Abstract
Lemierre's syndrome is characterized by anaerobic septicemia, internal jugular vein thrombosis, and septic emboli associated with infections of the head and neck. We describe an unusual and clinically confusing case of a young woman with an acute paresis of the abducens nerve and partial paresis of the right oculomotor nerve. After an extensive imaging diagnostic procedure, we also documented a peritonsillar abscess and various types of thromboses in intracranial and extracranial veins. Furthermore, we found brain and lung abscesses, which led us to establish the diagnosis of Lemierre's syndrome. Despite intensive anti-coagulation and antibiotic therapy, the patient developed a mycotic aneurysm in the right internal carotid artery directly adjacent to the previously thrombosed cavernous sinus. In summary, we were able to confirm that Lemierre's syndrome may occur in conjunction with uncharacteristic symptoms. Due to the sometimes confusing clinical symptoms as well as clinical and radiological specialties, we had to work on an interdisciplinary basis to minimize the delay prior to establishing the diagnosis and therapy.
Keywords: Lemierre syndrome, abducens nerve paresis, oculomotor nerve paresis
Lemierre's syndrome was initially described by Lemierre in 1936 [1]. The condition is characterized by anaerobic septicemia, internal jugular vein (IJV) thrombosis, and septic emboli associated with infections of the head and neck. In fact, Courmant and Cade [2] were the first to describe this condition in 1900.
Lemierre's syndrome frequently starts as an acute but harmless oropharyngeal infection. In especially aggressive forms and in rare cases, the infection may spread to deeper regions of the soft tissues of the neck, eventually leading to thrombophlebitis and septic emboli. The overall condition is then referred to as Lemierre's syndrome [3]. Fusobacterium necrophorum is the most common organism implicated in Lemierre's syndrome [4], which has a number of diverse clinical facets. The principal problem, however, is the presence of septic emboli in the lung and brain, accompanied by the formation of abscesses [5]. The use of modern broad-spectrum antibiotics has markedly reduced mortality rates (currently 6%) [6].
The reason why patients may experience severe damage due to Lemierre's syndrome is due to the diversity and subsequent confusing nature of clinical symptoms, causing a potential delay in diagnosis; this might result in lethal outcomes for patients [7]. Because patients with any of the various symptoms may report at a variety of medical departments and sub-specialties, it is important to adopt an interdisciplinary approach towards the disease. This could allow for more rapid diagnosis and institution of therapy. The general prognosis and outcome for the patient can be markedly improved by early targeted therapy.
Case Report
A 22-year-old woman reported to our emergency department with recent swallowing difficulties and throat pain. The clinical investigation revealed a local inflammation of the tonsils on the left side. The patient was otherwise healthy. A rapid test for group A streptococci was negative and the patient was discharged with a diagnosis of acute tonsillitis and symptomatic therapy with ibubrufen.
Six days later the patient presented at our ophthalmology outpatient department with acute paresis of the abducens nerve and partial paresis of the right oculomotor nerve (Figs. 1 and 2). Signs of paresis of the occulomotor nerve included general mydriasis of the right eye with impairment in function of the musculus levator and general impairment in motion of the right eye. Paresis of the right abducens nerve was seen when the patient was looking to the right side. The prism cover test showed +40 pdpt when looking to the right, a primary position at +20 pdpt when looking to the left +10 pdpt. One week later, the patient also developed a discrete paralysis of the abducens nerve on the left eye. In addition, there was an onset of exophthalmos on the right side (18-95-15), which was documented by the Hertel Exophthalmometer. The fundus and retina showed no pathological signs. Also, the neurological investigation revealed general photophobia, incomplete trismus and discrete signs of meningism together with fever. Hematology and clinical chemistry results were compatible with sepsis indicating substantial inflammation with leucocytosis of 16,000/µL (15,000/µL neutrophils, 45% left shift) and C-reactive protein of 271 g/L, activated coagulation with profound thrombocytopenia (21,000/µL), and an international normalized ratio of 1.27.
Fig. 1.

The patient presented with clinical signs of oculomotor nerve paresis on the right side. As a result, she had a drooping right eyelid. She also demonstrated exophthalmos on the right side.
Fig. 2.

The patient presented with paresis of the abducens nerve in the right eye when looking to the right.
