This report suggests that iatrogenic colon perforations in a prepped colon can be managed with endoclip closure.
Keywords: Colonic submucosal lesions, Perforation, Therapeutic colonoscopy, Endoclip
Abstract
Background and Objective:
Endoscopic removal of large colonic submucosal lesions can lead to a higher risk of perforation. Although not as common following diagnostic and therapeutic colonoscopy, it does occur more often following therapeutic colonoscopy. We present a case of a large submucosal mass excised endoscopically, resulting in a large perforation that was closed using endoclips. While endoclips are typically used for smaller perforations, we have found that they can be used safely on a larger defect.
Methods:
A 68-y-old woman presented with a 2.9-cm benign submucosal mass found in the hepatic flexure. It was removed via endoscopic polypectomy, leaving a perforation of 3cm x 3cm. The perforation was closed with endoscopic clips.
Results:
Histology of the specimen showed clear margins. At 4-wk follow-up, the patient had no complications. A colonoscopy at 6-mo follow-up showed only a scar at the procedure site with no complaints.
Conclusions:
Large iatrogenic colonic perforations can be managed successfully using endoclips, particularly in a prepped colon.
INTRODUCTION
Surgical resection has been the mainstay of treatment for large colonic lesions. Unfortunately, even with the introduction of laparoscopy, significant morbidity still exists. Endoscopic removal of large benign colonic submucosal lesions has been successfully performed, although it brings with it an increased risk of bleeding and perforation. In fact, reports show significant operative morbidity (36%) and mortality (7%).1 Traditionally, these complications have been addressed with a laparotomy,1 but recently laparoscopic2 and endoscopic techniques3,4 have been used successfully to close perforations.
The incidence of colonic perforation following colonoscopy can vary between 0.03% and 2%.4–6 Perforation rates increases with therapeutic interventions7 and the size of the polyp.6 We present a case of a large submucosal mass that was excised endoscopically, resulting in a 3-cm x 3-cm perforation that was closed using endoclips. Typically, these clips are used for smaller perforations2; however, we have found that they can be used safely on a larger defect. Endoclips have been used to clip a vessel in a bleeding ulcer or to achieve hemostasis from the base of a polyp after polypectomy.
MATERIALS AND METHODS
A 68-y-old woman presented with a 3-cm mass at the hepatic flexure (Figure 1), which was found during a routine outpatient colonoscopy. The mass was submucosal and the overlying mucosa was ulcerated. The lesion was firm. Biopsy of the lesion showed colonic mucosa with inflammatory changes. A subsequent CT scan of the abdomen confirmed that it was a 3-cm submucosal mass with benign features. The patient was taken for planned endoscopic resection with primary closure. The operating room was on standby in the event the resulting defect could not be closed endoscopically. A snare polypectomy was successfully performed that resulted in a 3-cm perforation (Figure 2). Seven endoclips (Resolution Clip; Boston Scientific, Natick MA) were placed in order to seal the colotomy (Figure 3). A frozen section of the specimen showed a benign stromal neoplasm.
Figure 1.

Hepatic flexure mass as seen on colonoscopy.
Figure 2.

Perforation after Snare Polypectomy.
Figure 3.

Endoclips closing the perforation site.
RESULTS
A postprocedure abdominal X-ray revealed expected free air (Figure 4), and the patient was admitted for observation. On postprocedure day 1, the patient's examination was unremarkable. She was started on a clear liquid diet. On postprocedure day 2, she advanced to a soft diet and was discharged home.
Figure 4.
