubley GJ. Prostate cancer in the older man. Oncology (Williston Park) 2001;15:1113–31. [PubMed] [Google Scholar]
- 3.Bhatt RS, Bubley GJ. The challenge of herbal therapies for prostate cancer. Clin Cancer Res. 2008;14:7581–2. doi: 10.1158/1078-0432.CCR-08-2316. [DOI] [PubMed] [Google Scholar]
- 4.Brand TC, Canby-Hagino ED, Pratap Kumar A, Ghosh R, Leach RJ, Thompson IM. Chemoprevention of prostate cancer. Hematol Oncol Clin North Am. 2006;20:831–43. doi: 10.1016/j.hoc.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Singh RP, Agarwal R. Prostate cancer and inositol hexaphosphate: efficacy and mechanisms. Anticancer Res. 2005;25:2891–903. [PubMed] [Google Scholar]
- 6.Vucenik I, Shamsuddin AM. Protection against cancer by dietary IP6 and inositol. Nutr Cancer. 2006;55:109–25. doi: 10.1207/s15327914nc5502_1. [DOI] [PubMed] [Google Scholar]
- 7.Fox CH, Eberl M. Phytic acid (IP6), novel broad spectrum anti-neoplastic agent: a systematic review. Complement Ther Med. 2002;10:229–34. doi: 10.1016/s0965-2299(02)00092-4. [DOI] [PubMed] [Google Scholar]
- 8.Jariwalla RJ. Rice-bran products: phytonutrients with potential applications in preventive and clinical medicine. Drugs Exp Clin Res. 2001;27:17–26. [PubMed] [Google Scholar]
- 9.Vucenik I, Shamsuddin AM. Cancer inhibition by inositol hexaphosphate (IP6) and inositol: from laboratory to clinic. J Nutr. 2003;133:3778S–84S. doi: 10.1093/jn/133.11.3778S. [DOI] [PubMed] [Google Scholar]
- 10.Brown KH, Solomons NW. Nutritional problems of developing countries. Infectious disease clinics of North America. 1991;5:297–317. [PubMed] [Google Scholar]
- 11.Raboy V. The ABCs of low-phytate crops. Nature biotechnology. 2007;25:874–5. doi: 10.1038/nbt0807-874. [DOI] [PubMed] [Google Scholar]
- 12.Grases F, Simonet BM, Perello J, Costa-Bauza A, Prieto RM. Effect of phytate on element bioavailability in the second generation of rats. J Trace Elem Med Biol. 2004;17:229–34. doi: 10.1016/S0946-672X(04)80023-3. [DOI] [PubMed] [Google Scholar]
- 13.Vucenik I, Yang GY, Shamsuddin AM. Inositol hexaphosphate and inositol inhibit DMBA-induced rat mammary cancer. Carcinogenesis. 1995;16:1055–8. doi: 10.1093/carcin/16.5.1055. [DOI] [PubMed] [Google Scholar]
- 14.Grases F, Simonet BM, Vucenik I, Perello J, Prieto RM, Shamsuddin AM. Effects of exogenous inositol hexakisphosphate (InsP(6)) on the levels of InsP(6) and of inositol trisphosphate (InsP(3)) in malignant cells, tissues and biological fluids. Life Sci. 2002;71:1535–46. doi: 10.1016/s0024-3205(02)01927-6. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal C, Dhanalakshmi S, Singh RP, Agarwal R. Inositol hexaphosphate inhibits constitutive activation of NF- kappa B in androgen-independent human prostate carcinoma DU145 cells. Anticancer Res. 2003;23:3855–61. [PubMed] [Google Scholar]
- 16.Agarwal C, Dhanalakshmi S, Singh RP, Agarwal R. Inositol hexaphosphate inhibits growth and induces G1 arrest and apoptotic death of androgen-dependent human prostate carcinoma LNCaP cells. Neoplasia. 2004;6:646–59. doi: 10.1593/neo.04232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gu M, Raina K, Agarwal C, Agarwal R. Inositol hexaphosphate downregulates both constitutive and ligand-induced mitogenic and cell survival signaling, and causes caspase-mediated apoptotic death of human prostate carcinoma PC-3 cells. Mol Carcinog. 2010;49:1–12. doi: 10.1002/mc.20560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gu M, Roy S, Raina K, Agarwal C, Agarwal R. Inositol hexaphosphate suppresses growth and induces apoptosis in prostate carcinoma cells in culture and nude mouse xenograft: PI3K-Akt pathway as potential target. Cancer Res. 2009;69:9465–72. doi: 10.1158/0008-5472.CAN-09-2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raina K, Rajamanickam S, Singh RP, Agarwal R. Chemopreventive efficacy of inositol hexaphosphate against prostate tumor growth and progression in TRAMP mice. Clin Cancer Res. 2008;14:3177–84. doi: 10.1158/1078-0432.CCR-07-5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shamsuddin AM, Yang GY. Inositol hexaphosphate inhibits growth and induces differentiation of PC-3 human prostate cancer cells. Carcinogenesis. 1995;16:1975–9. doi: 10.1093/carcin/16.8.1975. [DOI] [PubMed] [Google Scholar]
