Abstract
AIM: To investigate computed tomography (CT) and magnetic resonance imaging (MRI) manifestations of rectal gastrointestinal stromal tumors (GISTs) in order to enhance the recognition of these rare tumors.
METHODS: Fourteen patients with pathologically proven rectal GISTs were retrospectively reviewed. Patient histories were retrospectively reviewed for patient age, gender, presenting symptoms, endoscopic investigations, operation notes and pathologic slides. All tumors were evaluated for CD117, CD34 expression, and the tumors were stratified according to current criteria of the National Institutes of Health (NIH). In all cases the first pre-operation imaging findings (CT and MRI, n = 3; MRI only, n = 8; CT only, n = 3) were analyzed by two experienced radiologists by consensus, which include: tumor size, shape, CT density (hypodense, isodense and hyperdense), MRI signal intensity (hypointense, isointense and hyperintense), epicenter (intraluminal or extraluminal), margin (well-defined or ill-defined), internal component (presence of calcifications, necrosis, hemorrhage or ulceration), pattern and degree of enhancement, invasion into adjacent structures. After review of the radiologic studies, clinical and pathological findings were correlated with radiological findings.
RESULTS: The patients, 13 men and 1 woman, were aged 31-62 years (mean = 51.5 ± 10.7 years). The most common initial presentation was hematochezia (n = 6). The mean tumor diameter was 5.68 ± 2.64 cm (range 1.5-11.2 cm). Eight lesions were round or oval, and 6 lesions were irregular. Eleven lesions were well-defined and 3 had ill-defined margins. Ten tumors were extraluminal and 4 were intraluminal. The density and MR signal intensity of the solid component of the lesions were similar to that of muscle on unenhanced CT (n = 6) and T1-weighted images (n = 11), and hyperintense on T2-weighted MR images. Calcification was detected in 2 tumors. Following intravenous injection of contrast media, 3 lesions had mild enhancement and 11 lesions had moderate enhancement. Enhancement was homogenous in 3 lesions and heterogeneous in 11. In 1 of 11 patients who underwent both CT and MRI, the tumor was homogenous on CT scan and heterogeneous on MRI. Eight patients were classified as high risk according to the modified recurrent risk classification system of NIH.
CONCLUSION: Rectal GISTs usually manifest as large, well-circumscribed, exophytic masses with moderate and heterogeneous enhancement on CT and MRI. The invasion of adjacent organs, bowel obstruction and local adenopathy are uncommon.
Keywords: Gastrointestinal stromal tumors, Rectum, Computed tomography, Magnetic resonance imaging
Core tip: Rectal gastrointestinal stromal tumors (GISTs) are so rare that little information has been reported on their radiological features. This study describes the computed tomography (CT) and magnetic resonance imaging (MRI) features of rectal GISTs with clinical and pathological correlation, in order to better understand this rare disease. Rectal GISTs usually manifest as large, well-circumscribed, exophytic masses with moderate and heterogeneous enhancement on CT and MRI. The presence of invasion of adjacent organs, bowel obstruction and local adenopathy is uncommon.
INTRODUCTION
Gastrointestinal stromal tumors (GISTs), which arise from the interstitial cell of Cajal or its precursor, the intestinal mesenchymal precursor cell, are the most common mesenchymal neoplasms of the gastrointestinal tract. They are defined by their expression of CD117 (KIT), a tyrosine kinase growth factor receptor, which distinguishes them from other mesenchymal neoplasms such as leiomyomas, leiomyosarcomas, schwannomas, and neurofibromas and which determines the appropriateness of CD117-inhibitor therapy. Throughout the length of the gastrointestinal tract, GISTs arise most commonly in the stomach (60%-70%) followed by the small bowel (20%-25%), however, GISTs in the rectum are extremely rare (5%)[1]. It was reported that GISTs account for 0.6% of all malignant rectal tumors[2]. The imaging features of rectal GISTs are unclear due to their rarity and have only been described in small series[3-6]. Surgical resection remains the initial treatment for localized rectal GISTs[7], familiarity of these imaging features may permit preoperative diagnosis and improve the surgical management of patients. The purpose of our study was to describe the computed tomography (CT) and magnetic resonance imaging (MRI) features of rectal GISTs with clinical and pathological correlation, in order to enhance the understanding of this rare disease.
MATERIALS AND METHODS
The database of the Department of Surgery at our hospital was reviewed in order to identify patients presenting between January 2000 and June 2012 with histologically and immunochemically confirmed GISTs arising in the rectum. Fourteen patients were identified during this period. Patient histories were retrospectively reviewed for patient age, gender, presenting symptoms, endoscopic investigations, and surgical notes. Pathologic slides of the specimens and mitotic activity (number of mitoses per 50 consecutive high-power fields) were reviewed by an experienced pathologist, and the tumors were stratified according to the current criteria of the National Institutes of Health (NIH)[8]. All tumors were evaluated for CD117 and CD34 expression.
