Laparoscopic and robotic-assisted laparoscopic myomectomies demonstrated shorter hospital stays, less blood loss, and fewer transfusions than abdominal myomectomies. Robotic myomectomy offers a minimally invasive alternative for management of symptomatic myoma in a community hospital setting.
Keywords: Myomectomy, Robotic surgery, Laparoscopic, Laparoscopy, Fibroids
Abstract
Background and Objectives:
To evaluate the operative outcomes between robotic, laparoscopic, and abdominal myomectomies performed by a private gynecologic oncology practice in a suburban community hospital.
Methods:
The medical records of 322 consecutive robotic, laparoscopic, and abdominal myomectomies performed from January 2007 through December 2009 were reviewed. The outcomes were collected from a retrospective review of patient medical records.
Results:
Records for 14/322 (4.3%) patients were incomplete. Complete data were available for 308 patients, including 169 (54.9%) abdominal, 73 (23.7%) laparoscopic, and 66 (21.4%) robotic-assisted laparoscopic myomectomies. Patients were similar in age, body mass index, parity, and previous abdominopelvic surgery. Median operative time for robotic surgery (140 min) was significantly longer (P<.005) compared to laparoscopic (70 min) and abdominal (72 min) myomectomies. Robotic and laparoscopic myomectomies had significantly less estimated blood loss and hospital stay compared to abdominal myomectomies. There was no significant difference in complications or in the median size of the largest myoma removed between the different modalities. However, the median aggregate weight of myomas removed abdominally (200g; range, 1.4 to 2682) was significantly larger than that seen laparoscopically (115g; range, 1 to 602) and robotically (129g; range 9.4 to 935). Postoperative transfusion was significantly less frequent in robotic myomectomies compared to laparoscopic and abdominal myomectomies.
Conclusion:
While robotic-assisted laparoscopic myomectomies had longer operative times, laparoscopic and robotic-assisted laparoscopic myomectomies demonstrated shorter hospital stays, less blood loss, and fewer transfusions than abdominal myomectomies. Robotic myomectomy offers a minimally invasive alternative for management of symptomatic myoma in a community hospital setting.
INTRODUCTION
Fibroids are the most common benign tumor of the uterus and are present in up to 80% of women. Although only 25% of women are affected by symptoms like pelvic pain, pressure, heavy menses, recurrent pregnancy loss, and infertility, it remains the leading indication for hysterectomy and a common women's health concern.1,2 Treatment alternatives include medical management with oral contraceptives, nonsteroidal anti-inflammatory medications, or GnRH agonists. Additionally, evolving technology continues to expand the conservative options available for women desiring uterine preservation to include uterine artery embolization, MRI-guided high frequency ultrasound, and radio frequency ablation. Myomectomy, however, remains the gold-standard for women affected by symptoms of a fibroid uterus who desire uterine preservation.3
Myomectomy has traditionally been managed by laparotomy and has demonstrated effective clinical outcomes for symptoms as well as fertility.4,5 Comparison of outcomes for laparoscopic and robotic-assisted laparoscopic myomectomy (RALM) has demonstrated comparable clinical outcomes for blood loss, hospital stay, and complications despite longer robotic operative times.6,7 The feasibility of the adoption of robotic-assisted surgery by the community gynecologist has been discussed by Payne et al.8 The authors concluded that the length of stay and decrease in blood loss seen with robotic-assisted surgery “hold true not only for academic centers but also in community settings involving the general gynecologist.” However, the data regarding myomectomies have primarily been reported from university teaching hospitals and regional medical centers. Considering the limited adoption of these techniques in the community hospital setting, this study sought to evaluate operative outcomes of abdominal, laparoscopic, and RALM performed in a community hospital.
