Two cases of ACC of the larynx were treated with CRT for organ preservation. The patients completed a course of combined chemoradiotherapy with weekly carboplatin and paclitaxel and radiotherapy. Both patients are alive with local regional control and functional larynx, therefore, chemoradiation with weekly carboplatin and paclitaxel may be a potential alternative to the current treatment.
Keywords: Adenoid cystic carcinoma, Cancer, Case series, Chemoradiotherapy, Larynx, Organ-sparing, Organ preservation, Local regional control
Abstract
Objectives.
Two cases of adenoid cystic carcinoma (ACC) of the larynx were treated with chemoradiotherapy (CRT) for organ preservation. We reviewed case series and current literature to contrast the potential role of primary CRT as an organ-sparing modality with standard laryngectomy and radiotherapy in patients with laryngeal ACC.
Methods.
Two treatment-naïve patients with laryngeal ACC treated at Dana-Farber Cancer Institute between 2002 and 2007 were identified. Both patients were offered standard laryngectomy followed by adjuvant radiotherapy or organ-sparing treatment modality.
Results.
Both patients were males, aged 57 and 73. The patients completed a course of combined chemoradiotherapy with weekly carboplatin and paclitaxel and 7–8 weeks of radiotherapy to a total dose of 6,600 and 7,000 cGy over 50 and 57 days, respectively. There were no treatment breaks or delays because of toxicity. The major toxicities reported by both patients, as anticipated, were Grade 3 mucositis, desquamative dermatitis, and severe dysphagia, all of which resolved. Both patients are alive with local regional control and functional larynx; one at 112+ months with pulmonary metastases at 54 months, and the other disease free at 60+ months.
Conclusions.
Definitive chemoradiation with weekly carboplatin and paclitaxel may be a potential alternative to the current standard of surgery and radiation for patients with locally advanced laryngeal ACC who request an organ-sparing approach. In this group of patients, salvage laryngectomy may be reserved for those who are locally recurrent or chemoradiotherapy resistant. Although CRT provided long-term local regional control in our two patients, there are evident limitations in obtaining evidence for a determination of treatment of rare diseases. This report provides support for following an organ preservation plan in selected patients.
Implications for Practice:
Concurrent chemoradiotherapy may be used for larynx preservation for selected patients with adenoid cystic carcinoma of the larynx when the functional outcome after surgery is expected to be unsatisfactory or when surgical expertise in such procedures is not available. Laryngeal preservation with concurrent chemoradiotherapy with surgery reserved for recurrent disease seems to offer potential for laryngeal preservation without compromising overall survival. Selection of a treatment option: surgery versus organ-sparing chemoradiotherapy will depend on patient choice of treatment, local expertise, and the availability of appropriate support and rehabilitation services.
Introduction
Adenoid cystic carcinoma (ACC) is a rare cancer that generally develops in the major salivary glands. It may originate in minor salivary glands in other regions of the head and neck, such as the larynx, as well as in the lung, trachea, skin, or breast. There are approximately 1,200 new cases of ACC in the United States per year [1]. Because of the slow growth of the disease, the prevalence is high. According to the Surveillance Epidemiology and End Results (SEER) Database, in 2006, nearly 14,873 living persons in the United States had been diagnosed with ACC [2].
ACC is considered a low-grade malignancy characterized by slow growth, which inclines to spread along perineural spaces. It has a predisposition to recur at the primary site and in the head and neck region primarily along cranial nerves (local recurrence), and to metastasize to distant anatomical sites, particularly the lungs, potentially resulting in life-threatening complications [3–6]. Laryngeal ACC is an extremely rare form of the neoplasm. The majority of instances of laryngeal ACC are located in the subglottic area, a minority of cases in the supraglottic area, and a relatively few have a glottic origin [7–9]. Diagnosis may be delayed because of the lack of symptoms in the early stages of the disease. Initial complaints depend upon the location of the mass. Supraglottic tumors may present with dysphagia, subglottic with stridor and respiratory obstruction, and glottic with hoarseness. Generally, when diagnosed, tumors that have already invaded deeply into the tissue with submucosal and perineural spread require multimodality therapy.