In all cases, the first pre-operative CT or MRI was reviewed. Of the 14 patients, 3 underwent both CT and MRI examinations, 8 underwent only MRI examinations and 3 underwent only CT examinations. The CT and MRI technique varied somewhat due to the different imaging equipment and the retrospective nature of the study. However, intravenous contrast-enhanced images had been obtained for studies in all patients. A retrospective review of CT and MR images was implemented by two radiologists by consensus. The following imaging features of each mass were assessed: tumor size, shape, CT density (hypodense, isodense and hyperdense), MRI signal intensity (hypointense, isointense and hyperintense), epicenter (intraluminal or extraluminal), margin (well-defined or ill-defined), internal component (presence of calcifications, necrosis, hemorrhage or ulceration), pattern of enhancement (homogeneous or heterogeneous), and invasion into adjacent structures. The degree of enhancement of the lesion was assessed subjectively and categorized as follows: mild, when the enhancement was similar to that of adjacent muscle; moderate, when the enhancement was higher than that of muscle, but lower than that of blood vessels; and marked, when the enhancement was approaching that of blood vessels. High signal intensity in the necrosis on T1WI was defined as hemorrhage. The adjacent structures were also assessed for the presence of invasion. Findings on CT and MRI for abdominal adenopathy and hepatic metastasis were also evaluated. After review of the radiologic studies, surgical notes and excised specimens were correlated with radiological findings.
RESULTS
Clinical findings
Our patient cohort included 13 men and 1 woman with a mean age of 51.5 ± 10.7 years (range, 31-62 years), and the clinical findings are summarized in Table 1. Digital colorectal examination was performed in 7 patients. Colonoscopy showed a mass protruding from the rectal wall with intact overlying mucosa in 6 patients (Figure 1), while a central mucosal ulceration was revealed in 1 patient. Two of these 7 patients underwent additional endoscopic ultrasonography, which showed hypoechoic masses that were contiguous with the muscularis propria of the rectal wall (Figure 1). All masses were found in the lower part of the rectum, with a distance from the anal verge ranging from 2.0 to 5.5 cm. Twelve patients underwent radical resection, including abdominoperineal resection (n = 9) and low anterior resection (n = 3) depending on the extent and localization of the tumors. The other 2 patients underwent transanal excision. At the time of surgical exploration, none of the patients had evidence of remote metastasis. Tumor rupture was not found during surgery. No lymph node metastases were identified pathologically in all 12 patients who underwent lymphadenectomy.
Table 1.
Summary of the presenting complaints of 14 patients with rectal gastrointestinal stromal tumors
| Presenting symptoms or signs | n |
| Incidental finding on an imaging study | 2 |
| Change of defecation habit | 2 |
| Hematochezia | 6 |
| Pelvic pain | 1 |
| Narrow stools | 1 |
| Difficult defecation | 1 |
| Sense of anal falling inflation | 1 |
Figure 1.
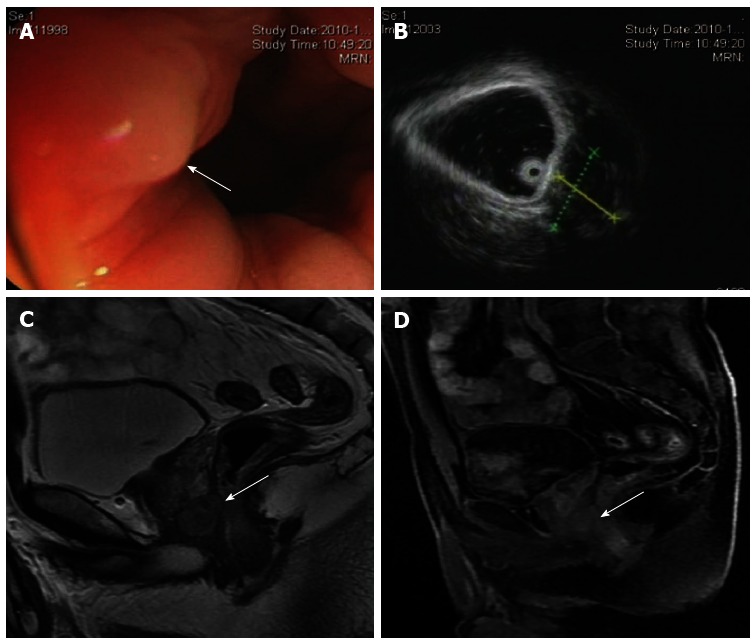
A 40-year-old man with a rectal gastrointestinal stromal tumor. A: Colonoscopy shows a mass protruding from the rectal wall with intact overlying mucosa (arrow); B: Endoscopic ultrasonography shows a well-defined hypoechoic mass located along the right anterior aspect of the rectal wall; C: Sagittal T2-weighted magnetic resonance imaging shows an oval, homogenous, hyperintense mass with a sharp margin bordering the anterior rectal wall. A small area of anatomical continuity between the tumor and the anterior rectal wall is observed (arrow); D: Postcontrast T1-weighted image shows a slightly homogenously enhancing mass (arrow).
