Abstract
It has been reported recently that small undifferentiated intramucosal early gastric cancer (EGC) < 20 mm in size without any lymphovascular involvement or ulcerative findings had virtually no risk of lymph-node (LN) metastasis. Consequently, the indications for endoscopic resection were expanded to include such undifferentiated EGC lesions. We describe herein a case of a small undifferentiated intramucosal EGC < 20 mm in size without lymphovascular involvement or ulcerative findings that involved lymph-node metastasis. A 57-year-old female underwent pylorus preserving gastrectomy as standard treatment for an undifferentiated EGC 15 mm in size without any ulcerative finding. The surgical specimen revealed a signet-ring cell carcinoma with a moderately to poorly differentiated adenocarcinoma limited to the mucosa that was 15 mm in size with no lymphovascular involvement or ulcerative findings. This case involved LN metastasis, however, and the lesion was diagnosed as pathological stage IIA (T1N2M0) according to the Japanese Classification of Gastric Carcinoma.
Keywords: Early gastric cancer, Endoscopic submucosal dissection, Expanded indications, Lymph-node metastasis, Undifferentiated type
Core tip: Herein is described rare case of small undifferentiated intramucosal early gastric cancer (EGC) < 20 mm in size with lymph-node (LN) metastasis. It has been reported recently that small undifferentiated intramucosal EGC < 20 mm in size without lymphovascular involvement or ulcerative findings had virtually no risk of LN metastasis. Therefore, such small undifferentiated EGCs have become candidates for endoscopic resection. It was within this context we experienced the present case involving a small undifferentiated intramucosal EGC < 20 mm in size without lymphovascular involvement or ulcerative findings that evidenced LN metastasis.
INTRODUCTION
Endoscopic resection (ER) is generally indicated for early gastric cancer (EGC) with no risk of lymph-node (LN) metastasis. Hirasawa et al[1] reported there was virtually no risk of LN metastasis in undifferentiated EGCs < 20 mm in size without lymphovascular involvement or ulcerative findings and such lesions could satisfy the indications for ER. We encountered, however, a case of a small undifferentiated intramucosal EGC meeting all of the above-mentioned criteria that actually involved LN metastasis and decided to report this seemingly rare occurrence.
CASE REPORT
A 57-year-old female underwent an esophagogastroduodenoscopy (EGD) for a medical check-up in December 2008. The results indicated gastric cancer, and she was referred to our hospital for treatment. The EGD revealed a pale depressed mucosal lesion that was Type 0-IIc in accordance with the Japanese Classification of Gastric Carcinoma (JCGC)[2] located on the anterior wall of the middle gastric body (Figure 1). The size of the lesion was approximately 15 mm, and there was no ulcerative finding. The biopsy specimen revealed a signet-ring cell carcinoma. Computed tomography (CT) indicated no distinct regional LN or distant metastasis. Laboratory results were within normal limits and the serum carcinoembryonic antigen level was normal. We diagnosed this lesion as clinical (c) T1(M), cN0, cM0, cStageIA according to the JCGC; therefore, pylorus preserving gastrectomy was performed as the standard treatment. The surgical specimen revealed a signet-ring cell carcinoma with a moderately to poorly differentiated adenocarcinoma limited to the mucosa without lymphovascular involvement or ulcerative findings (Figures 2 and 3A-E). The lesion was 15 mm × 12 mm in size, and the resection margin was free of tumor cells. In addition, tumor cells were positive for mucin (MUC)5AC and negative for MUC6 with an MUC5AC/MUC6 double layer and Ki-67 localization both absent (Figure 4). Some portions of the resected regional LNs (lesser curvature LNs; LN station 3), however, included metastatic cancer cells (3/32) that were also identified as a signet-ring cell carcinoma (Figure 3F). This lesion was then diagnosed as pathological (p)T1(M), ly0, v0, pN2, pM0, pStage IIA according to the JCGC. Four years after surgery, the patient was in good condition and disease free without any signs of tumor recurrence based on the latest follow-up EGD and CT examinations.
