Abstract
Aims
Contingency management (CM) uses tangible incentives to systematically reinforce abstinence and is among the most efficacious psychosocial substance abuse treatments. This study assessed the feasibility and initial efficacy of a portable CM procedure designed to address technical limitations for detecting drinking that have prevented using CM for alcohol problems.
Design
Participants received a cell phone, breathalyzer, and training on video-recording alcohol breath tests (BrACs) and texting results. For 4 weeks, staff texted participants 1–3 times daily indicating a BrAC was due within the hour. Participants were randomized to (1) modest compensation for submitting dated time-stamped BrAC videos regardless of results or (2) the same plus CM with escalating vouchers for on-time alcohol-negative tests (n-BrAC; <02 g/dL). Thank you texts were sent, with CM patients also informed of results-based earnings.
Setting
Participants’ natural environment.
Participants
Adults (N=30; ≥21 years) who drank frequently but not physiologically dependent.
Measurements
Drinking and related problems were assessed at Intake and Week 4. BrACs and self-reports of drinking were collected throughout. The primary outcome was percent of n-BrACs. Other outcomes were longest duration of consecutive n-BrACs (LDA) and self-reports of drinking.
Findings
On average, 88.6% (10.4%) of BrACs were submitted on time, without group differences (p>.5). Percent of n-BrACs and LDA were greater with CM, and there was an interaction effect on drinking frequency and negative consequences, with decreases over time with CM (p=.00; effect sizes d=.52 to .62).
Conclusion
Cell phone technology may be useful for extending CM to treatment for alcohol problems.
Keywords: alcohol, abstinence, cell phone, contingency management, mobile, reinforcement
Introduction
Excessive alcohol use is a major source of morbidity and mortality [1]. Approximately 17.6 million (8.5%) American adults have alcohol abuse or dependence [2], and 41.4% of substance abuse treatment admissions are for alcohol [3]. Most patients do not complete treatment successfully [4], and relapse rates are high [5].
Contingency management (CM) is among the most efficacious psychosocial treatments for substance use disorders [6;7;8] and holds potential to improve alcohol outcomes. CM utilizes tangible incentives to reinforce abstinence. For example, patients submit biologic samples two to three times per week and earn vouchers exchangeable for goods and services for tests that read negative. Voucher amounts typically escalate for each consecutive negative test to promote sustained abstinence, a reliable predictor of long-term outcomes, and vouchers reset when abstinence does not occur. CM is efficacious for increasing abstinence from cocaine, opiates, benzodiazepines, marijuana, and cigarette smoking [9;10].
Laboratory and clinical studies suggest that CM might also be useful for treating alcohol problems. Petry et al. [11] found that a greater percentage of alcohol-dependent veterans randomized to CM for alcohol-negative breath tests (n-BrACs) remained abstinent and had a longer time until relapse than standard care patients. However, Helmus et al. [12] reinforced twice weekly n-BrACs in dual diagnosis patients and found all tests were alcohol-negative despite reports of frequent drinking. In fact, alcohol measured in urine, blood, and breath peaks about 1 hour following consumption and is eliminated rapidly, requiring multiple tests daily to detect all use. Importantly, testing frequency is crucial to the effectiveness of CM [7]. Infrequent reinforcement of abstinence may result in insufficient exposure to incentives to improve outcomes.
One advance that improves detection of alcohol involves continuous alcohol monitoring devices (e.g., SCRAMx®) that constantly detect transdermal alcohol. However, SCRAMx® may have limited feasibility outside of the judicial system where it is typically used. Costs are high, and they resemble location monitoring devices, which may affect acceptability. By comparison, cell phones are widely accepted and familiar technology that may be useful, in conjunction with breathalyzers, to reliably and validly monitor and reinforce alcohol abstinence.
Research on cell phones to address barriers to detecting alcohol is lacking, but the smoking literature provides a parallel. Smoking is typically detected via expired carbon monoxide (CO). The short half-life of CO necessitates multiple tests daily to detect all smoking, as with alcohol. Dallery and colleagues [13;14] evaluated an internet-based CM protocol designed to address problems associated with frequent testing for smoking. Participants were provided a study laptop, webcam, CO monitor, and study e-mail address. Participants self-tested their CO level, recorded the process, reported results via webcam twice daily for four weeks, and earned vouchers for smoking-negative tests; 97.5% of tests were completed, and CM reduced smoking relative to baseline [14].
This study is the first to examine the feasibility of using cell phone technology to monitor real-world drinking and administer CM. Cell phones are user-friendly, widely available, and mobile, and can be used for daily surveys with good adherence [15]. The primary aim was to assess the efficacy of cell phone-based CM for reducing drinking as assessed by proportion of n-BrACs. CM effects on other indices of drinking and alcohol-related problems were considered likely. Exploratory aims were to assess the validity and acceptability of the procedures. If feasible, effective, and valid, these procedures could broaden the practical application of CM to treating alcohol problems.
