The authors discuss laparoscopic removal of an abdominal cerclage in a female patient who presented at 19 weeks with ruptured membranes.
Keywords: Laparoscopic, Abdominal, Cerclage, Pregnancy, Intrauterine
Abstract
We discuss laparoscopic removal of an abdominal cerclage in a 39-year-old woman, gravida 4, para 0, abortus 3, who presented at 19 weeks' gestation with ruptured membranes. This patient had a failed previous vaginal cerclage. An abdominal cerclage was performed at the time of abdominal myomectomy. A subsequent pregnancy was diagnosed, with ruptured membranes at 19 weeks' gestation, and the patient opted for pregnancy termination. After laparoscopic removal of the cerclage, cervical laminaria were placed, and the patient underwent an uncomplicated dilation and curettage procedure the following day.
INTRODUCTION
Abdominal cerclage was originally described by Benson and Durfee1 in 1965. Most patients who have had recurrent second trimester pregnancy loss as a result of an incompetent cervix, now termed cervical insufficiency, can be treated successfully with a transvaginal cerclage. A select group of patients who have recurrent pregnancy loss despite a transvaginal cerclage or who have an anatomically physically disabled cervix, making vaginal cerclage placement impossible, may benefit from the transabdominal approach.2–4
In the past, the major disadvantage of the transabdominal approach has been the necessity of 2 laparotomies: one associated with placement of the cerclage and the other with cesarean delivery.5 We recently reported our series of successful abdominal cerclage procedures performed laparoscopically.6
Some disorders of pregnancy in the second trimester, before fetal viability, warrant delivery. Previously, these women required either a laparotomy to remove the cerclage to allow vaginal delivery or a hysterotomy for delivery while leaving the cerclage in situ. We describe a successful laparoscopic removal of an abdominal cerclage in a patient with ruptured membranes at 19 weeks' gestation. To date, removing a cerclage suture laparoscopically at this gestational age has been accomplished only one previous time.7
CASE REPORT
The patient was a 39-year-old woman, gravida 4, para 0, abortus 3, who presented at 19 weeks' gestation with spontaneous ruptured membranes. She had a poor pregnancy history, including a spontaneous miscarriage at 8 weeks with her first pregnancy and a loss at 16 weeks in her second pregnancy that was attributed to cervical insufficiency. In her third pregnancy, despite a prophylactic McDonald cerclage that was placed early in pregnancy, she had another loss at 16 weeks.
The decision was made to place an abdominal cerclage before another pregnancy. The patient was noted to have multiple uterine fibroids, including one 3 × 3–cm fibroid at the cervical isthmus. At the time of laparotomy, a myomectomy was performed to remove the 2 fibroids, and the abdominal cerclage was placed using a 5-mm Mersilene band.
The patient conceived within 3 months of her cerclage placement and had an uneventful early pregnancy. Obstetric ultrasonongraphy at 17 weeks revealed a cervical length of 47 mm and no funneling. At 19 weeks, spontaneous ruptured membranes were confirmed. She was counseled about the options of pregnancy termination versus expectant management. She elected pregnancy termination and preferred dilatation and curettage over induction of labor. To achieve adequate cervical dilation, removal of the abdominal cerclage was necessary. We scheduled the patient for a laparoscopic removal of the cerclage to be followed by placement of a cervical laminaria and a dilation and curettage procedure the following day after sufficient time had elapsed for the laminaria to affect cervical dilation.
Operative Procedure
While under general anesthesia, the patient was placed in a lithotomy position. The patient's uterus was 1 cm below the umbilicus. A 10-mm incision was made vertically in the navel, and a Hasson trocar was placed through the umbilicus under direct visualization. We placed two 5-mm trocars bilaterally, slightly above the level of the umbilical incision, and a single accessory port was placed suprapubically. Initial survey of the abdomen revealed moderate adhesions, which were lysed (Figure 1). A 5-mm, 3-blade laparoscopic fan was instrumental for retraction and manipulation of both the bowel and the uterus because this uterus was soft as would be expected in a 19-week gravid uterus. The entire pelvis was filled with the gravid uterus, and we needed all of the ports. The port positions were instrumental in finding the proper angle to dissect and locate the previously placed abdominal cerclage.
Figure 1.
Dense adhesions in deep pelvis.
