Abstract
Objective
To test whether children with attention-deficit/hyperactivity disorder (ADHD), free of conduct disorder (CD) in childhood (M=8 years), have elevated risk taking, accidents, and medical illnesses in adulthood (M=41 years); whether development of CD influences risk taking during adulthood; and whether exposure to psychostimulants in childhood predicts cardiovascular disease. We hypothesized positive relationships between childhood ADHD and risky driving (past 5 years), risky sex (past year), between risk taking and medical conditions in adulthood; and that development of CD/antisocial personality (APD) would account for the link between ADHD and risk taking. We report causes of death.
Method
Prospective 33-year follow-up of 135 white boys with ADHD in childhood, without CD (probands), and 136 matched male comparisons without ADHD (comparisons), (M=41 years), blindly interviewed by clinicians.
Results
In adulthood, probands had relatively more risky driving, sexually transmitted disease, head injury, and emergency department admissions (ps<.05–.01). Groups did not differ on other medical outcomes. Lifetime risk taking was associated with negative health outcomes (ps=.01–.001). Development of CD/APD accounted for the relationship between ADHD and risk-taking. Probands without CD/APD did not differ from comparisons in lifetime risky behaviors. Psychostimulant treatment did not predict cardiac illness (p=.55). Probands had more deaths not related to specific medical conditions (p=.01).
Conclusions
Overall, among children with ADHD, it is those who develop CD/APD who have elevated risky behaviors as adults. Over their lifetime, those who did not develop CD/APD did not differ from comparisons in risk-taking behaviors. Findings also provide support for long-term safety of early psychostimulant treatment.
Keywords: ADHD, follow-up, medical illnesses, psychostimulant treatment, risky behaviors
Attention deficit-hyperactivity/disorder (ADHD) is characterized by deficits in impulse control and goal-oriented behavior that may lead to excessive, potentially dangerous, risk taking,1 and incur serious negative consequences, such as accidental injuries, and even premature death.2, 3 Follow-up studies of clinic-referred children with ADHD have shown that risky behavior continues into early adulthood, including a greater propensity for risky driving,4-6 and risky sexual behavior.7-9 Although accidents, non-psychiatric hospitalizations, emergency department (ED) visits, are elevated in adolescence/early adulthood,4, 8, 10-13 their relationship to risk-taking behavior has not been examined.
Relatively poor health outcomes in individuals with a history of ADHD may be expected for reasons other than risk taking. Characteristics of ADHD that increase risk taking may also foster diminished regard for health-conscious behavior.8, 14 In addition, psychostimulants, first-line treatments for ADHD, are known to have small, statistically, significant effects on blood pressure and heart rate, but not discernible effect on cardiovascular integrity.15-19 Nevertheless, concerns about long-term negative effects of psychostimulants on cardiovascular health have been raised.20, 21 Long-term health outcomes of children with ADHD are limited to one study8 of young adults that did not find elevated rates of medical illnesses in subjects with ADHD.
So far, no longitudinal study of children with ADHD has extended beyond early adulthood. Consequently, we do not know whether excessive risk taking persists well into adulthood, and whether health differences emerge later in life. Risky behaviors among boys with ADHD might diminish through adulthood with increased driving experience and the formation of formal relationships. Conversely, health differences might emerge, when propensity for serious illnesses increases.
The strong evidence that ADHD is a risk factor for conduct disorder (CD) and antisocial personality disorder (APD)8, 22-24 has raised questions about their contribution to risk-taking among children with ADHD. The limited information available suggests that conduct problems in childhood (not CD per se) partially account for risky driving in late adolescence/early adulthood.4, 25 There is no report of the influence of adolescent-onset CD among children with ADHD, but no comorbid CD.
We report a 33-year follow-up of children with ADHD, without CD (probands), extending previous research by reporting risk-taking behaviors and health outcomes at mean age 41. We hypothesized that, in adulthood, compared to individuals without ADHD in childhood (comparisons), probands would report significantly more (1) risky driving, (2) risky sex, (3) sexually transmitted diseases (STDs), injuries, and accidents. Moreover, that (4) risky driving would be related to accidents, injuries, and ED admissions, (5) risky sex would be associated with STDs, and (6) that the association between childhood ADHD and risky driving and sex would be significantly accounted for by the development of CD/APD. Because there is minimal information on ADHD and health outcomes, no directional hypotheses were advanced regarding medical conditions. We previously reported relatively higher mortality in probands.24 Here, we indicate causes of death.
Method
Participants
Probands
Probands were 6 to 12-year-old Caucasian boys (M=8.3 years), of middle and lower-middle class, referred by schools for behavior problems, had elevated teacher and parent ratings of hyperactivity, behavior problems at school and home, IQ>85, and English-speaking parents (N=207).26, 27 Children with neurological, significant medical disorders, psychosis or conduct disorder were excluded. No other psychiatric disorder was exclusionary. Based on information from teachers, parents, and a psychiatric evaluation, children with a pattern of aggressive or antisocial behavior were excluded to rule out comorbid CD. Thus, teachers’ ratings of conduct problems were low, 0.7+0.4 (0–3 scoring).28
Of the 207 probands, 182 (88%) received methylphenidate, a subset of these were also treated with dextroamphetamine or magnesium pemoline. Mean treatment duration was about two years (750+586 days; range=9–2,486), and mean total cumulative dose was 33,473+33,253 mg (range=430–179,818 mg) (1 mg methylphenidate = 0.5 mg dextroamphetamine = 2.5 mg magnesium pemoline), which translates to 44.6 mg per day. Children did not receive additional stimulant treatment elsewhere. Detailed characteristics appear in previous publications.26, 27
Of 207 probands with ADHD, 195 (94%) were assessed in late adolescence (age=18.1+1.3) (FU18),29, 30 176 (85%) in young adulthood (age=25.3+1.4) (FU25),22, 23, 31 and 135 (65%) in adulthood (age=41.4+2.9) (FU41).24, 32 Informant interviews were obtained in nine of the 135 probands with FU41 data who did not participate but consented to an informant interview (4 deceased, 2 refused, 1 incarcerated, 1 unable to locate, 1 in military).