Methods
Sample
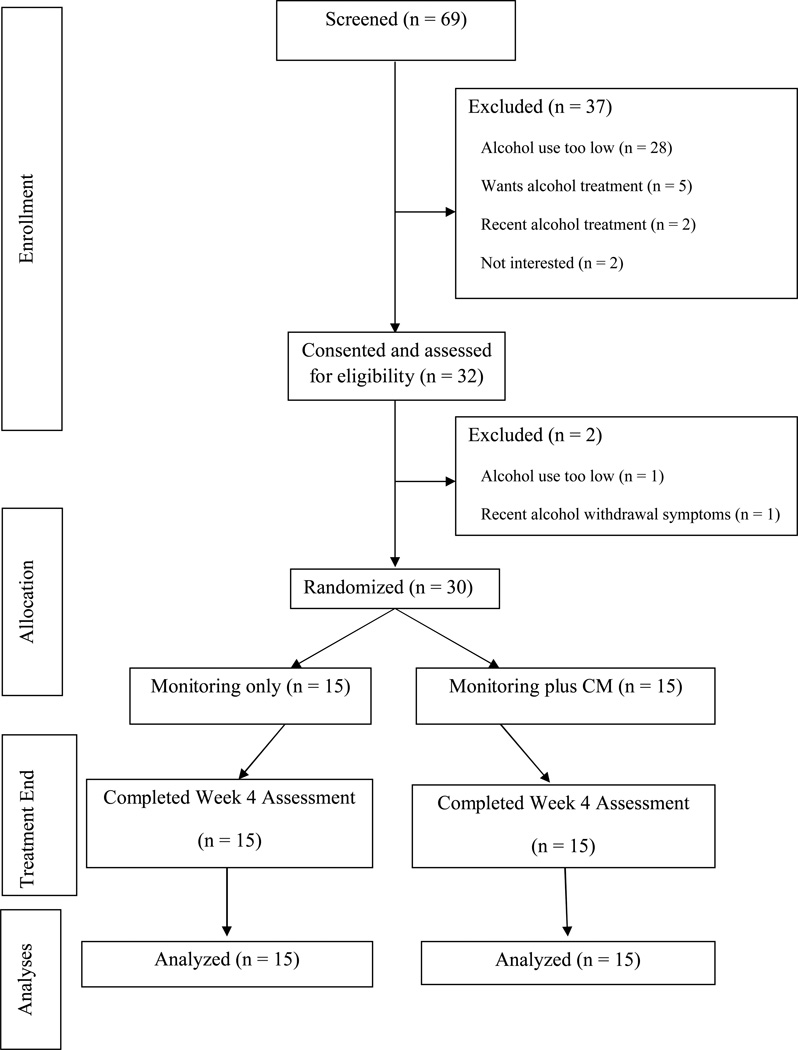
Recruitment (N = 30) occurred between February and August 2011. The sample size of 15 participants per group was estimated from CM studies with similar design features and an average effect size of d = 0.94[7]. Respondents to an ad stating, “Volunteers needed for a research study looking at alcohol use. If you are 21 or older and drink alcohol regularly, you may qualify to participate” were initially screened via telephone, and in-person interviews finalized eligibility and assessments. Inclusion criteria were (a) ≥21 years old, (b) ≥ 4 drinking days and ≥12 drinks per week on average in the past 2 months, (c) a valid photo ID, and willing to d) use cell phone and breathalyzer, and (e) sign an off-campus property transfer form. Exclusion criteria were (a) desire alcohol treatment now or received it in the past 6 months, (b) alcohol dependence with withdrawal per DSM-IV criteria, and (c) non-English speaking. Participants provided written informed consent, approved by the University’s Institutional Review Board. They were also asked to sign a separate consent (not required for participation) to allow audiotaping of assessments for oversight purposes. A Baccalaureate-level Research Assistant (RA) conducted all study procedures under supervision of investigators. See Figure 1 for participant flow.
Figure 1.
The flow of participants from the point of initial contact through data analysis is presented per Consolidating Standards of Reporting Trials (i.e., CONSORT) guidelines.
Assessments
A checklist based on modules from the Structured Clinical Interview for DSM-IV [16] defined past year alcohol use disorders at Intake. Remaining assessments occurred at Intake and Week 4. The Addiction Severity Index (ASI) [17;18;19;20] assesses severity of psychosocial functioning, with composite scores ranging from 0 to 1 (low to high problem severity). The Timeline Follow-back [21] uses calendar prompts to facilitate recall of substance use. The Drinker Inventory of Consequences (DrInC) [22] assesses alcohol problems, with higher scores indicating greater severity. Participants also completed a study satisfaction questionnaire at Week 4.
Participants received $15 in gift cards for the Intake interview, $10 for Week 4, and $65 and $25 for returning the cell phone and breathalyzer (see below), respectively.
Equipment
Equipment included a breathalyzer (BACTRACK Select S30; BACTRACK, San Francisco, CA), cell phone (Motorola Barrage; Motorola Mobility, Libertyville, IL), and accessories. This phone supports multimedia messaging, has a 2 megapixel resolution, and dates and time-stamps videos. The Verizon plan was $27 per month per phone, and included 200 minutes of talk (restricted to study numbers) and unlimited multimedia messaging.