Pathological findings
Immunohistochemical staining showed that all tumors were positive for CD117 (14/14) (Figure 2), while 13 patients were positive for CD34 (13/14). The masses were solid and grayish-white or dark-red with areas of hemorrhage or necrosis on the cut sections (Figure 3), and showed a spindle cell pattern under light microscope (Figure 2). According to the current NIH classification scheme, 8 tumors (8/14) had high risk, 3 (3/14) had intermediate risk, 3 (3/14) had low risk for aggressive behavior.
Figure 2.
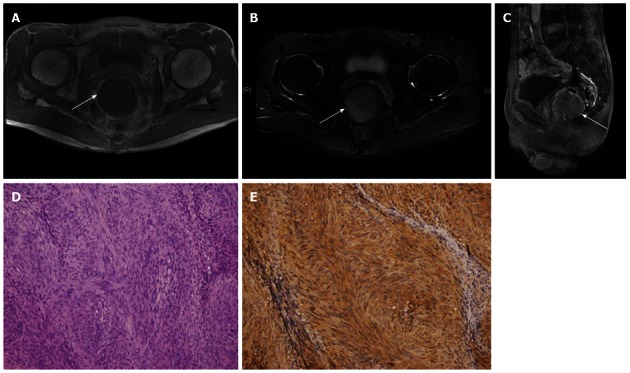
A 56-year-old man with a rectal gastrointestinal stromal tumor. A: Axial T1WI shows the lesion as a round, intraluminal, homogenous, hypointense mass with a sharp margin (arrow); B: It shows homogenous hyperintense on T2WI (arrow); C: Sagittal enhanced T1WI shows homogenous moderate enhancement (arrow); D: Photomicrograph shows fascicular proliferation of spindle-shaped tumor cells (hematoxylin and eosin, × 200); E: The tumor cells were strongly and diffusely positive for CD117 staining (immune-histochemistry, × 200).
Figure 3.
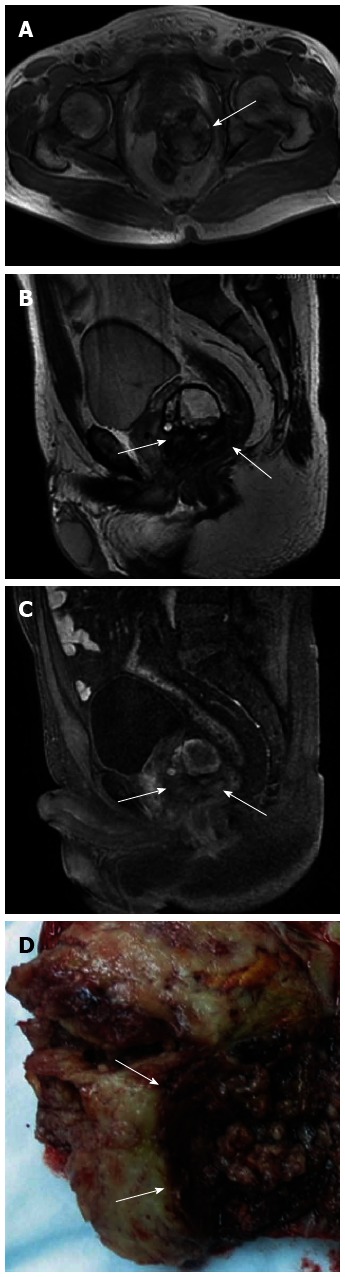
A 62-year-old man with a rectal gastrointestinal stromal tumor. A: The mass is located between the prostate and the anterior rectal wall and its epicenter is well outside the rectum. Axial T1-weighted MR image shows a high signal (arrow) within the mass, in keeping with hemorrhage; B: Sagittal T2WI shows a heterogenous mixed-intense mass with blurring contour (arrow); C: Postcontrast T1WI shows the solid component of the mass enhanced heterogeneously (arrow); D: Macroscopic cross section shows a pale yellow, tan and solid mass with hemorrhage (arrow).
Imaging findings
The diameter of the tumors ranged from 1.5 to 11.2 cm (mean, 5.68 ± 2.64 cm). The tumor was smaller than 5 cm in 4 patients and larger than 5 cm in 10 patients. Eight masses were either round (n = 2) or oval (n = 6), and 6 were irregular. The tumors showed definite intraluminal tumor growth in 4 patients, whereas extraluminal tumor growth was seen in the majority of our patients (10/14) (Figures 1-8). Eleven tumors showed a well-defined margin, and 3 tumors showed contour irregularity or blurring.
Figure 8.
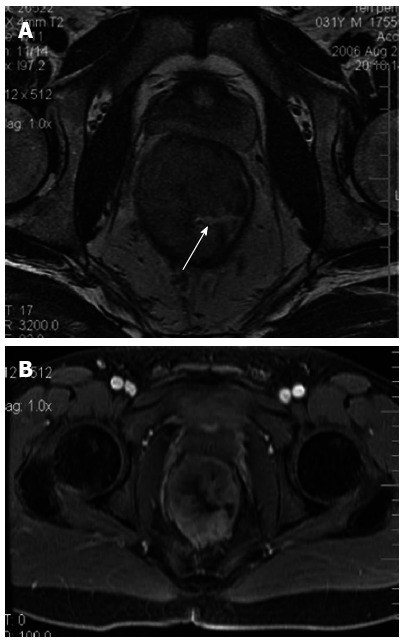
A 31-year-old man with a rectal gastrointestinal stromal tumor. A: Axial T2WI shows the lesion as an intraluminal mass with ulceration (arrow) of the rectal lumen; B: The mass is enhanced moderately heterogeneously following intravenous administration of gadolinium.
