Robotic assistance appears to enable the successful completion of complex hysterectomies with perioperative outcomes equivalent to laparoscopy.
Keywords: Hysterectomy, Laparoscopy, Robotic surgery
Abstract
Background and Objectives:
We compared the perioperative outcomes of hysterectomy performed by robotic (RH) versus laparoscopic (LH) routes for benign indications using the Dindo-Clavien scale for classification of the surgical complications.
Methods:
Retrospective chart review of all patients who underwent robotic (n=288) and laparoscopic (n=257) hysterectomies by minimally invasive surgeons at the University of Michigan from March 2001 until June 2010.
Results:
Age, body mass index, operative time, and estimated blood loss were not statistically different between groups. The RH subgroup had a larger uterine weight (LH 186.4±130.6 g vs RH 234.9±193.9 g, P=.001), higher prevalence of severe adhesions (13.2% vs 23.3%, respectively, P=.003), and stage III–IV endometriosis (4.7% vs 15.3%, respectively, P<.05). There were no differences in the rates of Dindo-Clavien grade I, grade II, and grade III surgical complications between the RH and LH groups (9.7%, 13.2%, and 3.1%, respectively, in the RH group vs 6.2%, 9.3%, and 5.8%, respectively, in the LH group, P>.05). However, the rates of urinary tract infection were higher in the RH group (LH 2.7% vs RH 6.9%, P=.02), whereas the conversion to laparotomy rate was higher in the LH group (LH 6.2% vs RH 1.7%, P=.007).
Conclusions:
Perioperative outcomes for laparoscopic and robotic hysterectomy for benign indications appear to be equivalent.
INTRODUCTION
Interest in minimally invasive gynecological surgery has grown tremendously over the past 20 years. Numerous studies have demonstrated the benefits of laparoscopy over laparotomy, including decreased blood loss, shorter length of hospital stay, decreased pain, earlier return to routine activities, and improved cosmesis.1,2 Despite these advantages, the percentage of gynecological hysterectomies performed laparoscopically has remained relatively stagnant at 12% to 14% nationally.3–5 Some of the proposed reasons for its lack of widespread implementation are the need for specialized training, its steep learning curve, longer operative time, 2-D view, limited degrees of instrument motion, and tremor amplification. The da Vinci surgical system (Intuitive Surgical, Sunnyvale, CA) has improved on these shortcomings intrinsic to laparoscopy and has been rapidly incorporated into clinical practice.
Feasibility studies have shown success in performing robotic hysterectomy, myomectomy, sacrocolpopexy, gynecologic cancer staging, and tubal reanastomsis.6–10 Similar to those about laparoscopy, studies have shown improved surgical outcomes (decreased blood loss, shorter length of stay, decreased pain, and earlier return to activities) with robotic surgery when compared with an abdominal route.11–14 Although there are clear benefits of both robotic and laparoscopic surgery over laparotomy, few studies have directly compared perioperative outcomes of robotic and laparoscopic hysterectomy for benign indications. In a recent review of the literature, Sarlos and Kots15 concluded that most clinical outcomes such as blood loss, complications, and hospital stay were comparable for the robotic and the laparoscopic hysterectomy. However, despite the paucity of supportive data, robotic surgery has been rapidly adopted into gynecological practice and has grown at a rate that has far exceeded that seen with laparoscopy.
The purpose of this study is to compare perioperative outcomes in all consecutive patients undergoing laparoscopic and robotic hysterectomy for benign indication at one academic center.