Training
The RA demonstrated the breathalyzer and cellphone functions (voice, video recording, text/video messaging) and provided written step-by-step instructions. To record a breath alcohol concentration test (BrAC), the breathalyzer is powered on. The phone’s video record button is pressed, and the phone placed in a stand at head level (e.g., on a shelf) or held at arms-reach with the elbow stabilized. Standing 2–3 feet away, the breathalyzer pre-test reading of 0.00 g/dL is displayed to the lens, the start button pressed (audible beep), and one inhales and exhales (audible) into the breathalyzer until a beep sounds. Next, the BrAC test result is displayed to the lens and the record button pressed to end recording. Lastly, the video is reviewed to confirm that the test was captured, and then sent to the RA. The process takes about 3 minutes. Participants completed at least three high quality videos, until comfortable and efficient.
Participants were instructed to keep equipment with them between 7 a.m. and 11 p.m. For the first three days, the RA called to inquire about any problems, thanked participants for videos sent at prompted times, and helped troubleshoot if needed.
Study Conditions
Participants were randomized to (1) BrAC Monitoring only (n=15) or (2) BrAC Monitoring plus CM (n=15), using a computerized urn randomization procedure, stratifying individuals on gender.
BrAC Monitoring only. The RA texted participants one to three times daily to indicate a BrAC was due within the hour and the compensation for a valid on-time video. If a BrAC video was not received within 30 minutes, a reminder text repeated that deadline and possible compensation. Prompts occurred 8am to 11pm, but were clustered during evenings and weekends (6pm to 11pm at least 5 evenings per week, and at least twice on two evenings per week). Prompts prior to 6pm occurred 1–2 times per week. Participants were informed that there would be up to 21 BrACs per week. On average, 10 prompts per week occurred; the exact number and timing of tests was not divulged to dissuade participants from concluding that any given prompt signaled completion of the daily requirements and that drinking could commence and go undetected .
Each video was reviewed for quality and a thank you text sent communicating earnings. Compensation for adherence was $1 per valid on-time video, $10 per 7-day period of all BrACs valid and on-time, and $20 for at least 90% of all videos being valid and on-time. Average earnings for perfect adherence were about $100, consistent with previous work involving daily calls or emails [23].
BrAC Monitoring plus CM involved the same procedures above. These participants also received escalating vouchers (promissory notes redeemable for a gift card or check in the amount earned) for valid on-time n-BrACs (< .02 g/dL) [24]. Vouchers started at $2 for the first n-BrAC and increased $0.50 for each consecutive n-BrAC, up to $10 maximum. Vouchers reset to $2 when a BrAC read ≥ .02 g/dL or was submitted late, and the highest voucher level attained prior to a reset was reinstated after five consecutive n-BrACs. If all tests were valid, on-time and negative, participants could earn about $340, an amount consistent with efficacious voucher CM therapies (about $1000 over 12 weeks). Thank you texts included voucher earnings and the amount possible for the next valid on-time n-BrAC.
Participants were encouraged to request voucher earnings at any point. All but one elected to receive a lump sum payment at Week 4.
Data Analyses
Analyses were conducted on an intent-to-treat basis. Baseline data were examined for differences by condition using chi-square tests (χ2) and analysis of variance (ANOVA).
The primary aim was to assess the efficacy of CM on reducing drinking. Percent n-BrACs (< .02 g/dL) was the primary outcome. Secondary drinking outcomes were longest duration of abstinence (LDA) defined as the greatest number of consecutive days of n-BrACs and self-reported (TLFB) number of drinking days and drinks per drinking day. Outcomes were examined as a function of condition using univariate or repeated measures ANOVA or ANCOVA1. Cohen’s d indicates effect sizes for ANOVA analyses, Cramer’s V for χ2; omega-squared (ω2) indicates proportion of variance accounted for. Changes in DrInC and ASI-Alcohol composite scores from Intake to Week 4 were examined using repeated measures ANOVA or ANCOVA, with condition as the independent variable.
In regard to the validity of procedures, the association between a BrAC ≥ 2 g/dL and TLFB self-reported drinking on a day was examined using the phi coefficient (Φ). For magnitude of drinking, Kendall’s tau and Spearman’s rho described the relationship between the highest BrAC result each day and TLFB number of drinks each day.
This is the first known study to examine feasibility and acceptability of breathalyzer and cell phone technologies to monitor real-world drinking. Feasibility was assessed via descriptive data on proportion of participants who returned equipment in working order and proportion of prompts resulting in on-time BrAC videos. Frequencies of breathalyzer malfunctions, invalid videos, and late videos by treatment conditions were examined using χ2; percent of on-time BrAcs by condition was examined using univariate ANOVA. Differences between conditions on the treatment satisfaction survey were examined using χ2 tests. Analyses were conducted with SPSS version 19 for Windows.
Results
Baseline Characteristics
Table 1 depicts baseline and demographic variables. Participants in the Monitoring only condition were on average significantly older, more educated, and had lower DrInC scores than CM participants.
Table 1.
