This report suggests that laparoscopic ureteral reimplantation offers an alternative surgical approach to open surgery after distal ureteral injuries.
Keywords: Laparoscopy, Ureteroneocystostomy, Ureteral reimplantation, Hysterectomy
Abstract
Objectives:
To examine the feasibility of early laparoscopic ureteroneocystostomy for ureteral obstruction due to hysterectomy injury.
Methods:
We retrospectively reviewed a 10-y experience from 2 institutions in patients who underwent early (<30 d) or late (>30 d) laparoscopic ureteroneocystostomy for ureteral injury after hysterectomy. Evaluation of the surgery included the cause of the stricture and intraoperative and postoperative outcomes.
Results:
A total of 9 patients with distal ureteral injury after hysterectomy were identified. All injuries were identified and treated as early as 21 d after hysterectomy. Seven of 9 patients underwent open hysterectomy, and the remaining patients had vaginal and laparoscopic radical hysterectomy. All ureteroneocystostomy cases were managed laparoscopically without conversion to open surgery and without any intraoperative complications. The Lich-Gregoir reimplantation technique was applied in all patients, and 2 patients required a psoas hitch. The mean operative time was 206.6 min (range, 120–280 min), the mean estimated blood loss was 122.2 cc (range, 25–350 cc), and the mean admission time was 3.3 d (range, 1–7 d). Cystography showed no urine leak when the ureteral stent was removed at 4 to 6 wk after the procedure. Ureteroneocystostomy patency was followed up with cystography at 6 mo and at least 10 y after ureteroneocystostomy.
Conclusion:
Early laparoscopic ureteral reimplantation may offer an alternative surgical approach to open surgery for the management of distal ureteral injuries, with favorable cosmetic results and recovery time from ureteral obstruction due to hysterectomy injury.
INTRODUCTION
Hysterectomy is the most frequent gynecologic procedure for benign uterine disease.1 Unfortunately, because of the close proximity of the ureter to the cervix and uterine artery, unintended injury to the ureter may occur during this procedure. Ureteral injury may occur because of suture, clip, or staple ligation; crush injury; or electrocautery thermal spread, which can lead to the development of hydronephrosis, loss of renal function, fistula formation, and possible sepsis if not detected intraoperatively.2 Optimal management of distal ureteral stricture includes resection of the stenosis, spatulation of the healthy ureter, and tension-free ureteroureteral anastomosis with optimal ureterovesical mucosa apposition. Traditionally, these procedures have been performed by an open approach after the acute phase has passed (>6 wk), but laparoscopy has emerged as a minimally invasive option.3–5
In 1992 Nezhat and Nezhat6 reported the first laparoscopic ureteroureterostomy for the repair of a ureteral injury during a laparoscopic gynecologic procedure. Since then, laparoscopic ureteroneocystostomy has been reported, but the reconstructive steps may be challenging to surgeons. We evaluated a 10-y multi-institutional experience with early and late laparoscopic ureteral reimplantation in patients who were treated for distal ureteral injury after hysterectomy performed by surgeons (F.J.K. and M.T.-M.) at 2 institutions.
MATERIALS AND METHODS
We retrospectively reviewed the charts of patients who underwent laparoscopic ureteroneocystostomy after hysterectomy from 2002 to 2011 at Denver Health Medical Center (Denver, CO, USA) and the ABC Medical School (São Paulo, Brazil). Data collection included demographics, cause of the stricture, and intraoperative and postoperative outcomes.