Surgery followed by adjuvant radiotherapy is currently the mainstay of therapy for many patients. Only those patients with very early lesions, resected with negative margins, and no perineural invasion escape radiotherapy. Radiotherapy alone is thought to be inferior when compared with combination of surgery and radiation. A retrospective study of all ACC head and neck sites conducted at the University of Florida compared radiotherapy alone or combined with surgery for local control (LC). At 5 and 10 years, LC was 56% versus 94% and 43% versus 91%, respectively, for surgery versus the combination. Similarly, in the same study, overall survival (OS) at 5 years (57% vs. 77%) and 10 years (42% vs. 55%) was superior when surgery was combined with adjuvant radiotherapy [10]. Consequently, primary radiotherapy is rarely recommended as a single treatment modality for ACC in general but selection bias may have led patients with more advanced, nonresectable tumors to be treated with radiotherapy only, thus affecting the overall results of this retrospective study. Chemotherapy has largely been reserved for palliation for recurrent or metastatic disease [11]. Evidence for concurrent chemotherapy and radiation as a primary treatment for ACC is limited [12–15].
Because of the inability to obtain data from large, prospective multi-institutional studies in ACC and more so in a rare presentation of ACC, guidance on treatment must rely on retrospective institutional case series. The objective of this article is to present two cases of laryngeal ACC treated with primary chemoradiotherapy for organ preservation and contrast the outcome with the results reported in the literature.
Materials and Methods
Two patients with laryngeal ACC were seen in the Head and Neck Oncology Program at the Dana-Farber Cancer Institute between 2002 and 2011. They were the only previously untreated patients with larynx ACC in that period. They were evaluated by a multidisciplinary team that included a surgeon, radiation oncologist, and medical oncologist. Primary assessment of both patients included computed axial tomography (CT) scan and/or magnetic resonance imaging (MRI) of the region, laryngeal biopsies, evaluation for distant metastases with laboratory tests for liver and bone abnormalities, and chest CT scan. The patients were offered the option of organ-sparing chemoradiotherapy based on a regimen used for primary treatment of squamous cell cancer of the head and neck (SCCHN) [28] or surgical laryngectomy followed by adjuvant radiation. Both patients were deemed eligible for chemoradiotherapy based on normal renal and liver function, ECOG performance status of zero, normal hematologic assessment, no serious concomitant illnesses, no evidence of metastases by chest CT scan, and mental capacity of giving informed consent for chemotherapy.
Chemotherapy with intravenous bolus of carboplatin, at an AUC of 1.5, and paclitaxel, 45 mg/m2, was given weekly starting with and during concomitant radiotherapy, such that at least three radiotherapy treatments succeeded the chemotherapy infusion each week to warrant optimal sensitization. Prior to chemotherapy, patients received premedication, including antiemetics, a steroid, antihistamine, and an H2 blocker. Toxicities were graded according to the National Cancer Institute's Common Terminology Criteria for Adverse Event Reporting v3.0.
Radiation therapy was delivered using standard fractionation of 1.8 Gy. A total dose of 66.0 Gy was delivered to patient 1 and 70.2 Gy to patient 2, delivered over 50 and 57 days, respectively. Three-dimensional planning was utilized to optimize the treatment and to minimize dose to the normal structures according to currently accepted conventional dose constraints. After therapy terminated, the patients were followed clinically at uniform intervals. They were treated symptomatically until adverse events were resolved. Follow-up CT or MRI scan of the primary site and chest were performed regularly following therapy for comparison to the baseline scan performed prior to treatment.