Baseline and Demographic Information by Treatment Condition
| Variables | Monitoring Only |
Monitoring Plus CM |
Statistic (df) |
|---|---|---|---|
| N | 15 | 15 | |
| Age (mean, SD) | 44.5 (14.3) | 34.2 (10.4) | F (1, 28) = 5.14* |
| Female (n) | 60.0% (9) | 66.7% (10) | χ2 (1) = 0.14 |
| Non-Hispanic Ethnicity (n) | 93.3% (14) | 86.7% (13) | χ2 (1) = 0.37 |
| Race (n) | χ2 (4) = 2.10 | ||
| African American | 6.7% (1) | 6.7% (1) | |
| Caucasian | 80.0% (12) | 60.0% (9) | |
| Native American | 0.0% (0) | 6.7% (1) | |
| Asian | 6.7% (1) | 13.3% (2) | |
| More than one race | 6.7% (1) | 13.3% (2) | |
| Marital Status (n) | χ2 (4) = 7.55 | ||
| Never Married | 26.7% (4) | 66.7% (10) | |
| Remarried | 0.0% (0) | 6.7% (1) | |
| Divorced | 20.0% (3) | 13.3% (2) | |
| Married | 46.7% (7) | 13.3% (2) | |
| Cohabitating | 6.7% (1) | 0.0% (0) | |
| Employment, Past 3 years (n) | χ2 (4) = 4.18 | ||
| Full-time | 80.0% (12) | 66.7% (10) | |
| Part-time – regular hours | 13.3% (2) | 13.3% (2) | |
| Part-time – irregular hours | 0.0% (0) | 6.7% (1) | |
| Student | 0.0% (0) | 13.3% (2) | |
| Retired or Disability | 6.7% (1) | 0.0% (0) | |
| Net Income, Past month (mean, SD) |
$2720 ($1792) | $1753 ($1384) | F (1, 28) = 2.74 |
| Education, years (mean, SD) | 16.7 (1.8) | 14.9 (2.3) | F (1, 28) = 5.88* |
| Alcohol Abuse (n) | 60.0% (9) | 60.0% (9) | χ2 (1) = 0.00 |
| Alcohol Dependence (n) | 33.3% (5) | 53.3% (8) | χ2 (1) = 1.22 |
| Substance Use, Past 30 Days | |||
| Days of Alcohol Use (mean, SD) |
24.2 (5.2) | 23.4 (4.6) | F (1, 28) = .20 |
| Drinks per Drinking Day (mean, SD) |
4.4 (3.2) | 4.2 (1.9) | F (1, 28) = 0.07 |
| Days of Cocaine Use (median, interquartile range) |
0.00 (0.0) | 0 (0.0) | U = 105.0 |
| Days of Marijuana Use (median, interquartile range) |
0.00 (0.0) | 0.00 (0) | U = 99.0 |
| ASI Alcohol score (mean, SD) | 0.32 (0.09) | 0.38 (.11) | F (1, 28) = 2.97 |
| DrInC scorea (mean, SD) | 65.0 (10.7) | 73.1 (9.0) | F (1, 28) = 5.04* |
Note. An asterisk indicates a p-value < 0.05.
Drinker Inventory of Consequences.
Drinking-related Outcomes
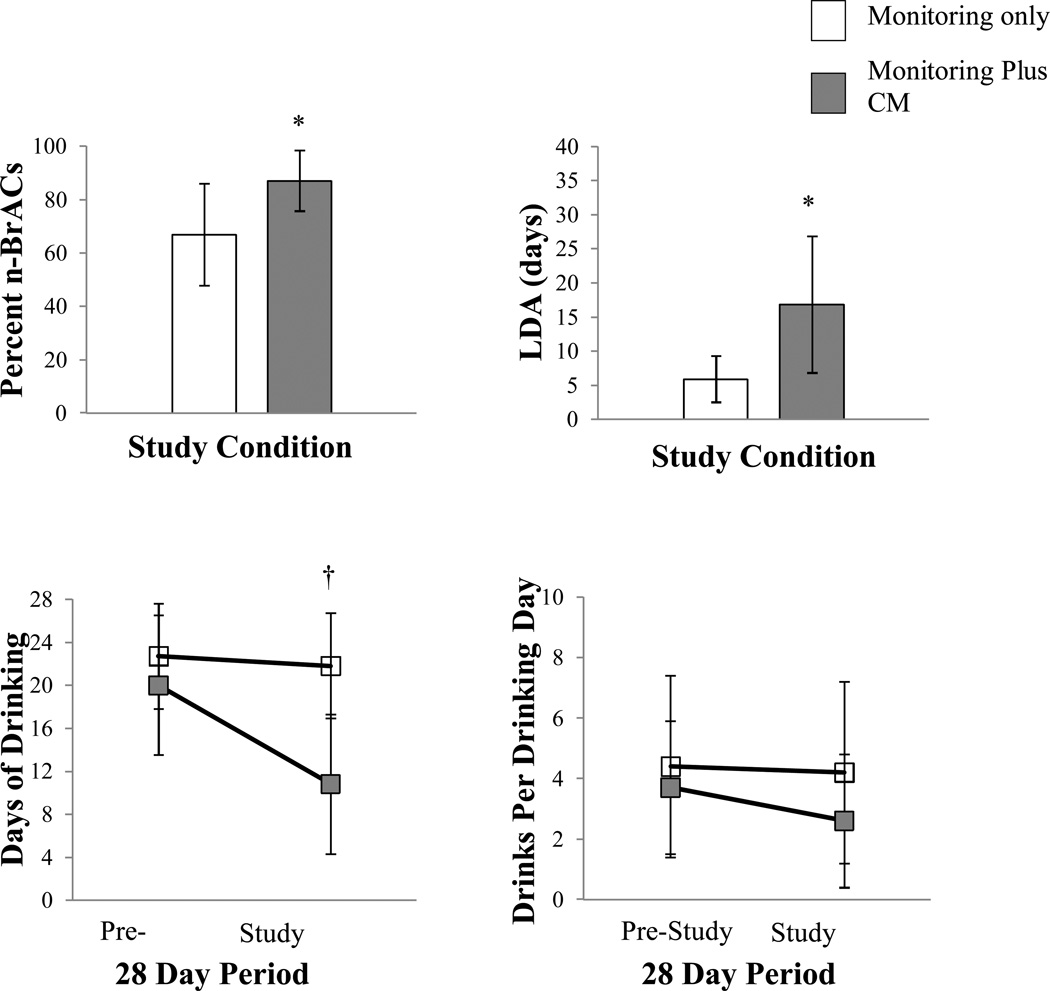
Number of BrAC prompts did not differ between conditions (CM, 629; Monitoring only, 610), F (1, 28) = 1.38, p = .25). Figure 2 depicts drinking outcomes by condition, Table 2 presents descriptive and statistical tests. CM participants submitted a higher percent n-BrACs and achieved a greater LDA than Monitoring-only participants. Self-reported days of drinking varied as a function of condition and time, with decreases over time with CM relative to Monitoring only. ASI Alcohol and DrInC scores also varied as a function of condition and time, with decreases over time with CM compared to Monitoring only.
Figure 2.