To clarify these inconclusive clinical symptoms, we performed a magnetic resonance imaging (MRI) investigation of the head, which revealed marked thromboses at various locations including the cavernous sinus on both sides (Fig. 3), more pronounced on the right side, and a thrombosis of the superior ophthalmic vein in the right eye (Fig. 4). Moreover, we found a small starting abscess in the right temporal lobe, which grew rapidly (Fig. 5). Due to the numerous symptoms, and the patient's difficulty in opening her mouth, we performed a computed tomography of the neck, which revealed an abscess in the left tonsil with a maximum diameter of 6 mm (Fig. 6). In the right internal jugular vein, we found a partially occluding thrombus. Despite the absence of pulmonary symptoms, we performed an additional computed tomography of the lung, which revealed multiple septic emboli and starting abscesses (Fig. 7).
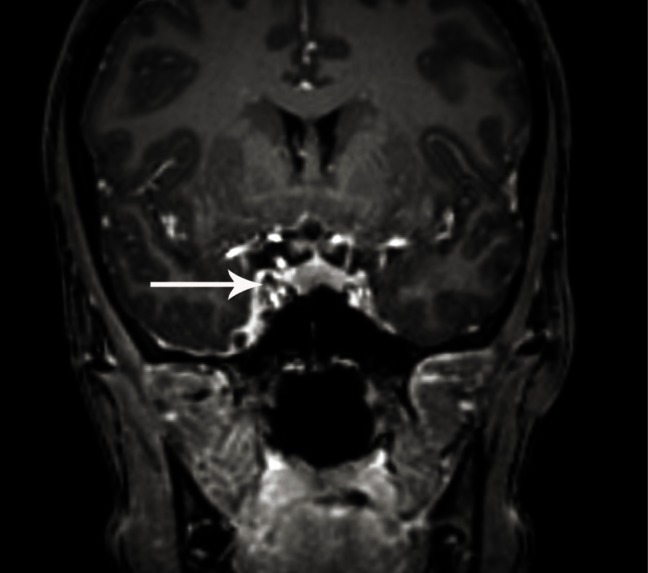
Fig. 3.
Coronal view on 3-D T1-weighted magnetic resonance imaging after administration of gadolinium reveals the cavernous sinus with thrombosis on both sides, but more pronounced on the right side (arrow).
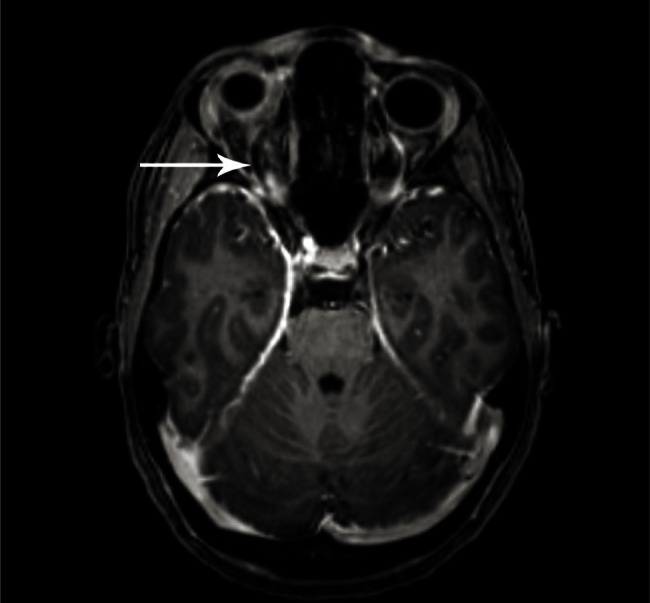
Fig. 4.
Axial view on a 3-D T1-weighted sequence after administration of gadolinium reveals a thrombosis in the superior ophthalmic vein on the right side (arrow).
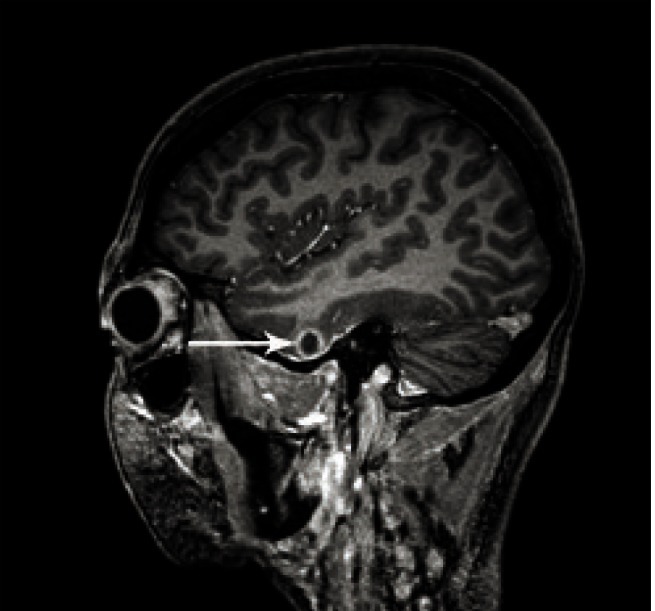
Fig. 5.