On unenhanced CT images, the density of the 6 tumors was 33-45 HU (mean, 38 HU) which was similar to that of muscle. Flecks of calcification were detected in 2 extraluminal tumors (Figures 4, 5). Following intravenous administration of contrast media, the majority (4/6) of rectal GISTs were moderately enhanced masses with areas of unenhanced low attenuation on CT scan. A homogeneous pattern of enhancement was less common and was present in 2 of the patients who underwent CT studies (Figure 6); in 1 patient who underwent both CT and MRI, the tumor was homogenous on CT scan, but demonstrated heterogeneous enhancement with foci of fluid signal on MR images. All the heterogeneous tumors showed areas of fluid density in keeping with cystic changes on cut sections.
Figure 4.
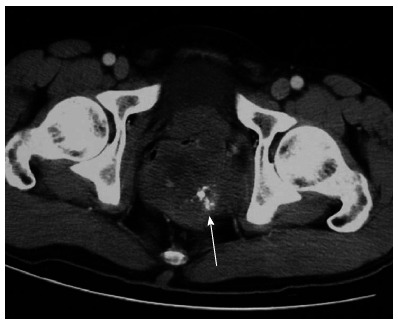
A 52-year-old man with a rectal gastrointestinal stromal tumor. The mass is located in the left posterior wall of the rectum with scattered calcification (arrow).
Figure 5.
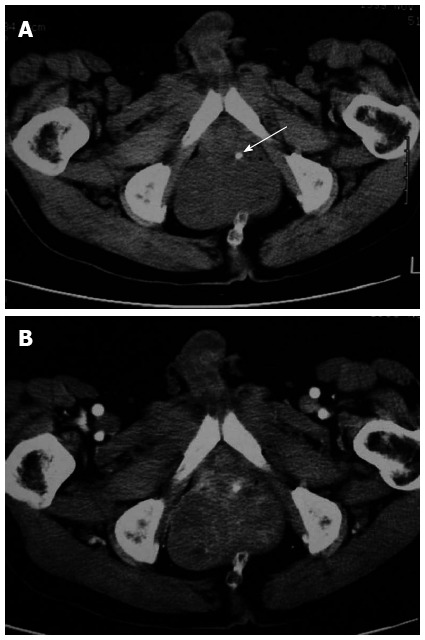
A 61-year-old man with a rectal gastrointestinal stromal tumor. A: The mass located in the left wall of the rectum with fleck of calcification at the tumor margin (arrow); B: The mass enhanced heterogeneously following intravenous administration of contrast media.
Figure 6.
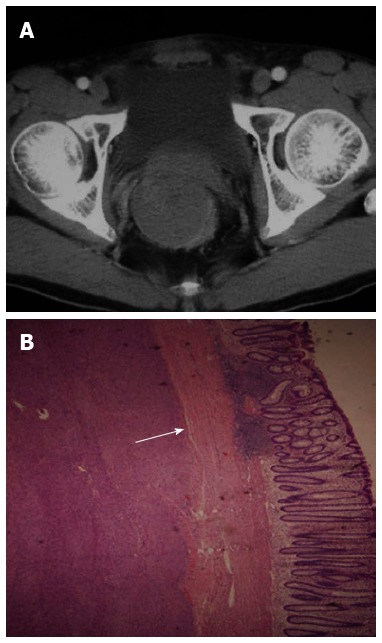
A 53-year-old man with a rectal gastrointestinal stromal tumor. A: Computed tomography scan shows a round intraluminal mass with a sharp margin; B: Photomicrograph shows the tumor originating from the muscularis propria (arrow) of the rectum (hematoxylin and eosin, × 20).
In the 11 cases examined with MRI, the solid component of all the tumors was isointense to skeletal muscle on T1-weighted images and hyperintense on T2-weighted images. There were some intratumoral high-intensity foci on T1WI representing hemorrhage (n = 1) (Figure 3) and hyperintensity on T2WI corresponding to necrosis (n = 8) (Figure 7). Nine of these 11 tumors were heterogeneous, with non-enhancing components showing fluid signal. After intravenous administration of gadolinium, 7 lesions had moderate enhancement and 4 lesions had mild enhancement on fat-suppressed T1WI. Ulceration to the rectal lumen was seen in 1 patient (Figure 8). Bowel obstruction, abdominal adenopathy and remote metastasis were not seen in any of our patients.
Figure 7.

A 59-year-old woman with a rectal gastrointestinal stromal tumor. The mass is located between the uterus and the anterior rectal wall with focal fluid signal on T2WI corresponding to necrosis (arrow).
DISCUSSION
Although an increasing amount of literature concerning GISTs has been published, there is little information reported on the radiological features of rectal GISTs due to their rarity. To our knowledge, this article is the largest study of rectal GISTs in the radiological literature.