Primary drinking outcomes were the percent of breath tests negative for alcohol (< 0.02 g/sL), LDA (longest duration (in days) of abstinence, defined by negative breath test results), and change in frequency and magnitude of drinking over the 28 days immediately pre-study compared to the 28-day intervention period. Study conditions differed significantly on the percent of breath tests negative for alcohol (< 0.02 g/dL), LDA, and as a function of condition and time on frequency of drinking. Data points represent means and standard deviations. The asterisk (*) indicates a significant difference between groups, p≤ .01. † indicates a significant condition by time interaction, p < .01.
Table 2.
Drinking-related Outcomes and Treatment Satisfaction
| Variables | Monitoring Only (n=15) |
Monitoring Plus CM (n=14) |
Statistic (df) |
p- value |
Effect sizea |
|---|---|---|---|---|---|
| Drinking-related Outcomes | |||||
| % negative breath samples (mean, SD) |
66.9 (19.1) | 87.1 (11.4) | F (1, 28) = 12.4 | .00 | .62 |
| Longest duration of negative samples (days) |
5.9 (3.4) | 16.8 (10.1) | F (1, 27) = 9.59 | .00 | .52 |
| Self-reported days of drinking, pre- to during treatment (mean, SD) |
24.2 (5.2) to 21.8 (4.5) | 23.4 (4.6) to 10.8 (6.5) | F (1, 27) = 10.02b | .00 | .54 |
| Self-reported drinks per drinking day, pre- to during treatment (mean, SD) |
4.4 (3.2) to 3.7 (2.2) | 4.2 (1.9) to 2.9 (2.2) | F (1, 27) = 0.92b | .35 | .06 |
| ASI Alcohol, Intake to treatment end |
0.32 (0.09) to 0.29 (0.10) | 0.38 (0.11) to 0.20 (.09) | F (1, 27) = 9.33b | .01 | .52 |
| DrInC Overall, Intake to treatment end |
65.0 (10.7) to 63.3 (8.3) | 73.1 (9.0) to 62.5 (6.2) | F (1, 28) = 11.76b | .00 | .60 |
| Treatment Satisfaction | |||||
| Overall Satisfaction (%, n) | χ2 (1) = 0.99 | .81 | .18 | ||
| Very dissatisfied | 13.3% (2) | 7.1% (1) | |||
| Moderately dissatisfied | 6.7% (1) | 7.1% (1) | |||
| Moderately satisfied | 40.0% (6) | 28.6% (4) | |||
| Very satisfied | 40.0% (6) | 57.4% (8) | |||
| Willingness to send videos without compensation (%, n) |
χ2 (1) = 1.13 | .89 | .20 | ||
| Not at all | 13.3% (2) | 14.3% (2) | |||
| Very unwilling | 13.3% (2) | 21.4% (3) | |||
| Somewhat willing | 46.7% (7) | 28.6% (4) | |||
| Moderately willing | 20.0% (3) | 28.6% (4) | |||
| Very willing | 6.7% (1) | 7.1% (1) | |||
| Monitoring affected drinking (%, n) |
χ2 (1) = 19.56 | <.01 | .82 | ||
| Not at all | 40.0% (6) | 0.0% (0) | |||
| Very little | 40.0% (6) | 7.1% (1) | |||
| Somewhat | 20.0% (3) | 21.4% (3) | |||
| Quite a bit | 0.0 (0) | 35.7% (5) | |||
| A lot | 0.0% (0) | 35.7% (5) | |||
| Best duration of monitoring to reduce drinking (%, n) |
χ2 (1) = 3.81 | .28 |
.37 |
||
| 2 months | 53.3% (8) | 21.4% (3) | |||
| 3 months | 20.0% (3) | 42.9% (6) | |||
| 4–6 months | 13.3% (2) | 21.4% (3) | |||
| More than a year | 6.7% (1) | 14.3 (2) | |||
| Ever falsify (% yes) | 0.0% (0) | 0.0% (0) | . | . |
Note. ASI: Addiction Severity Index; DrInC: Drinker Inventory of Consequences; Asterisk indicates p < .01.