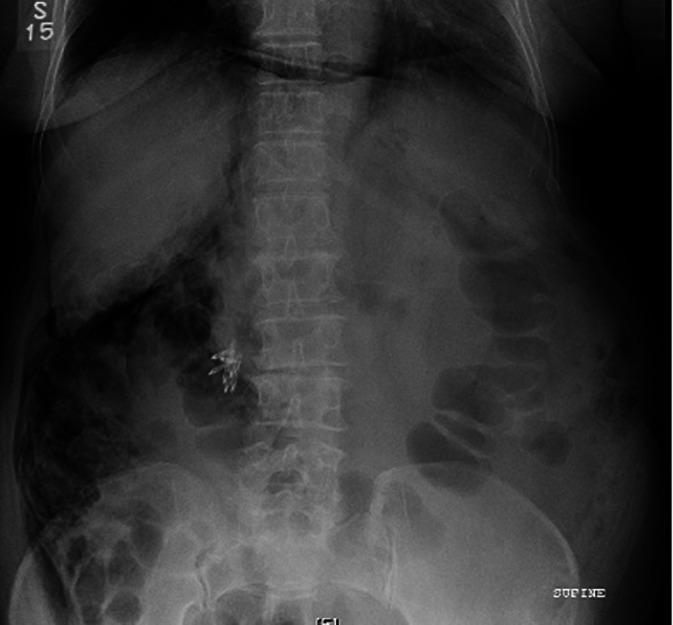
Postprocedure X-ray showing free air. Note the endoclips in the right upper quadrant.
Final pathology revealed a 2.9-cm submucosal leiomyoma with clear margins. The patient returned to the office 4 wk later without complaints. A colonoscopy at 6 mo showed a scar at the site.
DISCUSSION
Colonic leiomyomas are rare benign stromal tumors that can cause gastrointestinal bleeding,8 obstruction,9 and, in rare instances, progress to a sarcoma.10 Large benign colonic lesions have been removed by colonic resection and anastomosis, although recently they have been managed via an endoscopic mucosal resection11 and endoscopic polypectomy.12 The size, type (pedunculated or sessile), configuration, and site of the lesion all determine the type of procedure to be performed.
Pedunculated lesions13 and those over 2cm12 have been dealt with using endoloops or hemoclips. One report12 showed a 3.5-cm lipoma that was excised by endoscopic polypectomy with no complications. Endoloops can also be used to resect large colonic lipomas to prevent bleeding and perforation.14 Perforation risk increases with therapeutic colonoscopy,4,7,15 polyps > 2cm,16 in the elderly (>75yrs),15 and in female patients.17 Full-thickness endoscopic removal should be contemplated only after the lesion is proven benign either by imaging or histopathology, as a malignant lesion can potentially convert an early disease to stage 4 disease leading to bad prognosis.
Depending on the size of the perforation and clinical condition, treatment strategies vary. Small perforations can be managed conservatively with a success rate of 33% to 73%.18 Operative intervention can be managed by simple closure of the perforation15 or via a bowel resection with or without anastomosis.1 Colonic perforations have been dealt with laparoscopically leading to shorter hospital stay and decreased postoperative morbidity.19
Endoscopic closure of colonic perforation has been performed using endoclips, particularly when the perforation is < 1cm.4 Few authors3,20 have used the endoclips for perforations > 1 cm. Trecca et al.3 reported 2 perforations > 3cm that were managed using endoclips successfully. In both patients, 3 TriClips (Cook Medical, Bloomington, IN) were used. In our case, the perforation was 3cm in size, and 7 clips were used to close the defect. The patient was discharged on the second day. Of course, the number of clips used can vary, depending on the size of the perforation.3
Endoscopic closure of an iatrogenic colonic perforation at colonoscopy is feasible, because it is a prepped colon and there is minimal contamination. Closure should, however, be undertaken using minimal to no air insufflation.3 This helps with approximation of the edges and prevents fecal spillage. An experienced colonoscopist is the most important factor as the endoclip application can be technically challenging, and also depends on the site (hepatic flexure in our case) and size of the perforation.
Reports21,22 have shown clip closure to be successful in 69.2% to 92.6% of cases. Still, 2 of 27 patients who underwent clip application needed surgery, making it vitally important to monitor patients for complications following the procedure.21 We did not perform follow-up examination with X-ray for the clips3 or immediate colonoscopy,23 because the patient was clinically well. A follow-up endoscopy 6 mo postprocedure revealed a scar. Intravenous antibiotics and serial examinations are paramount in the postprocedure period to identify any leaks that can lead to peritonitis. Our patient made a remarkable recovery and was sent home in 2 d.