Comparisons
At FU18, white boys without ADHD (N=178; age=18.3+1.5) matched for age, social class, and geographic residence, were recruited from pediatric clinics within the same medical center.29 Children’s charts, which reported on children’s adjustment, were reviewed to select children without recorded behavior problems during elementary school. Parents were called, and asked whether a school teacher had ever complained about their child’s behavior. If not, the boy qualified as a comparison. Comparisons were reevaluated at FU25 (n=168/178, 94%) (age=25.0+1.8), and FU41 (n=136/178, 76%) (age=41.5+3.2). Seven of the 136 comparisons in FU41 were informant interviews (3 deceased, 3 refused, 1 unable to locate).
Study procedures were approved by the Institutional Review Board of the New York University Langone Medical Center. Participants and informants gave signed consent.
Measures
Detailed interviews about lifetime driving and sexual history, and medical history since the previous follow-up, were conducted by “blind”, highly trained, clinicians. Mean interval duration was 16.4+1.9 years (range: 11–20). Questions about risky driving and risky sex were adapted from existing instruments.33, 34
Risky Driving
We asked whether the individual ever had a license, length of time driving, total lifetime number of license revocations and citations, specific violations (e.g., driving while intoxicated, reckless driving), and age at first, and last, traffic violation.
Risky driving during adulthood was defined as occurring during the previous five years to ensure that earlier history did not confound adult findings.
Risky Sex
Participants were asked about age at first sexual intercourse, number of sexual partners, and birth control use in their 20s, 30s, and past year. We defined risky sex in adulthood as having occurred during the past year. It includes birth control, and number of sexual partners.
Conduct Disorder/Antisocial Personality Disorder
At each follow-up, “blind” clinicians formulated probable or definite diagnoses for all major psychiatric disorders.22, 24, 29 Diagnostic interviews used at FU18 and FU25 are available online (Tables S1–S3). At FU41, the Structured Clinical Interview for DSM-IV Axis I Disorders35 was administered. Definite diagnoses indicate that full DSM criteria were met. Probable diagnoses signify that, although less than full criteria occurred, they caused significant impairment. We considered APD present in adulthood if it occurred during the past five years.
Medical Outcomes
We inquired about 54 medical conditions, focusing on the period since the previous follow up. We grouped these into four categories: Neurological/Neuromuscular (e.g., epilepsy, head injury), Genitor-Urinary (e.g., STDs), cardiovascular (e.g., heart attack, hypertension), and Other. Because STDs and head injuries are of special interest in ADHD, we examined them individually. The specific medical conditions are available online (Table S1).
We inquired systematically about non-psychiatric hospitalizations, ED admissions, any injury causing work absences, and about the person’s role in motor vehicle accidents.
Mortality data were gathered through relatives’ reports, internet searches in Lexis-Nexis Accurint services, the Social Security Death Index, and Google searches for obituaries.
Data Analyses
We applied structural equation modeling (SEM) to test for the direct effect of ADHD on risky behaviors, and the indirect effect of ADHD on risky behaviors, through the effect of ADHD on the development of CD/APD (lifetime), and the effect of CD/APD on risky behaviors (lifetime). Thus, these sequential relationships reflect outcomes at any time in a participant’s life. SEM is well suited to test the relationship between childhood ADHD, CD/APD, and risky behaviors, because it can estimate different pathways simultaneously,36 and generates estimates of direct and indirect effects of the predictors on outcome. We report unstandardized b coefficients, which are regression coefficients and can be interpreted as such.
We built the model in several steps using Mplus.37 First, we tested a measurement model in which risky driving and risky sex were represented as two latent variables, each represented by observed (measured) variables or indicators. Indicators for risky driving include: license suspension/revocation, speeding citations, reckless driving, driving while intoxicated, and “Other moving violations”. License revoked, reckless driving, and driving intoxicated had low frequencies and were dichotomized between one or more. Distributions of license revocation and “Other moving violations” were highly skewed. To avoid dichotomizing these variables arbitrarily, we applied previously reported procedures,8 making the split at or above the 75th percentile.8 Lifetime risky sex included early sex (at or before age 15), number of sex partners, and birth control. Because respondents often gave approximate numbers of lifetime partners, these were categorized at the 25th, 50th, and 75th percentiles: 0–5, 6–10, 11–25, 26 or more. Responses to questions regarding birth control were: 1=never, 2=rarely, 3=sometimes, 4=most of the time, and 5=almost always. The distribution was bimodal: most respondents endorsed “never” or “almost always.” Therefore, we combined 4 and 5 into “regular birth control”, and 1–3 into “no/irregular, birth control.” Thus, early sex, 26 sex partners or more, and lack of birth control use in the 20s, 30s, and in the last year, were indicators of risky sex. Because we expected the three periods for birth control to be correlated, we specified correlated error variances for these variables. Correlations between the latent variables (risky driving and risky sex) were also specified. Individual items inevitably have some error. Latent variables combine multiple items to represent underlying constructs, while adjusting for measurement error;36 consequently, they are superior to numerous pairwise comparisons.