Results
Demographic characteristics are presented in Table 1. ACC-1 has been previously reported with 3 years of follow-up [12]. The patient is a 41-year-old white male who presented with subglottic ACC. He is a nonsmoker, has mild hypertension, and a history of gastroesophageal reflux disease. At the initial consultation, he presented with increasing dyspnea that required tracheostomy for airway protection. He had no evidence of malignancy within the neck other than some slight thickening in the subcricoid area anteriorly, consistent with infiltration of the soft tissues through the cartilages seen on his CT scan. Nasopharyngoscopic evaluation visualized the tumor in the subglottic region that was abutting the vocal cords with no mobility impairment. The tumor was anteriorly situated, close to the midline with no obvious vocal cords, and the arytenoids were damaged. The distal end of the tumor was not visible through the open larynx. The biopsy demonstrated the presence of laryngeal ACC.
Table 1.
Patient characteristics
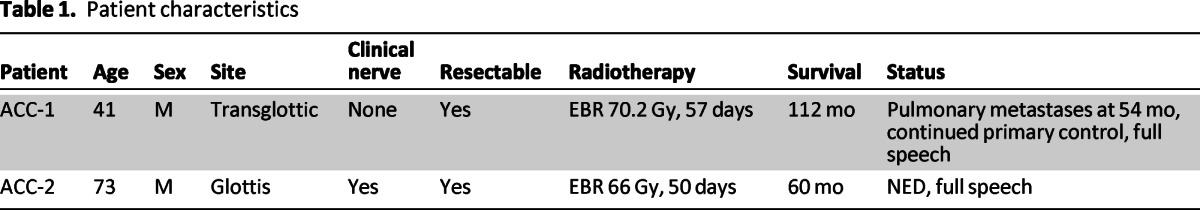
The second patient, with glottic ACC, is a 73-year-old white male who presented with 2.5-year history of progressive hoarseness, without dyspnea. He reported a history of tobacco use (from age 23 to 40) and had the following comorbidities: atrial fibrillation, hypothyroidism, and osteoarthritis. During initial presentation, no abnormalities were found upon physical exam, but a flexible nasopharyngoscopy evaluation demonstrated right vocal fold immobility involving the upper portion of the right cord and the aryepiglottic fold with possible involvement of the true cord. His right vocal cord appeared to be elevated and lateralized, not allowing for proper closure. The vocal cord edges were smooth bilaterally, and periarytenoid and postcricoid edema were present. A laryngeal biopsy of the right posterior submucosal mass showed ACC with perineural invasion present but no lymphovascular involvement.
Both patients were offered an organ-sparing procedure or surgical therapy (standard laryngectomy) followed by radiation therapy. They both were highly desirous of maintaining their voice and selected a nonsurgical option. Both patients received daily radiotherapy over 7–8 weeks with weekly chemotherapy. Treatment was well tolerated without any delay or myelosupression. Radiotherapy given concurrently with weekly chemotherapy was given without interruption. Both patients experienced a complication of Grade 3 mucositis and dermatitis during the course of the treatment requiring topical and narcotic analgesia and occasional intravenous fluid hydration. Both patients had a feeding tube placed prophylactically for nutritional support and removed upon the completion of treatment. All acute side effects completely resolved within 6 months. The tracheostomy tube was removed during the treatment in the patient with transglottic mass. The site healed during and closed after chemoradiotherapy.
Both patients had responded to chemoradiotherapy confirmed with radiographic assessment. With a follow-up of 60+ and 112+ months, neither patient required salvage surgery for local or local regional failure. One patient developed distant metastases to the lung at 54 months and remains alive at 112 months treated with local therapy for pulmonary metastases.
Discussion
ACC of the larynx is a rare malignancy. In the absence of large, prospective multi-institutional studies to provide guidance on therapeutic approach, treatment, by necessity, must rely on retrospective institutional case series. Case series involve a small number of patients and selection biases exist, thus, they are more likely to be confounded and limited in any statement of causality of correlations observed. In spite of the limitations, however, our study has impactful information that can create awareness to clinicians that chemoradiotherapy may be a reasonable and rational treatment option for laryngeal ACC.