METHODS
All myomectomies performed consecutively in a single gynecology practice from January 2007 through December 2009 were identified. All procedures were performed by 1 of 2 gynecologic oncologists in a single community hospital. Both surgeons were experienced advanced laparoscopists. The same providers performed the preoperative evaluation and counseling for each patient to determine the indication and route of surgery. The hospital electronic medical record was used to review and collect data from each patient's chart including scanned outpatient encounters and imaging reports presented as part of the preoperative admission documentation. All patients with documented removal of at least 1 myoma were included. Patients were excluded if no record was available or no documentation of myoma removal was evident in the record.
Demographic data, including age, race, body mass index (BMI), and parity were collected. Additionally, baseline clinical data including indication for surgery, symptomatology, number of myoma, size of largest myoma, American Society of Anesthesiologists (ASA) physical status classification, and history of prior abdominal or pelvic surgery was recorded. Perioperative outcomes, which included operative time, length of hospital stay, estimated blood loss, packed red blood cell (PRBC) transfusion, and intraoperative and postoperative complications, as well as aggregate myoma weight, were collected for comparison among operative groups.
Surgical indications were categorized into symptoms of bleeding, pain or pressure, fertility, and other. The largest myoma was documented as the greatest diameter of the single largest myoma reported on preoperative imaging by ultrasound or magnetic resonance imaging (MRI). The myoma weight was determined as the aggregate weight of tissue reported from the pathology report. Operative time and estimated blood loss was extracted from the anesthesia record. Length of hospital stay was documented as date of discharge less date of admission, whereas 0 d indicates same day surgery. The primary outcomes were identified as length of hospital stay, estimated blood loss, and operative time. Finally, intraoperative or postoperative complications, transfusions, and myoma characteristics were secondarily compared among groups.
Symmetrically distributed numerical variables were summarized with means and standard deviations while other variables were summarized with medians and ranges. Appropriate parametric tests were utilized where data demonstrated normal distribution, and nonparametric tests were used for alternative parameters. For numerical variables, univariable comparisons were conducted with either analysis of variance or Kruskal-Wallis analysis of ranks (for non-normal data). χ2 and Fisher exact test were used for categorical data. Statistical analysis was performed using SPSS for Windows Inc. version 16 (Nov 2007). Differences were considered significant at P<.05. This protocol was granted exempt status by the Holy Cross Hospital Institutional Review Board.
RESULTS
A total of 322 records were analyzed with 14/322 (4.3%) records excluded for incomplete or absent data. Complete data were available for 308/322 (95.7%) patients including 169 (54.9%) abdominal, 73 (23.7%) laparoscopic, and 66 (21.4%) robotic-assisted myomectomies. Patients in each category were similar in age, BMI, parity, and previous abdominopelvic surgery (Table 1). Patients who reported their race as black, however, more often underwent abdominal myomectomy (Table 2). Additionally, evaluation of baseline clinical characteristics revealed no statistically significant difference in patients with prior myomectomy, ASA classification, or presenting symptoms of pain, pressure, and bleeding (Tables 1 and 2). Patients with a fertility indication more frequently had an abdominal myomectomy (Table 2).
Table 1.
Operative Outcomes of Abdominal, Laparoscopic, and Robotic Assisted-Laparoscopic Myomectomy in a Community Hospital
Comparison of Demographic Data
| Type of Myomectomy | n | Age [(yrs) Median (range)] p=0.69 | BMI (p=0.067) | Black [n (%); p=0.001] | White [n (%); p=0.001] | Asian [n (%); p=0.001] | Other Race [n (%); p=0.001] | Prior Parity [n (%); p=0.053] | Prior Surgery [n (%); p=0.74] | Prior Myomectomy [n (%); p=0.063] | ASA 1 [n (%); p=0.13] | ASA 2 [n (%); p=0.13] | ASA 3 [n (%); p=0.13] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdominal | 169 | 39 (27–50) | 27 (18–46) | 103 (61%) | 38 (22%) | 12 (7%) | 16 (10%) | 26 (15%) | 70 (42%) | 20 (12%) | 33 (21%) | 108 (70%) | 13 (8%) |
| Laparoscopic | 73 | 39 (23–56) | 25 (19–52) | 23 (32%) | 31 (42%) | 7 (10%) | 12 (16%) | 16 (22%) | 30 (41%) | 2 (3%) | 18 (27%) | 47 (71%) | 37 (2%) |
| Robotic | 66 | 40 (26–51) | 27 (19–53) | 28 (42%) | 22 (33%) | 9 (14%) | 7 (11%) | 18 (27%) | 24 (36%) | 5 (8%) | 13 (31%) | 1 (60%) | 6 (10%) |
Table 2.
