Abstract
Background
Reasons underlying dialysis decision-making in Octogenarians and Nonagenarians have not been further explored in prospective studies.
Methods
This regional, multicentre, non-interventional and prospective study was aimed to describe characteristics and quality of life (QoL) of elderly (≥80 years of age) with advanced chronic kidney disease (stage 3b-5 CKD) newly referred to nephrologists. Predictive factors of death and dialysis initiation were also assessed using competing-risk analyses.
Results
All 155 included patients had an estimated glomerular filtration rate (eGFR) below 45 ml/min/1.73 m2. Most patients had a non anaemic haemoglobin level (Hb) with no iron deficiency, and normal calcium and phosphate levels. They were well-fed and had a normal cognitive function and a good QoL. The 3-year probabilities of death and dialysis initiation reached 27% and 11%, respectively. The leading causes of death were cardiovascular (32%), cachexia (18%), cancer (9%), infection (3%), trauma (3%), dementia (3%), and unknown (32%). The reasons for dialysis initiation were based on uncontrolled biological abnormalities, such as hyperkalemia or acidosis (71%), uncontrolled digestive disorders (35%), uncontrolled pulmonary or peripheral oedema (29%), and uncontrolled malnutrition (12%). No patients with acute congestive heart failure or cancer initiated dialysis. Predictors of death found in both multivariate regression models (Cox and Fine & Gray) included acute congestive heart failure, age, any walking impairment and Hb <10 g/dL. Regarding dialysis initiation, eGFR <23 mL/min/1.73 m2 was the only predictor found in the Cox multivariate regression model whereas eGFR <23 mL/min/1.73 m2 and diastolic blood pressure were both independently associated with dialysis initiation in the Fine & Gray analysis. Such findings suggested that death and dialysis were independent events.
Conclusions
Octogenarians and Nonagenarians newly referred to nephrologists by general practitioners were highly selected patients, without any symptoms of the common geriatric syndrome. In this population, nephrologists’ dialysis decision was based exclusively on uremic criteria.
Keywords: Chronic kidney disease, Renal replacement therapy, Conservative management, Elderly, Competing-risk analysis
Background
Nephrologists are increasingly confronted with an elderly population of patients who have a large number of co-morbid conditions requiring ongoing care [1]. Indeed elderly patients with chronic kidney disease (CKD) experience a high rate of complications, such as atherosclerotic cardiovascular disease, congestive heart failure, diabetes mellitus, cognitive and functional impairment, and CKD-related complications including anaemia [1-5]. CKD is present at a high rate in the population of elderly aged 70 and over, affecting about one person out of three in France, but only a few of them present clinically relevant markers requiring appropriate care [6]. CKD at a moderate and more severe stage defined by an estimated glomerular filtration rate (eGFR) level <60 mL/min/1.73 m2 affects about 38% of subjects over 70 years in the United States [7]. Additionally, overall incidence of end-stage renal disease (ESRD) is still increasing in French elderly aged 85 years or older, and especially in diabetics [6].
Old age is no longer seen as an absolute contraindication of dialysis in most industrialized countries [6,8-11]. In France, about 3 individuals out of 1000 elderly over 75 years benefit from a renal replacement therapy, dialysis or renal transplantation, with a significant increase of dialysis prevalence [6]. However, deciding whether or not dialysis can offer a substantial prolongation of life expectancy with an acceptable quality of life (QoL) among pre-ESRD (end-stage renal disease) Octogenarians is still a difficult task for nephrologists [5,8-11]. Advanced dementia and severe neurological sequels of stroke were shown as the conditions underlying the nephrologists’ decision-making not to provide dialysis in elderly patients [12].
Recent studies suggested that dialysis provided a survival advantage compared to conservative management for most of stages 4-5 CKD patients over the age of 75 [13-15]. However, this advantage was lost for patients with multiple co-morbidities and ischemic heart disease [13-15]. Particularly, Demoulin et al. raised the question of the proportion of patients with stage 4 CKD unnecessarily prepared for dialysis in a cohort of 386 patients including some octogenarians [15].
In a context of a lack of prospective studies exploring dialysis decision-making in Octogenarians and Nonagenarians, we implemented the OPAIR (étude Observationnelle des Patients Agés Insuffisants Rénaux) study in 2007. This trial was aimed to: 1) describe the characteristics of French very elderly pre-ESRD patients newly referred to nephrologists, and their QoL; 2) evaluate death, dialysis initiation, and their predictive factors. Additionally, these two clinical outcomes were incorporated into competing-risk analyses used, to the best of our knowledge, for the first time in elderly [16].
Methods
This was a regional, multicentre, non-interventional and prospective study conducted in a cohort of very elderly pre-ESRD patients not on dialysis recruited by 20 nephrology centres in France.
Study population
Patients were included between April 2007 and April 2008 if they were: incident patients newly referred to nephrologists or prevalent patients with a nephrology follow-up less than nine months (started after July 1st, 2006), ≥80 years of age, not on dialysis, and with serum creatinine >170 μmol/L for men and >150 μmol/L for women to guarantee the inclusion of CKD patients with a high risk of disease progression. Nephrologists provided prognosis information to patients and/or families when discussing inclusion or exclusion for dialysis during several consultations. The acceptance of dialysis if necessary was not therefore an inclusion criterion.
Patients with a planned dialysis in the next three months were excluded from the study.
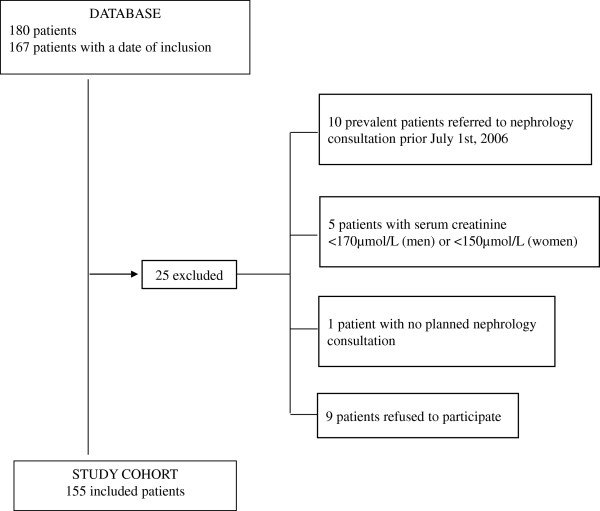
Among the 180 eligible patients registered in the database, 25 subjects were excluded for a final study population of 155 subjects, as outlined in Figure 1.
Figure 1.
The OPAIR study flow chart.