In our practice, therapeutic colonoscopy for large polyps is managed in the operating room with the patient anesthetized. We often perform diagnostic laparoscopy in suspicious cases to confirm that there is no leak at the site. CO2 colonoscopy is often performed to minimize intraabdominal free air, and to minimize distension of the colon, in the event that we need to convert to a laparoscopic procedure. Colonic perforations that are 3cm x 3cm following a benign excision can be closed using endoclips, which is possible in view of the prepped colon, with immediate identification of the perforation and with minimal contamination. Laparoscopic repair of an iatrogenic colon perforation has been shown to be feasible with decreased morbidity and shorter hospital stay compared to the open approach.24 Delayed diagnosis is associated with higher morbidity1 and can be dealt with by laparoscopy or with laparotomy.
To date, 3 cases have been reported in the literature with successful outcomes for perforations of 3cm3,20 that have been closed with endoclips. The case reported herein is about the largest perforation managed following a leiomyoma excision from the colon.
Immediate identification of the perforation is critical to using the endoscopic technique. Endoclip application can be challenging, and the success rate can depend on the colonoscopist, presence of fecal contamination, and the size and site of the perforation. An experienced colonoscopist with vast experience in therapeutic procedures is the most important factor for a successful outcome. Other factors are clean bowel with minimal contamination, the site of the perforation, and the availability of operating room facility. While endoscopic removal of 1-cm to 2-cm lesions has been reported, we believe this is the first reported case of an endoscopically resected 3-cm leiomyoma leading to perforation that was successfully repaired using endoclips. Immediate thorough evaluation of the polypectomy site for both bleeding and perforation is a good practice, particularly in high-risk cases and this avoids delayed diagnosis. Serial clinical examination following the procedure is very important to help identify any signs of sepsis. As endoscopic technology continues to evolve, and its use increases, we believe this method will become the standard of care.
Contributor Information
Vamsi R. Velchuru, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA.; Division of Colon Rectal Surgery, University of Illinois of Chicago, Chicago, IL, USA.
Marek Zawadzki, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA.; Division of Colon Rectal Surgery, University of Illinois of Chicago, Chicago, IL, USA.
Amy L. Levin, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA..
Christine M. Bouchard, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA..
Slawomir Marecik, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA..
Leela M. Prasad, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA.; Division of Colon Rectal Surgery, University of Illinois of Chicago, Chicago, IL, USA.
John J. Park, Division of Colon and Rectal Surgery, Advocate Lutheran General Hospital, Park Ridge, IL, USA..
References:
- 1. Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg. 2008;143(7):701–707 [DOI] [PubMed] [Google Scholar]
- 2. Kilic A, Kavic Stephen. Laparoscopic colotomy repair following colonoscopic polypectomy. JSLS. 2008;12(1):93–96 [PMC free article] [PubMed] [Google Scholar]
- 3. Trecca A, Gaj F, Gagliardi G. Our experience with endoscopic repair of large colonoscopic perforations and review of the literature. Tech Coloproctol. 2008;12:315–322 [DOI] [PubMed] [Google Scholar]
- 4. Jovanovic I, Zimmermann L, Fry LC, Monkemuller K. Feasibility of endoscopic closure of an iatrogenic colon perforation occurring during colonoscopy. Gastrointest Endosc. 2011;73(3)550–555 [DOI] [PubMed] [Google Scholar]