MATERIALS AND METHODS
After institutional review board approval, consecutive cases of laparoscopic and robotic hysterectomy for benign indications were collected by search of billing codes and retrospectively reviewed by electronic medical record. Included were all laparoscopic and robotic hysterectomies performed from March 1, 2001 until June 30, 2010, by the faculty of the Minimally Invasive Gynecology Division at the University of Michigan Health System. All 3 surgeons were fellowship trained in minimally invasive gynecological surgery and were proficient in laparoscopic hysterectomy but had newly incorporated robotic surgery during the study period. The University of Michigan is a teaching hospital, and residents and/or fellows participated in all procedures at various levels as deemed appropriate by the faculty surgeon. Data regarding the extent of trainee involvement were not collected and are not part of this study. The surgical approach was determined preoperatively according to the surgeon's and patient's preferences, based on the specific patient's characteristics. Women with a preoperative diagnosis of malignancy and those who underwent concomitant procedures for treatment of urinary incontinence and/or pelvic organ prolapse were excluded from the study. Only patients with American Association of Gynecologic Laparoscopists (AAGL) type IVE total hysterectomy and type III laparoscopic supracervical hysterectomy were included.16
A systematic chart review using standardized case report forms was conducted. Demographic and patient variables collected were age, parity, body mass index, race, medical and surgical history, preoperative symptoms, previous treatment(s), and primary indication for surgery. Recorded surgical variables were surgical route, surgical procedure, operating time (intubation to exit from the operating room), revised American Fertility Society endometriosis score,17 Diamond adhesion index score,18 culdotomy technique, estimated blood loss, final pathological diagnosis, specimen weight, and length of hospital stay. No charts were excluded because <1% of all charts were missing data for uterine weight and operative time only.
All patients were scheduled for postoperative follow-up within 4 to 8 weeks from surgery. Patients' attendance at this visit and duration of postoperative follow-up were obtained from the medical records.
The medical records were reviewed for intraoperative and postoperative complications occurring for 12 weeks after hysterectomy. However, complications clearly related to surgery such as cuff dehiscence were included regardless of the time of occurrence. The postoperative complications were classified into severity grades according to the Dindo-Clavien scale.19 This classification is based on the type of therapy needed to correct the complication and was found to be reproducible and applicable to various surgical fields, including gynecology.20 Grade I complication includes any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, and radiological interventions. Grade II complications include blood transfusions or total parenteral nutrition or other intervention that requires pharmacological treatment with drugs other than such allowed for grade I complications. Grade III complications require surgical, endoscopic, or radiological intervention.
Surgical Procedures
Total hysterectomy was performed according to the AAGL type IVE, laparoscopically directed removal of the entire uterus, and supracervical hysterectomy was performed according to AAGL laparoscopic supracervical hysterectomy type III; occlusion and division of uterine arteries were performed laparoscopically.16 All patients were given prophylactic antibiotics at the start of surgery. The ZUMI or the RUMI uterine manipulators backloaded with a KOH colpotomy ring (all by Cooper Surgical, Trumbull, CT) were used. The uterine arteries were controlled with the use of electrosurgical instruments.
The da Vinci robotic surgical platform was used in all cases of robotic hysterectomy. The monopolar shears and the Gyrus PK dissecting forceps (Gyrus ACMI, Norwalk, OH) were placed in the right and left robotic arms, respectively, for the hysterectomy procedure, and the tenaculum or Prograsp forceps were sometimes used in the fourth robotic arm (all by Intuitive Surgical, Sunnyvale, CA). Culdotomy or amputation of the uterine corpus was performed using the monopolar scissors at 30 W coagulation current. The vaginal cuff was closed with a series of figure-eight stitches using a 0-Vicryl suture (Ethicon, Cincinnati, OH) with intracorporeal knot-tying.
The laparoscopic hysterectomy was performed using the Gyrus PK cutting forceps. Culdotomy or amputation of the uterine corpus was performed using the monopolar J-hook (range: 30–50 W cut current), bipolar spatula (Gyrus ACMI), or Harmonic scalpel (Ethicon). The Endostich device (Covidien, Mansfield, MA) was used for vaginal cuff closure using a series of 0-Vicryl interrupted or figure-eight sutures and extracorporeal knot-tying. The uterosacral ligaments were incorporated in the angle closures of both surgical approaches.
Statistical analyses were performed using the SPSS software, version 17.0 (IBM, Armonk, NY). Two-tailed statistical significance was set at .05. A normal distribution of the data was determined using the Kolmogorov-Smirnov test. The Student t test was used for comparison of means for normally distributed data, whereas the Mann-Whitney U test was used for comparison of non-normally distributed data. The χ2 and the Fisher exact test were used when appropriate for comparison of proportions.