Outcomes
After inclusion, the study follow-up was designed for 2 years. However, frequency of nephrology consultations was freely determined by the nephrologists. Finally, all the patients were tracked until the occurrence of death, dialysis initiation, lost of follow-up, or the end of the study (December 31st, 2010), whichever came first.
Data collection
For each inclusion of a new patient, a standardized form was prospectively completed. At the time of study entry, extensive clinical data were collected, including demographics, lifestyle, physical examination, medical history, co-morbid conditions, and biochemical data. Cognitive status was screened using the Mini Mental State Examination (MMSE). This 30-point questionnaire was administered by trained staff to ensure reliability of data collection [17]. A mean MMSE score greater than or equal to 24 points (out of 30) illustrated a normal cognitive function for patients. Health-related QoL was assessed using the validated Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) across eight dimensions (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role emotional, mental health) using 36 items [18]. The SF36-questionnaire was fully explained to each patient, and then the forms were filled out by patients themselves. Two summary scores were obtained: physical health score by aggregating physical functioning, role-physical, bodily pain and general health, and the mental health score by aggregating vitality, social functioning, role emotional, and mental health. The SF-36 produced a score on a 0–100 scale for each dimension and each summary measure, a low score indicating a poor health status.
During the study, occurrence of death and dialysis initiation was reported. As the study was non interventional, the participating nephrologists were free to plan follow-up care visits according to their usual practice.
Data about prior decision to offer dialysis or conservative care were not collected at the start of the study.
Ethics statement
No French ethics committee oversight was required as the design of the study was strictly observational [19].
Each patient was informed about the aim and the course of the study in agreement with French regulations concerning observational studies [19]. After reading the patient information sheet, physicians obtained a verbal consent from each patient. All patients had capacity to consent or not. A written consent was not required for this kind of study based on the strict respect of usual medical practice and physician-patient relationship.
Anonymity was guaranteed. Data processing was under the modified law of January 6th, 1978 relating to the protection of data subjects regarding the processing of personal data.
Statistical analysis
We estimated that a sample size of 200 patients would be sufficient to detect 25% of patients on dialysis at the end of the 24-month follow-up period with a precision of 6% and a 95% confidence interval (CI).
Baseline characteristics were described as means and standard deviations (SD) for continuous variables, and frequencies and proportions for categorical variables.
In survival analysis, the two outcomes of interest were death and dialysis initiation. They were considered as competing risks, whereas other events were censored. A competing risk is an event which either hinders observation of the event of interest, or modifies its probability of occurrence [20,21]. When competing risks are present, analysis of time-to-event data requires the adoption of specific methods, which may in turn influence the results and their interpretation [16,20,22].
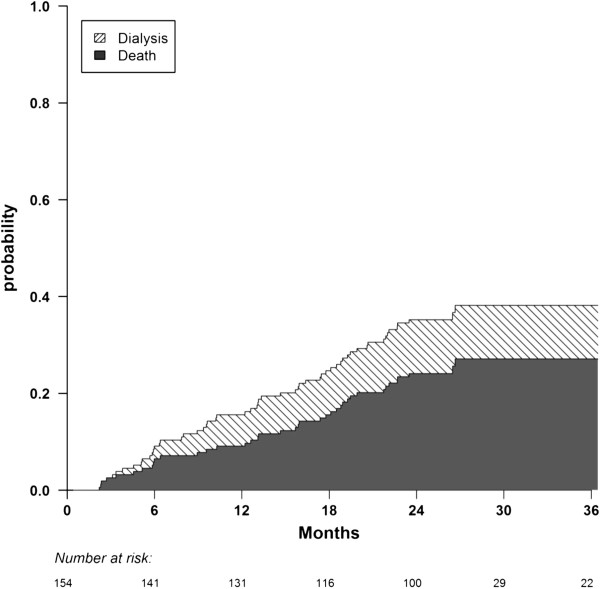
The crude cumulative incidence functions were estimated for death and dialysis initiation using the method of Kalbfleisch and Prentice [21,23]. As recommended, the duration shown on the cumulative incidence curves was extended to 3 years because only 10% of the patients were still under follow-up at this time [24].
Bivariate analyses were performed using the Cox proportional hazard regression model on the cause-specific hazard of death and dialysis initiation, and the Fine and Gray regression model on the sub-distribution hazard of death and dialysis initiation [22,25].
We used four multivariate survival regression models on the whole cohort: i) a Cox proportional hazard regression model on the cause-specific hazard of death, ii) a Cox proportional hazard regression model on the cause-specific hazard of dialysis initiation, iii) a Fine & Gray regression model on the sub-distribution hazard of death, iv) a Fine & Gray regression model on the sub-distribution hazard of dialysis initiation [22]. The Fine & Gray model provides complementary competing-risk data to the Cox proportional hazards model by considering the sub-distribution hazard [16].
The STROBE guidelines recommend that cohort studies report on the amount of missing data and the method used to handle missing data [26]. For covariates with missing values, we obtained values by multiple imputations using the MICE package as recommended for the Cox proportional hazard model analysis [27]. This was achieved through regression switching imputation using linear or logistic regression models depending on the nature of the incomplete covariate fitted [27,28]. This procedure was repeated five times to obtain five draws for each missing value in five distinct datasets.
Covariates were selected in the multivariate analysis using a stepwise procedure adapted to multiple imputation methodology [29]. It was not possible to include the covariates “Acute Congestive Heart Failure” and “Cancer” in bivariate and multivariate regression analyses on the cause-specific hazard and sub-distribution hazard of dialysis initiation, because no dialysis events occurred for patients with such characteristics (no convergence of models). Rubin’s approach was adopted, whereby the coefficients and variances obtained with the final model on each imputed dataset were averaged by taking into account the intra-variance of the model and the inter-variance between the imputed datasets [30].
Additionally, the Cox model implicitly assumes a log-linear model for the continuous variables, i.e. the risk ratio for the ages of 20 to 30 years is the same as that for the ages of 70 to 80 years. The log-linear assumption was assessed using the Martingale residuals [31]. Since the log-linearity assumption was violated for haemoglobin and eGFR, they were transformed into categorical variables. The cut-off values were identified as follows: i) with graphic investigations using Martingale residual plots; ii) with maximization of the Gray test; and iii) on the basis of medical expertise and consensus.
All statistical management was performed using the R statistical programming language and computing environment with survival, cmprsk, and MICE packages [32].
Results
After inclusion visit (visit 1: n=155), most of the patients received further nephrology consultations (visit 2: n=137, visit 3: n=125, visit 4: n=107, visit 5: n=88, visit 6: n=62, visit 7: n=43, visit 8: n=30, visit 9: n=18, visit 10: n=13, visit 11: n=6, visit 12: n=1, visit 13: n=1, visit 14: n=1). The mean duration of the follow-up was 24.7 months (inter-quartile range: 17.9, 26.9).
