An unusual collection of fluid in the perihepatic space needs to be investigated for abscess in patients with a remote history of cholecystectomy.
Keywords: Laparoscopic cholecystectomy, Retained gallstones, Abdominal abscess, Gallstones
Abstract
Background:
A common intraoperative complication during laparoscopic cholecystectomy is gallbladder perforation with spillage of gallstones. The undesirable consequence of spilled gallstones is the formation of abscesses months or years after an operation.
Case Description:
Our clinical report describes an intraabdominal abscess formation in an 82-year-old man that developed 8 years after a laparoscopic cholecystectomy. A computed tomography scan of the abdomen showed an elongated fluid collection in the right abdominal compartment musculature at the level of the internal oblique muscle. Abdominal ultrasonography confirmed a large fluid collection, with 2 echogenic masses in the dependent portion. Incision and drainage of the abscess were performed, and 2 gallstones were found.
Conclusion:
Any unusual collection of fluid in the perihepatic space and abdominal wall in the area of the surgical incision in a patient with a remote history of cholecystectomy should be evaluated for abscess related to retained gallstone. Early abscess formation is usually diagnosed and treated by the surgeon. However, the late manifestation might be a clinical problem seen in the primary care physician's office. Therefore, the primary care physician should incorporate diagnosis of gallstone-related abscess in patients with abdominal abscess formation of unknown etiology.
INTRODUCTION
The beginning of the era of laparoscopic cholecystectomy started on September 12, 1985 in Germany by Prof DrMed Erich Muhe (or since its introduction in France in 1987 by Dubois et al).1 Laparoscopic cholecystectomy is now considered the gold standard of surgical intervention for the treatment of symptomatic cholelithiasis and gallbladder disease.2,3
This commonly performed and well-established minimally invasive surgery is still associated with adverse effects and complications. The most feared complication of laparoscopic cholecystectomy is injury to the common bile duct. The initial high occurrence rate (1.9%) of this type of injury during the early era of laparoscopic surgery has since decreased and stabilized to 0.5%.4,5 Surgeons take precautions to avoid and detect this type of injury by using the “critical view” technique and intraoperative cholangiography.5 Other common complications include retained common bile duct stones, bile leaks, and superficial wound infections. The complications that occur more often with laparoscopic cholecystectomy are perforations of the gallbladder during laparoscopic surgery and spillage of gallstones.6 In their review of the scientific literature, Papasavas et al7 found that in contrast to 127 case reports of complications secondary to dropped gallstones during laparoscopic cholecystectomy, only 2 such events have been described for open cholecystectomies since the year 1963. This is obviously a matter of concern because additional studies reported incidents of gallbladder perforation during laparoscopic surgery varying from 10% to 40%, a 7.3% incidence of gallstone spillage, and an estimated 33% of unretrieved gallstones.8–13,14
In rare instances, postoperative residual gallstones can contribute to associated abscess formation.14 The formation of abscesses occurs in remote locations to the site of the gallbladder fossa, making diagnosis and causation difficult to establish after the index operation.14 Most of these abscesses have been reported to manifest during the first 4 to 9 months after the initial operation, whereas only a few can be detected as late as 15 years after laparoscopic cholecystectomy.15 In our case, the time between laparoscopic cholecystectomy and abdominal wall abscess formation was 8 years.
CASE DESCRIPTION
An 82-year-old man was admitted to the clinic with complaints of right upper quadrant abdominal pain and soreness in the right subcostal area lasting 2 months. He described the pain as constant and rated it a 5 on a 10-point scale, where 10 represents the worse pain ever. He denied any nausea, vomiting, fever, or chills. His past medical history was significant for hypertension, coronary artery disease, dyslipidemia, Crohn disease, diverticulosis, osteoarthritis, benign prostatic hypertrophy, depression, sleep apnea, and environmental allergies. Eight years prior, he had undergone an uncomplicated laparoscopic cholecystectomy with intraoperative cholangiography. The medical records and operative report were reviewed and there was no description of gallbladder perforation or spillage of stones. Electrocautery and blunt dissection were used to mobilize the gallbladder, and an Endobag was used for gallbladder removal.
On physical examination, the patient's pulse rate was 72 bpm, blood pressure was 110/60 mm Hg, temperature was 97.6°F, and respiratory rate was 16 breaths/minute. On palpation of the abdomen, the patient indicated right subcostal tenderness.