RESULTS
A total of 545 patients underwent hysterectomy for benign disease during the study period; 257 were performed laparoscopically (LH) and 288 were performed robotically (RH). Among all patients, 98% had documented follow-up after surgery, with 83% of patients followed for ≥4 weeks and 60% followed for ≥6 weeks.
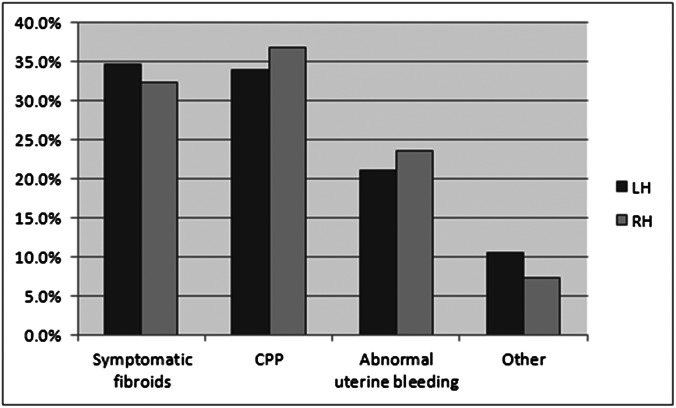
Patients' demographics are compared in Table 1. There were no statistically significant differences in mean age, body mass index, and prevalence of diabetes or hypertension between the 2 groups. There was a higher prevalence of higher-order (≥2) laparotomies in the robotic cohort (LH 14.8% vs RH 26.0%, P<.05). In both cohorts, the most common indications for surgery were chronic pelvic pain and symptomatic uterine fibroids, followed by abnormal uterine bleeding (P>.05) (Figure 1).
Table 1.
Comparison of Patient Demographics Between the Laparoscopic (LH) and Robotic (RH) Cohorts
| LH (n=257) | RH (n=288) | P Value | |
|---|---|---|---|
| Agea (y) | 42.3±6.9 | 43.2±7.1 | .1 |
| Parityb | 2 (0–5) | 2 (0–6) | .8 |
| BMIa,c (kg/m2) | 29.1±6.7 | 30.3±8.6 | .08 |
| Race (%) | .03 | ||
| White | 212 (82.5) | 213 (74.0) | |
| Black | 32 (12.5) | 37 (12.8) | |
| Asian | 5 (1.9) | 8 (2.8) | |
| Other | 8 (3.1) | 30 (10.4) | |
| Diabetes (%) | 15 (5.8) | 16 (5.6) | .6 |
| Hypertension (%) | 38 (14.8) | 47 (16.3) | .5 |
| Previous laparotomy (%) | .002 | ||
| ≥1 | 90 (35.0) | 151 (52.4) | |
| ≥2 | 38 (14.8) | 75 (26.0) |
Expressed as mean ± standard deviation.
Expressed as median (range).
BMI = body mass index.
Figure 1.
Primary indications for hysterectomy in the laparoscopic (LH) and robotic (RH) cohorts. CPP = chronic pelvic pain. “Others” refers to adnexal masses, endometrial hyperplasia, and cervical dysplasia.
Operative characteristics for each group are summarized in Table 2. The rates of total hysterectomy and concomitant adnexectomy were similar in both groups, as were the estimated blood loss and operative time. Intraoperatively confirmed stage III–IV endometriosis and the incidence of severe adhesions (defined as a Diamond adhesion score >11) were more common in women undergoing robotic hysterectomy. The mean uterine weight was also greater in the robotic cohort (LH 186.4±130.6 g, 95% confidence interval 170.0–202.8 g vs RH 234.9±193.9 g, 95% confidence interval 212.3–257.7 g, P=.001). The conversion to laparotomy rates were significantly higher in the laparoscopic cohort (LH 6.2% vs RH 1.7%, P=.007).
Table 2.