Intra-axial brain abscess in the right temporal lobe, which worsened rapidly despite treatment with a broad-spectrum antibiotic (arrow).
Fig. 6.
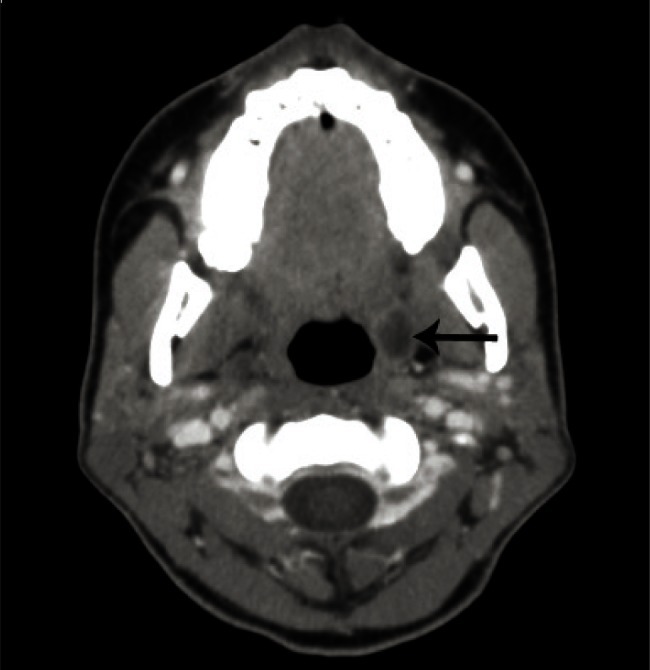
Computed tomography of the neck shows a clearly delineated tonsillary abscess on the left side with a maximum diameter of 1.3 cm.
Fig. 7.

Note the numerous septic emboli in both lungs. The emboli are clearly seen along the bronchovascular bundle.
Given the presence of the peritonsillar abscess and the various types of thromboses in intracranial and extracranial veins, we established a diagnosis of Lemierre's syndrome and started high-dose intravenous antibiotic therapy with amoxicillin/clavulanic acid and clindamycin after taking two pairs of blood cultures. In addition, anticoagulation therapy with 20,000 units of heparin was started because of the presence of numerous venous thrombi. The next day, both anaerobic cultures were positive for Gram-negative pleomorphic bacilli, which were subsequently identified as Fusobacterium necrophorum using 16s-RNA sequencing. With minimal inhibitory concentrations of 0.094 to 0.004 mg/L, the isolate was highly susceptible to penicillin, amoxicillin, ceftriaxon and metronidazole. Operative drainage of the left tonsillary abscess was delayed by 5 days due to thrombocytopenia. Although the patient's general clinical condition seemed to improve gradually, she developed a progressive brain abscess in the right temporal lobe (Fig. 5). As a result, she was switched to ceftriaxon and metronidazole for better penetration of the blood-brain barrier. Nevertheless, the patient developed a mycotic aneurysm in the right internal carotid artery (Fig. 8), directly adjacent to the previously thrombosed cavernous sinus. Due to the risk of aneurysm rupture with major bleeding, the patient was transferred from our hospital to a neurosurgical intensive care unit of a large university clinic. Despite intensive anti-coagulation therapy with heparin, the thromboses in the IJV, the cavernous sinus and the ophthalmic vein as well as the cranial nerve palsy persisted during the first two weeks. Three months after that observation period and an intensive antibiotic therapy, the patient was discharged from the hospital in a very good condition. There was only a discrete residual sign of an abducens nerve paralysis on both sides with emphasis on the right side. The oculomotor nerve paralysis on the right side had completely disappeared without any residual paralysis. The patient had no other complications in this follow-up.
Fig. 8.