The measurement model estimating relationships between observed variables (i.e., risky driving and sex items), and latent constructs for lifetime risky driving and risky sex, fit the data well (χ2[21]=29.63, p=.10; comparative fit index [CFI]=0.97; Tucker Lewis index [TLI]=0.96; root mean square error of approximation [RMSEA]=0.04) (Figure S1, available online). Risky driving and risky sex were significantly correlated (ρ=.38, p<.001).
Next, we tested the relationship between childhood ADHD and lifetime risky driving and risky sex by adding childhood ADHD (proband vs. comparison) as a predictor. The paths from childhood ADHD to risky driving and risky sex represent direct effects of childhood ADHD on these outcomes. The model fit the data well (χ2(27)=39.37, p=.06; CFI=0.96; TLI=0.95; RMSEA=0.04). Finally, we added lifetime CD/APD to test whether their development contributed to group differences in risky driving and risky sex (χ2(30) = 43.05, p=.06, CFI=.97, TLI=.96, RMSEA=.04). This model includes the direct effect of childhood ADHD on risky driving and risky sex, adjusting for CD/APD, and the indirect effect of childhood ADHD on risky driving and risky sex, through ADHD’s effect on the development of CD/APD.
Analyses of risk-taking behaviors in adulthood followed approaches described above for lifetime relationships. Risky driving in adulthood encompassed the past five years. We ascertained whether any of the following had occurred: license revocation, speeding citation, reckless driving, drunk driving, and “Other moving violations.” However, we did not obtain their frequency over the past five years. Questions about risky sex in adulthood were about the past year. Therefore, risky sex in adulthood reflects behavior during the previous year. The measurement model for risky sex did not have an acceptable solution, therefore, we included the two variables separately (no birth control use and two or more sexual partners, in the past year; Figure S2, available online). This model fit the data well (2(11)=12.98, p=.29; CFI=0.98; TLI=0.98; RMSEA=0.03).
We could not build an explanatory model to test whether APD accounted for relationships between childhood ADHD and risky behaviors because no comparison had APD during the previous five years. Therefore, we compared probands with APD (N=24; 23 definite, 1 probable) and without APD (N=104), in the past five years. We also contrasted these two proband groups to comparisons (N=134).
We contrasted groups on injuries, hospitalizations, and health outcomes using chi-square, or Fisher’s Exact Test, when appropriate.
Among probands, logistic regressions tested relationships between lifetime risk taking and relevant health outcomes, and between childhood psychostimulant exposure and cardiovascular conditions. For tests of relationships between risky driving and health outcomes, total number of violations was categorized at the 25th, 50th, and 75th percentiles: 0–5, 6–10, 11 and more. Significance level was set at =.05, two-tailed.
Results
Sample Characteristics
Sample characteristics are detailed elsewhere.24 Briefly, probands and comparisons did not differ in age (41.4+2.9 and 41.5+3.2, p=.78). At FU41, probands had significantly lower SES than comparisons (3.4+1.0 vs. 2.4+1.1, p<.001). Most probands and comparisons were married (70% and 79%, p=.10). Almost all probands and comparisons self-identified as heterosexual (132/135 [98%] and 132/136 [97%], respectively), one proband and three comparisons as homosexual, and two probands and one comparison as bisexual. Probands and comparisons did not differ on: driving experience (23.1+4.6 and 23.9+3.9 years, respectively, p=.14) or ever having a driver’s license (128/135 [95%] vs. 134/136 [99%], respectively, p=.10).
Do Adults with ADHD in Childhood Engage in More Risky Driving and Risky Sex than Peers Without ADHD?
Over their lifetime, probands had engaged in significantly more risky driving (b[SE]=0.61[0.15], p<.001, R-square=0.13) and more risky sex (b[SE]=0.67[0.16], p<.001, R-square=0.24) than comparisons. Rates and fitted relative risks for each item are indicated in Table 1.
Table 1.
Lifetime History of Risky Driving and Sexual Behaviors
| Risky Behaviors | Probands (N = 135)a |
Comparisons (N = 136)a |
χ2 or t | p | Fitted Risk Ratiob |
|---|---|---|---|---|---|
| n/N (%) or Mean (SD) |
n/N (%) or Mean (SD) |
||||
| Risky Drivingc | |||||
| License revoked
or suspended |
68/125 (54) | 41/134 (31) | 15.03 | .0001 | 1.77 |
| Cited for speeding ≥
5 times |
45/125 (36) | 30/133 (23) | 5.65 | .02 | 1.57 |
| Cited for
reckless driving |
17/124 (14) | 8/133 (6) | 4.33 | .04 | 2.18 |
| Cited for driving
while intoxicated |
20/127 (16) | 16/134 (12) | 0.80 | .37 | 1.78 |
| Cited other
moving violationsd |
69/122 (57) | 54/133 (41) | 6.49 | .01 | 1.26 |
| Total number of
traffic violations, Mean (SD) |
8.91 (10.92) | 4.56 (6.41) | 3.93 | .0001 | n/a |
| Risky Sex | |||||
| Sexual debut by age 15 | 64/132 (48) | 26/129 (20) | 23.18 | .0001 | 2.18 |
| Lifetime number of sexual partners |
|||||
| 0–5 | 34/127 (27) | 41/123 (33) | 1.28 | .26 | n/a |
| 6–10 | 27/127 (21) | 30/123 (24) | 0.35 | .56 | n/a |
| 11–25 | 29/127 (23) | 31/123 (25) | 0.19 | .66 | n/a |
| 26 or more | 37/127 (29) | 21/123 (17) | 5.10 | .02 | 2.27 |
| No birth control use in his 20s |
48/130 (37) | 24/130 (18) | 11.06 | .001 | 1.90 |
| No birth control use in his 30s |
56/130 (43) | 32/130 (25) | 9.89 | .002 | 1.39 |
| No birth control use
last year |
65/126 (52) | 53/128 (41) | 2.64 | .10 | 1.29 |
Note. Variable Ns due to skips and missing data.