Comparison of Intraoperative Surgical Characteristics Between the Laparoscopic (LH) and Robotic (RH) Cohorts
| LH (n=257) | RH (n=288) | P Value | |
|---|---|---|---|
| Total hysterectomy (%) | 185 (72.0) | 213 (74.0) | .6 |
| Concomitant USO/BSOa (%) | 102 (39.7) | 109 (37.8) | .3 |
| Stage III/IV endometriosis (%) | 12 (4.7) | 44 (15.3) | .001 |
| Severe adhesionsb (%) | 34 (13.2) | 67 (23.3) | .003 |
| Uterine weightc (g) | 186.4±130.6 | 234.9±193.9 | .001 |
| Estimated blood lossc (mL) | 100.9±136.4 | 99.4±166.5 | .9 |
| Operative timec (min) | 228.1±60.1 | 231.0±64.2 | .9 |
| Conversion to laparotomy (%) | 16 (6.2) | 5 (1.7) | .007 |
USO = unilateral salpingo-oophorectomy; BSO = bilateral salpingo-oophorectomy.
Defined as Diamond adhesion score ≥11.
Expressed as mean ± standard deviation.
The surgical complications classified according to the Dindo-Clavien scale in the 2 groups are compared in Table 3. Although grade I and grade II complications were seemingly more prevalent in the robotic group (grade I, LH 6.2% vs RH 9.7% and grade II, LH 9.3% vs 13.2%), whereas grade III complications were more prevalent in the laparoscopic group (LH 5.8% vs RH 3.1%), these differences did not reach statistical significance (P>.1). There were no cases of grade IV or grade IV complications in either group.
Table 3.
Comparison of Postoperative Surgical Complications Between the Laparoscopic (LH) and Robotic (RH) Cohorts According to the Dindo-Clavien Scale
| Gradea | LH (n=257) | RH (n=288) | P Value |
|---|---|---|---|
| I (%) | 16 (6.2) | 28 (9.7) | .2 |
| II (%) | 24 (9.3) | 38 (13.2) | .2 |
| III (%) | 15 (5.8) | 9 (3.1) | .1 |
| IIIa (%) | 1 (0.4) | 4 (1.4) | |
| IIIb (%) | 14 (5.4) | 5 (1.7) |
There were no cases of grade IV or grade V complications in either group.
The various perioperative complications in the 2 groups are compared in Table 4. The incidence of viscus injury (bowel, bladder, ureter) was low in both groups (LH 1.2% vs RH 1.7%, P=.4). Overall, there were 4 bladder injuries, 3 of which were recognized and repaired intraoperatively, and 2 bowel injuries, 1 of which was recognized and repaired intraoperatively. One patient who underwent robotic hysterectomy sustained a combined bladder and bowel injury diagnosed 14 days postoperatively after presenting with fever and pelvic abscess. There were 2 ureteral injuries in the LH group and 1 in the RH group. All 3 cases were managed conservatively with either temporary ureteral stenting or percutaneous nephrostomy.
Table 4.
Comparison of Perioperative Complications Between the Laparoscopic (LH) and Robotic (RH) Cohorts
| LH (n=244) | RH (n=255) | P Value | |
|---|---|---|---|
| Viscus injurya (%) | 3 (1.2) | 5 (1.7) | .4 |
| Blood transfusion (%) | 3 (1.2) | 1 (0.3) | .3 |
| Vesicovaginal fistula (%) | 1 (0.4) | 0 | .9 |
| Vaginal cuff complicationsb (%) | 6 (2.3) | 14 (4.9) | .09 |
| Vaginal cuff dehiscence (%) | 5 (1.9) | 1 (0.3) | .08 |
| Thrombotic event (%) | 2 (0.8) | 0 | .2 |
| Pneumonia (%) | 0 | 2 (0.7) | .3 |
| Urinary tract infection (%) | 7 (2.7) | 20 (6.9) | .02 |
| Urinary retention (%) | 11 (4.3) | 31 (10.8) | .003 |
| Ileus (%) | 0 | 2 (0.7) | .3 |
| Wound complicationsc (%) | 5 (1.9) | 9 (3.1) | .3 |
| Reoperation (%) | 13 (5.1) | 5 (1.7) | .03 |
Bowel, bladder, and ureteral injury.
Vaginal cuff abscess, cuff cellulitis, and cuff hematoma.
Wound infection and wound hematoma.