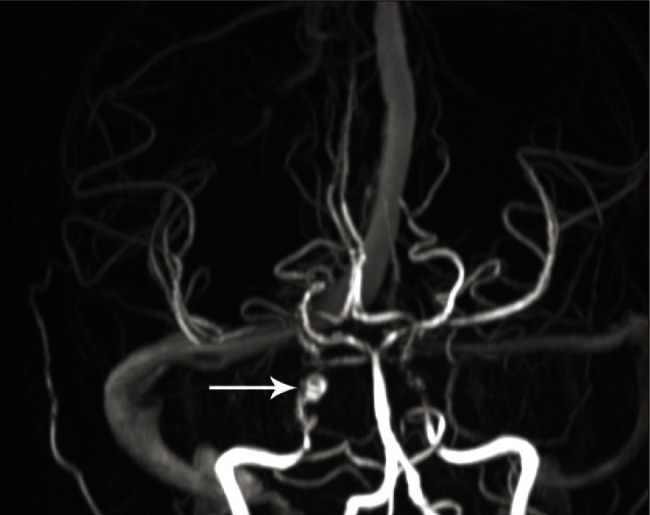
In addition to known venous thrombi, the magnetic resonance angiography revealed a recent mycotic aneurysm in the right internal carotid artery, directly adjacent to the previously thrombosed cavernous sinus on the right side.
Discussion
The definition of Lemierre's syndrome includes acute bacterial pharyngitis, or an oropharyngeal infection leading to aggressive forms of ipsilateral thrombophlebitis [8]. The primary oropharyngeal infection is usually followed by thrombosis in the ipsilateral internal jugular vein. Although the pathogenesis of this condition is not fully understood, it is suspected that the infection in the lateral parapharyngeal cavity causes a hematogenic or lymphogenic connection between the primary infected site in the oropharynx and the vascular space, eventually leading to thrombosis in the IJV [9,10]. This process has not yet been fully clarified. The theory is contradicted, in part, by our case-the infection in the left tonsil led to thrombosis in the right-sided internal jugular vein, and eventually to a mycotic aneurysm in the right-sided internal carotid artery. We believe this is more likely to be indicative of general septic dissemination, which led to a septic venous thrombosis on the contralateral side. The infection starts as a harmless condition in the oropharynx (as in our case) and may lead to grave complications resulting from septic dissemination, such as abscesses in the lung, bone, joints, soft tissues, brain, eyes, and the cardiovascular system [8,10-14].
Due to the diversity of the symptoms, it is understandably difficult to establish the clinical diagnosis of Lemierre's syndrome. The various symptoms may be confusing to the clinician. Our patient had a primary paresis of the oculomotor and abducens nerve and was therefore initially treated at our ophthalmological outpatient department, subsequently at the neurology department, and finally at the department of internal medicine. Rapid and clear communication between our doctors, as well as investigations performed simultaneously at the radiology department made it possible to establish the diagnosis within 6 hours after the patient's admission to the emergency department. Targeted antibiotic, surgical and anti-coagulatory treatment was started immediately. To our knowledge, at present, there is no description of Lemierre's syndrome being associated with the leading symptom of paresis of the oculomotor and abducens nerves. In one study, the authors observed impairment of the sixth and twelfth cranial nerves in a patient with Lemierre's syndrome, in conjunction with a so-called clival syndrome [15]. Only one case report mentions isolated paresis of the sixth cranial nerve, which had developed not due to a thrombosis in the cavernous sinus but presumably as a secondary outcome of meningitis [16].
The first step in the diagnosis of Lemierre's syndrome is evaluation of the IJV thrombosis by a radiologic procedure, which is best achieved with contrast-assisted computed tomography, MRI or ultrasound. If the clinician suspects Lemierre's syndrome, he/she should also perform an imaging investigation of the lung (preferably computed tomography).
The above-mentioned case confirms the fact that patients may have septic emboli in the lung despite the absence of clinical symptoms like cough or sputum. Finally, it is mandatory to perform an MRI investigation of the brain for timely identification of abscesses or intracranial venous thromboses, as in the patient described in this report.