- 21.Singh RP, Agarwal C, Agarwal R. Inositol hexaphosphate inhibits growth, and induces G1 arrest and apoptotic death of prostate carcinoma DU145 cells: modulation of CDKI-CDK-cyclin and pRb-related protein-E2F complexes. Carcinogenesis. 2003;24:555–63. doi: 10.1093/carcin/24.3.555. [DOI] [PubMed] [Google Scholar]
- 22.Singh RP, Sharma G, Mallikarjuna GU, Dhanalakshmi S, Agarwal C, Agarwal R. In vivo suppression of hormone-refractory prostate cancer growth by inositol hexaphosphate: induction of insulin-like growth factor binding protein-3 and inhibition of vascular endothelial growth factor. Clin Cancer Res. 2004;10:244–50. doi: 10.1158/1078-0432.ccr-1080-3. [DOI] [PubMed] [Google Scholar]
- 23.Greenberg NM, DeMayo F, Finegold MJ, Medina D, Tilley WD, Aspinall JO, et al. Prostate cancer in a transgenic mouse. Proc Natl Acad Sci U S A. 1995;92:3439–43. doi: 10.1073/pnas.92.8.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaplan-Lefko PJ, Chen TM, Ittmann MM, Barrios RJ, Ayala GE, Huss WJ, et al. Pathobiology of autochthonous prostate cancer in a pre-clinical transgenic mouse model. Prostate. 2003;55:219–37. doi: 10.1002/pros.10215. [DOI] [PubMed] [Google Scholar]
- 25.Oto A, Yang C, Kayhan A, Tretiakova M, Antic T, Schmid-Tannwald C, et al. Diffusion-weighted and dynamic contrast-enhanced MRI of prostate cancer: correlation of quantitative MR parameters with Gleason score and tumor angiogenesis. AJR American journal of roentgenology. 2011;197:1382–90. doi: 10.2214/AJR.11.6861. [DOI] [PubMed] [Google Scholar]
- 26.Verma S, Turkbey B, Muradyan N, Rajesh A, Cornud F, Haider MA, et al. Overview of dynamic contrast-enhanced MRI in prostate cancer diagnosis and management. AJR American journal of roentgenology. 2012;198:1277–88. doi: 10.2214/AJR.12.8510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Troiani T, Serkova NJ, Gustafson DL, Henthorn TK, Lockerbie O, Merz A, et al. Investigation of two dosing schedules of vandetanib (ZD6474), an inhibitor of vascular endothelial growth factor receptor and epidermal growth factor receptor signaling, in combination with irinotecan in a human colon cancer xenograft model. Clin Cancer Res. 2007;13:6450–8. doi: 10.1158/1078-0432.CCR-07-1094. [DOI] [PubMed] [Google Scholar]
- 28.Degrassi A, Russo M, Scanziani E, Giusti A, Ceruti R, Texido G, et al. Magnetic resonance imaging and histopathological characterization of prostate tumors in TRAMP mice as model for pre-clinical trials. Prostate. 2007;67:396–404. doi: 10.1002/pros.20511. [DOI] [PubMed] [Google Scholar]
- 29.Raina K, Rajamanickam S, Singh RP, Deep G, Chittezhath M, Agarwal R. Stage-specific inhibitory effects and associated mechanisms of silibinin on tumor progression and metastasis in transgenic adenocarcinoma of the mouse prostate model. Cancer Res. 2008;68:6822–30. doi: 10.1158/0008-5472.CAN-08-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klawitter J, Anderson N, Klawitter J, Christians U, Leibfritz D, Eckhardt SG, et al. Time-dependent effects of imatinib in human leukaemia cells: a kinetic NMR-profiling study. Br J Cancer. 2009;100:923–31. doi: 10.1038/sj.bjc.6604946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raina K, Serkova NJ, Agarwal R. Silibinin feeding alters the metabolic profile in TRAMP prostatic tumors: 1H-NMRS-based metabolomics study. Cancer Res. 2009;69:3731–5. doi: 10.1158/0008-5472.CAN-09-0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serkova NJ, Niemann CU. Pattern recognition and biomarker validation using quantitative 1H-NMR-based metabolomics. Expert Rev Mol Diagn. 2006;6:717–31. doi: 10.1586/14737159.6.5.717. [DOI] [PubMed] [Google Scholar]
- 33.Raina K, Blouin MJ, Singh RP, Majeed N, Deep G, Varghese L, et al. Dietary feeding of silibinin inhibits prostate tumor growth and progression in transgenic adenocarcinoma of the mouse prostate model. Cancer Res. 2007;67:11083–91. doi: 10.1158/0008-5472.CAN-07-2222. [DOI] [PubMed] [Google Scholar]