Comparison of Preoperative Symptoms/Indications
| Type of Myomectomy | n | Pain/Pressure [n (%); p=0.072] | Bleeding [n (%); p=0.64] | Fertility [n (%); p=0.0005] | Other [n (%); p=0.003] |
|---|---|---|---|---|---|
| Abdominal | 169 | 55 (33%) | 66 (39%) | 92 (54%) | 5 (3%) |
| Laparoscopic | 73 | 35 (48%) | 24 (33%) | 19 (26%) | 10 (14%) |
| Robotic | 66 | 23 (35%) | 23 (35%) | 23 (35%) | 7 (11%) |
Operative time for robotic surgery (140 min; range, 55 to 328) was longer compared to laparoscopic (70 min; range, 17 to 218) and abdominal myomectomy (17 min; range, 13 to 185; P<.005). Laparoscopic and robotic myomectomy had significantly (P<.005) less estimated blood loss as well as shorter hospital stay compared to abdominal myomectomy (Table 3). Among secondary outcomes, there was no significant difference between all modalities of surgery for postoperative complication or between laparoscopic and robotic surgery for conversion to laparotomy. However, postoperative transfusion was significantly (P<.005) less frequent in robotic myomectomy compared to laparoscopic and abdominal myomectomy (Table 3).
Table 3.
Comparison of Perioperative Outcomes
| Type of Myomectomy | n | Procedure Time [(min) Median (range) p<0.0005] | Hospital Stay [(days) Median (range) p<0.0005] | EBL [(mL) Median (range) p<0.0005] | Post-op Complications [n (%) p=0.58] | Transfusion [n (%) p<0.0005] | Conversions to Laparotomy [n (%) p=0.5] |
|---|---|---|---|---|---|---|---|
| Abdominal | 169 | 72 (13–185) | 2 (0–12) | 200 (10–2500) | 17 (10%) | 43 (26%) | N/A |
| Laparoscopic | 73 | 70 (17–218) | 0 (0–6) | 100 (10–1800) | 5 (7%) | 9 (12%) | 6 (8%) |
| Robotic | 66 | 140 (55–328) | 1 (0–17) | 100 (10–1000) | 8 (12%) | 4 (6%) | 3 (5%) |
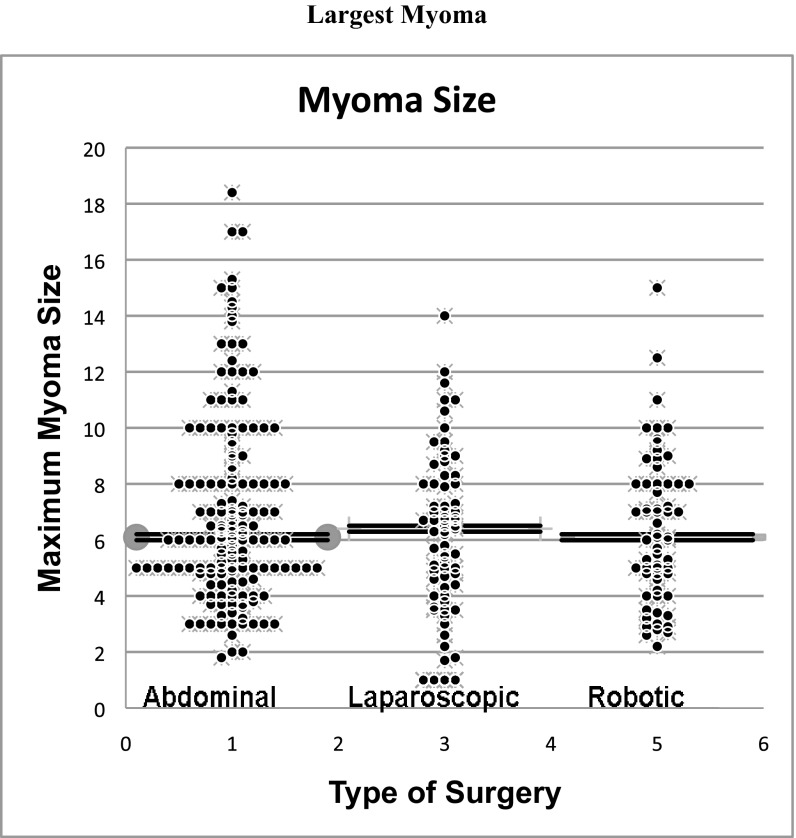
The characteristics of myomas between the operative groups were compared. There was no significant difference in the median size of the largest myoma removed robotically (6.1 cm; range, 1.8 to 18.4), laparoscopically (6.4 cm; range, 1 to 14), or abdominally (6.1 cm; range, 2.2 to 15; P=.13), although most myomas >10 cm were removed abdominally (Figure 1). The median aggregate weight of myoma removed abdominally (200g; range, 1.4 to 2682), however, was significantly (P<.005) larger than that of myomas removed laparoscopically (115g; range, 1 to 602) and robotically (129g; range, 9.4 to 935).
Figure 1.
Largest myoma on preoperative imaging, which was removed by abdominal, laparoscopic, or robotically assisted laparoscopic myomectomy.