There were fewer patients with vaginal cuff dehiscence in the RH cohort (0.5%) than in the LH cohort (2.7%), but this difference did not reach statistical significance (P=.07) (Table 4). All patients reported coitus immediately preceding cuff dehiscence. However, not all episodes were associated with the first coitus after the hysterectomy. Five of the 6 patients with cuff dehiscence presented within 3 months after their surgery, and the sixth patient presented on the 29th postoperative day. There was no significant relationship between vaginal cuff dehiscence and age, body mass index, menopausal status, diabetes, tobacco use, estimated blood loss, or type of energy used for culdotomy (data not shown).
The rates of other vaginal cuff complications (ie, cellulitis, abscess, and hematoma) were similar in the 2 groups (LH 2.3% vs RH 4.9%, P=.09) (Table 4). Vaginal cuff abscess occurred in 1.2% of LH patients versus 2.4% of RH patients (P=.2). The incidence of cuff abscess increased with the severity of endometriosis, with a 1.1% incidence in patients without endometriosis, 2.6% incidence in patients with stage I–II endometriosis, and 9.3% incidence in patients with stage III–IV endometriosis (P=.01). There was no association between vaginal cuff abscess and body mass index, diabetes, tobacco use, operative time, estimated blood loss, or the need for morcellation (data not shown).
There was a significantly higher rate of urinary tract infection and urinary retention in the RH cohort than in the LH cohort (Table 4). Urinary retention was not associated with age, body mass index, presence of diabetes, smoking status, previous cesarean sections, previous abdominal surgeries, uterine weight, intra-abdominal adhesions, or estimated blood loss (data not shown).
Overall, the need for reoperation was statistically greater in the LH cohort (Table 4). The indications for reoperation in the laparoscopic cohort included vaginal cuff dehiscence (n=5), significant vaginal cuff bleeding (n=2), vaginal cuff abscess (n=2), cystoscopic repair of ureteral injury (n=1), vesicovaginal fistula (n=1), prolapsed fallopian tube through the vaginal cuff (n=1), and trocar site hematoma (n=1). In the RH cohort, 5 patients underwent reoperation for vaginal cuff abscess (n=2), vaginal cuff bleeding (n=1), cuff dehiscence (n=1), and repair of bladder and bowel injury (n=1).
DISCUSSION
This series directly compares perioperative outcomes of LH with RH for benign indications. Our data suggest that more complex surgeries are being performed robotically, as indicated by the higher prevalence of stage III–IV endometriosis, high-order (≥2) previous laparotomies, severe adhesions, and a larger mean uterine weight. Despite the greater complexity of surgery, surgical outcomes including surgical complications, estimated blood loss, and operative time are similar between RH and LH groups, and the overall complication rate is acceptably low. Because this is a retrospective study, the difference in complexity of cases between the 2 groups reflects the surgeons' preference to perform complex hysterectomies via the robotic route. A randomized study would be better designed to compare the outcome of the 2 surgical approaches for cases of similar complexity.
Another drawback of our study is the different distribution of the LH and RH cases over the ∼10-year study period, with more LH cases performed in the earlier years and more RH cases performed in later years. This may introduce a bias in the occurrence of surgical complication in the laparoscopic groups because it could be assumed that the surgeons gained additional surgical experience during the 10 years of the study. However, this bias may be offset by the surgeons being novice robotic surgeons when this technique was introduced.
Previous studies reporting surgical complications of laparoscopic and robotic hysterectomy classified these complications into major and minor categories. In these studies, the rate of major complications varied widely, from <1% to 20%. This wide range is probably because of the absence of a standard definition of a major or minor complication as well as extreme variability in the follow-up time for reporting of complications, ranging from 1 day to >6 weeks.11–15 In the current study, the Dindo-Clavien scale was used to classify the surgical complications. This system grades surgical complications according to the treatments required19 and has been shown to be reproducible and fairly easy to use.20 Using the Dindo-Clavien scale, there were no statistically significant differences in surgical complications between the 2 groups, and the rates of grade III complications were low in both groups, indicating that both surgeries can be performed safely. Nevertheless, our study may still be underpowered to detect differences in rare postoperative complications such as viscus injury. Further studies and meta-analyses could provide additional data on the occurrence of these rare complications.