Calculated using fitted proportions for each group estimated in the structural equation model. These fitted proportions were nearly identical to the observed proportions, but they take into account the underlying latent variables representing the constructs of risky driving and risky sex.
Among those who ever had a driver’s license.
Making illegal turn, failing to yield, failing to stop, or tailgating.
As hypothesized, during adulthood, probands had engaged in more risky driving than comparisons (past five years) (b[SE]=0.48[0.22], p<.05, R-square=0.07). However, contrary to expectations, they had not engaged in significantly more risky sex (past year): birth control (b[SE]=0.26[0.16], n.s.); two or more sexual partners (b[SE]= 0.05[0.21], n.s.). Hospitalizations, ED Admissions, Injuries, Accidents, and Medical Conditions
Elsewhere, we report that significantly more probands than comparisons had been hospitalized in psychiatric facilities.24 Such was not the case for non-psychiatric hospitalizations (35% of probands versus 34% of comparisons, p=.86). However, significantly more probands had three or more ED admissions (37% vs. 21%, p<.01), and reported having had a head injury (9% vs. 3%, p<.05), but they did not indicate significantly more work absences due to injuries of any kind (52%, probands, 45%, comparisons, p=.25) (Table 2).
Table 2.
Medical Outcomes Since the Last Follow-Up Interview (mean, 16.4 years)
| Medical Outcome | Probands (N = 135)a |
Comparisons (N = 136)a |
χ 2 | p ≤ |
|---|---|---|---|---|
| n/N (%) | n/N (%) | |||
| Non-psychiatric hospitalization | 47/135 (35) | 46/136 (34) | 0.03 | .86 |
| Visited ED 3 times or more | 48/131 (37) | 28/136 (21) | 8.44 | .004 |
| Motor vehicle accidents/injuriesb | ||||
| Judged at fault in ≥ 2 accidents | 39/110 (35) | 22/118 (19) | 8.21 | .004 |
| Someone injured in accident | 53/109 (49) | 24/118 (20) | 20.22 | .0001 |
| Any injury causing work absence | 69/133 (52) | 61/136 (45) | 1.33 | .25 |
| Medical Conditions | ||||
| Neurological/Neuromuscular | 37/135 (27) | 36/136 (26) | 0.03 | .86 |
| Head injury | 12/135 (9) | 4/136 (3) | 4.31 | .04 |
| Genito-urinary | 30/135 (22) | 19/136 (14) | 3.11 | .08 |
| Sexually Transmitted | ||||
| Diseasec | 20/135 (15) | 9/136 (7) | 4.76 | .03 |
| Cardiovascular | 37/135 (27) | 37/136 (27) | 0.00 | .97 |
| Otherd | 97/135 (72) | 93/136 (68) | 0.39 | .53 |
Note: ED = Emergency Department.
Variable Ns due to skips, missing data, and/or inclusion of cases who died due to the listed medical conditions.
Among those who ever had an accident.
Excludes human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS).
Cancer, dermatologic, endocrine/glandular, gastrointestinal, hematologic/blood disorders, infectious, metabolic, musculoskeletal, respiratory, systemic, and other medical conditions.
Probands were more likely to have been judged at fault in two or more motor vehicle accidents (35% vs. 19%, p<.01), and involved in two or more accidents resulting in injury (49% vs. 20%, p<.0001). Posthoc, we examined whether accidents resulting in injuries were significantly related to head injury. They were not (p=.27).
Rates of STDs were higher in probands than comparisons (15% vs. 7%, p<.05); other medical conditions were not significantly different.
Relationship between Lifetime Risk-Taking, Accidents, and Medical Outcomes among Probands
Frequency of traffic violations was significantly related to being judged at fault in two or more accidents. Compared to probands who had five traffic violations or less, those with 6–10 and over 10 violations, were more likely to be judged at fault in two or more accidents (odds ratio [OR] [CI]=4.70[1.60;13.83], p<.01, and OR[CI]=7.05[2.59;19.16], p<.001, respectively). Also compared to probands with five violations or less, those with over 10 violations were more likely to have accidents that caused injury (OR[CI]=3.81[1.47;9.88], p<.01), and have multiple ED admissions (OR[CI]=6.02[2.39;15.17], p<.0001), but not more head injuries (OR[CI]=2.44[0.65;9.13], p=.18). No difference found for those with 6–10 violations (ps .18–.83).
Only a trend was found between no birth control in the 20s and ever having an STD (OR[CI]=2.41[0.92;6.33], p=.07). Birth control in the 30’s (OR[CI]=1.77[0.68;4.61], p=.25), and in the previous year (OR[CI]=1.35[0.50;3.62], p=.55), did not predict STDs. Probands with 11– 25, and 26 or more, partners had higher rates of STDs than those with fewer partners (10 or less) (OR[CI]=4.53[1.21;17.03] p=.03) and (OR[CI]=4.58[1.30;16.17], p=.02), respectively. Early sexual debut was unrelated to STDs (OR[CI]=1.36[0.52;3.54]).