DISCUSSION
Myomectomy is performed commonly for women with symptomatic fibroid uterus desiring uterine preservation and future fertility. Laparoscopic myomectomy was first reported in 1979.9 This technique has been performed safely and has consistently demonstrated advantages, such as decreased blood loss, shorter hospital stay, less postoperative disability, and comparable complications compared to abdominal myomectomy.10–17 Clinical outcomes for fertility and obstetrical outcomes are also comparable to abdominal myomectomy.18 Comparison of outcomes for laparoscopic and robotic-assisted laparoscopic myomectomy has demonstrated comparable clinical outcomes for blood loss, hospital stay, and complications despite longer robotic operative times in university hospitals and medical centers.6,7 The American College of Obstetricians and Gynecologist and the American Association of Gynecologic Laparoscopist have confirmed the advantages of laparoscopy over laparotomy. Despite advances in laparoscopic technique, as well as the advantages of laparoscopic myomectomy reported over 30 y, most gynecologic procedures are still performed through abdominal incisions.8,19
The technical skill required for excision of myoma and lack of surgeon experience are considered significant limiting factors to the wide acceptance of this technique.18,20 Technical advantages of robotic-assisted laparoscopic surgery may help overcome these challenges and perhaps improve the adoption of the laparoscopic technique.8,11 These advantages include 3-dimensional visualization, instrument articulation, improved dexterity, and the elimination of tremor and counterintuitive movements.21,22 Specifically, these advantages offer the community-based gynecologist greater facility with which to suture and surgically dissect laparoscopically. Specifically, this study demonstrated primary surgical outcomes of operative time, decreased hospital stay, and decreased estimated blood loss with robotic-assisted laparoscopic myomectomy that were consistent with published reports in university-based teaching hospitals and regional medical centers. These findings, coupled with the demonstrated advantages of robotic-assisted laparoscopic surgery, may improve the adaptation of this technique by general gynecologists desiring to offer a more minimally invasive approach to their patients in a community-based practice.