After displacement of the uterus to the right and somewhat posteriorly and advancing the laparoscope anterior to the uterine fundus, we identified the vesicouterine reflection at the level of the internal cervical os. It required careful dissection with laparoscopic scissors and Maryland forceps along the left lateral vesicouterine reflection, undermining and lifting the bladder off of this portion of the lower uterine segment. Proceeding posteriorly was not an option because of the size of the uterus. This dissection uncovered the Mersilene knot that was positioned just anterolateral to the left uterine artery. We mention this to emphasize that at this gestation age, the lower uterine segment is soft and difficult to manage without incising into either the bladder or the uterine artery laterally. The knot was then grasped with a blunt grasper to elevate the suture. Laparoscopic scissors were gently placed under the single strand of the suture and the suture was transected. We removed the suture and knot. Blood loss was minimal and we ended her surgery. We then placed 10 laminaria in her cervix in preparation for her dilation and curettage procedure that was scheduled for the following day.
DISCUSSION
We have previously published a case report11 of a successful laparoscopic removal of an abdominal cerclage in a 17-week-gestation pregnancy. We reconfirm in this case report that in an even larger uterus at 19 weeks, an operative laparoscopy is a viable alternative for removing a cerclage previously placed by laparotomy.
An important technical aspect of the case was placement of the trocars.10,11 We placed the lateral trocars at least as high as the navel incision (Figures 2, 3, and 4). This allowed us to achieve the proper angle to address the depth and width of the larger uterus, which can block the visualization of the camera and trocars when they are placed through an infraumbilical port. In this case, we were able to displace the uterus posteriorly and lateral enough to develop a bladder flap, accessing the space of Retzius to ensure we had palpated and located the area of the suture and the knot. We were able to grasp the knot and elevate and transect the suture while firmly holding the knot. We then removed the entire knot and suture with good hemostasis. The lateral ports had been placed at a level slightly higher than the umbilicus under direct visualization to gain access to the cervical isthmus and bladder flap. In an earlier article,12 in a pregnancy at 17 weeks, a posterior approach was discussed. In this case, at 19 weeks' gestation, the uterus was too large to displace anteriorly or laterally enough to gain access to the posterior area between the uterosacral ligaments. We mention this because at the time of this surgery (10/27/2010), we were reporting the second case of removal of an abdominal cerclage as far as 19 weeks' gestation.7 This dissection was difficult to perform, and we would not recommend the posterior approach at 19 weeks' gestation.
Figure 2.
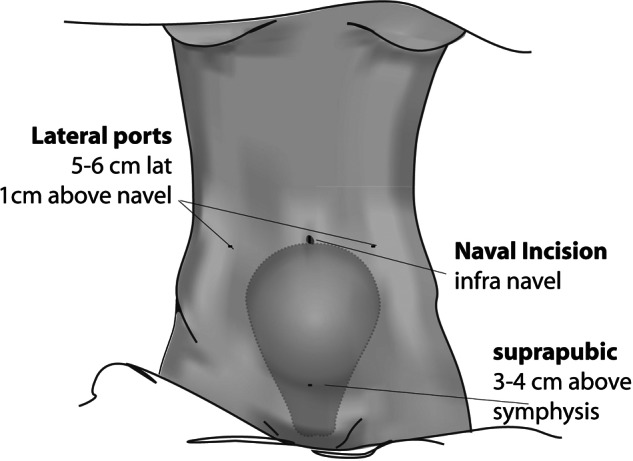
Uterus at 19+ weeks (our patient).
Figure 3.
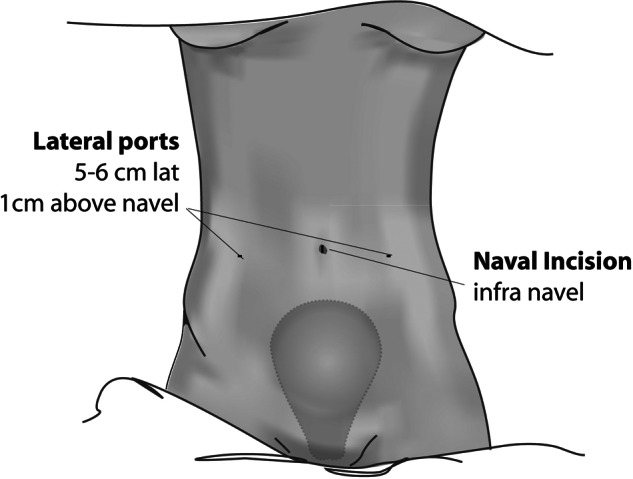
Example of uterus at 16 weeks.