Does CD/APD Account for the Relationship between Childhood ADHD and Risky Behaviors?
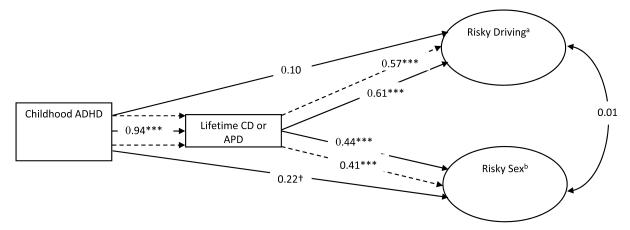
Figure 1 shows the direct and indirect effect of childhood ADHD on lifetime risky driving and risky sex, through its effect on the development of CD/APD. Intercorrelations are available online (Table S2, available online). We report elsewhere,24 that probands had a significantly elevated lifetime rate of CD/APD. As hypothesized, childhood ADHD predicted risky driving and risky sex through the development of CD/APD, as indicated by the significant indirect effect of childhood ADHD on risky driving and risky sex (b[SE]=0.57[0.11], p<.0001 and b[SE]=0.41[0.10], p<.0001, respectively). Importantly, after accounting for the presence of CD/APD, childhood ADHD was no longer significantly predictive of risky driving and risky sex (b[SE]=0.10[0.16], p=.53, b[SE]=0.22[0.13], p=.08, respectively). This model accounted for 51% of the variance in risky driving, and 70% of the variance in risky sex. Table S3 (available online), shows contrasts between probands with lifetime CD/APD (N=84, 62%), without CD/APD ever (N=51, 38%), and comparisons.
Figure 1.
Explanatory Model of Risk-Taking Behaviors. Note: Unstandardized coefficients. Solid arrows represent direct effects which adjust for all of the variables in the model. Thus, if one predicts risky driving from childhood attention-deficit/hyperactivity disorder (ADHD), after taking conduct disorder (CD)/antisocial personality disorder (APD) into consideration, ADHD is not significantly predictive (b=0.10). Dashed arrows represent the indirect effects of ADHD on risky driving and risky sex through its effect on the development of CD/APD. a License revoked, speeding > 5 times, reckless driving, drunk driving, other moving violation. b More than 25 sexual partners, early sex, no birth control in 20s, no birth control in 30s, and no birth control in the past year. *** p<.001, ** p<.01. † p <.10
As adults, probands who had APD in the past five years were more likely to have their license revoked or suspended (30% vs. 7%, p<.01), and be cited for “other” moving violations (35% vs. 13%, p<.05) than probands free of APD (Table S4, available online). However, probands with and without APD in adulthood did not differ significantly with respect to reckless and drunk driving (10% vs. 4%, and 4% vs. 4%), nor citations for speeding (57% versus 43%). Notably, probands free of APD differed from comparisons only on speeding violations (43% vs. 30%; p<.05). They did not differ significantly in rate of license suspensions (7% vs. 5%) or other moving violations (13% in both).
Does Stimulant Treatment in Childhood Predict Cardiovascular Disease in Adulthood?
There was no association between cumulative dose of stimulant and cardiovascular disease [OR(CI)=1.00(1.00;1.00), p=.55].
Deceased Subjects
A larger proportion of probands than comparisons were deceased [15/207 (7%) vs. 5/178 (3%), p=.05].24 Deceased subjects did not differ from those interviewed, and those lost to follow-up, in baseline socioeconomic status (SES), IQ, or teacher hyperactivity ratings (Table S5, available online). Table 3 specifies cause of, and age at, death. Probands had more deaths unrelated to identified medical conditions than comparisons (10/207 vs. 1/178, p=0.01). Post-hoc analyses did not show significant associations between probands’ mortality and lifetime psychiatric disorders other than ADHD (ps, .20–.73) (Table S6, available online).
Table 3.
Cause of Death and Age at Death
| Probands (N = 207) |
Comparisons (N = 178) |
χ 2 | p | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Cause of Death | n (%) | Age at Death (Years) |
n (%) | Age at Death (Years) |
||
| Total | 15 (7) | 5 (3) | 3.83 | .05 | ||
| Related to identified physical conditions | 4 (2) | 37–38 | 3 (2) | 26–43 | FET | 1.00 |
| Cancer | 2 (1) | 37, 37 | 2 (1) | 42, 43 | ||
| Diabetic coma | 1 (.5) | 38 | 0 | |||
| AIDS | 0 | 1 (.6) | 33 | |||
| Cardiac arrest | 1 (.5) | 38 | 0 | |||
| Unrelated to identified physical conditions | 10 (5) | 16–40 | 1 (.6) | 26 | 6.28 | .01 |
| Suicide | 3 (1) | 21, 30, 30 | 0 | |||
| Alcohol/Drug Overdose | 1 (.5) | 39 | 1 (.6) | 26 | ||
| Homicide | 2 (1) | 22, 40 | 0 | |||
| Occupational deatha | 2 (1) | 30, 40 | 0 | |||
| Hit by a car | 1 (.5) | 16 | 0 | |||
| Fall from roof | 1 (.5) | 24 | 0 | |||
| Other | 1 (.5) | 34 | 1 (.6) | 36 | — | — |
| 9/11b | 0 | 1 (.6) | 36 | |||
| Unknown | 1 (.5) | 34 | 0 | |||
Note: AIDS = Acquired Immune Deficiency Syndrome; FET = Fisher’s Exact Test.
One pilot died in a plane crash, one firefighter died in a fire.
Terrorist attack in New York City’s World Trade Center on 9/11/2001.