Patient characteristics
Baseline characteristics of the cohort are shown in Table 1. Patients were octogenarians and nonagenarians with a median age of 84 years at study entry. Most of them lived at home, in couple, and walk independently (Table 1). Among patients with handicap (n=43), 40% of them had hearing loss, 16% severe visual impairment, 14% dementia, 7% hemiplegia, and 37% other disorders.
Table 1.
Demographic and baseline characteristics
| Characteristics | N=155 |
Missing data n (%) |
||
|---|---|---|---|---|
|
Demography |
Age, years |
|
85±3.8 |
0 (0.0%) |
| |
Sex ratio |
|
1:1 |
0 (0.0%) |
| |
Social data, n (%) |
|
|
36 (23.4%) |
| |
|
Live at home |
133 (90.5%) |
|
| |
|
Live in couple |
63 (51.6%) |
|
|
Smoking status, n (%) |
|
|
|
19 (12.3%) |
| |
No smoking |
|
94 (69.1%) |
|
| |
Former or current smoking |
|
42 (30.9%) |
|
|
Clinical |
BMI, kg/m2 |
|
26.1±5.2 |
21 (13.6%) |
| |
SBP, mm Hg |
|
142.9±20.5 |
0 (0.0%) |
| |
DBP, mm Hg |
|
73.5±10.6 |
0 (0.0%) |
| |
Walking |
|
|
10 (6.5%) |
| |
|
Total disability |
4 (2.8%) |
|
| |
|
Need assistance |
44 (30.3%) |
|
| |
|
Walk independently |
97 (66.9%) |
|
|
Handicap, n (%) |
|
|
43 (30.3%) |
13 (8.4%) |
|
Peripheral oedema, n (%) |
|
|
58 (38.2%) |
3 (1.9%) |
|
Aetiology of renal disease, n (%) |
|
|
|
1 (0.6%) |
| |
Vascular nephropathy* |
|
53 (34.4%) |
|
| |
Diabetic nephropathy |
|
11 (7.2%) |
|
| |
Tubulointerstitial nephritis |
|
11 (7.2%) |
|
| |
Glomerulonephritis |
|
3 (1.9%) |
|
| |
Undefined aetiology |
|
59 (38.3%) |
|
| |
Other |
|
17 (11.0%) |
|
|
Stages CKD**, n (%) |
|
|
|
0 (0.0%) |
| |
Stage 3b CKD |
|
35 (22.3%) |
|
| |
Stage 4 CKD |
|
105 (67.8%) |
|
| |
Stage 5 CKD |
|
15 (9.9%) |
|
|
Cognitive function, MMSE score |
|
|
26.0±4.2 |
34 (22.1%) |
|
Quality of life, SF-36 score |
|
|
|
49 (31.8%) |
| |
Physical health summary score |
|
35.5±8.9 |
|
| |
Mental health summary score |
|
45.2±10.5 |
|
|
Laboratory tests |
Serum creatinine, mg/dL |
|
2.5±0.8 |
0 (0.0%) |
| |
eGFR, ml/min/1.73m2 |
|
24.3±6.7 |
0 (0.0%) |
| |
Blood urea, mmol/L |
|
14.3±10.0 |
31 (20.1%) |
| |
Albumin, g/dL |
|
3.9±0.5 |
79 (51.3%) |
| |
CRP, mg/dL |
|
0.9±1.0 |
70 (45.5%) |
| |
Proteinuria, g/24 hours |
|
0.98±1.79 |
83 (53.9%) |
| |
Cholesterol, mmol/L |
|
5.0±1.1 |
74 (48.1%) |
| |
HDL, mmol/L |
|
1.7±2.0 |
93 (60.4%) |
| |
LDL, mmol/L |
|
3.2±3.2 |
93 (60.4%) |
| |
Triglycerides, mmol/L |
|
1.5±0.8 |
74 (48.1%) |
| |
Calcium, mmol/L |
|
2.3±0.2 |
27 (17.5%) |
| |
Phosphate, mg/dL |
|
3.8±0.9 |
36 (23.4%) |
| |
Haemoglobin, g/dL |
|
11.7±1.7 |
15 (9.7%) |
| |
Haematocrit, % |
|
35.6±5.2 |
23 (14.9%) |
| |
Ferritin, ng/mL |
|
226.3±325.0 |
90 (58.4%) |
| TSAT, % | 23.5±9.2 | 118 (77.6%) |
Data expressed as mean ± standard deviation or n (%) when appropriate.
* including HTA; ** according to Modified diet in renal disease (MDRD’s formula).
BMI=body mass index, SBP=systolic blood pressure, DBP=diastolic blood pressure, CKD=chronic kidney disease, MMSE=mini mental state examination, SF-36=medical outcomes study 36-item short-form health survey, eGFR=estimated glomerular filtration rate, CRP=C-reactive protein, HDL=high density lipoprotein, LDL=low density lipoprotein, TSAT=transferrin saturation.
Unknown causes and vascular nephropathies were the most frequent aetiologies of renal disease (Table 1). CKD was severe as outlined in Table 1. All patients had an eGFR below 45 ml/min/1.73 m2 [according to the Modified Diet in Renal Disease (MDRD)’s formula]. Few patients had undergone renal biopsies (2%) or nephrectomy (6.5%).
All laboratory results are presented in Table 1. Most patients had a non anaemic haemoglobin level (Hb ≥11 g/dL: 66%) with no iron deficiency [ferritin level ≥100 ng/mL: 59%; transferrin saturation (TSAT) ≥20%: 63%]. Regarding inflammatory status of patients, 70% of patients had a C-reactive protein (CRP) level <10 μg/dL.
Most of patients were non smokers (Table 1) and only 16% of patients had a history of obesity. Regarding lipid disorders, 58% of patients had none, 33% hypercholesterolemia and 9% hypertriglyceridemia. The majority of patients were non diabetic (67%) as outlined in Table 2.
Table 2.
Summary of co-morbidities (N=155)
| Co-morbidities, n (%) | N=155 |
|---|---|
| Diabetes |
51 (33.4%) |
| Arrhythmia |
58 (37.7%) |
| Coronary artery disease |
33 (21.6%) |
| Congestive heart failure* |
22 (14.3%) |
| Valvular heart disease |
18 (11.7%) |
| Peripheral vascular disease |
27 (17.6%) |
| Stroke |
16 (10.3%) |
| Neoplasia (<5 years) |
21 (13.7%) |
| Respiratory insufficiency |
18 (11.7%) |
| Continuous oxygen therapy |
1 (0.6%) |
| Cirrhosis | 2 (1.3%) |
* including 19 episodes of acute congestive heart failure.