Clinical characteristics
It was reported that rectal GISTs occur in adults between the fifth and sixth decades with a significant male predominance (71%)[9]. In this study, there was a marked male predominance with a male: female ratio of 13:1, and the mean age at onset was 51.5 years, in line with the pathological literature. The clinical manifestations of rectal GISTs depend on the location and size of the tumors and are often nonspecific[10-12]. A GIST can remain clinically silent and present late when the tumor is large. Two of our patients were asymptomatic and the tumors were incidental findings, perhaps due to their small size (less than 3.0 cm in maximum diameter) and tendency to grow exophytically. The exophytic growth pattern may also explain why rectal GISTs rarely cause intestinal obstruction even when they are large. Miettinen et al[9] reported that rectal bleeding was the most common symptom in patients with a large rectal GIST more than 5 cm. In this study, the most frequent symptom was also hematochezia.
Imaging features
Rectal GISTs generally manifest as large eccentric masses growing beyond the rectal wall[3-6]. Our series showed a similar growth pattern. Although larger tumors have a higher rate of malignancy, size does not predict benignity, and small GISTs have been known to behave in a malignant fashion[13-16]. Since most rectal GISTs arise within the muscularis propria of the intestinal wall, they most commonly have an exophytic growth pattern with the epicenter located well outside the rectum[17,18]. GISTs arising from the anterior rectal wall in male patients can even mimic tumors of prostatic origin on CT[19,20]. Thus, the classic rule regarding determination of the organ of origin based on the location of the epicenter of a tumor is often not applicable. In such cases, enhanced MRI should be performed. MRI with direct multiplanar capability is definitely more useful in determining the exact tumor origin, delineating the spatial relation to adjacent structures, and outlining the pelvic floor surgical anatomy. In our study, tumor-rectal wall continuity was revealed in the sagittal plane, which suggested the diagnosis of a rectal mass. On the other hand, invasion of adjacent organs was better seen on MRI compared with CT examination.
In this study, most of the tumors were round or oval and smooth with well-defined margins. On unenhanced CT, rectal GISTs appear as isodense with normal muscle as the standard for comparison. On unenhanced MRI, rectal GISTs appear as isointense to skeletal muscle on T1-weighted images and hyperintense on T2-weighted images, and moderately or mildly enhanced on CT and/or MR studies. A heterogeneous pattern of enhancement is more common on CT and/or MR studies, and was present in 11 of our cases. Heterogeneity corresponds to intralesional necrosis or hemorrhage, which was confirmed on cut sections. It is likely that MRI may be superior to CT in detecting the internal component. Only one of our patients underwent both CT and MRI, and the tumor was homogenous on CT scan, but was heterogeneous with fluid signal on MR images.
Although calcification is not a usual clinicopathologic feature of GISTs, it has been reported in previous studies[21-23]. Most calcifications within GISTs are circumscribed and patchy. In our study, one of the two calcified tumors showed focal calcification and the other was mottled. Previous episodes of bleeding or tumor necrosis with cystic degeneration may cause calcification[24,25]. Because these tumors are submucosal, the overlying mucosa can be intact. However, overlying mucosal ulcerations are often present and cause bleeding, and are more common in high risk GISTs[26-28].
Differential diagnosis
Unfortunately, there is significant overlap between the imaging appearances of rectal GISTs and other rectal diseases, such as epithelial neoplasms, lymphoma or carcinoids. Most of these tumors may be differentiated from rectal GISTs by the presence of the following features: well-demarcated margins, prominent extraluminal location and no surrounding adenopathy, and the lack of bowel lumen constriction despite the large size of the rectal GIST. This behavior is unlike most cases of adenocarcinoma which has a propensity for luminal obstruction. The appearance of a smooth regular border is a feature that allows these tumors to be differentiated from malignant epithelial neoplasms. Signs of intratumoral degeneration, such as cystic change, hemorrhage, and calcification, should exclude lymphoma from the differential diagnosis.
Due to the submucosal origin of the tumors, endoscopy is only of use when the tumor infiltrates the mucosa and can be detected[29]. In addition to endoscopy, endoscopic ultrasonography is a valuable technique in the diagnosis of these tumors because it can reliably distinguish intramural lesions from extrinsic compression. Enhanced MRI with an endoluminal coil has been performed to determine the tumor origin in some reported cases[30-32], but these procedures are invasive, and are rarely used in routine examinations.
Pathological features
CD117 is the most specific and important diagnostic molecular marker of GISTs. Most GISTs (more than 95%) express CD117, which can be detected immunohistochemically[9,33]. Although CD117-positive expression is very common in GISTs and a major defining characteristic of GISTs, it is not absolutely necessary for the diagnosis of GISTs. CD34 is also commonly expressed in GISTs, which is less specific compared with CD117 and is not considered a requirement for the diagnosis of GISTs either[34-36]. The review of pathology in our patients showed that the tumors were strongly positive for CD117 and in most cases also CD34, consistent with previous reports.