In summary, we were able to confirm that Lemierre's syndrome may occur in conjunction with various symptoms, including uncharacteristic ones such as paresis of the abducens and oculomotor nerves. Due to the diverse clinical symptoms associated with this condition, clinical and radiological specialties must work on an interdisciplinary basis to minimize the delay until the establishment of the diagnosis and institution of therapy. This, in turn, will avoid any catastrophic or lethal outcome of this disease. Lemierre's syndrome has often been described in the literature in the last few years, but to our knowledge, there is no description of this disease with such primary ophthalmological symptoms. Therefore, the ophthalmologist should consider this rare syndrome when discovering such a clinical condition.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Lemierre A. On certain septicaemias due to anaerobic organisms. Lancet. 1936;227:701–703. [Google Scholar]
- 2.Courmont P, Cade A. Sur une septico-pyohemie de l'homme simulant la peste et causee par un streptobacille anaerobie. Arch Med Exp Anat Pathol. 1900;4:17–28. [Google Scholar]
- 3.Shannon GW, Ellis CV, Stepp WP. Oropharyngeal bacteroides melaninogenicus infection with septicemia: Lemierre's syndrome. J Fam Pract. 1983;16:159–160. 163, 166. [PubMed] [Google Scholar]
- 4.Riordan T, Wilson M. Lemierre's syndrome: more than a historical curiosa. Postgrad Med J. 2004;80:328–334. doi: 10.1136/pgmj.2003.014274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kos S, Kraft M, Michot MP. Lemierre syndrome: diagnosis with multimodal imaging. Rofo. 2007;179:1198–1199. doi: 10.1055/s-2007-963464. [DOI] [PubMed] [Google Scholar]
- 6.Chirinos JA, Lichtstein DM, Garcia J, Tamariz LJ. The evolution of Lemierre syndrome: report of 2 cases and review of the literature. Medicine (Baltimore) 2002;81:458–465. doi: 10.1097/00005792-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Jankowich M, El-Sameed YA, Abu-Hijleh M. A 21-year-old man with fever and sore throat rapidly progressive to hemoptysis and respiratory failure: diagnosis: Lemierre syndrome with Fusobacterium necrophorum sepsis. Chest. 2007;132:1706–1709. doi: 10.1378/chest.07-0631. [DOI] [PubMed] [Google Scholar]
- 8.Weeks DF, Katz DS, Saxon P, Kubal WS. Lemierre syndrome: report of five new cases and literature review. Emerg Radiol. 2010;17:323–328. doi: 10.1007/s10140-010-0858-y. [DOI] [PubMed] [Google Scholar]
- 9.Carlson ER, Bergamo DF, Coccia CT. Lemierre's syndrome: two cases of a forgotten disease. J Oral Maxillofac Surg. 1994;52:74–78. doi: 10.1016/0278-2391(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 10.Syed MI, Baring D, Addidle M, et al. Lemierre syndrome: two cases and a review. Laryngoscope. 2007;117:1605–1610. doi: 10.1097/MLG.0b013e318093ee0e. [DOI] [PubMed] [Google Scholar]
- 11.Beldman TF, Teunisse HA, Schouten TJ. Septic arthritis of the hip by Fusobacterium necrophorum after tonsillectomy: a form of Lemierre syndrome? Eur J Pediatr. 1997;156:856–857. doi: 10.1007/s004310050730. [DOI] [PubMed] [Google Scholar]
- 12.Leugers CM, Clover R. Lemierre syndrome: postanginal sepsis. J Am Board Fam Pract. 1995;8:384–391. [PubMed] [Google Scholar]
- 13.Bentham JR, Pollard AJ, Milford CA, et al. Cerebral infarct and meningitis secondary to Lemierre's syndrome. Pediatr Neurol. 2004;30:281–283. doi: 10.1016/j.pediatrneurol.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Agarwal R, Arunachalam PS, Bosman DA. Lemierre's syndrome: a complication of acute oropharyngitis. J Laryngol Otol. 2000;114:545–547. doi: 10.1258/0022215001906110. [DOI] [PubMed] [Google Scholar]
- 15.Peer Mohamed B, Carr L. Neurological complications in two children with Lemierre syndrome. Dev Med Child Neurol. 2010;52:779–781. doi: 10.1111/j.1469-8749.2010.03718.x. [DOI] [PubMed] [Google Scholar]
- 16.Jones C, Siva TM, Seymour FK, O'Reilly BJ. Lemierre's syndrome presenting with peritonsillar abscess and VIth cranial nerve palsy. J Laryngol Otol. 2006;120:502–504. doi: 10.1017/S002221510600034X. [DOI] [PubMed] [Google Scholar]