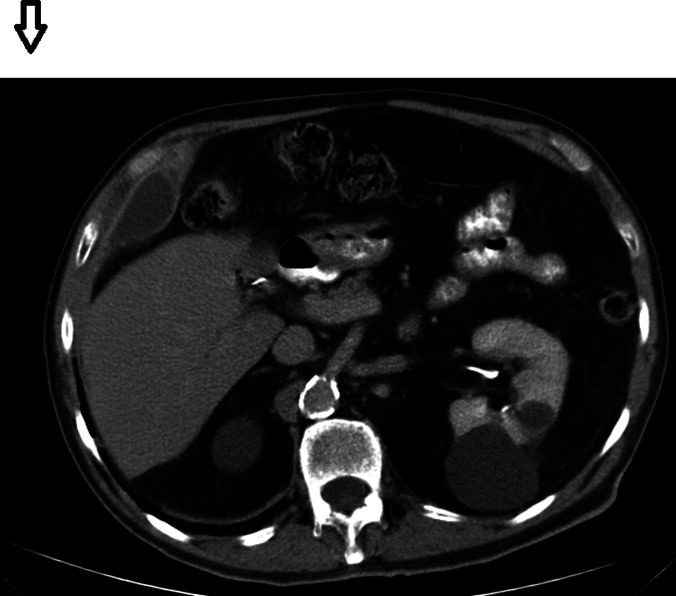
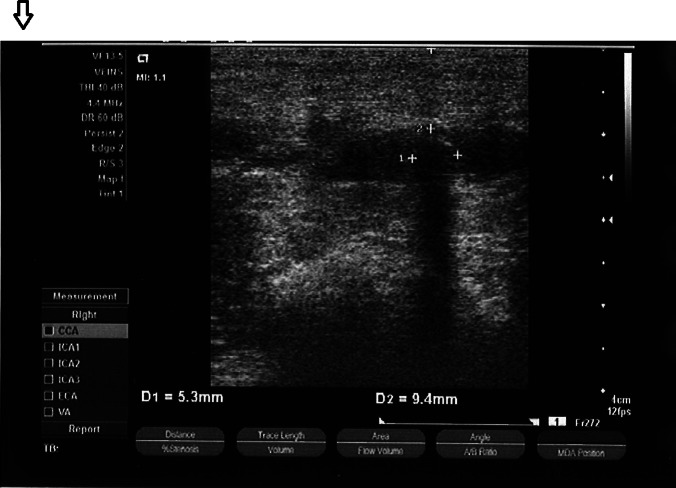
The initial laboratory tests revealed a hemoglobin level of 14.3g/dL and white blood cell count of 10.5 × 1000 cells/μL. A computed tomography scan of the abdomen performed both before and after intravenous administration of contrast showed an elongated fluid collection with an enhancing mature wall under the right abdominal musculature compartment (Figure 1). The fluid collection was elongated in the cephalocaudal plane and measured 11 cm in height, 8 cm in maximal depth, and 3 cm in width (Figure 2). Ultrasonography of the right upper quadrant of the abdomen performed in the clinic showed a large volume of fluid collection 6 cm in length and 2 cm in depth, extending from the subdiaphragmatic space toward the iliac wing on the right side. Ultrasonography also revealed 2 echogenic structures on the dependent portion of the cavity with posterior shadowing (Figure 3), one of which measured 9.4 × 5.3 mm.
Figure 1.
Gallstone-related abdominal abscess. Computed tomography depicting right flank fluid collection with surrounding inflammatory changes.
Figure 2.
Gallstone-related abdominal abscess. Computed tomography image of the abdominal abscess.
Figure 3.
Gallstone-related abdominal abscess. Ultrasonographic study showing a gallstone in the abscess cavity with typical posterior shadowing.
A diagnosis of abdominal wall abscess was suspected, and ultrasonography-guided aspiration was performed in the clinic. The aspiration returned 70 mL of white purulent material. A Gram stain of the collected fluid showed 1+ white blood cells, and the culture did not grow any organisms after 3 days. Two weeks later, incision and drainage of the abdominal wall abscess were performed with the patient under general anesthesia at the hospital. Ultrasonography was used to identify the area of the abscess on the right upper abdominal quadrant, which was approximately 2 cm deep, 8 cm wide, and 10 cm long. In the dependent portion of this space, 2 shadowing 5-mm objects were seen. In this area, the incision was made down to the subcuticular tissue, and the muscle of the abdominal wall was split to enter the abscess cavity. A collection of white pus was seen and evacuated with a suction device. Two stones were found and one was sent for pathologic examination. The other remained with the suction material. The cavity was irrigated with saline solution, and a 19-Fr Blake drain was placed in the most dependent part of the abscess. The pathology report of the stone described a single, medium, orange/tan irregular calculus, with a 44-mg mass and a size of 5 mm to 9 mm, that was composed primarily of cholesterol.