The pathologic differentiation and biologic behavior of GISTs have been continuing topics of controversy for many years. A small number of GISTs recur or metastasize despite a histologically benign appearance. Therefore, some authors support stratifying GISTs into very low-, low-, intermediate-, and high-risk categories rather than classifying them as benign or malignant. The NIH risk classification system, which consists of tumor size, mitotic count (number of mitoses per 50 consecutive high-power fields), anatomic location, and tumor rupture, is recommended as a valuable tool for estimating the clinical behavior of GISTs[8]. Rectal GISTs have a high-risk tendency[23] which was observed in the majority of our patients.
Attempts to predict the potential high-risk behavior of GISTs from their imaging features is difficult. It was reported that GISTs with irregular margins, size larger than 10 cm, central necrosis, ulceration, and heterogeneous contrast enhancement are normally regarded as denoting aggression[37,38]. These signs are mainly derived from a study population of stomach and small intestine GISTs and seldom from rectal GISTs. However, our series is small and no correlation between radiologic appearance and risk levels could be established with regard to the degree of necrosis, hemorrhage, ulceration, or contrast material enhancement.
There are several limitations in this study. The study was retrospective and the reviewers of the imaging studies knew that all patients had a pathologically confirmed rectal GIST, which may have increased the sensitivity for detecting each imaging sign. In addition, different CT and MRI equipment and techniques were used. However, these problems are simply unavoidable due to the rarity of this type of tumor, and this should not have significantly affected the imaging features studied.
In summary, we present the largest series of radiological studies of rectal GISTs to date. These tumors often present with hematochezia. They are normally seen as large, bulky, exophytic rectal masses with heterogenous enhancement on CT and MRI. Cross-sectional imaging, which allows better visualization of the origin of the mass, its internal components, and other organ involvement, is indicated for surgical planning.
COMMENTS
Background
Rectal gastrointestinal stromal tumors (GISTs) are very rare, which accounts for 0.6% of all rectal malignant tumors. Only a few reports concerning the radiological features of rectal GIST has been published due to its rarity. Surgical resection remains the mainstay of therapy for localized rectal GISTs, familiarity of their radiological features may permit preoperative diagnosis and improves surgical management of patients. Thus, it is very important to enhance the understanding of the imaging features of this rare tumor.
Research frontiers
The current imaging knowledge of rectal GISTs is based on a few case reports. Grassi et al reported a 4-cm mass in a 70-year-old man that showed marked, irregular, eccentric thickening of the lateral left wall of the lower third of the rectum. Hama et al reported a 9.8-cm mass in a 50-year-old man that was contiguous with the prostate and enhanced on both computed tomography (CT) and magnetic resonance imaging (MRI). Levy et al reported six anorectal gastrointestinal stromal tumors, and found that anorectal GISTs were typically large, well-demarcated anorectal masses containing hemorrhage.
Innovations and breakthroughs
This study contained a relative large cohort of cases of rectal GISTs confirmed by histology and immunochemistry. All the patients had a complete medical records including age, gender, presenting symptoms, endoscopic examinations, surgical notes and pre-operative cross-sectional imaging studies. The authors focused on the correlation of imaging features of this rare tumor with clinical and pathological characteristics.
Applications
Rectal GISTs are normally seen as large, bulky, exophytic rectal masses with heterogenous enhancement on CT and MRI. Cross-sectional imaging, which allows better visualization of the origin of the mass, its internal components, and other organ involvement, is indicated for surgical planning.
Terminology
GIST is the most common mesenchymal neoplasm of the gastrointestinal tract, which arises from the interstitial cell of Cajal or its precursor. The rectum is the rare primary site involving about 5% cases. Due to the submucosal origin of the rectal GISTs, the presence of the following features allows these tumors to be differentiated from malignant epithelial neoplasms: well-demarcated margins, prominent extraluminal location and no surrounding adenopathy, and the lack of bowel lumen constriction despite the large size of the tumor.
Peer review
The authors reported imaging features of rectal gastrointestinal stromal tumors with clinical and pathological correlation. The main strength of this study is the relatively large number (n = 14) of patients and broader spectrum of imaging findings in this rare tumor. The findings are instructive to both radiologists and physicians.