Currently, surgery followed by radiotherapy is the mainstay of the treatment for ACC. Partial laryngectomy and minimally invasive surgery may be options for carefully selected patients, especially those with relatively small primary tumors. But laryngeal ACC, unfortunately, is usually diagnosed as a locally advanced disease with perineural invasion. By way of comparison, functional organ preservation is widely recommended in squamous cell carcinoma (SCC) of the larynx [16]. The mainstay of treatment in advanced SCC is surgery, a combination of chemotherapy plus radiation therapy (CRT) or induction chemotherapy, followed by CRT [16–19]. In SCC of head and neck, total laryngectomy does not provide a significant survival advantage over CRT [20, 21]. Also, systemic treatment for ACC is not effective [22]; however, the radiation sensitizing effects of chemotherapy are independent of their systemic effect, and organ preservation is a reasonable goal for patients based on this therapeutic option [23, 24]. In one of the largest case series of 15 patients with laryngeal ACC treated at Princess Margaret between 1963 and 2005, local or regional recurrence was noted in 5 out of 15 patients (33.3%) and the distant metastasis was the most common pattern of failure (66.7%). The 5- and 10-year overall and disease-specific survival rates were 64% and 46%, and 69% and 49%, respectively. Interestingly, 3 out of 15 subjects were treated nonsurgically, two with radiation alone and one patient with CRT. The patients treated with radiotherapy alone had local recurrences at 6 months, one underwent salvage surgery, and the other refused salvage laryngectomy. The subject undergoing CRT had no local regional failure but eventually died of distant metastasis at 2.1 years [25]. Some other early studies utilized aggregate data to analyze laryngeal adenoid cystic carcinoma and adenocarcinoma, thus making it difficult to distinguish which treatment modality was used for each individual patient. For example, Alavi et al. presented five patients treated with surgery alone or followed by adjuvant radiotherapy with 2-year survival of 100% and a 5-year survival of 75%. Cohen et al. reported eight patients with similar treatment approaches, but high early survival of 87.5% at 2 years that dropped to 44.4% at 5 years [8, 26]. Recent studies, such as Calzada et al., stratified patients based on treatment modality and provided complementary data on local regional control. However, their lack of long-term follow-up is a limitation, as it weakens any conclusions made on recurrence. Due to short follow-up, Calzada et al. was able to report only 2-year DFS of 80% [27], as opposed to the 5-year follow-up reported in earlier surgical studies done by Cohen et al. and Alavi et al.
CRT has rarely been reported in ACC, however, it might prove useful for organ preservation and local regional control. Haddad et al. have shown that CRT in five patients with locally advanced ACC is an efficacious well-tolerated treatment [12]. In the current study, follow-up is 60+ and 112+. In the Princess Margaret larynx series, patients had undergone total laryngectomy alone or followed by adjuvant radiotherapy. The median survival was about 7 years and the local and regional recurrence rate was 25% (n = 3/12). In contrast, our study with CRT reports similar follow-up and no local regional recurrence (Table 2). Analysis of prior larynx ACC series supports the notion of high rate of local control with multimodality therapy. ACC can be associated with a long period of survival with local regional control in the face of the development of late distant metastases as seen in one of our two cases. In review of the referenced literature, we noted that out of the 36 patients included in this report, only 3 (8.3%) received CRT and this resulted in functional larynx and no local regional recurrence in all three. Based on this mature albeit limited data, we suggest that CRT is a reasonable treatment option that may be offered as an organ-sparing modality. Carboplatin and paclitaxel are the drugs of choice based on their excellent toxicity profile, radiation sensitizing properties, and long track record in SCC of head and neck [28–30].
Table 2.