Discussion
Previous studies have reported elevated risky driving4-6, 13 and risky sexual behaviors7, 9 in children with ADHD followed into their mid 20s. This follow-up of children with ADHD (probands) reaches into the children’s fourth and fifth decade. At mean age 41, risky driving, but not risky sex, was significantly higher among probands than among their peers without ADHD (comparisons). At the time the children were diagnosed with ADHD, at average age 8, conduct disorder (CD) was systematically excluded; subsequently, a proportion developed CD and antisocial personality disorder (APD). It is among those who developed CD/APD that risky driving and risky sex was relatively more frequent over time. Thus, taking CD/APD into consideration eliminated the effect of early ADHD on risk-taking behavior. In fact, probands without CD/APD had not engaged in more risky behaviors than the comparisons (Tables S3 and S4, available online), indicating that ADHD, itself, was not predictive of risk-taking behavior; rather, it appears that ADHD affects risk-taking indirectly, through fostering the development of CD/APD. This finding adds to a consistent literature documenting that a multitude of adverse outcomes among children with ADHD is accounted for by the development of conduct disorder.22, 29, 38, 39
Over their lifetime, probands exhibited relatively higher rates of risky sex practices. However, when considering recent behavior, there was no difference between probands and comparisons. It seems likely that risky sex diminished over time due to the establishment of formal relationships. For example, an equivalently large proportion of probands and comparisons were married (70% and 79%),24 and most who reported having sex in the past year indicated having had only one sexual partner (89%, both groups).
We also report health-related outcomes. Among these, the most striking is the elevated rate of premature deaths in probands (7% vs. 3%, p=.05).24 Probands had significantly higher rates of deaths that were unrelated to identified medical conditions (5% vs. 0.6%; p=.01). The vast majority of probands died from causes that were unrelated to physical conditions (71% vs. 20% in comparisons). An association between childhood ADHD and suicide has been suggested,40-42 possibly linked to CD and depression.41 In the three suicides in this study, two had CD (one, major depression), and all three had a substance use disorder. Unexpectedly, lifetime psychiatric diagnoses were not significantly associated with mortality. Overall, deceased subjects (fortunately) are too few for clear inferences.
Other than mortality, we found few elevated adverse health outcomes among probands, and most were related to risk taking. Probands were more likely to have been admitted to EDs multiple times, and to have had a head injury. They were also more often responsible for motor vehicle accidents, and more of them had accidents resulting in injury. Risky driving was related to accidents and health outcomes, but not to head injuries. Of note, among probands with a head injury, only half reported ever missing work due to an injury, raising question about severity of the injury, especially since probands and comparisons did not differ in rate of injuries causing work absences.
Prior follow-ups of children with ADHD into their mid 20’s have reported conflicting results regarding an association between STDs and ADHD.8, 9 Following children with ADHD into their 30s and 40s, we found elevated rates of STDs. It is possible that this finding reflects the extended follow-up (33 years), which increased the likelihood of contracting STDs. STDs were positively related to having had more than 10 sexual partners.
It is unexpected, and encouraging, that probands and comparisons did not differ in rates of other medical conditions, given the lifestyle of individuals with childhood ADHD. Besides more risk taking, at FU41, probands had elevated rates of non-alcohol substance use disorder and nicotine dependence,24 known risk factors for multiple illnesses. Our results concur with Barkley et al.’s follow-up into early adulthood.8
Long-term effects of stimulants on cardiovascular health have been a major concern.18, 19, 27, 43 We found no evidence that children exposed to relatively high stimulant doses were at comparatively higher risk of cardiovascular diseases. Others have reported similar findings in children and young adults.15, 16, 44
As in all studies, generalizations are limited by sample characteristics, in this instance, white, lower middle, and middle class males. We relied on self-reports, possibly over- or under-estimating risky behaviors and medical conditions. Although this feature applies to both groups, differential reporting is possible. However, self-reports of risky driving have been found to correspond well to official records.6, 45, 46 We did not conduct medical exams, nor reviewed lifetime medical records. Unfortunately, the latter are unobtainable in the absence of centralized medical care. We did not find that exposure to stimulant treatment in childhood increased cardiac disease in later life. However, this study does not address risks associated with stimulant treatment that occurs, or extends, beyond childhood.
In sum, we found that men with ADHD in childhood, but without comorbid conduct disorder, were not at greater risk for elevated risky behavior, unless they developed conduct disorder or antisocial personality. The few negative health outcomes associated with childhood ADHD were related to risk taking, which in turn was predicted by CD/APD, confirming the negative long-term consequences of the emergence of conduct disorder among boys with ADHD. Importantly, findings add to growing evidence of the long-term safety of stimulant treatment in childhood.
Supplementary Material
Figure S1: Measurement Model of Risk-Taking Behaviors. Note: Unstandardized coefficients. Fit Statistics: χ2(21)=29.63, p=.10; Comparative Fit Index (CFI)=.97; Tucker Lewis Index (TLI)=.96; Root Mean Square Error of Approximation (RMSEA)=.04. *** p<.001, ** p<.01, *p<.05.