Regarding cognitive performance, 81% of men and 71% of women had a normal cognition as their mean MMSE score was greater than or equal to 24. According to the age of patients, 77% of patients aged <90 years and 67% of patients ≥90 years had a normal cognitive function (MMSE score ≥24).
Data concerning QoL at inclusion using SF-36 questionnaire are presented as median scores in Figure 2. Their physical and mental health summary scores are presented in Table 1.
Figure 2.
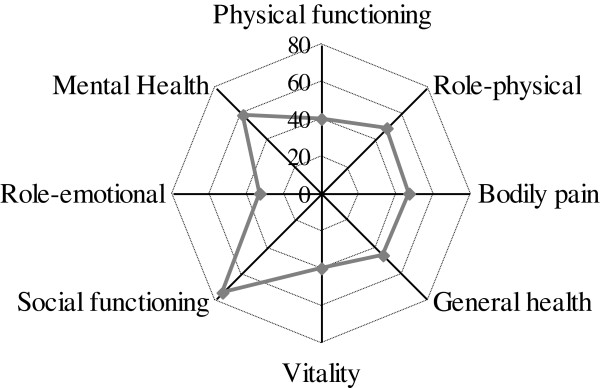
Quality of life at inclusion (using SF-36 questionnaire). Medians are represented.
Outcomes
A total of 83 patients were prematurely withdrawn for the following reasons: 18 patients with no further planned nephrology consultation, 17 patients initiated dialysis, 41 patients died and 7 patients were lost to follow-up. Finally, 72 patients were still alive at the end of the study.
The 3-year probabilities of death and dialysis initiation reached 27% and 11% respectively, as shown in Figure 3. The leading causes of death were cardiovascular (32%), cachexia (18%), cancer (9%), infection (3%), trauma (3%), dementia (3%), and unknown (32%).
Figure 3.
Cumulative incidence of death and dialysis initiation during follow-up. Cumulative incidences are stacked.
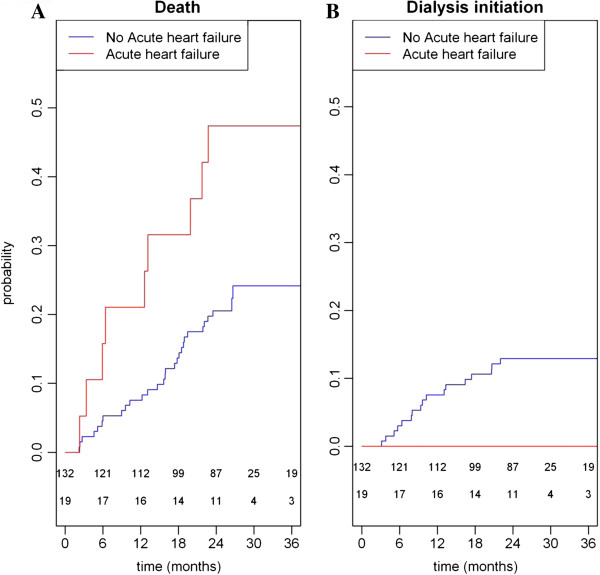
No dialysis initiation was observed among 19 patients with acute congestive heart failure at inclusion, and 21 patients with a history of cancer within the last 5 years before inclusion. Thus a total of 40 patients (26%) were withdrawn from dialysis only because of these antecedents.
Regarding the 17 patients who initiated dialysis, they underwent in majority hemodialysis (n=12, 71%) or peritoneal dialysis (n=5, 29%). Among hemodialysis patients, 7 patients started treatment with an arteriovenous fistula and 5 patients with a venous catheter. The reasons for dialysis initiation were based on uncontrolled biological abnormalities, such as hyperkalemia or acidosis (n=12, 71%), uncontrolled digestive disorders (n=6, 35%), uncontrolled pulmonary oedema or peripheral (n=5, 29%), and malnutrition (n=2, 12%). The delay before initiation of dialysis was 12±6 months. The mean age of these patients was 84.9±2.9 years when dialysis therapy was started; overall values ranged from 80.5 to 89.3 years. The median eGFR was 10.3 (interquartile range: 7.8-14.4) mL/min/1.73 m2; overall values ranged from 6.0 to 19.4 mL/min/1.73 m2. Among them, 7 patients died before the end of the study. For these dialysis patients, one-year and two-year survival rates were 64.7% and 58.8%, respectively. Additionally, 3 patients underwent fistula creation without receiving dialysis.
Competing-risk analysis of death and dialysis initiation
Variables associated with death using Cox bivariate regression analysis were: handicap, acute congestive heart failure, peripheral oedema, age, MMSE score, walking impairment, and haemoglobin level (Hb) <10 g/dL (data not shown). In the Cox multivariate regression analysis, acute congestive heart failure, age, walking impairment and Hb<10 g/dL were independently associated with death as shown in Table 3. All predictors of death in the Fine & Gray model were those found in the Cox model (Table 3). No other variables as those identified in the Cox model were significant in the Fine & Gray analysis.
Table 3.
Competing-risk models of variables associated with death and dialysis initiation (multivariate regression Cox and Fine & Gray models)
|
Outcomes |
Predictive variables |
Cox analysis |
Fine & Gray analysis |
||
|---|---|---|---|---|---|
| RR | CI | RR | CI | ||
|
Death |
Acute congestive heart failure |
2.62 |
[1.17 - 5.89] |
2.86 |
[1.31 - 6.26] |
| |
Age (years) |
1.09 |
[1.01 - 1.18] |
1.09 |
[1.01 - 1.18] |
| |
Walking impairment |
2.11 |
[1.00 - 4.43] |
2.17 |
[1.05 - 4.49] |
| |
Hb <10 g/dL |
3.73 |
[1.74 - 7.99] |
3.85 |
[1.77 - 8.39] |
|
Dialysis initiation |
DBP (per cm Hg) |
1.03 |
[0.99 - 1.07] |
1.03 |
[1.01 - 1.06] |
| |
eGFR <23 mL/min/1.73m2 |
12.95 |
[2.93 - 57.18] |
13.37 |
[3.04 - 58.69] |
| Hb <10 g/dL | 0.49 | [0.06 – 3.75] | 0.32 | [0.04 – 2.57] | |
RR=risk ratio, CI=confidence interval, Hb=haemoglobin, DBP=diastolic blood pressure, eGFR=estimated glomerular filtration rate.