Postoperative vaginal cuff abscess was an infrequent complication in both the LH and RH groups and was directly related to the presence and severity of endometriosis. We postulate that this relationship is a consequence of greater tissue dissection, greater use of electrosurgery, more tissue necrosis, and possibly a less hemostatic surgical bed associated with both the laparoscopic and the robotic approach to an obliterated cul-de-sac.
Previous studies have consistently shown the incidence of cuff dehiscence complicating total LH and RH to be higher than the vaginal and abdominal routes.21–23 The incidence of cuff dehiscence after total laparoscopic hysterectomy was found to be as high as 4.9% in a large retrospective study from 2007.24 However, the data from this large study were recently reanalyzed and showed the 10-year cumulative incidence of dehiscence after total LH to be 1.35%.25 In the current study, the incidence of cuff dehiscence after total laparoscopic hysterectomy was higher when compared with RH. This difference approached, but did not reach, statistical significance (P=.07), possibly because the sample size was underpowered to detect this relatively rare complication.
Operative cost is another important consideration when comparing LH with RH. Two previous studies26,27 estimated that the added cost of robotic hysterectomy over laparoscopic hysterectomy is in the range of $2600. This factor needs to be considered when determining the appropriate route of surgery, especially because operative outcomes for these 2 routes appear to be similar.
Our study is limited by its retrospective and nonrandomized design, leading to possible inaccurate or incomplete data collection, which may result in an underestimation of surgical complications. The nonrandomized retrospective design is also known to be associated with possible selection case bias, where more difficult cases may have been chosen for a robotic approach according to surgeon preference. Another limitation of our study is the long duration of the study period, during which some surgical and postoperative management practices may have changed. Conversely, collecting data over a long period enabled us to include a relatively large number of patients.
CONCLUSION
Perioperative outcomes for LH and RH for benign indications are equivalent. These findings are similar to a recent Cochrane Review that concluded limited evidence showed that robotic surgery did not benefit women with benign gynecological disease as far as effectiveness or safety.28 Our study suggested that some outcomes trend toward improvement with a robotic route, including a lower incidence of vaginal cuff dehiscence and a lower rate of conversion to laparotomy. Future studies using a randomized study design may further investigate the operative outcomes of the robotic and laparoscopic routes.
Contributor Information
Kristin E. Patzkowsky, Montefiore Medical Center, Centennial Women's Center, Bronx, NY, USA.
Sawsan As-Sanie, University of Michigan Health Center, Ann Arbor, MI, USA..
Noam Smorgick, University of Michigan Health Center, Ann Arbor, MI, USA..
Arleen H. Song, Celebration Hospital, Celebration, FL, USA..
Arnold P. Advincula, University of Michigan Health Center, Ann Arbor, MI, USA..
References:
- 1. Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomized controlled trials. BMJ. 2005;330:1478–1486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cohcrane Database Syst Rev. 2009;8:CD003677. [DOI] [PubMed] [Google Scholar]
- 3. Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990–1997. Obstet Gynecol. 2002;99:229–234 [DOI] [PubMed] [Google Scholar]
- 4. Jacoby VL, Autry A, Jacobson G, Domush R, Nkagawa A, Jacoby A. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041–1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–1095 [DOI] [PubMed] [Google Scholar]
- 6. Advincula AP, Song AH, Burke W, Reynolds RK. Preliminary experience with robot-assisted laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004;11:511–518 [DOI] [PubMed] [Google Scholar]