Figure 1.
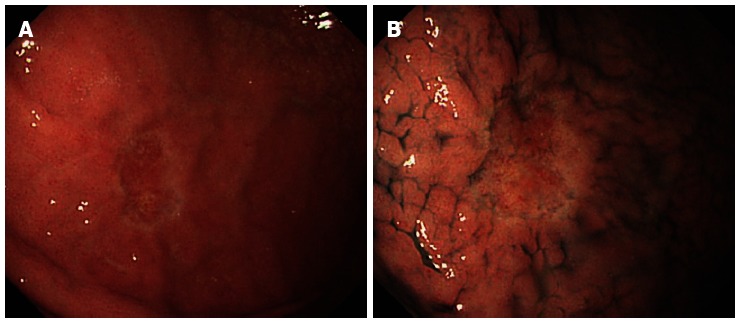
Pre-treatment endoscopic examination. Esophagogastroduodenoscopy revealed pale depressed mucosal lesion on anterior wall of middle gastric body approximately 15 mm in size with no ulcerative finding and non-atrophic background mucosa. A: Conventional white light endoscopy; B: With indigo-carmine dye staining.
Figure 2.
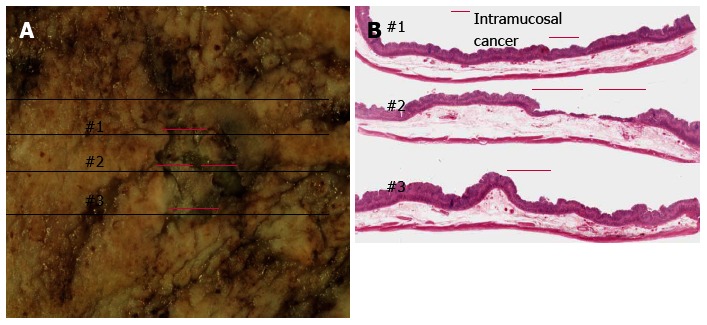
Surgically resected specimen. A: Formalin-fixed specimen from pylorus preserving gastrectomy; B: Panoramic view of lesion with hematoxylin and eosin staining. Mucosal lesion 15 mm × 12 mm in size with no ulcer finding and pink lines corresponding to lesion depression (hematoxylin and eosin staining, × 1).
Figure 3.
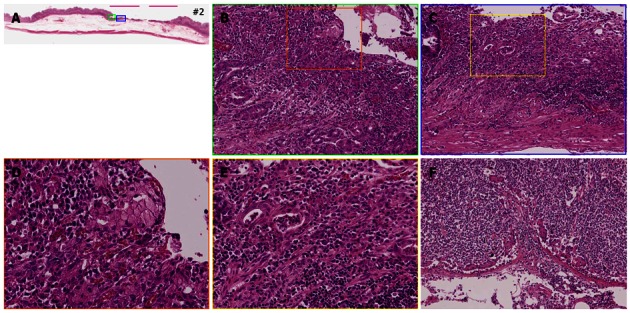
Histopathological findings. A: Panoramic view with hematoxylin and eosin staining (× 1); B: Signet-ring cell carcinoma identified at lesion edge (green frame in A, × 40); C: Moderately to poorly differentiated adenocarcinoma limited to mucosa visible in lesion center. Low magnification view (bule frame in A, × 40); D: High magnification view of red frame in B (× 200); E: High magnification view of yellow frame in C (× 200); F: Image showing signet-ring cell carcinoma invasion of station 3 lymph node (N2) (× 40).
Figure 4.
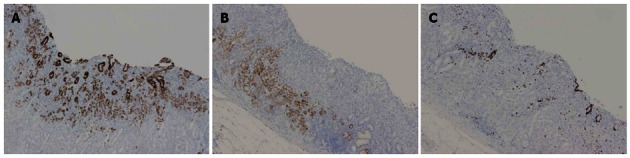
Immunochemical staining. Tumor cells positive for mucin (MUC)5AC (A, × 10) and negative for MUC6 with an MUC5AC/MUC6 double layer (B, × 4)and Ki-67 (C, × 4) localization both absent.