Footnotes
Supported by Key Program of Shanghai Science and Technology Commission, No. 09441900500
P- Reviewers Chen F, Nouh MR S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Tryggvason G, Kristmundsson T, Orvar K, Jónasson JG, Magnússon MK, Gíslason HG. Clinical study on gastrointestinal stromal tumors (GIST) in Iceland, 1990-2003. Dig Dis Sci. 2007;52:2249–2253. doi: 10.1007/s10620-006-9248-4. [DOI] [PubMed] [Google Scholar]
- 2.Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100:162–168. doi: 10.1111/j.1572-0241.2005.40709.x. [DOI] [PubMed] [Google Scholar]
- 3.Lau S, Lui CY, Yeung YP, Lam HS, Mak KL. Gastrointestinal stromal tumor of rectum: a report of 2 cases. J Comput Assist Tomogr. 2003;27:609–615. doi: 10.1097/00004728-200307000-00028. [DOI] [PubMed] [Google Scholar]
- 4.Levy AD, Remotti HE, Thompson WM, Sobin LH, Miettinen M. Anorectal gastrointestinal stromal tumors: CT and MR imaging features with clinical and pathologic correlation. AJR Am J Roentgenol. 2003;180:1607–1612. doi: 10.2214/ajr.180.6.1801607. [DOI] [PubMed] [Google Scholar]
- 5.Grassi N, Cipolla C, Torcivia A, Mandala S, Graceffa G, Bottino A, Latteri F. Gastrointestinal stromal tumour of the rectum: report of a case and review of literature. World J Gastroenterol. 2008;14:1302–1304. doi: 10.3748/wjg.14.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chekrine T, Jouhadi H, Bouchbika Z, Benchakroun N, Tawfiq N, Sahraoui S, Benider A. Gastrointestinal stromal tumour of the rectum: a report of two cases. Pan Afr Med J. 2012;12:19. [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CW, Wu CC, Hsiao CW, Fang FC, Lee TY, Che FC, Tsai WC, Jao SW. Surgical management and clinical outcome of gastrointestinal stromal tumor of the colon and rectum. Z Gastroenterol. 2008;46:760–765. doi: 10.1055/s-2008-1027243. [DOI] [PubMed] [Google Scholar]
- 8.Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39:1411–1419. doi: 10.1016/j.humpath.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 9.Miettinen M, Furlong M, Sarlomo-Rikala M, Burke A, Sobin LH, Lasota J. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the rectum and anus: a clinicopathologic, immunohistochemical, and molecular genetic study of 144 cases. Am J Surg Pathol. 2001;25:1121–1133. doi: 10.1097/00000478-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Kourda N, Kourda J, Aouam J, Zaouche A, Ben Jilani SB, Zermani R. Rectal leiomyosarcoma: report on two cases and a practical approach to differential diagnosis. Pathologica. 2010;102:417–419. [PubMed] [Google Scholar]
- 11.Anagnostou E, Miliaras D, Panagiotakopoulos V. Diagnosis of gastrointestinal stromal tumor (GIST) on transurethral resection of the prostate: a case report and review of the literature. Int J Surg Pathol. 2011;19:632–636. doi: 10.1177/1066896911408304. [DOI] [PubMed] [Google Scholar]
- 12.Yoon KJ, Kim NK, Lee KY, Min BS, Hur H, Kang J, Lee S. Efficacy of imatinib mesylate neoadjuvant treatment for a locally advanced rectal gastrointestinal stromal tumor. J Korean Soc Coloproctol. 2011;27:147–152. doi: 10.3393/jksc.2011.27.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amato A. Colorectal gastrointestinal stromal tumor. Tech Coloproctol. 2010;14 Suppl 1:S91–S95. doi: 10.1007/s10151-010-0631-y. [DOI] [PubMed] [Google Scholar]
- 14.Rossi S, Gasparotto D, Toffolatti L, Pastrello C, Gallina G, Marzotto A, Sartor C, Barbareschi M, Cantaloni C, Messerini L, et al. Molecular and clinicopathologic characterization of gastrointestinal stromal tumors (GISTs) of small size. Am J Surg Pathol. 2010;34:1480–1491. doi: 10.1097/PAS.0b013e3181ef7431. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki T, Sadahiro S, Tanaka A, Okada K, Okamura H, Machida T, Kumaki N. Gastrointestinal stromal tumor of the rectum: report of three cases. Tokai J Exp Clin Med. 2011;36:58–62. [PubMed] [Google Scholar]
- 16.de Azevedo CR, Paiva TF, Rossi BM, Guimarães GC, de Souza Begnami MD, Oliveira TB, Barros E Silva MJ, Fanelli MF, de Mello CA. Pathologic complete response with neoadjuvant imatinib for locally advanced pelvic GIST. Int J Clin Oncol. 2011;16:279–283. doi: 10.1007/s10147-010-0133-y. [DOI] [PubMed] [Google Scholar]
- 17.Takano M, Saito K, Kita T, Furuya K, Aida S, Kikuchi Y. Preoperative needle biopsy and immunohistochemical analysis for gastrointestinal stromal tumor of the rectum mimicking vaginal leiomyoma. Int J Gynecol Cancer. 2006;16:927–930. doi: 10.1111/j.1525-1438.2006.00217.x. [DOI] [PubMed] [Google Scholar]