Figure S2. Childhood attention-deficit/hyperactivity disorder (ADHD) Predicting Risky Driving and Risky Sex in Adulthood. Note: Unstandardized coefficients. Fit Statistics: χ2(11) =12.98, p=.29; Comparative Fit Index (CFI)=.98; Tucker Lewis Index (TLI)=.98; Root Mean Square Error of Approximation (RMSEA)=.03. *** p<.001, ** p<.01, * p<.05
Table S1. Description of Medical Conditions and Illnesses Falling Into Each Medical Problem Category
Table S2. Bivariate Tetrachoric Correlations Between Variables in the Structural Equation Model (N=271)
Table S3. Lifetime History of Risky Driving and Sexual Behaviors of Probands With and Without Lifetime Conduct Disorder (CD) or Antisocial Personality Disorder (APD) and All Comparisons
Table S4. Relationship between Childhood Attention-Deficit/Hyperactivity Disorder (ADHD), Antisocial Personality Disorder (APD), and Risky Driving in the Past Five Years
Table S5. Childhood Characteristics of Probands who Were Interviewed, Lost to Follow-Up, and Deceased
Table S6. Mortality Rates by Mental Disorder in Probands
Acknowledgments
Research was supported by National Institute of Mental Health grants MH-18579 (R.G.K.) and T32 MH-067763 (F.X.C.), and by the National Institute on Drug Abuse grant DA-16979 (F.X.C.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Olazagasti, Klein, Mannuzza, and Castellanos, Ms. Belsky, Mr. Hutchison, and Ms. Lashua-Shriftman report no biomedical financial interests or potential conflicts of interest.
Supplemental material cited in this article is available online.
References
- 1.Barkley RA. ADHD and the Nature of Self-Control. Guilford Press; New York: 1997. [Google Scholar]
- 2.Nunn S. Death by motorcycle: Background, behavioral, and situational correlates of fatal motorcycle collisions. J Forensic Sci. 2011;56(2):429–437. doi: 10.1111/j.1556-4029.2010.01657.x. [DOI] [PubMed] [Google Scholar]
- 3.Boyce WF, Davies D, Gallupe O, Shelley D. Adolescent risk taking, neighborhood social capital, and health. J Adolesc Health. 2008;43(3):246–252. doi: 10.1016/j.jadohealth.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: A 3-to 5-year follow-up survey. Pediatrics. 1993;92(2):212. [PubMed] [Google Scholar]
- 5.Lambert NM. Analysis of the driving histories of ADHD subjects. 1995;417:1–21. DOT HS 808. [Google Scholar]
- 6.Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: Driving abilities, safe driving behavior, and adverse driving outcomes. Accid Anal Prev. 2007;39(1):94–105. doi: 10.1016/j.aap.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45(2):192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 8.Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. The Guilford Press; 2010. [Google Scholar]
- 9.Flory K, Molina BSG, Pelham WE, Jr, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. J Clin Child Psychol. 2006;35(4):571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- 10.Barkley RA. Accidents and attention-deficit/hyperactivity disorder. Econ Neurosci. 2001;3:64–68. [Google Scholar]
- 11.Bruce B, Kirkland S, Waschbusch D. The relationship between childhood behaviour disorders and unintentional injury events. Paediatr Child Health. 2007;12(9):749–754. doi: 10.1093/pch/12.9.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Saf Res. 2007;38(1):113–128. doi: 10.1016/j.jsr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Weiss G, Hechtman L, Perlman T, Hopkins J, Wener A. Hyperactives as young adults: A controlled prospective ten-year follow-up of 75 children. Arch Gen Psychiatry. 1979;36(6):675–681. doi: 10.1001/archpsyc.1979.01780060065007. [DOI] [PubMed] [Google Scholar]
- 14.Chuah SC, Drasgow F, Roberts BW. Personality assessment: Does the medium matter? No. J Res Pers. 2006;40(4):359–376. [Google Scholar]
- 15.Olfson M, Huang C, Gerhard T, et al. Stimulants and cardiovascular events in youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(2):147–156. doi: 10.1016/j.jaac.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127(6):1102–1110. doi: 10.1542/peds.2010-3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein RG, Bessler AW. Stimulant side effects in children. In: Kane JM, Lieberman JA, editors. Adverse Effects of Psychotropic Drugs. Guilford Press; New York: 1992. pp. 470–496. [Google Scholar]
- 18.Hammerness PG, Perrin JM, Shelley-Abrahamson R, Wilens TE. Cardiovascular risk of stimulant treatment in pediatric attention-deficit/hyperactivity disorder: Update and clinical recommendations. J Am Acad Child Adolesc Psychiatry. 2011;50(10):978–990. doi: 10.1016/j.jaac.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Huang YS, Tsai MH. Long-term outcomes with medications for attention-deficit hyperactivity disorder: Current status of knowledge. CNS Drugs. 2011;25(7):539–554. doi: 10.2165/11589380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 20.Nissen SE. ADHD drugs and cardiovascular risk. N Engl J Med. 2006;354(14):1445–1448. doi: 10.1056/NEJMp068049. [DOI] [PubMed] [Google Scholar]
- 21.Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder. Circulation. 2008;117(18):2407–2423. doi: 10.1161/CIRCULATIONAHA.107.189473. [DOI] [PubMed] [Google Scholar]
- 22.Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys: Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993;50(7):565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- 23.Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155(4):493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- 24.Klein RG, Mannuzza S, Ramos-Olazagasti MA, et al. Clinical and functional outcome of childhood ADHD 33 years later [published online ahead of print Oct 2012] Arch Gen Psychiatry. doi: 10.1001/archgenpsychiatry.2012.271. DOI: 10.1001/archgenpsychiatry.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thompson AL, Molina BSG, Pelham W, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. J Pediatr Psychol. 2007;32(7):745–759. doi: 10.1093/jpepsy/jsm002. [DOI] [PubMed] [Google Scholar]