Robotic-assisted laparoscopy has been proposed as a way to overcome many of the technical challenges to traditional laparoscopy through improved imaging as well as enhanced dexterity of surgical instruments.8,11 While these characteristics have been demonstrated in university-based teaching hospitals and medical centers, this is the first comparison of abdominal, laparoscopic and RALM in a community hospital.10 This study demonstrated reduced blood loss and shorter hospital stay consistent with previously published reports. Additionally, the differences in operative times and comparable rates of complications in our community hospital were similar to those of university-based teaching hospitals and medical centers with experienced surgeons.
Strengths of this study include the large, continuous case series with a high rate of complete patient data sets in a single community hospital with access to all routes of surgery. Limitations of this study include all those inherent to the retrospective design. A statistical difference was demonstrated in clinical outcomes although the descriptive nature of the study results may reflect some differences from the preselection process and individual patient characteristics. P values were reported, nonetheless, as a direct comparison to studies reported from medical centers and university-based hospitals.
Concerns over increased costs, operating times, and number of laparoscopic ports associated with robotic surgery continue to be addressed. New evidence suggests comparable costs and operating times for robotic-assisted laparoscopy compared with conventional laparoscopy, especially when performed by experienced robotic surgeons.6,23–25
CONCLUSION
Laparoscopic and robotic-assisted myomectomies performed in this community hospital demonstrated clinical outcomes consistent with those published from university-based teaching hospitals and medical centers in the hands of experienced laparoscopist. Further prospective randomized studies evaluating whether the same outcomes are observed with general gynecologists trained in robotic surgery are warranted. This is especially true in the community hospital setting. Regardless, robotic-assisted laparoscopic myomectomy offers a minimally invasive alternative for management of symptomatic myoma and may expand the adoption of the laparoscopic technique in the community hospital setting.
Contributor Information
Joseph M. Gobern, Department of Obstetrics and Gynecology, Walter Reed National Military Medical Center, Bethesda, MD, USA.
C. J. Rosemeyer, Department of Obstetrics and Gynecology, Walter Reed National Military Medical Center, Bethesda, MD, USA.
James F. Barter, Women's Health Specialist, Holy Cross Hospital, Silver Spring, MD, USA..
Albert J. Steren, Women's Health Specialist, Holy Cross Hospital, Silver Spring, MD, USA..
References:
- 1. Laughlin SK, Stewart EA. Uterine Leiomyomas: Individualizing the Approach to a Heterogenous Condition. Obstet Gynecol. 2011;117(2):396–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agdi M, Tulandi T. Minimally invasive approach for myomectomy. Semin Reprod Med. 2010;28(3):228–234 [DOI] [PubMed] [Google Scholar]
- 3. Bonney V. The techniques and results of myomectomy. Lancet. 1931;220:171–177 [Google Scholar]
- 4. Babaknia A, Rock JA, Jones HW., Jr Pregnancy success following abdominal myomectomy for infertility. Fertil Steril. 1978;30(6):644–647 [DOI] [PubMed] [Google Scholar]
- 5. Parker WH. Uterine myomas: management. Fertil Steril. 2007;88(2):255–271 [DOI] [PubMed] [Google Scholar]
- 6. Bedient CE, Magrina JF, Noble BN, Kho RM. Comparison of robotic and laparoscopic myomectomy. Am J Obstet Gynecol. 2009;201(6):566.e1–5 [DOI] [PubMed] [Google Scholar]