Surgical Technique
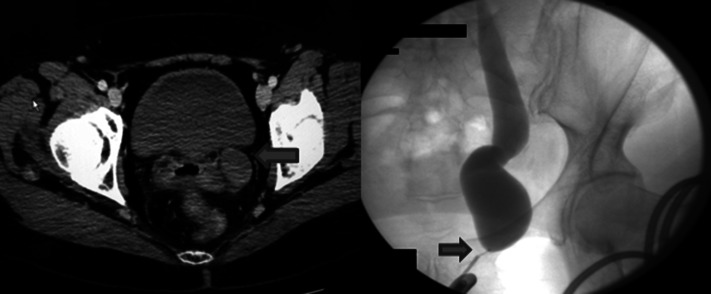
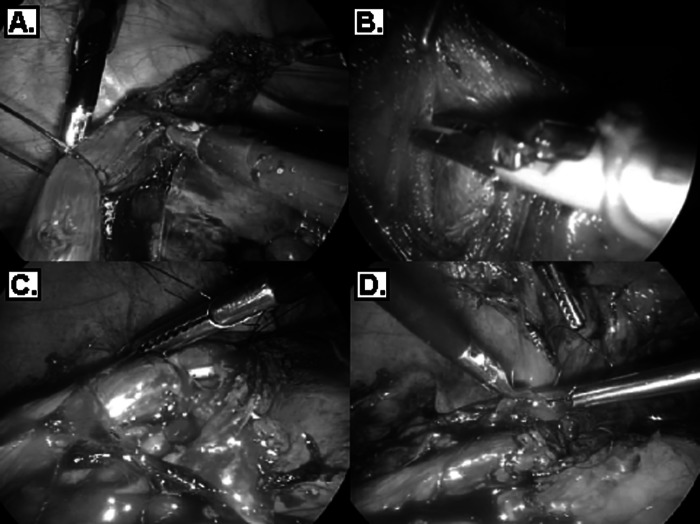
Identification of the ureteral stricture was made preoperatively with computed tomography (CT)–intravenous pyelography and then intraoperatively with retrograde ureteropyelography (Figure 1). A council-tip Foley catheter (Bard, Covington, GA) was then placed, followed by a 5-mm ureteral catheter, and then a Superstiff guidewire (Boston Scientific, Natick, MA) catheter was inserted. Laparoscopic ureteroneocystostomy was performed in a transperitoneal manner with the Lich-Gregoir technique. The Kocher maneuver was performed after incision of the line of Toldt, and the ureter was released, dissected above the stenotic area, clipped distally, and sectioned (Figure 2A). The bladder was mobilized to achieve a good length up to the incised ureter without requiring insufflation of the bladder. By use of laparoscopic scissors, the bladder was incised and dissected with good mucosa exposure (Figure 2B). Mucosa-mucosa anastomosis was performed with absorbable No. 3.0 Polysorb suture (Johnson & Johnson, New Brunswhick, NJ) starting at the 6-o'clock position after spatulation of the distal ureter (Figure 2C). Before the ureterovesical anastomosis was finalized, a ureteral stent was placed with assistance from the Superstiff guidewire, and the bladder anastomotic site was tested for watertightness with irrigation and filling up the bladder with 250 cc of sterile saline solution (Figure 2D).
Figure 1.
Left distal hydronephrosis of left ureter at 2 y after hysterectomy (CT scan and ascendant pyelogram). (Arrow) stenosis of the ureter.
Figure 2.
(A) Resection of stenotic area. (B) Mucosal exposure of the detrusor muscle of the bladder. (C) Ureterovesical anastomosis after ureteral spatulation. (D) Suture of muscular layer of the bladder wall (detrusor).
A Foley catheter was removed 1 wk postoperatively. Cystography was performed at 4 to 6 wk at the time the double-J ureteral stent was removed if no extravasation was identified. CT intravenous urography was performed and serum creatinine levels were obtained at 3 mo to reassess the ureteroneocystostomy. Renal nuclear (Mercaptoacetyltriglycine) scans were ordered for patients who had questionable decreased renal function postoperatively.
RESULTS
A total of 9 patients with ureteral stricture due to iatrogenic injury from hysterectomy were identified. A percutaneous nephrostomy tube was placed in 4 patients (44.4%) before the ureteroneocystostomy. Interestingly, in 1 of these patients, the ureter was medially deviated because of previous procedures (Figure 3). In the 5 patients who did not have urinary diversion, hydronephrosis and ureteral obstruction with ipsilateral flank pain developed at 7 d and 1, 2, 3, and 13 y after hysterectomy. Ureterovaginal fistula developed in 2 patients with long-term obstruction. Preoperative creatinine levels were normal in all patients, ranging from 0.5 mg/dL to 0.9 mg/mL. The mean patient age was 48.5 y (range, 30–76 y).