- 34.Shappell SB, Thomas GV, Roberts RL, Herbert R, Ittmann MM, Rubin MA, et al. Prostate pathology of genetically engineered mice: definitions and classification. The consensus report from the Bar Harbor meeting of the Mouse Models of Human Cancer Consortium Prostate Pathology Committee. Cancer Res. 2004;64:2270–305. doi: 10.1158/0008-5472.can-03-0946. [DOI] [PubMed] [Google Scholar]
- 35.Huss WJ, Hanrahan CF, Barrios RJ, Simons JW, Greenberg NM. Angiogenesis and prostate cancer: identification of a molecular progression switch. Cancer Res. 2001;61:2736–43. [PubMed] [Google Scholar]
- 36.Ozawa MG, Yao VJ, Chanthery YH, Troncoso P, Uemura A, Varner AS, et al. Angiogenesis with pericyte abnormalities in a transgenic model of prostate carcinoma. Cancer. 2005;104:2104–15. doi: 10.1002/cncr.21436. [DOI] [PubMed] [Google Scholar]
- 37.Marti HH, Risau W. Systemic hypoxia changes the organ-specific distribution of vascular endothelial growth factor and its receptors. Proc Natl Acad Sci U S A. 1998;95:15809–14. doi: 10.1073/pnas.95.26.15809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh RP, Agarwal R. Inducible nitric oxide synthase-vascular endothelial growth factor axis: a potential target to inhibit tumor angiogenesis by dietary agents. Curr Cancer Drug Targets. 2007;7:475–83. doi: 10.2174/156800907781386632. [DOI] [PubMed] [Google Scholar]
- 39.Greten FR, Karin M. The IKK/NF-kappaB activation pathway-a target for prevention and treatment of cancer. Cancer Lett. 2004;206:193–9. doi: 10.1016/j.canlet.2003.08.029. [DOI] [PubMed] [Google Scholar]
- 40.Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 41.Calvo MB, Figueroa A, Pulido EG, Campelo RG, Aparicio LA. Potential role of sugar transporters in cancer and their relationship with anticancer therapy. Int J Endocrinol. 2010;2010:1–14. doi: 10.1155/2010/205357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang W, Zhu Z, Thompson HJ. Dietary energy restriction modulates the activity of AMP-activated protein kinase, Akt, and mammalian target of rapamycin in mammary carcinomas, mammary gland, and liver. Cancer Res. 2008;68:5492–9. doi: 10.1158/0008-5472.CAN-07-6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jansen M, Ten Klooster JP, Offerhaus GJ, Clevers H. LKB1 and AMPK family signaling: the intimate link between cell polarity and energy metabolism. Physiol Rev. 2009;89:777–98. doi: 10.1152/physrev.00026.2008. [DOI] [PubMed] [Google Scholar]
- 44.Glunde K, Serkova NJ. Therapeutic targets and biomarkers identified in cancer choline phospholipid metabolism. Pharmacogenomics. 2006;7:1109–23. doi: 10.2217/14622416.7.7.1109. [DOI] [PubMed] [Google Scholar]
- 45.Griffin JL, Shockcor JP. Metabolic profiles of cancer cells. Nat Rev Cancer. 2004;4:551–61. doi: 10.1038/nrc1390. [DOI] [PubMed] [Google Scholar]
- 46.Serkova NJ, Gamito EJ, Jones RH, O’Donnell C, Brown JL, Green S, et al. The metabolites citrate, myo-inositol, and spermine are potential age-independent markers of prostate cancer in human expressed prostatic secretions. Prostate. 2008;68:620–8. doi: 10.1002/pros.20727. [DOI] [PubMed] [Google Scholar]
- 47.Pollack MN. Insulin, insulin-like growth factors, insulin resistance, and neoplasia. Am J Clin Nutr. 2007;86:s820–2. doi: 10.1093/ajcn/86.3.820S. [DOI] [PubMed] [Google Scholar]
- 48.Chen N, Ma WY, Dong Z. Inositol hexaphosphate inhibits ultraviolet B-induced signal transduction. Mol Carcinog. 2001;31:139–44. doi: 10.1002/mc.1048. [DOI] [PubMed] [Google Scholar]
- 49.Huang C, Ma WY, Hecht SS, Dong Z. Inositol hexaphosphate inhibits cell transformation and activator protein 1 activation by targeting phosphatidylinositol-3′ kinase. Cancer Res. 1997;57:2873–8. [PubMed] [Google Scholar]
- 50.Jelluma N, Yang X, Stokoe D, Evan GI, Dansen TB, Haas-Kogan DA. Glucose withdrawal induces oxidative stress followed by apoptosis in glioblastoma cells but not in normal human astrocytes. Mol Cancer Res. 2006;4:319–30. doi: 10.1158/1541-7786.MCR-05-0061. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.