Variables associated with dialysis initiation using Cox bivariate regression analysis were: serum creatinine level, eGFR <23 mL/min/1.73 m2, systolic and diastolic blood pressure (DBP, data not shown). In the Cox multivariate regression analysis, eGFR <23 mL/min/1.73 m2 was the only variable independently associated with dialysis initiation as shown in Table 3. However, in the Fine & Gray analysis, eGFR <23 mL/min/1.73 m2 and DBP were both independently associated with dialysis initiation as shown in Table 3.
Patients with acute congestive heart failure were 2.62-fold more likely to die than others (Figure 4 - panel A). In the other hand, they were not offered dialysis treatment (Figure 4 - panel B). Consequently, acute congestive heart failure was a comorbid condition both predictor of death and dialysis initiation. Moreover, no other predictor of death was found as predictor of dialysis initiation in both models (Cox and Fine &Gray) (Table 3), suggesting that the 2 clinical outcomes were independent for patients without acute congestive heart failure.
Figure 4.
Cumulative incidences of death (panel A) and dialysis initiation (panel B) for patients with acute heart failure (red) and other patients (blue).
Discussion
The major strength of the OPAIR study is its prospective and observational design with measurements of QoL and cognitive function. We focused on CKD management in Octogenarians and Nonagenarians before dialysis decision-making in addition to previous studies devoted to elderly including patients starting dialysis [9,10], and those conducted in general population [4,33,34]. We provided useful information on a very elderly pre-ESRD French population newly referred to nephrologists, and dialysis decision-making in usual clinical practice in this population. Death and dialysis initiation were found to be independent clinical outcomes, except for acute congestive heart failure patients. Finally, we highlighted that the patient’s age had no impact on dialysis decision as nephrologists seem to use similar acceptance criteria for dialysis in very elderly as those in younger subjects.
The OPAIR study prospectively profiled the clinical characteristics of very elderly French patients with an advanced CKD newly referred to nephrologists. Regarding kidney disease, most of them had a severely impaired renal function, and should potentially progress to ESRD requiring a renal therapy replacement or die. Nephrologists considered going into aetiology of renal disease in patients (2% biopsies) of no importance, suggesting a probabilistic aetiology. However, CKD-related complications were meticulously controlled; most of them had a haemoglobin level over 11 g/dL, and normal calcium and phosphate levels. Among OPAIR participants, the 3-year probabilities of death and dialysis initiation amounted to 27% and 11%, respectively. Such findings suggest that participants were 2.5-fold more likely to die than to progress to ESRD requiring dialysis. Our results were relatively consistent with those found in previous studies with disparate settings showing death, largely cardiovascular, as the most common outcome in CKD patients rather than progression to advanced stages of CKD, even among patients with stage 4 CKD, and especially true in elderly [4,8-10,13,15,33,35].
This specific geriatric population was relatively healthy. Included patients had moderate co-morbidities, a preserved cognitive function and no deterioration of QoL. Their physical and mental health summary scores illustrated indeed a good health status despite their age and were close to those of younger elderly (≥75 years) in general population [36]. They were also well-fed. With regard to management of very elderly (≥80 years) with renal disease, there was therefore an indication bias in the selection process on behalf of GPs towards referring patients for nephrology consultation in the OPAIR study. GPs, consciously or unconsciously, had restricted access to patients who could potentially require a dialysis, based on renal criteria and good health. Indeed most patients referred to nephrologists were neither elderly institution residents, nor malnourished frail elderly with geriatric syndrome. Such results outlined that the clinical profile of these very elderly pre-ESRD patients did not fit to the profile of geriatric patients.
Congestive heart failure or a history of cancer had a significant impact on access to dialysis. No included patients with acute congestive heart failure underwent dialysis. This condition, by contrast, was found as a strong predictor of death. Additionally, no patients with a history of cancer underwent dialysis, whereas no increased risk of death from cancer was found. Thus 26% of patients with one of these two antecedents, easily recognized by clinicians, were not offered dialysis. The observational nature of data cannot explain the process that has led to a lack of dialysis for these patients. Several hypotheses can be advanced. First, patients with congestive heart failure had a higher risk of death, and therefore died maybe before requiring dialysis. Second, nephrologists decided not to offer dialysis for fear of worsening the quality of life without improving survival in such patients. Indeed a recent study has suggested that there is no benefit in terms of survival for patients with cardiovascular co-morbidities [13]. Third, patients with heart failure or a history of cancer were more able to decline to undergo dialysis. As none of these patients underwent dialysis, it is likely that these three hypotheses were combined. Such a result suggests that nephrologists have introduced a dialysis indication bias in patients with congestive heart failure or a history of cancer.
Finally, competing risk-analyses in the OPAIR study focused on a geriatric population newly referred to nephrologists with a good health status, despite their old age. As both competing-risk analyses (Cox, Fine and Gray) enable us to conclude that probabilities of death and dialysis initiation were independent in this specific geriatric population, they reinforce the identification of both indication bias in the selection process on behalf of GPs and nephrologists. The nephrologists’ dialysis decision-making was based exclusively on renal criteria as we found that eGFR <23 mL/min/1.73 m2 was the main predictive factor of dialysis initiation. In the opposite, eGFR <23 ml/min/1.73 m2 was not a predictor of death in competing-risk frameworks of the OPAIR study. Our findings suggest that predictors of death, such as age, walking impairment and anaemia (Hb <10 g/dL) in very elderly pre-ESRD patients newly referred to nephrologists seem to be features of physiological ageing process.
It is well-known that patients with severe co-morbidities may not always benefit from dialysis [15,37,38]. Of note, the prevalence of diabetes and cardiovascular diseases in French 2009 incident dialysis patients, 41% and 57% respectively, was significantly higher than in the largely older OPAIR patients [39]. Otherwise, in a vignette study, a consensus seemed to exist across GPs, non nephrology specialists and nephrologists about recognizing that dialysis was not appropriate for elderly patients under some circumstances such as terminal cancer, but still on debate about other co-morbidities, such as mild shortness of breath, diabetes and mild cognitive impairments [37]. At the opposite, younger CKD patients are usually referred to nephrologists on the basis of the level of renal function whatever their co-morbid conditions, QoL and cognitive function are. Finally, our study reinforce recommendations, emphasizing the importance of referral to specialist nephrology services largely for CKD patients on the basis of glomerular filtration rate (stage 4-5) or high levels of proteinuria [40].