Cohen’s d for ANOVA analyses; Cramer’s V for χ2 analyses.
Statistical tests respresent condition by time interaction effects.
Validity
Frequency of drinking defined by BrACs and TLFB reports were significantly correlated, Φ = .175, p = .00. Quantity of drinking defined by the highest BrAC reading each day and TLFB number of drinks each day were significantly correlated (Kendall’s tau-b = .27, p = .00) and monotonically related (Spearman’s rho = .31, p = .00).
BrAC prompts occurred until 11pm. Drinking after 11pm was reported on one or more days by 8 (53.3%) Monitoring only and 9 (60.0%) CM participants (χ2 (1) = 0.14, p = .71). The median (IQR) number of days that drinking occurred after hours was 3.0 (8.0) and 1.0 (2.0) in the CM and Monitoring conditions, respectively (Mann-Whitney U = 82.5, p = .22), suggesting that CM participants did not simply adjust their drinking to avoid detection.
Feasibility and acceptability
Everyone (100%) returned breathalyzers and cell phones in good working order. No one requested study withdrawal, and there were no study-related adverse events. Most BrAC videos were valid and submitted on-time, with an average (± SD) of 86.0% ± 12.9% in Monitoring only and 91.2% ± 7.8% in the CM condition (F (1, 28) = 1.94, p = .18, d = 0.14). Problems included breathalyzer malfunctions (CM: 7 instances; Monitoring only: 1), invalid videos (e.g., too dark; CM: 2 instances; Monitoring only: 3), and late videos (CM: 13 instances; Monitoring only: 8), without group differences (χ2 ≥ 1.33; ps ≥ .29). When breathalyzers malfunctioned, the RA helped problem-solve and provided replacement breathalyzers if needed2.
All participants except one (administrative error) completed the Treatment Satisfaction survey (see Table 2). On perceived effect of procedures on drinking, 71% of CM participants endorsed “quite a bit” or “a lot” compared to 0% of Monitoring only participants. Differences between conditions on the remaining items were not significant. Most participants reported being at least moderately satisfied with procedures, and most endorsed 2–3 months of monitoring as the best duration of time to reduce drinking.
Compensation and Voucher Earnings
Compensation for adherence was on average (± SD) $69.2 ± $27.9 and $61.3 ± $27.8 in the CM and Monitoring only condition, respectively, F (1, 28) = 0.61, p = .44, with $2.33 ± $0.99 earned per day. CM participants earned on average $219 ± $106 in vouchers for n-BrACs, or $3.91 ± $4.77 per day. All but one CM participant elected to receive total voucher earnings in a check at the end of the study.
Discussion
This study examined the feasibility and initial efficacy of using cell phones and breathalyzers to remotely monitor alcohol consumption and reinforce abstinence in individuals’ natural environments. Adherence rates were high, and participants encountered few problems, supporting feasibility. CM was associated with increased rates and durations of alcohol abstinence and decreases in self-reported days of drinking and problem severity during the intervention.
Although cell phones are nearly ubiquitous, few participants were familiar with self-videotaping and multimedia messaging procedures. Training on equipment occurred primarily in a single 30-min session, with few problems. Adherence with the testing and submission process was 89% overall, consistent with previous research using similar compensation for daily surveys [23] and other tools with demonstrated benefits on adherence [15].
CM increased the likelihood of n-BrACs and LDA. Treatment effect sizes were “medium” to “large” in magnitude [25] and in the range found in previous CM research with single drug targets and similar reinforcement magnitudes [7,8]. Reductions in alcohol-related problems were noted with CM as well, even though participants’ problems had not risen to the level that motivated seeking treatment. Whether similar results would be observed in patients trying to quit or reduce their drinking is an important empirical question.
This study highlights several methodological considerations for future research. First, BrAC and TLFB drinking measures were significantly correlated, indicating validity of the remote monitoring procedure. However, correlations were only Φ = .175 for drinking frequency and Kendall’s tau-b = .27 for drinking magnitude. The relatively short elimination rate of alcohol and the testing schedule made capturing all instances of drinking unlikely, while the self-report data were comprehensive. Measures more sensitive to fluctuations in drinking over short intervals, like ecological momentary assessments or daily diaries indicating timing of drinking, may be more appropriate to assess validity of this procedure.