DISCUSSION
ER is widely accepted as a minimally invasive treatment for intramucosal EGC with virtually no risk of LN metastasis[2-6]. An earlier report, however, demonstrated undifferentiated intramucosal EGC had a higher probability of LN metastasis (4.2%)[3], and gastrectomy with regional lymphadenectomy has been considered essential treatment for such lesions. More recently, Hirasawa et al[1] reported small undifferentiated intramucosal EGCs < 20 mm in size without lymphovascular involvement or ulcerative findings had virtually no risk of LN metastasis (95%CI, up to 0.96%). Therefore, such small undifferentiated EGCs have become candidates for ER. It was within this context we experienced the present case involving a small undifferentiated intramucosal EGC < 20 mm in size without any lymphovascular involvement or ulcerative findings that evidenced LN metastasis.
Both Nasu et al[7] and Park et al[8] previously reported similar cases of a small undifferentiated intramucosal EGC < 20 mm in size (13 and 17mm, respectively) without lymphovascular involvement or findings of ulceration that involved LN metastasis. In addition, Abe et al[9] reported three cases involving LN metastasis of small undifferentiated intramucosal EGCs < 20 mm in size (10, 12 and 20 mm, respectively) without any ulcerative findings and concluded ER should not be indicated for undifferentiated EGCs > 10 mm in size. There was no reference in those three cases, however, regarding the existence of lymphovascular involvement. Hirasawa et al[10] also reported a case with LN metastasis of a small undifferentiated intramucosal EGC that was 13 mm in size and without an ulcerative finding. According to their case report, routine histological examination of the endoscopic submucosal dissection specimen sectioned at intervals of 2 mm indicated an intramucosal tumor without lymphovascular involvement or ulceration. Hematoxylin and eosin staining of one of the 60 additional deep-cut sections of the original resected specimen, however, revealed lymphatic involvement in the mucosa. The authors then suggested practical limitations in determining lymphovascular involvement through routine histological examinations may not always facilitate the detection of LN metastasis.
Based on the various published reports supportive of the findings in our particular case, the possibility of LN metastasis developing from a small undifferentiated intramucosal EGC < 20 mm in size without ulceration exists even if there is no apparent lymphovascular involvement[7,8]. It is highly desirable, therefore, to clarify the predictive factors for the development of LN metastasis with such small undifferentiated intramucosal EGCs. Takizawa et al[11] evaluated the conditions in which LN metastasis was unlikely and ER of undifferentiated EGCs had a greater probability of being effective. Such conditions included intramucosal cancers without lymphovascular involvement or ulcerative findings and: (1) lesions < 10 mm in size; (2) the presence of Ki-67 localization; (3) the presence of a double layer (MUC5AC/MUC6); and/or (4) the presence of only a signet-ring cell carcinoma. The conditions in our case included a lesion > 10 mm in size, the absence of Ki-67 localization, the absence of a double layer (MUC5AC/MUC6), and the presence of not only a signet-ring cell carcinoma but also a moderately and poorly differentiated adenocarcinoma. In addition, more recently, Takizawa et al[12] reported that LN metastasis was significantly more common in mixed predominantly undifferentiated (MU)-type intramucosal cancer than in pure undifferentiated (PU)-type intramucosal cancer and concluded MU-type tumors might have greater malignant potential than PU-type tumors. Actually, the present case was MU-type intramucosal cancer with lymph-node metastasis.
If it were possible to evaluate the pathology of all resected specimens in detail using deep-cut sections and immunohistochemical staining as indicated in the above-mentioned reports[10-12], we might be able to predict those cases in which LN metastasis of small undifferentiated intramucosal EGCs would most likely occur, but it is not always feasible to perform such extensive pathological evaluations in clinical practice. We need to recognize the distinct possibility, therefore, of LN metastasis developing from small undifferentiated intramucosal EGCs < 20 mm in size without lymphovascular involvement or ulcerative findings because of the practical limitations related to such histological examinations[10]. It is, therefore, imperative that physicians thoroughly explain the possibility of LN metastasis to patients before performing ER for small undifferentiated intramucosal EGCs so as to obtain their informed consent and then conduct more careful follow-up surveillance examinations including CT scans, ultrasonography and/or EUS in addition to EGDs subsequent to ER treatment.