In clinical practice, it is usual to start dialysis aimed to potentially improve among CKD patients less than 80 years of age and stop it if no improvement of patient’s condition is observed. At the opposite, decision to initiate dialysis among patients aged 80 years and over is based on medical considerations with strong arguments that dialysis will offer sufficient survival benefit taking into account the treatment burden of dialysis, in the best interest of the patients. In clinical practice, the appropriate decision-making in CKD elderly is based on a subtle balance between overtreatment by initiating dialysis earlier than may be necessary or maintaining dialysis with no increase in life expectancy or no improvement of QoL, and undertreatment involving late referrals to nephrologists and unplanned dialysis that leads to severely impaired QoL [11,41]. Among more than 1.8 million adults in a community-based cohort, untreated CKD among adults aged 75 years or older with baseline eGFR of 15 to 29 mL/min/1.73 m2 was approximately 2- to 10-fold more common than CKD treated by dialysis [42]. After dialysis decision-making, primary concerns of nephrologists are focused on the right moment to adequately prepare patients for dialysis and initiate dialysis in elderly. Other challenge for nephrologists treating very elderly population is posed by the choice of access and the timing of its creation. Recently, Hiremath et al. have suggested that the optimal strategy in elderly with stage 4 CKD, excluding those with a proteinuric diabetic nephropathy, should be to wait and start with a central venous catheter when required followed by an arteriovenous fistula creation, whereas most guidelines have recommended assessment of patients for access creation at stage 4 CKD [43-45].
The latest updated guidelines suggested that the timing of dialysis therapy initiation in older patients with advanced CKD should remain focused on individualized decision-making guided by clinical judgment, symptom burden and patient preference [46,47]. This approach consisted in identifying motivated patients with a good prognosis (no risk of renal progression) or those with many co-morbid conditions giving more importance to CKD compared to risk of death. This could probably explain that MMSE and QoL scores were not linked to renal prognosis in the OPAIR study. We can suppose that patients with the lowest QoL scores had no regular follow-up care and were withdrawn from dialysis. Previous data showed that an individualized model may be more appropriate than a disease-oriented model of care for many older adults with CKD [37,46-49]. Such individualized approach calls for listening to the patient, and providing prognosis and treatment information to patients and/or families. In particular, they should be informed that QoL is better improved in autonomous CKD patients on self-care dialysis than in those non-autonomous [50]. The patient will have anyway the final decision to be admitted or not into a dialysis program.
Our study has several limitations. First, the number of included patients was lower than expected. This highlighted the difficulty to establish a regular nephrology care in very elderly. As nephrology consultations are overloaded, elderly CKD patients are often followed-up by GPs. As a result, the analysis of risk factors for initiation of dialysis was underpowered. Indeed, only 17 dialysis initiations were observed during the study. For a multivariate analysis in survival analysis, it is recommended to have at least 10 events observed for each covariate [51]. Additionally, the risk of death was 2.5-fold greater than the risk of initiation of dialysis in our study. According to the incidence of dialysis initiation and death events in our study, it would be necessary to include at least 1,000 patients to study 10 covariates. Increasing the number of included patients and consequently the number of patients who initiated dialysis would require the extension of the enrolment period beyond 12 months. However, such decision would require a complex organization given the age of our patients. Second, the choice of both prevalent and incident CKD cases to be included into the study may have introduced a selection bias with an overrepresentation of prevalent cases with low risk of death as they had survived until study initiation. However, the study initiation started with the inclusion of patient to avoid the immortality bias. Third, we used the MDRD’s formula whereas it has not been yet validated in elderly. Additionally, as a function of both residual GFR and changes in lean body muscle mass (sarcopaenia) perhaps related to inflammation and chronic acidosis in stage 5 CKD, eGFR (MDRS’ formula) overestimates true GFR (inulin clearance) by about 3.3 mL/min/1.73 m2 or by about 42% [52]. Given the dependence of serum creatinine on muscle mass, there is a particular concern that eGFR slope in the elderly may be affected by changes in muscle over time. However, although potentially inaccurate as indicator of true GFR, eGFR is widely used in clinical practice and does seem to have prognostic value for death and ESRD [51]. Fourth, despite collecting extensive information about cognitive function and QoL, no positive association was drawn about their role as predictors of dialysis likelihood, on condition of no bias related to the small size of population.
Conclusions
In summary, the consistent findings of our study provide an important extension of the contemporary literature on a comprehensive view of the burden of CKD and the common practice to offer dialysis in a pre-ESRD population of Octogenarians and Nonagenarians newly referred to nephrologists.
The reasons underlying dialysis decision-making were explored from GPs and nephrologists’ perspectives. We have shown that French nephrologists have a precise clinical judgement analysis in their dialysis decision-making based on uremia criteria; these findings confirm that nephrology referral is pertinent even in very elderly pre-ESRD patients.
This original competing-risk approach potentially highlights the appropriate targets and strategies for dialysis decision-making in very elderly healthy CKD patients. Nevertheless, OPAIR raises the question of the indication of dialysis in patients with cardiac failure. This clinical condition was an important cause of death.
Additionally, further clinical research including Octogenarians reaching end-stage renal failure is needed to determine the most appropriate treatment, conservative or renal replacement therapy, which should be offered regarding co-morbidities and health status. The ongoing follow-up of the large French PSPA cohort including 581 patients older than 75 years with end-stage renal failure (eGFR less than 20 mL/min/1.73 m2) should provide tools to help the physicians, the patients and their families in dialysis decision making process [53].
Abbreviations
CI: Confidence interval; CKD: Chronic kidney disease; CRP: C-reactive protein; DBP: diastolic blood pressure; eGFR: Estimated glomerular filtration rate; ESRD: End-stage renal disease; Hb: Haemoglobin; MDRD’s formula: Modified diet in renal disease; MMSE: Mini Mental State examination; QoL: Quality of life; SD: Standard deviation; SF-36: Medical Outcomes Study 36-item Short-Form Health Survey; TSAT: Transferring saturation
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Responsibility for the design, analysis, interpretation of data and conclusion lies with the authors. All authors gave their final approval regarding submission for publication. All authors read and approved the final manuscript.
Authors’ information
BF, Head of Department of Nephrology, Hôpital Louis Pasteur, Colmar, France JBB, Research fellow of Department of Biostatistics, EA 2694, UDSL, Lille, France; Geriatric Department, University Hospital, Lille, France LF, Head of Department of Nephrology, University Hospital, Vandœuvre-lès-Nancy, France; EA 4360 Apemac, Nancy University, P. Verlaine Metz University, and Paris Descartes University, France.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Bernadette Faller, Email: bernadette.faller@ch-colmar.fr.
Jean-Baptiste Beuscart, Email: jean-baptiste.beuscart@univ-lille2.fr.
Luc Frimat, Email: l.frimat@chu-nancy.fr.
Acknowledgements
The authors gratefully acknowledge the contributions made by all nephrologists and the site study staff. They are also extremely grateful to the patients who have contributed to this study. They would like to especially thank Brigitte Risse and Murielle Popieul for data management and clinical monitoring, and Brigitte Bourdillat for the manuscript editing.