Reported laryngeal ACC
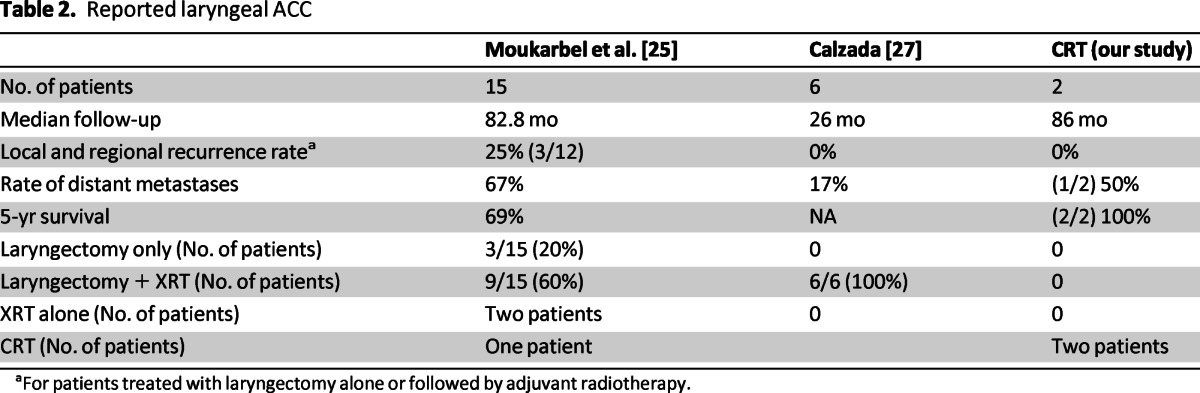
aFor patients treated with laryngectomy alone or followed by adjuvant radiotherapy.
We believe patients should be offered the option of organ preservation because of the importance of the larynx to speech and swallowing. Organ function-preserving approaches are not appropriate for all patients with locoregionally advanced cancer of the larynx. Chemoradiotherapy usually preserves laryngeal function, but it is associated with considerable acute toxicity that is manageable. However, in rare cases, chemoradiotherapy may compromise the goal of functional larynx preservation. Patients with destruction of vocal cords or cartilage destruction may have nonfunctional larynx with chemoradiotherapy, and in these cases, total laryngectomy followed by postoperative RT may be preferable in this setting. Where possible, an attempt at functional larynx preservation should be undertaken with surgery as salvage if needed. In laryngeal ACC, it also appears to be quite reasonable to attempt to control local regional disease with chemoradiotherapy rather than laryngectomy.
Conclusions
Unfortunately, although randomized clinical trials in laryngeal ACC are much needed, they are currently nonexistent and treatment recommendations must be based on limited evidence. In spite of its limitations, our study supports an alternative treatment option for patients with laryngeal ACC, avoiding surgery as an initial, and reserving it for salvage in the case of failure post-CRT. Patients with laryngeal ACC in our study and from Princess Margaret who refused surgery and were treated with organ-sparing definitive CRT have achieved the treatment goal of long-term organ preservation and survival. Organ preservation should not be done at the cost of quality of life. In our study, xerostomia was the only major long-term side effect, and patients preserved their larynx and kept their speech and swallowing intact. An organ preservation decision should be evaluated on an individualized basis, taking into consideration age, comorbidities, extent of disease on presentation, and most importantly, the preference of the patient.
Author Contributions
Collection and/or assembly of data: Krzysztof J. Misiukiewicz
Data analysis and interpretation: Krzysztof J. Misiukiewicz
Manuscript writing: Krzysztof J. Misiukiewicz, Nadia Camille
Final approval of manuscript: Krzysztof J. Misiukiewicz, Roy Tishler, Robert Haddad, Sewanti Limaye, Marshall Posner
Disclosures
The authors indicated no financial relationships.