Figure 3.

Intraoperative pyelogram of ureter deviated past midsagittal plane.
Table 1 shows patient demographics and preoperative data. Seven patients (77.8%) underwent open hysterectomy: The procedure was performed in 5 patients (71.4%) because of myoma and in 1 patient (14.3%) because of cervical cancer; moreover, 1 patient (14.3%) underwent emergent laparotomy and hysterectomy for bleeding due to uterine hemorrhage and failure to coagulate after vaginal delivery. Vaginal hysterectomy was performed in 1 patient (11.1%), whereas 1 patient (11.1%) underwent laparoscopic radical hysterectomy.
Table 1.
Patient Demographics and Stricture Etiology
| Patient No. | Age (y) | BMIa (kg/m2) | ASA | Side | Ureteral Position | Etiology |
|---|---|---|---|---|---|---|
| 1 | 58 | 28.2 | 2 | Left | distal | OHa, myoma |
| 2 | 46 | 32.8 | 2 | Right | distal | OH, myoma |
| 3 | 50 | 31.2 | 2 | Left | distal | OH, myoma |
| 4 | 43 | 21.5 | 3 | Right | distal | OH, myoma |
| 5 | 42 | 35.1 | 3 | Right | distal | ORHa, cervical cancer |
| 6 | 76 | 20.7 | 3 | Left | distal | VHa, myoma |
| 7 | 30 | 25.3 | 1 | Right | distal | OH, myoma |
| 8 | 55 | 18.9 | 1 | Left | distal | LRHa, cervical cancer |
| 9 | 40 | 20.5 | 1 | Left | distal | OH, uterine atony |
ASA = American Society of Anesthesiologists class; BMI = body mass index; LRH = laparoscopic radical hysterectomy; OH = open hysterectomy; ORH = open radical hysterectomy; VH = vaginal hysterectomy.
All ureteroneocystostomies were successfully performed by a laparoscopic approach without conversion to open surgery. Surgical outcomes are summarized in Table 2. The mean operative time was 206.6 min (range, 120–280 min), and the mean estimated blood loss was 122.2 cc (range, 25–350 cc). The increased operating room time was because of intraperitoneal adhesions from previous surgery including hysterectomy. The mean hospital stay was 3.3 d (range, 1–7 d). Two patients were hospitalized for 1 wk: 1 patient because of a blood transfusion reaction (the patient who underwent emergent hysterectomy and was repaired 7 d thereafter) and another as a result of a complicated urinary tract infection. CT cystography or voiding cystography showed no urine leak and a patent ureteroneocystostomy in all patients. In 2 cases the bladder received a psoas hitch to allow for a tension-free ureterovesical anastomosis. Postoperative creatinine levels were normal for all patients (range, 0.7–1.1 mg/dL). In 1 patient with a psoas hitch, lower-grade ureterovesical reflux was observed without clinical repercussion on renal function (Figure 4).
Table 2.
Surgical Outcomes
| Patient No. | ORTa (min) | EBLa (mL) | Procedure | Hospital Stay (d) | Complications |
|---|---|---|---|---|---|
| 1 | 250 | 250 | Ureteroneocystostomy | 3 | No |
| 2 | 240 | 150 | Ureteroneocystostomy | 7 | Transfusion reaction |
| 3 | 200 | 25 | Ureteroneocystostomy | 2 | No |
| 4 | 280 | 25 | Ureteroneocystostomy | 3 | No |
| 5 | 220 | 100 | Ureteroneocystostomy and psoas hitch | 3 | No |
| 6 | 130 | 50 | Ureteroneocystostomy | 2 | No |
| 7 | 120 | 50 | Ureteroneocystostomy | 1 | No |
| 8 | 240 | 350 | Ureteroneocystostomy and psoas hitch | 7 | Urinary tract infection |
| 9 | 180 | 100 | Ureteroneocystostomy | 2 | No |
EBL = estimated blood loss; ORT = operative time.
Figure 4.

Postoperative aspect of CT cystogram after psoas hitch with low-grade reflux.