- 7. Daneshgari F, Kefer JC, Moore C, Kaouk J. Robotic abdominal sacrocolpopexy/sacrouteropexy repair of advanced female pelvic organ prolapse (POP): utilizing POP-quantification based staging and outcomes. BJU Int. 2007;100:875–879 [DOI] [PubMed] [Google Scholar]
- 8. Degueldre M, Vandromme J, Huong PT, Cadiere GB. Robotically assisted laparoscopic microsurgical tubal reanastomosis: a feasibility study. Fertil Steril. 2000;74:1020–1023 [DOI] [PubMed] [Google Scholar]
- 9. Marchal F, Rauch P, VAndromme J, et al. Telerobotic-assisted laparoscopic hysterectomy for benign and oncologic pathologies: initial clinical experience with 30 patients. Surg Endosc. 2005;19:826–831 [DOI] [PubMed] [Google Scholar]
- 10. Reynolds RK, Advincula AP. Robot-assisted laparoscopic hysterectomy: technique and initial experience. Am J Surg. 2006;191:555–560 [DOI] [PubMed] [Google Scholar]
- 11. Boggess JF. A comparative study of three surgical methods for hysterectomy with staging for endometrial cancer; robotic assistance, laparoscopy, laparotomy. Am J Obstet Gynecol. 2008;199:360.e1–9 [DOI] [PubMed] [Google Scholar]
- 12. Boggess JF, Gehrig PA, Cantrell L, et al. A case-control study of robotic assisted type III radical hysterectomy with pelvic lymph-node dissection compared with open radical hysterectomy. Am J Obstet Gynecol. 2008;199:357.e1–7 [DOI] [PubMed] [Google Scholar]
- 13. Magrina JF, Kho RM, Weaver AL, Motero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008;109:86–91 [DOI] [PubMed] [Google Scholar]
- 14. Shashoua AR, Gill D, Locher SR. Robotic-assisted total laparoscopic hysterectomy versus conventional total laparoscopic hysterectomy. JSLS. 2009;13(3):364–369 [PMC free article] [PubMed] [Google Scholar]
- 15. Sarlos D, Kots LA. Robotic versus laparoscopic hysterectomy: a review of recent comparative studies. Curr Opin Obstet Gynecol. 2011;23:283–288 [DOI] [PubMed] [Google Scholar]
- 16. Olive DL, Parker WH, Cooper JM, Levine RL. The AAGL classification system for laparoscopic hysterectomy. J Am Assoc Gynecol Laparosc. 2000;7:9–15 [DOI] [PubMed] [Google Scholar]
- 17. The American Fertility Society Revised American Fertility Society classification of endometriosis: 1985. Fertil Steril. 1985;43:351–352 [DOI] [PubMed] [Google Scholar]
- 18. Diamond MP, Daniell JF, Johns DA, et al. Postoperative adhesion development after operative laparoscopy: evaluation at early second-look procedures. Operative Laparoscopy Study Group Fertil Steril. 1991;55:700–704 [PubMed] [Google Scholar]
- 19. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196 [DOI] [PubMed] [Google Scholar]
- 21. Donnez O, Jadoul P, Squifflet J, Donnez J. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG. 2009;116:492–500 [DOI] [PubMed] [Google Scholar]
- 22. Garry R, Fountain J, Mason S, et al. The eVALuate study: two parallel randomized trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004;328:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Makinen J, Johansson J, Tomas C, et al. Morbidity of 10,110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473–1478 [DOI] [PubMed] [Google Scholar]
- 24. Hur HC, Guido RS, Mansuria SM, Hacker MR, Sanfilippo JS, Lee TT. Incidence and patient characteristics of vaginal cuff dehiscence after different modes of hysterectomies. J Minim Invasive Gynecol. 2007;14:311–317 [DOI] [PubMed] [Google Scholar]
- 25. Hur HC, Donnellan N, Mansuria S, Barber RE, Guido R, Lee T. Vaginal cuff dehiscence after different modes of hysterectomy. Obstet Gynecol. 2011;118:794–801 [DOI] [PubMed] [Google Scholar]
- 26. Sarlos D, Kots L, Stevanovic N, Schaer G. Robotic hysterectomy versus conventional laparoscopic hysterectomy: outcome and cost analyses of a matched case-control study. Eur J Obstet Gynecol Reprod Biol. 2010;150:92–96 [DOI] [PubMed] [Google Scholar]
- 27. Pasic RP, Rizzo JA, Fang H, et al. Comparing robot-assisted with conventional laparoscopic hysterectomy: impact on cost and clinical outcomes. J Minim Invasive Gynecol. 2010;17:730–738 [DOI] [PubMed] [Google Scholar]
- 28. Liu H, Lu D, Wang L, Shi G, Clarke J. Robotic surgery for benign gynaecolgical disease. Cochrane Database Syst Rev. 2012;15;2:CD008978. [DOI] [PubMed] [Google Scholar]