This study was funded by Amgen that was not involved in any steps of it or in the preparation of the manuscript.
OPAIR centres (Association des néphrologues de l’Est). Nephrology departments in Auxerre Hospital, Besançon CHU, Chalon sur Saône Hospital, Charleville Mézières Hospital, Colmar Hospital, Drevon Clinic in Dijon, Dôle Hospital, Evry Hospital, Lagny Polyclinic, Laon Hospital, Luxembourg Hospital, Montbéliard Hospital, Mediterranean Languedoc Haemodialysis Centre in Montpellier, Mulhouse Hospital, Nancy CHU, Reims CHU, Strasbourg CHU, Bethesda Clinic in Strasbourg, Troyes Hospital, and Verdun Hospital.
References
- Rosner M, Abdel-Rahman E, Williams ME. for the ASN Advisory Group on Geriatric Nephrology. Geriatric nephrology: responding to a growing challenge. Clin J Am Soc Nephrol. 2010;5:936–942. doi: 10.2215/CJN.08731209. [DOI] [PubMed] [Google Scholar]
- Kurella M, Chertow GM, Fried LF, Cummings SR, Harris T, Simonsick E, Satterfield S, Ayonayon H, Yaffe K. Chronic kidney disease and cognitive impairment in the elderly: the health, aging, and body composition study. J Am Soc Nephrol. 2005;16:2127–2133. doi: 10.1681/ASN.2005010005. [DOI] [PubMed] [Google Scholar]
- Stevens LA, Li S, Wang C, Huang C, Becker BN, Bomback AS, Weinstock Brown W, Rios Burrows N, Jurkovitz CT, McFarlane SI, Norris KC, Shlipak M, Whaley-Connell AT, Chen S, Bakris GL, McCullough PA. Prevalence of CKD and comorbid illness in elderly patients in the United States: results from the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2010;55:S23–33. doi: 10.1053/j.ajkd.2009.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roderick PJ, Atkins RJ, Smeeth L, Mylne A, Nitsch D, Hubbard RB, Bulpitt CJ, Fletcher AE. CKD and mortality risk in older people: a community-based population study in the United Kingdom. Am J Kidney Dis. 2009;53:950–960. doi: 10.1053/j.ajkd.2008.12.036. [DOI] [PubMed] [Google Scholar]
- Anderson S, Halter JB, Hazzard WR, Himmelfarb J, McFarland Horne F, Kaysen GA, Kusek JW, Nayfield SG, Schmader K, Tian Y, Ashworth JR, Clayton CP, Parker RP, Tarver ED, Woolard NF, High KP. for the workshop participants. Prediction, progression, and outcomes of chronic kidney disease in older adults. J Am Soc Nephrol. 2009;20:1199–1209. doi: 10.1681/ASN.2008080860. [DOI] [PubMed] [Google Scholar]
- Stengel B. L’insuffisance rénale chronique : une épidémie ? Presse Med. 2011;40:1020–1027. doi: 10.1016/j.lpm.2011.06.020. [DOI] [PubMed] [Google Scholar]
- Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- Joly D, Anglicheau D, Alberti C, Nguyen A, Touam M, Grünfeld JP, Jungers P. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J Am Soc Nephrol. 2003;14:1012–1021. doi: 10.1097/01.ASN.0000054493.04151.80. [DOI] [PubMed] [Google Scholar]
- Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med. 2007;146:177–183. doi: 10.7326/0003-4819-146-3-200702060-00006. [DOI] [PubMed] [Google Scholar]
- Couchoud C, Labeeuw M, Moranne O, Allot V, Esnault V, Frimat L, Stengel B. and for the French Renal Epidemiology and Information Network (REIN) registry. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24:1553–1561. doi: 10.1093/ndt/gfn698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurella M, Winkelmayer WC. Treated and untreated kidney failure in older adults. What’s the right balance? JAMA. 2012;307:2545–2546. doi: 10.1001/jama.2012.6667. [DOI] [PubMed] [Google Scholar]
- Clement R, Chevalet P, Rodat O, Ould-Aoudia V, Berger M. Withholding or withdrawing dialysis in the elderly: the perspective of a western region of France. Nephrol Dial Transplant. 2005;20:2446–2452. doi: 10.1093/ndt/gfi012. [DOI] [PubMed] [Google Scholar]
- Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22:1955–1962. doi: 10.1093/ndt/gfm153. [DOI] [PubMed] [Google Scholar]
- Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood R, Farrington K. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26:1608–1614. doi: 10.1093/ndt/gfq630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demoulin N, Beguin C, Labriola L, Jadoul M. Preparing renal replacement therapy in stage 4 CKD patients referred to nephrologists: a difficult balance between futility and insufficiency. A cohort study of 386 patients followed in Brussels. Nephrol Dial Transplant. 2011;26:220–226. doi: 10.1093/ndt/gfq372. [DOI] [PubMed] [Google Scholar]
- Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170:244–256. doi: 10.1093/aje/kwp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:196–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- Claudot F, Alla F, Fresson J, Calvez T, Coudane H, Bonaïti-Pellié C. Ethics and observational studies in medical research: various rules in a common framework. Int J Epidemiol. 2009;38:1104–1108. doi: 10.1093/ije/dyp164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706. doi: 10.1002/(SICI)1097-0258(19990330)18:6<695::AID-SIM60>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Kalbfleisch JD, Prentice RL. In: The statistical analysis of failure time data. Second. Wiley series in probability and statistics, editor. New Jersey: Balding DJ; 2002. Competing risks and multistate models; pp. 247–277. [Google Scholar]
- Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26:2389–2430. doi: 10.1002/sim.2712. [DOI] [PubMed] [Google Scholar]
- Prentice RL, Kalbfleisch JD, Peterson AVJ, Flournoy N, Farewell VT, Breslow NE. The analysis of failure times in the presence of competing risks. Biometrics. 1978;34:541–554. doi: 10.2307/2530374. [DOI] [PubMed] [Google Scholar]
- Pocock SJ, Clayton TC, Altman DG. Survival plots of time-to-event outcomes in clinical trials: good practice and pitfalls. Lancet. 2002;359:1686–1689. doi: 10.1016/S0140-6736(02)08594-X. [DOI] [PubMed] [Google Scholar]
- Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. doi: 10.1080/01621459.1999.10474144. [DOI] [Google Scholar]
- An Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- Van Buuren S, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45:1–67. [Google Scholar]