- 18.Dickhoff C, Leguit RJ, Slors JF, Vervenne WL, Bemelman WA. Giant rectal gastrointestinal stromal tumors: a report of two cases. Case Rep Gastroenterol. 2008;2:54–69. doi: 10.1159/000119317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madden JF, Burchette JL, Raj GV, Daly JT, Tannenbaum M. Anterior rectal wall gastrointestinal stromal tumor presenting clinically as prostatic mass. Urol Oncol. 2005;23:268–272. doi: 10.1016/j.urolonc.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Hiromura T, Nishioka T, Nishioka S, Ikeda H, Tomita K. Anorectal gastrointestinal stromal tumor mimicking prostatic tumor on CT and MRI. Euro J Radiol Extra. 2005;53:115–118. [Google Scholar]
- 21.Testroote M, Hoornweg M, Rhemrev S. Rectal GIST presenting as a submucosal calculus. Dig Dis Sci. 2007;52:1047–1049. doi: 10.1007/s10620-006-9160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ong K, Singaporewalla RM, Tan KB. Extensive calcification within a gastrointestinal stromal tumour: a potential diagnostic pitfall. Pathology. 2006;38:451–452. doi: 10.1080/00313020600924922. [DOI] [PubMed] [Google Scholar]
- 23.Liegl-Atzwanger B, Fletcher JA, Fletcher CD. Gastrointestinal stromal tumors. Virchows Arch. 2010;456:111–127. doi: 10.1007/s00428-010-0891-y. [DOI] [PubMed] [Google Scholar]
- 24.Dickson AM, Schuss A, Goyal A, Katz DS. Radiology-Pathology Conference: Calcified untreated gastric cancer. Clin Imaging. 2004;28:418–421. doi: 10.1016/j.clinimag.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Yoshida H, Mamada Y, Taniai N, Mizuguchi Y, Nakamura Y, Nomura T, Okuda T, Uchida E, Fukuda Y, Watanabe M, et al. Spurt bleeding from a calcificated gastrointestinal stromal tumor in the stomach. J Nippon Med Sch. 2005;72:304–307. doi: 10.1272/jnms.72.304. [DOI] [PubMed] [Google Scholar]
- 26.Manouras A, Pappas A, Katergiannakis V, Filis K, Chrysikos J, Pattas M, Genetzakis M, Tsekouras D, Lagoudianakis E. Gastrointestinal stromal tumors of the rectum: report of five cases. Acta Gastroenterol Belg. 2009;72:257–261. [PubMed] [Google Scholar]
- 27.Hamada M, Ozaki K, Horimi T, Tsuji A, Nasu Y, Iwata J, Nagata Y. Recurrent rectal GIST resected successfully after preoperative chemotherapy with imatinib mesylate. Int J Clin Oncol. 2008;13:355–360. doi: 10.1007/s10147-007-0735-1. [DOI] [PubMed] [Google Scholar]
- 28.Woźniak A, Rutkowski P, Sciot R, Ruka W, Michej W, Debiec-Rychter M. Rectal gastrointestinal stromal tumors associated with a novel germline KIT mutation. Int J Cancer. 2008;122:2160–2164. doi: 10.1002/ijc.23338. [DOI] [PubMed] [Google Scholar]
- 29.Lev D, Kariv Y, Messer GY, Isakov J, Gutman M. Gastrointestinal autonomic nerve (GAN) tumor of the rectum. J Clin Gastroenterol. 2000;30:438–440. doi: 10.1097/00004836-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Raghunathan G, Mortele KJ. Magnetic resonance imaging of anorectal neoplasms. Clin Gastroenterol Hepatol. 2009;7:379–388. doi: 10.1016/j.cgh.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Iwa N, Shiozaki K, Izawa H, Baba M, Kanai T, Kobayashi Y, Kobayashi TK, Takami M. Gastrointestinal stromal tumor arising from anorectum: correlation of imprint cytology and radiologic imaging. Ann Diagn Pathol. 2007;11:212–216. doi: 10.1016/j.anndiagpath.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Baik SH, Kim NK, Lee CH, Lee KY, Sohn SK, Cho CH, Kim H, Pyo HR, Rha SY, Chung HC. Gastrointestinal stromal tumor of the rectum: an analysis of seven cases. Surg Today. 2007;37:455–459. doi: 10.1007/s00595-006-3424-1. [DOI] [PubMed] [Google Scholar]
- 33.Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 34.Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006;130:1466–1478. doi: 10.5858/2006-130-1466-GSTROM. [DOI] [PubMed] [Google Scholar]
- 35.Burkill GJ, Badran M, Al-Muderis O, Meirion Thomas J, Judson IR, Fisher C, Moskovic EC. Malignant gastrointestinal stromal tumor: distribution, imaging features, and pattern of metastatic spread. Radiology. 2003;226:527–532. doi: 10.1148/radiol.2262011880. [DOI] [PubMed] [Google Scholar]
- 36.Ghanem N, Altehoefer C, Furtwängler A, Winterer J, Schäfer O, Springer O, Kotter E, Langer M. Computed tomography in gastrointestinal stromal tumors. Eur Radiol. 2003;13:1669–1678. doi: 10.1007/s00330-002-1803-6. [DOI] [PubMed] [Google Scholar]
- 37.Machado-Aranda D, Malamet M, Chang YJ, Jacobs MJ, Ferguson L, Silapaswan S, Goriel Y, Kolachalam R, Mittal VK. Prevalence and management of gastrointestinal stromal tumors. Am Surg. 2009;75:55–60. [PubMed] [Google Scholar]
- 38.Jakob J, Mussi C, Ronellenfitsch U, Wardelmann E, Negri T, Gronchi A, Hohenberger P. Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Ann Surg Oncol. 2013;20:586–592. doi: 10.1245/s10434-012-2647-1. [DOI] [PubMed] [Google Scholar]