Figure 4.
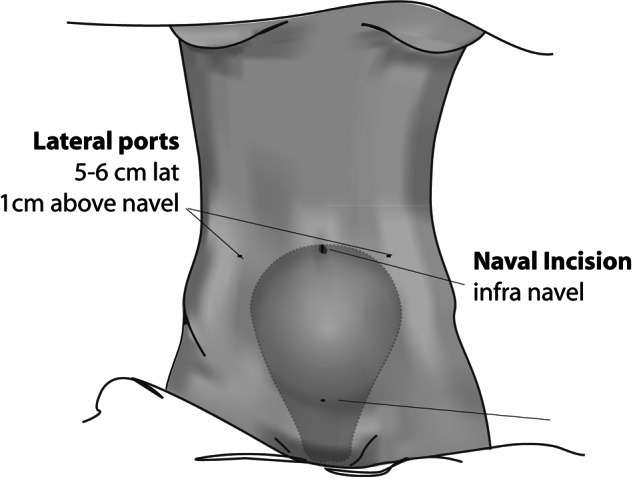
Example of uterus at 20 weeks.
CONCLUSION
An abdominal cerclage can be removed laparoscopically in the second trimester of pregnancy. At 19 weeks' gestation, this surgery requires a clear operative strategy and superior laparoscopic skills.
Contributor Information
James F. Carter, Department of Obstetrics and Gynecology, Medical University of South Carolina, Charleston, SC, USA..
Ashlyn Savage, Department of Obstetrics and Gynecology, Medical University of South Carolina, Charleston, SC, USA..
David E. Soper, Department of Obstetrics and Gynecology, Medical University of South Carolina, Charleston, SC, USA..
References:
- 1. Benson RC, Durfee RB. Transabdominal cervicouterine cerclage during pregnancy for treatment of cervical incompetency. Obstet Gynecol. 1965;25:145–155 [PubMed] [Google Scholar]
- 2. Novy MJ. Transabdominal cervicoisthmic cerclage: a reappraisal 25 years after its introduction. Am J Obstet Gynecol. 1991;164:1635–1642 [DOI] [PubMed] [Google Scholar]
- 3. Cammarano CL, Herron MA, Parer JT. Validity of indications for transabdominal cerclage for cervical incompetence. Am J Obstet Gynecol. 1995;172:1871–1875 [DOI] [PubMed] [Google Scholar]
- 4. Leiman G, Harrison NA, Rubin A. Pregnancy following conization of the cervix. Complications related to cone size. Am J Obstet Gynecol. 1980;136:14–18 [DOI] [PubMed] [Google Scholar]
- 5. Lesser KB, Childers JM, Surwit EA. Transabdominal cerclage: a laparoscopic approach. Obstet Gynecol. 1998;91:855–856 [DOI] [PubMed] [Google Scholar]
- 6. Carter J, Soper D, Goetzl L, Van Dorsten J. Abdominal cerclage for the treatment of recurrent cervical insufficiency: laparoscopy or laparotomy? Am J Obstet Gynecol. 2009;201:111.e1–e4 [DOI] [PubMed] [Google Scholar]
- 7. Agdi M, Tulandi Placement and removal of abdominal cerclage by laparoscopy. Reprod Biomed Online. 2008. February;16(2):308–310 [DOI] [PubMed] [Google Scholar]
- 8. Scarantino SE, Reilly JG, Moretti ML, Pillari VT. Laparoscopic removal of a transabdominal cervical cerclage. Am J Obstet Gynecol. 2000. May;182(5):1086–1088 [DOI] [PubMed] [Google Scholar]
- 9. McComiskey M, Dornan JC, Hunter D. Removal of transabdominal cerclage. Ulster Med J. 2006;75(3):228. [PMC free article] [PubMed] [Google Scholar]
- 10. Carter JF, Soper DE. Laparoscopy in pregnancy. JSLS. 2004;8:57–60 [PMC free article] [PubMed] [Google Scholar]
- 11. Carter JF, Soper DE. Laparoscopic abdominal cerclage: a case report. JSLS. 2005;9:491–493 [PMC free article] [PubMed] [Google Scholar]
- 12. Carter JF, Soper DE. Laparoscopic removal of abdominal cerclage: a case report. JSLS. 2007;11(3):375–377 [PMC free article] [PubMed] [Google Scholar]