- Marshall A, Altman D, Holder R. Comparison of imputation methods for handling missing covariate data when fitting a Cox proportional hazards model: a resampling study. BMC Med Res Methodol. 2010;10:112. doi: 10.1186/1471-2288-10-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood AM, White IR, Royston P. How should variable selection be performed with multiply imputed data? Stat Med. 2008;27:3227–3246. doi: 10.1002/sim.3177. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation after 18+ years. J Am Stat Assoc. 1996;91:473–489. doi: 10.1080/01621459.1996.10476908. [DOI] [Google Scholar]
- Therneau T, Gramsch P, Fleming T. Martingale-based residuals for survival models. Biometrika. 1990;77:147–160. doi: 10.1093/biomet/77.1.147. [DOI] [Google Scholar]
- R Foundation for Statistical Computing. R: A Language and Environment for Statistical Computing. Vienna, Austria: ; 2010. http://www.R-project.org/ [Google Scholar]
- Stengel B, Metzger M, Froissart M, Rainfray M, Berr C, Tzourio C, Helmer C. Epidemiology and prognostic significance of chronic kidney disease in the elderly - The three-city prospective cohort study. Nephrol Dial Transplant. 2011;26:3286–3295. doi: 10.1093/ndt/gfr323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmelgam BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, Southern DA, McLaughlin K, Mortis G, Culleton BF. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int. 2006;69:2155–2161. doi: 10.1038/sj.ki.5000270. [DOI] [PubMed] [Google Scholar]
- Dalrymple LS, Katz R, Kestenbaum B, Shlipak MG, Sarnak MJ, Stehman-Breen C, Seliger S, Siscovick D, Newman AB, Fried L. Chronic kidney disease and the risk of end-stage renal disease versus death. J Gen Intern Med. 2010;26:379–385. doi: 10.1007/s11606-010-1511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leplège A, Coste J. Mesure de la santé perceptuelle et de la qualité de vie. Paris, Editions Estem: Méthodes et applications; 2002. [Google Scholar]
- Visser A, Dijkstra GJ, Huisman RM, Gansevoort RT, de Jong PE, Reijneveld SA. Differences between physicians in the likelihood of referral and acceptance of elderly patients for dialysis-influence of age and comorbidity. Nephrol Dial Transplant. 2007;22:3255–3261. doi: 10.1093/ndt/gfm382. [DOI] [PubMed] [Google Scholar]
- Patwardhan MB, Samsa GP, Matchar DB, Haley WE. Advanced chronic kidney disease practice patterns among nephrologists and non-nephrologists: a database analysis. Clin J Am Soc Nephrol. 2007;2:277–283. doi: 10.2215/CJN.02600706. [DOI] [PubMed] [Google Scholar]
- Couchoud C, Lassalle M, Stengel B, Jacquelinet C. Renal Epidemiology and Information Network: 2009 annual report. Nephrol Ther. 2011;7:S41–S214. doi: 10.1016/S1769-7255(09)73954-9. [DOI] [PubMed] [Google Scholar]
- Crowe E, Halpin D, Stevens P. on behalf of the Guideline Development Group. Early identification and management of chronic kidney disease: summary of NICE guidance. BMJ. 2008;337:812–814. doi: 10.1136/bmj.a812. [DOI] [PubMed] [Google Scholar]
- Loos C, Briançon S, Frimat L, Hanesse B, Kessler M. Effect of end-stage renal disease on the quality of life of older patients. J Am Geriatr Soc. 2003;51:229–233. doi: 10.1046/j.1532-5415.2003.51062.x. [DOI] [PubMed] [Google Scholar]
- Hemmelgarn BR, James MT, Manns BJ, O’Hare AM, Muntner P, Ravani P, Quinn RR, Turin TC, Tan Z, Tonelli M. for the Alberta Kidney Disease Network. Rates of treated and untreated kidney failure in older vs younger adults. JAMA. 2012;307:2507–2515. doi: 10.1001/jama.2012.6455. [DOI] [PubMed] [Google Scholar]
- Hiremath S, Knoll G, Weinstein MC. Should the arteriovenous fistula be created before starting dialysis? a decision analytic approach. PLoS One. 2011;6:e28453. doi: 10.1371/journal.pone.0028453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- K/DOQI Workgroup. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48(Suppl 1):S176–S247. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, Wee P, Vanholder R. EBPG on vascular access. Nephrol Dial Transplant. 2007;22(Suppl 2):ii88–117. doi: 10.1093/ndt/gfm021. [DOI] [PubMed] [Google Scholar]
- Uhlig K, Boyd C. Guidelines for the older adult with CKD. Am J Kidney Dis. 2011;58:162–165. doi: 10.1053/j.ajkd.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Leipzig RM, Whitlock EP, Wolff TA, Barton MB, Michael YL, Harris R, Petitti D, Wilt T, Siu A. for the U.S. Preventive Services Task Force Geriatric Workgroup: . Reconsidering the approach to prevention recommendations for older adults. Ann Intern Med. 2010;153:809–814. doi: 10.7326/0003-4819-153-12-201012210-00007. [DOI] [PubMed] [Google Scholar]
- Roderick PJ. Chronic kidney disease in older people: a cause for concern? Nephrol Dial Transplant. 2011;26:3083–3086. doi: 10.1093/ndt/gfr515. [DOI] [PubMed] [Google Scholar]
- O’Hare AM. The management of older adults with a low eGFR: moving toward an individualized approach. Am J Kidney Dis. 2009;53:925–927. doi: 10.1053/j.ajkd.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loos-Ayav C, Frimat L, Kessler M, Chanliau J, Durand PY, Briançon S. Changes in health-related quality of life in patients of self-care vs. in-center dialysis during the first year. Qual Life Res. 2008;17:1–9. doi: 10.1007/s11136-007-9286-1. [DOI] [PubMed] [Google Scholar]
- Concato J, Peduzzi P, Holford TR, Feinstein AR. Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol. 1995;48:1495–501. doi: 10.1016/0895-4356(95)00510-2. [DOI] [PubMed] [Google Scholar]
- Botev R, Mallié JP, Couchoud C, Schück O, Fauvel JP, Wetzels JFM, Lee N, De Santo NG, Cirillo M. Estimating glomerular filtration rate: Cockcroft–Gault and Modification of Diet in Renal Disease formulas compared to renal inulin clearance. Clin J Am Soc Nephrol. 2009;4:899–906. doi: 10.2215/CJN.05371008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moranne O, Couchoud C, Vigneau C. and PSPA Study Investigators. Characteristics and treatment course of patients older than 75 years, reaching end-stage renal failure in France. The PSPA study. J Gerontol A Biol Aci Med Sci. 2012;67:1394–1399. doi: 10.1093/gerona/gls162. [DOI] [PubMed] [Google Scholar]