DISCUSSION
Iatrogenic ureteral injury is a grave complication that can occur during abdominal or pelvic surgeries. Ureteral injuries have a documented incidence of 0.3% to 1.5%.7 Fortunately, ureteral injuries from open hysterectomy are also rare and occur in 0.2% to 0.4% of these procedures.8,9 Leonard et al.1 published a series of 1300 laparoscopic hysterectomies, with a ureteral injury rate of 0.3%, comparable with that in the published open series.
Unfortunately, our patients were diagnosed after the hysterectomy. Five patients had the repair within 30 d of injury, showing that early repair is feasible and efficient contrary to the dogma that one should wait 3 to 6 mo after injury for repair. Pathology reports from the injury sites confirmed fibrotic tissue and complete obliteration of the ureteral lumen.
Open surgical procedures have good long-term results with reported success rates >80%.2 However, open surgical procedures are associated with a longer hospital stay, extra blood loss, and the need for additional pain medication.4 Nevertheless, minimally invasive techniques have gained in popularity in recent years.10–20 Since the first report of a laparoscopic ureteroneocystostomy was published by Nezhat and Nezhat6 in 1992, only a few reports with small sample sizes have been recorded in the literature. Moreover, these reports were not limited only to post-hysterectomy ureteral injuries and did not address the optimal timing of the ureteral reimplantation. Our series focused on patients who required ureteroneocystostomy after hysterectomy only. In addition, even more extensive ureteric defects were successfully repaired with the psoas-hitch technique and Boari flap laparoscopically.
Recently, robot-assisted techniques have been described for ureteral reimplantation. However, robot-assisted ureteral reimplantation in adult patients is not a universal reality because of the cost and inexperience of surgeons in countries outside of the United States and a few Asian and European countries. The laparoscopic approach certainly can be performed in most practices where a robot is not available.
This study has several limitations. It is retrospective and limited by the small sample of patients. However, the feasibility of performing the procedure early may offer benefits to the patients who often may have a percutaneous nephrostomy tube placed and may decrease the anxiety level of the surgeon who caused the injury.
CONCLUSION
The laparoscopic technique of early ureteral reimplantation for the repair of ureteral obstruction due to hysterectomy injury may be challenging, but it is feasible. Our 10-y experience showed that early laparoscopic ureteroneocystostomy offers similar success rates compared with open procedures, decreasing issues associated with delayed repair of injuries.
Contributor Information
Alexandre Pompeo, Division of Urology, Department of Surgery, Denver Health Medical Center and University of Colorado Health Sciences Center, Denver, CO, USA.; Division of Urology, ABC Medical School, São Paulo, Brazil.
Wilson R. Molina, Division of Urology, Department of Surgery, Denver Health Medical Center and University of Colorado Health Sciences Center, Denver, CO, USA..
David Sehrt, Division of Urology, Department of Surgery, Denver Health Medical Center and University of Colorado Health Sciences Center, Denver, CO, USA..
Marcos Tobias-Machado, Division of Urology, ABC Medical School, São Paulo, Brazil..
Renato M. Mariano Costa, Jr, Division of Urology, ABC Medical School, São Paulo, Brazil..
Antonio Carlos Lima Pompeo, Division of Urology, ABC Medical School, São Paulo, Brazil..
Fernando J. Kim, Division of Urology, Department of Surgery, Denver Health Medical Center and University of Colorado Health Sciences Center, Denver, CO, USA.; Tony Grampsas Cancer Institute, Denver, CO, USA.