- 5. Korman LY, Overholt BF, Box T, Winker CK. Perforation during colonoscopy in endoscopic ambulatory surgical centers. Gastrointest Endosc. 2003;58(4):554–557 [DOI] [PubMed] [Google Scholar]
- 6. Ahlawat S, Gupta N, Benjamin SB, Al-Kawas FH. Large colorectal polyps: endoscopic management and rate of malignancy: does size matter? J Clin Gastroenterol. 2011;45:347–354 [DOI] [PubMed] [Google Scholar]
- 7. Damore LJ, 2nd, Rantis PC, Vernava AM, 3rd, Longo WE. Colonoscopic perforations. Etiology, diagnosis, and management. Dis Colon Rectum. 1996;39(11):1308–1314 [DOI] [PubMed] [Google Scholar]
- 8. Moussi A, Nouira R, Bourguiba B, Daldoul S, Zaouche A. Rare cause of a lower gastrointestinal bleeding. Tunis Med. 2010;88(12):961–963 [PubMed] [Google Scholar]
- 9. Padberg BC, Emmermann A, Zornig C, Germer M, Schroder S. Leiomyomatosis of the colon: Case report and literature review. Pathologe. 2007;28(2):161–165 [DOI] [PubMed] [Google Scholar]
- 10. Agaimy A, Wunsch PH. True smooth muscle neoplasms of the GIT: morphological spectrum and classification in a series of 85 cases from a single institute. Lagenbecks Arch Surg. 2007;392(1):75–81 [DOI] [PubMed] [Google Scholar]
- 11. Repici A, Tricerri R. Endoscopic polypectomy: techniques, complications and follow-up. Tech Coloproctol. 2004. December;8 Suppl 2:s283–290 Review [DOI] [PubMed] [Google Scholar]
- 12. Geraci G, Pisello F, Antonio S, Modica G, Sciumè C. Endoscopic resection of a large colonic lipoma: case report and review of the literature. Case Rep Gastroenterol. 2010. February 3;4(1):6–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Luigiano C, Ferra F, Ghersi S, et al. Endoclip–assisted resection of large pedunculated colorectal polyps: Technical aspects and outcome. Dig Dis Sci. 2010. June;55(6)1726–1731 [DOI] [PubMed] [Google Scholar]
- 14. Jansen JB, Temmerman A, Tjhie-Wensing JW. Endoscopic removal of a large colonic lipomas. Ned Tijdschr Geneeskd. 2010;154:A2215 Dutch [PubMed] [Google Scholar]
- 15. Lohsiriwat V, Sujarittanakarn S, Akaraviputh T, Lertakyamanee N, Lohsiriwat D, Kachinthorn U. What are the risk factors of colonoscopic perforation? BMC Gastroenterol. 2009;24:9:71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pèrez Roldán F, González Carro P, Legaz Huidobro ML, et al. Endoscopic resection of large colorectal polyps. Rev Esp Enferm Dig. 2004;96:36–47 [DOI] [PubMed] [Google Scholar]
- 17. Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol. 2000;95(12):3418–3422 [DOI] [PubMed] [Google Scholar]
- 18. Lohsiriwat V. Colonoscopic perforation: Incidence, risk factors, management and outcome. World J Gastroenterol. 2010;16(4):425–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bleier JI, Moon V, Feingold D, et al. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2008;22:646–649 [DOI] [PubMed] [Google Scholar]
- 20. Barbagallo F, Castello G, Latteri S, et al. Successful endoscopic repair of an unusual colonic perforation following polypectomy using an endoclip device. World J Gastroenterol. 2007;13(20):2889–2891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Magdeburg R, Collet P, Post S, Kaehler G. Endoclipping of iatrogenic colonic perforation to avoid surgery. Surg Endosc. 2008;22:1500–1504 [DOI] [PubMed] [Google Scholar]
- 22. Taku K, Sano Y, Fu KI, et al. Iatrogenic perforation associated with therapeutic colonoscopy: A multicenter study in Japan. J Gastroenterol Hepatol. 2007;22:1409–1414 [DOI] [PubMed] [Google Scholar]
- 23. Kirschnaik A, Kratt T, Stüker D, et al. A new endoscopic over the scope clip system for the treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66(1):162–167 [DOI] [PubMed] [Google Scholar]
- 24. Bleier JI, Moon V, Feingold D, et al. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2008;22(3):646–649 [DOI] [PubMed] [Google Scholar]