- 7. Nezhat C, Lavie O, Hsu S, Watson J, Barnett O, Lemyre M. Robotic-assisted laparoscopic myomectomy compared with standard laparoscopic myomectomy–a retrospective matched control study. Fertil Steril. 2009;91(2):556–559 [DOI] [PubMed] [Google Scholar]
- 8. Payne TN, Pitter MC. Robotic-assisted surgery for the community gynecologist: can it be adopted? Clin Obstet Gynecol. 2011;54(3):391–411 [DOI] [PubMed] [Google Scholar]
- 9. Semm K. New methods of pelviscopy (gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy and adnectomy. Endoscopy. 1979;11(2):85–93 [DOI] [PubMed] [Google Scholar]
- 10. Advincula AP, Xu X, Goudeau S, 4th, Ransom SB. Robot-assisted laproscopic myomectomy versus abdominal myomectomy: a comparison of short-term surgical outcomes and immediate costs. J Minim Invasive Gynecol. 2007;14(6):698–705 [DOI] [PubMed] [Google Scholar]
- 11. Barakat EE, Bedaiwy MA, Zimberg S, Nutter B, Nosseir M, Falcone T. Robotic-assisted, laparoscopic, and abdominal myomectomy: a comparison of surgical outcomes. Obstet Gynecol. 2011;117(2):256–265 [DOI] [PubMed] [Google Scholar]
- 12. Falcone T, Bedaiwy MA. Minimally invasive management of uterine fibroids. Curr Opin Obstet Gynecol. 2002;14(4):401–407 [DOI] [PubMed] [Google Scholar]
- 13. Nezhat C, Nezhat F, Silfen SL, Schaffer N, Evans D. Laparoscopic myomectomy. Int J Fertil. 1991;36(5):275–280 [PubMed] [Google Scholar]
- 14. Miller CE, Johnston M. Laparoscopic myomectomy using ultrasonic dissection. Surg Technol Int. 1995;(4):227–233 [PubMed] [Google Scholar]
- 15. Mais V, Ajossa S, Guerriero S, Mascia M, Solla E, Melis GB. Laparoscopic versus abdominal myomectomy: a prospective, randomized trial to evaluate benefits in early outcome. Am J Obstet Gynecol. 1996;174(2):654–658 [DOI] [PubMed] [Google Scholar]
- 16. Ascher-Walsh CJ, Capes TL. Robot-assisted laparoscopic myomectomy is an improvement over laparotomy in women with a limited number of myomas. J Minim Invasive Gynecol. 2010;17(3):306–310 [DOI] [PubMed] [Google Scholar]
- 17. Nash K, Feinglass J, Zei C, Lu G, Mengesha B, Lewicky-Gaupp C, Lin A. Robotic-assisted laparoscopic myomectomy versus abdominal myomectomy: a comparative analysis of surgical outcomes and costs. Arch Gynecol Obstet. 2012;285(2):435–440 [DOI] [PubMed] [Google Scholar]
- 18. Sami WM, Heaton RL. The role of laparoscopic myomectomy in the management of uterine fibroids. Curr Opin Obstet Gynecol. 2011;23(4):273–277 [DOI] [PubMed] [Google Scholar]
- 19. Matthews CA. Applications of robotic surgery in gynecology. J Womens Health (Larchmt). 2010;19(5):863–867 [DOI] [PubMed] [Google Scholar]
- 20. Lee CL, Wang CJ. Laparoscopic myomectomy. Taiwan J Obstet Gynecol. 2009;48(4):335–341 [DOI] [PubMed] [Google Scholar]
- 21. Visco AG, Advincula AP. Robotic gynecologic surgery. Obstet Gynecol. 2008;112:1369–1384 [DOI] [PubMed] [Google Scholar]
- 22. Robotic-assisted surgery ACOG Technology Assessment in Obstetrics and Gynecology No. 6. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114:1153–1155 [DOI] [PubMed] [Google Scholar]
- 23. Shashoua AR, Gill D, Locher SR. Robotic-assisted total laparoscopic hysterectomy versus conventional total laparoscopic hysterectomy. JSLS. 2009;13(3):364–369 [PMC free article] [PubMed] [Google Scholar]
- 24. Jonsdottir GM, Jorgensen S, Cohen SL, et al. Increasing minimally invasive hysterectomy: effect on cost and complications. Obstet Gynecol. 2011;117(5):1142–1149 [DOI] [PubMed] [Google Scholar]
- 25. Bush A, Morris SN, Millham FH, Isaacson KB. Women's preferences for minimally invasive incisions. J Minim Invasive Gynecol. 2011;18(5)L:640–643 [DOI] [PubMed] [Google Scholar]