Second, although this monitoring strategy captured alcohol-positive tests, representing improved sensitivity over typical periodic in-person testing, self-reports indicated some occasions of drinking beyond the daily monitoring period. One option to improve detection may be to extend monitoring beyond 11pm, although other studies have also used this cutoff [26] and extending monitoring may impact acceptability. Another option may be to increase the frequency of breath tests. There is precedence for asking social drinkers to respond to four random prompts daily to complete Interactive Voice Response (IVR) surveys for 14 days, with 92% adherence [26], and for asking smokers trying to quit to respond to four random prompts daily to complete surveys via palmtop computers for one week, with 78% adherence [27]. Nevertheless, increasing testing frequency in this context may be impacted by its relatively greater response demands.
Third, this intervention was relatively brief. Generally, higher treatment intensity and duration improves outcomes [28;29]. With CM, longer durations do not inevitably translate into improved outcomes [7], but research on CM for alcohol problems is also limited. Longer durations of monitoring and reinforcement may be appropriate and acceptable in individuals with higher severity of alcohol problems seeking to reduce use. Anecdotally, most participants indicated that a longer monitoring duration would be best to decrease drinking.
Fourth, text message prompts, reminders, and thank-you’s were completed manually. Existing technologies such as IVR and internet could automate these procedures in whole or in part, broadening scope and reach. Automated monitoring and reinforcement of alcohol abstinence may ultimately be less costly than some other forms of treatment, and costs may decrease further as technology advances and video capture features become more commonplace, perhaps obviating the need to provide cell phones. Research suggests the cost-effectiveness of CM therapy for illicit substance use [30]. Future studies are needed to evaluate the cost-effectiveness and long-term efficacy of these specific procedures in treatment populations.
Fifth, participants were encouraged to redeem earnings at least weekly because research indicates that delayed reinforcement adversely affects outcomes [e.g., 7;31;32]. However, all but one participant elected to receive earnings in one lump sum at the end. Congratulatory messages sent to participants had earnings specified and may have served as second order reinforcers. Also possibly involved is that in the extant literature, delays to reinforcement have largely been researcher-imposed, whereas the participants herein chose their preferred delays.
Limitations include that the sample size was relatively small, possibly limiting generalizability. There were baseline differences between conditions, although these were controlled statistically to the extent possible. This was not a treatment study. Individuals with greater severity of alcohol problems may require modifications such as more dense testing schedules to realize improvements, while those desiring to reduce their drinking may be motivated and more likely to decrease drinking in response to the monitoring alone procedures. In this study, monitoring occurred for four weeks, and the acceptability of longer durations is unclear. Future research may examine adjusting the testing schedule to capture more drinking episodes and effects on feasibility and acceptability. In any case, the random prompt method used herein was acceptable and efficacious in substantially reducing drinking, at least in the short term.
Several strengths of this study are noteworthy. These results provide evidence of the feasibility of an innovative strategy to address technical limitations on monitoring and reinforcing alcohol abstinence. The portable procedures were sufficient to detect instances of drinking that would go undetected with conventional methods. CM was associated with significant reductions in alcohol use. Both objective and subjective measures were collected allowing examination of convergence and divergence in measures.
Overall, this study provides initial evidence of feasibility and efficacy of this innovative CM procedure for reducing alcohol use. Coupled with the substantial literature of improvements in substance use treatment outcomes with CM, this study suggests a remote monitoring and reinforcement procedure that has potential to extend the benefits of CM to treating alcohol problems.
Acknowledgements
This study, and preparation of this report, was funded by NIH grants P30-DA023918, R01-DA027615, R01-DA022739, R01-DA13444, P50-DA09241, P60-AA03510, R01-DA024667, R01HD075630, and R21-DA029215.
Footnotes
Declaration of interest: None.
Of the three baseline variables that differed between conditions (Table 1), none were significantly correlated with percent n-BrACs, the primary outcome. Years of education was significantly correlated with LDA (r = −0.44, p = .02) and ASI Alcohol (r = .40, p = .03), and age was significantly correlated with TLFB drinking frequency (r = .56, p = .00) and magnitude(r = −.42, p = .02). Analyses were conducted first including only the baseline variable significantly correlated with the outcome as a covariate, if any. Analyses were repeated using the two remaining non-significantly correlated baseline variables as covariates, and conclusions were the same. Analyses presented include only the baseline variable that correlated with the outcome measure as a covariate (years of education in the LDA and ASI Alcohol analyses, age in the TLFB-based frequency and magnitude of drinking analyses)
The principle issue related to breathalyzer maintenance that arose during the study was the tendency for the plastic mouthpieces to break. Research staff hand delivered replacement pieces to participants the same day when needed to avoid disrupting breath test procedures. Future efforts should consider supplying extra mouthpieces to participants upfront to avoid these costs in staff time and effort.