References:
- 1. Leonard F, Fotso A, Borguese B, Chopin N, Foulot H, Chapron C. Ureteral complications from laparoscopic hysterectomy indicated for benign uterine pathologies: a 13-year experience in a continuous series of 1300 patients. Hum Reprod. 2007;22(7):2006–2011 [DOI] [PubMed] [Google Scholar]
- 2. Sakellariou P, Protopapas AG, Voulgaris Z, et al. Management of ureteric injuries during gynecological operations: 10 years experience. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):179–184 [DOI] [PubMed] [Google Scholar]
- 3. Simmons MN, Gill IS, Fergany AF, Kaouk JH, Desai MM. Laparoscopic ureteral reconstruction for benign stricture disease. Urology. 2007;69(2):280–284 [DOI] [PubMed] [Google Scholar]
- 4. Rassweiler JJ, Gözen AS, Erdogru T, Sugiono M, Teber D. Ureteral reimplantation for management of ureteral strictures: a retrospective comparison of laparoscopic and open techniques. Eur Urol. 2007;51(2):512–522 [DOI] [PubMed] [Google Scholar]
- 5. Modi P, Goel R, Dodiya S. Laparoscopic ureteroneocystostomy for distal ureteral injuries. Urology. 2005;66(4):751–753 [DOI] [PubMed] [Google Scholar]
- 6. Nezhat C, Nezhat F. Laparoscopic repair of ureter resected during operative laparoscopy. Obstet Gynecol. 1992;80(3 Pt 2):543–544 [PubMed] [Google Scholar]
- 7. Parpala-Sparman T, Paananen I, Santala M, Ohtonen P, Hellstrom P. Increasing numbers of ureteric injuries after the introduction of laparoscopic surgery. Scand J Urol Nephrol. 2008;42(5):422–427 [DOI] [PubMed] [Google Scholar]
- 8. Harkki-Siren P, Sjoberg J, Mäkinen J, et al. Finnish national register of laparoscopic hysterectomies. A review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt 1):118–122 [DOI] [PubMed] [Google Scholar]
- 9. Mäkinen J, Johansson J, Tomas C, et al. Morbidity of 10110 hysterectomy by type of approach. Hum Reprod. 2001;16(7):1473–1478 [DOI] [PubMed] [Google Scholar]
- 10. Phipps JH, Tyrrell NJ. Transilluminating ureteric stents for preventing operative ureteric damage. Br J Obstet Gynaecol. 1992;99(1):81. [DOI] [PubMed] [Google Scholar]
- 11. Paulson JD. Laparoscopically assisted vaginal hysterectomy. A protocol for reducing urinary tract complications. J Reprod Med. 1996;41(9):623–628 [PubMed] [Google Scholar]
- 12. Ostrzenski A, Radolinski B, Oatrzenska KM. A review of laparoscopic ureteral injury in pelvic surgery. Obstet Gynecol Surv. 2008;58(12):794–799 [DOI] [PubMed] [Google Scholar]
- 13. Ehrlich RM, Gershman A, Fuchs G. Laparoscopic vesicoureteroplasty in children: initial case reports. Urology. 1994;43(2):255–261 [DOI] [PubMed] [Google Scholar]
- 14. Reddy PK, Evans RM. Laparoscopic ureteroneocystostomy. J Urol. 1994;152(6 Pt 1):2057–2059 [DOI] [PubMed] [Google Scholar]
- 15. Nezhat CH, Malik S, Nezhat F, Nezhat C. Laparoscopic ureteroneocystostomy and vesicopsoas hitch for infiltrative endometriosis. JSLS. 2004;8(1):3–7 [PMC free article] [PubMed] [Google Scholar]
- 16. Modi P, Gupta R, Rizvi SJ. Laparoscopic ureteroneocystostomy and psoas hitch for post hysterectomy ureterovaginal fistula. J Urol. 2008;180(2):615–617 [DOI] [PubMed] [Google Scholar]
- 17. Fugita OE, Dinlenc C, Kavoussi L. The laparoscopic Boari flap. J Urol. 2001;166(1):51–53 [PubMed] [Google Scholar]
- 18. Smith RP, Oliver JL, Peters CA. Pediatric robotic extravesical ureteral reimplantation: comparison with open surgery. J Urol. 2011;185(5):1876–1881 [DOI] [PubMed] [Google Scholar]
- 19. Marchini GS, Hong YK, Minnillo BJ, et al. Robotic assisted laparoscopic ureteral reimplantation in children: case matched comparative study with open surgical approach. J Urol. 2011;185(5):1870–1875 [DOI] [PubMed] [Google Scholar]
- 20. Kasturi S, Sehgal SS, Christman MS, Lambert SM, Casale P. Prospective long-term analysis of nerve sparing extravesical robotic assisted laparoscopic ureteral reimplantation. Urology. 2012;79(3):680–683 [DOI] [PubMed] [Google Scholar]