References
- 1.Statistical basis: This is based on an incidence rate of 0.4 per 100,000 (Source: SEER) and a population of 305.8 million (Source: U.S. Census Bureau) [Google Scholar]
- 2.Statistical basis: This is based upon the prevalence rate of 1.49 per 100,000 (Source: SEER) [Google Scholar]
- 3.Kokemueller H, Eckardt A, Brachvogel P, et al. Adenoid cystic carcinoma of the head and neck—A 20 years experience. Int J Oral Maxillofac Surg. 2004;33:25–31. doi: 10.1054/ijom.2003.0448. [DOI] [PubMed] [Google Scholar]
- 4.da Cruz Perez DE, de Abreu Alves F, Nobuko Nishimoto I, et al. Prognostic factors in head and neck adenoid cystic carcinoma. Oral Oncol. 2006;42:139–146. doi: 10.1016/j.oraloncology.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 5.da Cruz Perez DE, de Abreu Alves F, Nobuko Nishimoto I, et al. Adenoid cystic carcinoma of the head and neck: Predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg. 1999;125:149–152. doi: 10.1001/archotol.125.2.149. [DOI] [PubMed] [Google Scholar]
- 6.Khan AJ, DiGiovanna MP, Ross DA, et al. Adenoid cystic carcinoma: A retrospective clinical review. Int J Cancer. 2001;96:149–158. doi: 10.1002/ijc.1013. [DOI] [PubMed] [Google Scholar]
- 7.Batsakis JG, Luna MA, el-Naggar AK. Nonsquamous carcinomas of the larynx. Ann Otol Rhinol Laryngol. 1992;101:1024–1026. doi: 10.1177/000348949210101212. [DOI] [PubMed] [Google Scholar]
- 8.Alavi S, Namazie A, Calcaterra TC, et al. Glandular carcinoma of the larynx: The UCLA experience. Ann Otol Rhinol Laryngol. 1999;108:485–489. doi: 10.1177/000348949910800512. [DOI] [PubMed] [Google Scholar]
- 9.Dexemple P, Huth J, Rebufy M, et al. Cystic adenoid carcinoma of the larynx: Two cases. Ann Otolaryngol Chir Cervicofac. 2003;120:244–248. [PubMed] [Google Scholar]
- 10.Mendenhall WM, Morris CG, Amdur RJ, et al. Radiotherapy alone or combined with surgery for adenoid cystic carcinoma of the head and neck. Head Neck. 2004;26:154–162. doi: 10.1002/hed.10380. [DOI] [PubMed] [Google Scholar]
- 11.Laurie SA, Licitra L. Systemic therapy in the palliative management of advanced salivary gland cancers. J Clin Oncol. 2006;24:2673–2678. doi: 10.1200/JCO.2005.05.3025. [DOI] [PubMed] [Google Scholar]
- 12.Haddad RI, Posner MR, Busse PM, et al. Chemoradiotherapy for adenoid cystic carcinoma: Preliminary results of an organ sparing approach. Am J Clin Oncol. 2006;29:153–157. doi: 10.1097/01.coc.0000203756.36866.17. [DOI] [PubMed] [Google Scholar]
- 13.Maruya S, Namba A, Matsubara A, et al. Salivary gland carcinoma treated with concomitant chemoradiation with intraarterial cisplatin and docetaxel. Int J Clin Oncol. 2006;11:403–406. doi: 10.1007/s10147-006-0587-0. [DOI] [PubMed] [Google Scholar]
- 14.Sasiaja M, Funa N, Kamata M, et al. Unresectable adenoid cystic carcinoma of the trachea treated with chemoradiotherapy. Clin Oncol (R Coll Radiol) 2000;12:272. [PubMed] [Google Scholar]
- 15.Tse DT, Benedetto P, Dubovy S, et al. Clinical analysis of the effect of intraarterial cytoreductive chemotherapy in the treatment of lacrimal gland adenoid cystic carcinoma. Am J Ophthalmol. 2006;141:44–53. doi: 10.1016/j.ajo.2005.08.068. [DOI] [PubMed] [Google Scholar]
- 16.Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349:2091–2098. doi: 10.1056/NEJMoa031317. [DOI] [PubMed] [Google Scholar]
- 17.Posner MR, Hershock DM, Blajman CR, et al. Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N Engl J Med. 2007;357:1705–1715. doi: 10.1056/NEJMoa070956. [DOI] [PubMed] [Google Scholar]