There were no complications from the surgery, and the patient was discharged home on the same day of the operation. On the first clinic follow-up visit, 5 days postoperatively, the drain was removed. One month later, the patient remained in good condition without any complaints. During the same visit, abdominal ultrasonography was performed and revealed a small amount of fluid in the abdominal wall.
DISCUSSION
Gallbladder perforations followed by bile leak and gallstone spillage are potential intraoperative events. However, complications caused by gallstone spillage are rare.9 These complications differ in manifestation, location, and onset of symptoms after laparoscopic cholecystectomy.
The most frequent complication of residual gallstones after cholecystectomy is abscess formation.16–18 The abscess location includes the intraperitoneal and extraperitoneal spaces. The most common areas of intraperitoneal abscesses are in the subhepatic and subphrenic spaces.14 Extraperitoneal locations of infections include abdominal wall ports and incision sites.14
Abscess formation caused by intraoperative spilled gallstones may occur weeks, months, or even years after cholecystectomy. In a retrospective review, the median and mean times from laparoscopic cholecystectomy until the first onset of symptoms were 3 months and 5.5 months, respectively.14 Brueggemeyer et al6 described a case of the right flank and retroperitoneal abscess after 72 months; however, their extensive review of the literature did not show any such case later than 12 months after laparoscopic cholecystectomy in 23 cases reported from 1992 to 1996. The longest reported abscess formation was 20 years after an open cholecystectomy.15 The longest interval documented between previous laparoscopic cholecystectomy and abscess formation was 15 years.15 In the case presented here, an abdominal wall abscess developed as a result of the 2 retained gallstones after a laparoscopic cholecystectomy performed 8 years earlier. In this particular patient, the late presentation of symptoms of the abscess formation could have been masked by the chronic abdominal pain related to colitis.
In laparoscopic cholecystectomies, perforation of the gallbladder may occur during grasping, traction, dissection, and extraction of the gallbladder. The quality of the gallbladder wall is also a contributing factor to gallbladder perforation. Currently, graspers are used to hold the gallbladder wall, and if they are used with too much traction, gallbladder perforation and spillage of stones can result.15 However, traction of the gallbladder during operation is indispensable for proper dissection from its bed. Therefore, the question remains whether it is best to replace graspers with a different gentler instrument with which adequate traction can be addressed for proper exposure.15 If perforation does occur during grasping and traction, the spilled material should be evacuated and the perforation site controlled by clips, by an endoloop, or by placing the grasper in such a way that it closes the perforation.6
During extraction, the gallbladder is squeezed through an abdominal incision, which can cause it to rupture and spill stones. For this reason, surgeons may use a sterile retrieval bag for extraction of the gallbladder. In addition, the retrieval bag facilitates manual breakdown of large gallstones that are often unable to be extracted through the small incisions made during laparoscopic cholecystectomy. The bag prevents spillage of the gallbladder contents into the abdominal cavity and the abdominal wall. If there is spillage of gallstones, it can be addressed during the operation with suitable surgical instruments, application of a suction-irrigation system, stone forceps, a disposable bag, or a combination of these.6
An outpatient ultrasonogram of the abdominal wall/cavity was helpful in the initial evaluation of a patient who was suspected of having an abscess related to possible retained gallstones. It is advisable that health care providers include this complication on their list of differential diagnoses when an unusual abdominal wall or cavity abscess develops in a postcholecystectomy patient.
CONCLUSION
Abdominal cavity abscess formation secondary to retained gallstones after cholecystectomy is a rare condition that can manifest itself many years after an initial operation. Gallbladder perforation and retained or unretrieved gallstones after spillage need to be carefully recorded for later review and for help with diagnosis of the complication in the future. Universal use of a protective bag for gallbladder removal might decrease the chance of a trocar site abscess and superficial site infection. Presence of the highly reflective echoes with posterior shadowing in the abscess cavity can be pathognomic for gallstone abscess in patients with known histories of cholecystectomy, especially those performed with the laparoscopic technique.