- 26.Gittelman R, Abikoff H, Pollack E, Klein DF, Katz S, Mattes J. A controlled trial of behavior modification and methylphenidate in hyperactive children. In: Whalen C, Henker B, editors. Hyperactive Children. Academic Press; Orlando: 1980. pp. 221–243. [Google Scholar]
- 27.Gittelman-Klein R, Klein DF, Katz S, Saraf K, Pollack E. Comparative effects of methylphenidate and thioridazine in hyperkinetic children: I. clinical results. Arch Gen Psychiatry. 1976;33(10):1217–1231. doi: 10.1001/archpsyc.1976.01770100079008. [DOI] [PubMed] [Google Scholar]
- 28.Mannuzza S, Klein RG, Abikoff H, Moulton JL., Iii Significance of childhood conduct problems to later development of conduct disorder among children with ADHD: A prospective follow-up study. J Abnorm Child Psychol. 2004;32(5):565–573. doi: 10.1023/b:jacp.0000037784.80885.1a. [DOI] [PubMed] [Google Scholar]
- 29.Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up: I. psychiatric status. Arch Gen Psychiatry. 1985;42(10):937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- 30.Mannuzza S, Klein RG, Bonagura N, Malloy P, Giampino TL, Addalli KA. Hyperactive boys almost grown up: V. replication of psychiatric status. Arch Gen Psychiatry. 1991;48(1):77–83. doi: 10.1001/archpsyc.1991.01810250079012. [DOI] [PubMed] [Google Scholar]
- 31.Mannuzza S, Klein RG, Bessler A, Malloy P, Hynes ME. Educational and occupational outcome of hyperactive boys grown up. J Am Acad Child Adolesc Psychiatry. 1997;36(9):1222–1227. doi: 10.1097/00004583-199709000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Proal E, Reiss PT, Klein RG, et al. Brain gray matter deficits at 33-year follow-up in adults with attention-deficit/hyperactivity disorder established in childhood. Arch Gen Psychiatry. 2011;68(11):1122–1134. doi: 10.1001/archgenpsychiatry.2011.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barkley RA. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3rd ed Guildford Press; New York: 2006. [Google Scholar]
- 34.National Comorbidity Survey [Accessed September/14, 2012]; http://www.hcp.med.harvard.edu/ncs/instruments.php#jump4.
- 35.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- 36.Kline RB. Principles and Practice of Structural Equation Modeling. 3rd ed Guilford Press; New York: 2011. [Google Scholar]
- 37.Muthén LK, Muthén BO. Mplus User’s Guide. 6th ed Muthén & Muthén; Los Angeles: 2010. [Google Scholar]
- 38.Mannuzza S, Klein RG, Moulton JL. Lifetime criminality among boys with attention deficit hyperactivity disorder: A prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008;160(3):237–246. doi: 10.1016/j.psychres.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow[g486]up of hyperactive children: Antisocial activities and drug use. J Child Psychol Psychiatr. 2004;45(2):195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 40.Manor I, Gutnik I, Ben-Dor D, et al. Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents-A pilot study. Eur Psychiatry. 2010;25(3):146–150. doi: 10.1016/j.eurpsy.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 41.James A, Lai F, Dahl C. Attention deficit hyperactivity disorder and suicide: A review of possible associations. Acta Psychiatr Scand. 2004;110(6):408–415. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 42.Kelly TM, Cornelius JR, Clark DB. Psychiatric disorders and attempted suicide among adolescents with substance use disorders. Drug Alcohol Depend. 2004;73(1):87–97. doi: 10.1016/j.drugalcdep.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Stiefel G, Besag F. Cardiovascular effects of methylphenidate, amphetamines and atomoxetine in the treatment of attention-deficit hyperactivity disorder. Drug Saf. 2010;33(10):821–842. doi: 10.2165/11536380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 44.Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896–1904. doi: 10.1056/NEJMoa1110212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6):1089–1095. [PubMed] [Google Scholar]
- 46.Barkley RA, Murphy KR, Dupaul GJ, Bush T. Driving in young adults with attention deficit hyperactivity disorder: Knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc. 2002;8(5):655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: Measurement Model of Risk-Taking Behaviors. Note: Unstandardized coefficients. Fit Statistics: χ2(21)=29.63, p=.10; Comparative Fit Index (CFI)=.97; Tucker Lewis Index (TLI)=.96; Root Mean Square Error of Approximation (RMSEA)=.04. *** p<.001, ** p<.01, *p<.05.
Figure S2. Childhood attention-deficit/hyperactivity disorder (ADHD) Predicting Risky Driving and Risky Sex in Adulthood. Note: Unstandardized coefficients. Fit Statistics: χ2(11) =12.98, p=.29; Comparative Fit Index (CFI)=.98; Tucker Lewis Index (TLI)=.98; Root Mean Square Error of Approximation (RMSEA)=.03. *** p<.001, ** p<.01, * p<.05
Table S1. Description of Medical Conditions and Illnesses Falling Into Each Medical Problem Category
Table S2. Bivariate Tetrachoric Correlations Between Variables in the Structural Equation Model (N=271)
Table S3. Lifetime History of Risky Driving and Sexual Behaviors of Probands With and Without Lifetime Conduct Disorder (CD) or Antisocial Personality Disorder (APD) and All Comparisons
Table S4. Relationship between Childhood Attention-Deficit/Hyperactivity Disorder (ADHD), Antisocial Personality Disorder (APD), and Risky Driving in the Past Five Years
Table S5. Childhood Characteristics of Probands who Were Interviewed, Lost to Follow-Up, and Deceased
Table S6. Mortality Rates by Mental Disorder in Probands