- 18.Lefebvre JL, Chevalier D, Luboinski B, et al. Larynx preservation in pyriform sinus cancer: Preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. EORTC Head and Neck Cancer Cooperative Group. J Natl Cancer Inst. 1996;88:890–899. doi: 10.1093/jnci/88.13.890. [DOI] [PubMed] [Google Scholar]
- 19.The Department of Veterans Affairs Laryngeal Cancer Study Group. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med. 1991;324:1685–1690. doi: 10.1056/NEJM199106133242402. [DOI] [PubMed] [Google Scholar]
- 20.Pfister DG, Laurie SA, Weinstein GS, et al. American Society of Clinical Oncology clinical practice guideline for the use of larynx-preservation strategies in the treatment of laryngeal cancer. J Clin Oncol. 2006;24:3693–3704. doi: 10.1200/JCO.2006.07.4559. [DOI] [PubMed] [Google Scholar]
- 21.Weber RS, Berkey BA, Forastiere A, et al. Outcome of salvage total laryngectomy following organ preservation therapy: The Radiation Therapy Oncology Group trial 91–11. Arch Otolaryngol Head Neck Surg. 2003;129:44–49. doi: 10.1001/archotol.129.1.44. [DOI] [PubMed] [Google Scholar]
- 22.Laurie SA, Ho AL, Fury MG, Sherman E, et al. Systemic therapy in the management of metastatic or locally recurrent adenoid cystic carcinoma of the salivary glands: A systematic review. Lancet Oncol. 2011;12:815–824. doi: 10.1016/S1470-2045(10)70245-X. [DOI] [PubMed] [Google Scholar]
- 23.Tishler RB, Schiff PB, Geard CR, et al. Taxol: A novel radiation sensitizer. Int J Radiat Oncol Biol Phys. 1992;22:613–617. doi: 10.1016/0360-3016(92)90888-o. [DOI] [PubMed] [Google Scholar]
- 24.Milas L, Hunter NR, Mason KA, et al. Enhancement of tumor radioresponse of a murine mammary carcinoma by paclitaxel. Cancer Res. 1994;54:3506–3510. [PubMed] [Google Scholar]
- 25.Moukarbel RV, Goldstein DP, O'Sullivan B, et al. Adenoid cystic carcinoma of the larynx: A 40-year experience. Head Neck. 2008;30:919–924. doi: 10.1002/hed.20802. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J, Guillamondegui OM, Batsakis JG, et al. Cancer of the minor salivary glands of the larynx. Am J Surg. 1985;150:513–518. doi: 10.1016/0002-9610(85)90166-7. [DOI] [PubMed] [Google Scholar]
- 27.Calzada AP, Miller M, Lai CK, et al. Adenoid cystic carcinoma of the airway: A 30-year review at one institution. Am J Otolaryngol. 2012;33:226–231. doi: 10.1016/j.amjoto.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 28.Carter DL, Asmar L, Barrera D, et al. Favorable survival observed after carboplatin, paclitaxel, and concurrent accelerated hyperfractionated radiotherapy for treatment of locally advanced head and neck carcinoma. Invest New Drugs. 2008;26:473–481. doi: 10.1007/s10637-008-9128-1. [DOI] [PubMed] [Google Scholar]
- 29.Suntharalingam M, Haas ML, Conley BA, et al. The use of carboplatin and paclitaxel with daily radiotherapy in patients with locally advanced squamous cell carcinomas of the head and neck. Int J Radiat Oncol Biol Phys. 2000;47:49–56. doi: 10.1016/s0360-3016(00)00408-9. [DOI] [PubMed] [Google Scholar]
- 30.Haddad R, Sonis S, Posner M, et al. Randomized phase 2 study of concomitant chemoradiotherapy using weekly carboplatin/paclitaxel with or without daily subcutaneous amifostine in patients with locally advanced head and neck cancer. Cancer. 2009;115:4514–4523. doi: 10.1002/cncr.24525. [DOI] [PubMed] [Google Scholar]