In order to satisfactorily demonstrate the validity of treating small undifferentiated intramucosal EGCs with ER, a large prospective study analyzing therapeutic outcomes will need to be conducted in the near future before the recently expanded indications for treating such lesions with ER should be accepted for general clinical use.
ACKNOWLEDGMENTS
The authors wish to express their appreciation to Christopher Dix for his assistance in editing this manuscript.
Footnotes
P- Reviewer Hoeppner J S- Editor Zhai HH L- Editor A E- Editor Lu YJ
References
- 1.Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, Fujisaki J, Sano T, Yamaguchi T. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–152. doi: 10.1007/s10120-009-0515-x. [DOI] [PubMed] [Google Scholar]
- 2.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 3.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 4.Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229. doi: 10.1136/gut.48.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oda I, Gotoda T, Hamanaka H, Eguchi T, Saito Y, Matsuda T, Bhandari P, Emura F, Saito D, Ono H. Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Dig Endosc. 2005;17:54–58. [Google Scholar]
- 6.Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer. 2007;10:1–11. doi: 10.1007/s10120-006-0408-1. [DOI] [PubMed] [Google Scholar]
- 7.Nasu J, Hori S, Asagi A, Nishina T, Ikeda Y, Tanimizu M, Iguchi H, Aogi K, Kurita A, Nishimura R. A case of small undifferentiated intramucosal gastric cancer with lymph node metastasis. Gastric Cancer. 2010;13:264–266. doi: 10.1007/s10120-010-0562-3. [DOI] [PubMed] [Google Scholar]
- 8.Park YD, Chung YJ, Chung HY, Yu W, Bae HI, Jeon SW, Cho CM, Tak WY, Kweon YO. Factors related to lymph node metastasis and the feasibility of endoscopic mucosal resection for treating poorly differentiated adenocarcinoma of the stomach. Endoscopy. 2008;40:7–10. doi: 10.1055/s-2007-966750. [DOI] [PubMed] [Google Scholar]
- 9.Abe N, Watanabe T, Sugiyama M, Yanagida O, Masaki T, Mori T, Atomi Y. Endoscopic treatment or surgery for undifferentiated early gastric cancer? Am J Surg. 2004;188:181–184. doi: 10.1016/j.amjsurg.2003.12.060. [DOI] [PubMed] [Google Scholar]
- 10.Hirasawa T, Fujisaki J, Fukunaga T, Yamamoto Y, Yamaguchi T, Katori M, Yamamoto N. Lymph node metastasis from undifferentiated-type mucosal gastric cancer satisfying the expanded criteria for endoscopic resection based on routine histological examination. Gastric Cancer. 2010;13:267–270. doi: 10.1007/s10120-010-0577-9. [DOI] [PubMed] [Google Scholar]
- 11.Takizawa K, Shimoda T, Nakanishi Y, Taniguchi H, Oda I, Gotoda T. Expanded indication of endoscopic resection from the pathological viewpoint-the ability of sm invasion of early gastric cancer of undifferentiated type. Stomach Intes. 2006;41:9–17. [Google Scholar]
- 12.Takizawa K, Ono H, Kakushima N, Tanaka M, Hasuike N, Matsubayashi H, Yamagichi Y, Bando E, Terashima M, Kusafuka K, et al. Risk of lymph node metastases from intramucosal gastric cancer in relation to histological types: how to manage the mixed histological type for endoscopic submucosal dissection. Gastric Cancer. 2012:Nov 29; [Epub ahead of print]. doi: 10.1007/s10120-012-0220-z. [DOI] [PubMed] [Google Scholar]