References
- 1.Mokdad A, Marks J, Stroup D, Gerberding J. Actual causes of death in the United States 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set (TEDS): 1998–2008. Rockville, MD: State Admissions to Substance Abuse Treatment Services; DASIS Series: S-55; 2010 HHS Publication No. (SMA) 10-4613. [Google Scholar]
- 4.Treatment Episode Data Set (TEDS) SAMHSA Center for Behavioral Health Statistics and Quality. Rockville MD 2011: Drug and Alcohol Services Information System Series: S-55; 2008. Discharges from Substance Abuse TreatmentServices. DHHS Publication No.(SMA) 11-4628. [Google Scholar]
- 5.Polich JM, Armor DJ, Braiker HB. The course alcoholism: of years Four treatment after treatment. New York: John Wiley & Sons; 1981. Stability and change in drinking patterns; pp. 159–200. [Google Scholar]
- 6.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto W. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- 7.Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101(2):192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- 8.Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101(11):1546–4560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- 9.Higgins ST, Alessi SM, Dantona RL. Voucher-based contingency management interventions: A substance abuse treatment innovation. Addict Behav. 2002;27(6):887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- 10.Stitzer M, Petry N. Contingency management for treatment of substance abuse. Annu Rev Clin Psychol. 2006;2:411–434. doi: 10.1146/annurev.clinpsy.2.022305.095219. [DOI] [PubMed] [Google Scholar]
- 11.Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes and they will come: Contingency management for the treatment of alcohol dependence. J Consult Clin Psychol. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- 12.Helmus TC, Saules KK, Schoener EP, Roll JM. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: a feasibility study. Psychol Addict Behav. 2003;17(3):249–251. doi: 10.1037/0893-164X.17.3.249. [DOI] [PubMed] [Google Scholar]
- 13.Dallery J, Glenn IM. Effects of an internet-based voucher reinforcement program for smoking abstinence: a feasibility study. J Appl Behav Anal. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dallery J, Glenn IM, Raiff BR. An internet-based abstinence reinforcement treatment for cigarette smoking. Drug Alcohol Depend. 2007;86(2–3):230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Brendryen H, Kraft P. Happy Ending: a randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction. 2008;103:478–484. doi: 10.1111/j.1360-0443.2007.02119.x. [DOI] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- 17.McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, O’Brien CP. New data from the Addiction Severity Index: Reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Bovasso GB, Alterman AI, Cacciola JS, Cook TG. Predictive validity of the Addiction Severity Index's composite scores in the assessment of 2-year outcomes in a methadone maintenance population. Psychol Addict Behav. 2001;15:171–176. [PubMed] [Google Scholar]
- 19.Kosten TR, Rounsaville BJ, Kleber HD. Concurrent validity of the Addiction Severity Index. J Nerv Ment Dis. 1983;17:606–610. doi: 10.1097/00005053-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Leonard C, Mulvey K, Gastfriend DR, Shwartz M. The Addiction Severity Index: A field study of internal consistency and validity. J Subst Abuse Treat. 2000;18:129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 21.Sobell MB, Maisto SA, Sobell LC. Developing a prototype for evaluating alcohol treatment effectivenes. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances. New York: Pergamon Press; 1980. [Google Scholar]
- 22.Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Rockville, MD: NIAAA; 1995. The Drinker Inventory of Consequences (DrInC). An Instrument for Assessing Adverse Consequences of Alcohol Abuse. [Google Scholar]
- 23.Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: results from an event-based daily diary. AIDS Behav. 2008;12:104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petry NM. Contingency management for substance abuse treatment: A guide to implementing evidence-based practice. New York, NY: US Routledge/Taylor & Francis Group; 2012. [Google Scholar]
- 25.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1988. [Google Scholar]
- 26.Collins RL, Kashdan TB, Gollnisch G. The feasibility of using cellular phones to collect ecological momentary assessment data: Application to alcohol consumption. Exp Clin Psychopharmacol. 2006;11(1):73–78. doi: 10.1037//1064-1297.11.1.73. [DOI] [PubMed] [Google Scholar]
- 27.Wetter DW, McClure JB, Cofta-Woerpel L, Costello TJ, Reitzerl LR, Businelle MS, et al. A randomized clinical trial of a palmtop computer-delivered treatment for smoking relapse prevention among women. Psychol Addict Behav. 2011;25(2):365–371. doi: 10.1037/a0022797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moos RH, Moos BS. Long-term influence of duration and intensity of treatment on previously untreated individuals with alcohol use disorders. Addiction. 2003;98(3):325–338. doi: 10.1046/j.1360-0443.2003.00327.x. [DOI] [PubMed] [Google Scholar]
- 29.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcomes Study (DATOS) Psych Addict Behav. 1997;11(4):294–307. [Google Scholar]
- 30.Olmstead TA, Petry NM. The cost-effectiveness of prize-based and voucher-based contingency management in a population of cocaine- or opioid-dependent outpatients. Drug Alcohol Depend. 2009;102(1–3):108–115. doi: 10.1016/j.drugalcdep.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Packer RR, Howell DN, McPherson S, Roll JM. Investigating reinforcer magnitude and reinforcer delay: A contingency management analog study. Exp Clin Psychopharmacol. 2012 doi: 10.1037/a0027802. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 32.Roll JM, Reilly MP, Johanson CE. The influence of exchange delays on cigarette versus money choice: a laboratory analog of voucher-based reinforcement therapy. Exp Clin Psychopharmacol. 2000;8(3):366–370. doi: 10.1037//1064-1297.8.3.366. [DOI] [PubMed] [Google Scholar]