Contributor Information
Andrew Dobradin, Winter Park, Florida, USA..
Stephanie Jugmohan, Winter Park, Florida, USA..
Luis Dabul, Winter Park, Florida, USA..
References:
- 1. Dubois F, Icard P, Berthelot G, Levard H. Coeliscopic cholecystectomy. Preliminary report of 36 cases. Ann Surg. 1990;211(1):60–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Litynski GS. Highlights in the History of Laparoscopy. Frankfurt, Germany: Barbara Bernert Verlag; 1996:165–168 [Google Scholar]
- 3. Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg. 2007;193(1):73–78 [DOI] [PubMed] [Google Scholar]
- 4. Buddingh TK, Weersma R, Savenije RA, van Dam GM, Nieuwenhuijs V. Lower rate of major bile duct injury and increased intraoperative management of common bile duct stones after implementation of routine intraoperative cholangiography. J Am Coll Surg. 2011;213(2):267–274 [DOI] [PubMed] [Google Scholar]
- 5. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101–125 [PubMed] [Google Scholar]
- 6. Brueggemeyer M, Saba A, Thibodeaux L. Abscess formation following spilled gallstones during laparoscopic cholecystectomy. JSLS. 1997;1(2):145–152 [PMC free article] [PubMed] [Google Scholar]
- 7. Papasavas PK, Caushaj PF, Gagné DJ. Spilled gallstones after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2002;12(5):383–386 [DOI] [PubMed] [Google Scholar]
- 8. Schäfer M, Suter C, Klaiber C, Wehrli H, Frei E, Krähenbühl L. Spilled gallstones after laparoscopic cholecystectomy. A relevant problem? A retrospective analysis of 10,174 laparoscopic cholecystectomies. Surg Endosc. 1998;12(4):305–309 [DOI] [PubMed] [Google Scholar]
- 9. Memon MA, Deeik RK, Maffi TR, Fitzgibbons RJ., Jr The outcome of unretrieved gallstones in the peritoneal cavity during laparoscopic cholecystectomy. A prospective analysis. Surg Endosc. 1999;13(9):848–857 [DOI] [PubMed] [Google Scholar]
- 10. Rice DC, Memon MA, Jamison RL, et al. Long-term consequences of intraoperative spillage of bile and gallstones during laparoscopic cholecystectomy. J Gastrointest Surg. 1997;1(1): 85–91 [DOI] [PubMed] [Google Scholar]
- 11. Sarli L, Pietra N, Costi R, Grattarola M. Gallbladder perforation during laparoscopic cholecystectomy. World J Surg. 1999;23(11):1186–1190 [DOI] [PubMed] [Google Scholar]
- 12. Kimura T, Goto H, Takeuchi Y, et al. Intraabdominal contamination after gallbladder perforation during laparoscopic cholecystectomy and its complications. Surg Endosc. 1996;10(9):888–891 [DOI] [PubMed] [Google Scholar]
- 13. Diez J, Arozamena C, Gutierez L, et al. Lost stones during laparoscopic cholecystectomy. HPB Surg. 1998;11(2):105–108, discussion 108–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Woodfield JC, Rodgers M, Windsor JA. Peritoneal gallstones following laparoscopic cholecystectomy. Surg Endosc. 2004;18(8):1200–1207 [DOI] [PubMed] [Google Scholar]
- 15. Arishi AR, Rabie ME, Khan MS, et al. Spilled gallstones: the source of an enigma. JSLS. 2008;12(3):321–325 [PMC free article] [PubMed] [Google Scholar]
- 16. Horton M, Florence MG. Unusual abscess patterns following dropped gallstones during laparoscopic cholecystectomy: etiology and sequelae. Am J Surg. 1998;175(5):375–379 [DOI] [PubMed] [Google Scholar]
- 17. Whiting J, Welch NT, Hallissey MT. Subphrenic abscess caused by gallstones “lost” at laparoscopic cholecystectomy one year previously: management by minimally invasive techniques. Surg Laparosc Endosc. 1997;7(1):77–78 [PubMed] [Google Scholar]
- 18. Wilton PB, Andy OJ, Jr, Peters JJ, Thomas CF, Patel VS, Scott-Conner CE. Laparoscopic cholecystectomy. Leave no (spilled) stone unturned. Surg Endosc. 1993;7(6):537–538 [DOI] [PubMed] [Google Scholar]