Abstract
Objective
We evaluated the effect of perceived discrimination, optimism, and their interaction on health care utilization among African American adults with sickle cell disease (SCD).
Methods
Measures of optimism and perceived discrimination were obtained in 49 African American SCD patients. Multiple regression analyses controlling for sex and age tested effects of optimism and perceived discrimination on the number of emergency department visits (ED) and number and duration of hospitalizations over the past year.
Results
A perceived discrimination-optimism interaction was associated with number of emergency departments visits (b = .29, p = .052), number of hospitalizations (b = .36, p = .019), and duration of hospitalizations (b = .30, p = .045) such that those with high perceived discrimination/high optimism had the greatest health care utilization.
Conclusions
African American SCD patients with high perceived discrimination/high optimism had greater health care utilization than patients who reported either low perceived discrimination or low optimism. This study suggests that patient personality and coping styles should be considered when evaluating the effects of stress on SCD-related outcomes.
Keywords: sickle cell anemia, discrimination, health care
BACKGROUND
Sickle Cell Disease
Sickle cell disease (SCD) is one of the most commonly inherited diseases with more than 89 000 known cases in the United States.1 Although medical treatment for SCD has drastically improved, patients with the disease continue to have an extremely low life expectancy that is approximately 30 years below that of persons without SCD.2,3 Individuals with the disease typically experience complications due to sickled red blood cells that clump together and adhere to walls of capillaries and veins resulting in vaso-occlusion.4 These vaso-occlusive events lead to frequent painful episodes (the hallmark of SCD and the most common reason for hospitalization beyond infancy) and end-organ damage.5 One in 5 patients with SCD experiences 3 or more acute care encounters each year, and the frequency of readmissions within 30 days is greater than 30%.1 The estimated yearly health care cost for SCD in the United States is approximately $1.1 billion.6 SCD-related problems result in a disproportionately high use of health care resources, as indexed by the number of emergency department visits, hospitalizations, and days hospitalized each year.6,7
African Americans, Perceived Discrimination, and Hypertension
SCD is an economic burden to patients and their families, most of whom are already socially and economically disadvantaged.8 The daily psychosocial stress experienced by patients with SCD provides an added risk for poor disease outcomes.9 For example, hypertension, a factor associated with chronic stress in normal participants, may be associated with more harmful outcomes in SCD patients since small changes in blood pressure might pose a large risk to this population.10,11 Perceived discrimination represents a stressful experience that may not only be common to individuals with SCD but may also have serious health consequences.
Patients with SCD often perceive discriminatory treatment due to their chronic need for narcotic medications during painful events and providers’ reluctance to prescribe them; as a result, patients are frequently viewed as drug addicts.12,13 Further, even outside of the medical system, persons with SCD have to deal with the stigma of the disease.14 The experience of discrimination may also be magnified because patients with SCD are typically racial/ethnic minorities. African Americans often have less trust in their physicians, clinical research, and hospitals, and feel they would receive better treatment if they were of a different race.15–20
Several studies have shown that experiences of racial discrimination are associated with poor health and an increased rate of hypertension among African Americans.21–24 Individuals who experience long-term background stressors (eg, discrimination) also show an impaired response and a delayed recovery from acute stress.25
Among African Americans, perceived discrimination has a significant negative effect on both mental and physical health;10 however, high perceived discrimination does not consistently lead to negative health outcomes. Evidence suggests that personality factors and coping styles may moderate the health effects of discrimination and other psychosocial stressors.26 For instance, a person’s interpretation or response to hostile or ambiguous stimuli, as a result of a particular personality or coping style, may largely determine its physiological and/or psychological impact. Coping styles such as denial or suppression, for example, have been linked to greater levels of hypertension than coping styles that employ problem solving or active coping.22,27–29
Optimism and Health
Personality has long been implicated in behavioral and health outcomes.30–35 However, no studies have specifically examined the effect of personality on perceived stress in SCD. In this population, personality traits may moderate the association between perceived discrimination and health outcomes.
One such personality trait, optimism, defined as a generalized expectation that good things will happen, has been significantly associated with a variety of physical health indicators including mortality, survival, cardiovascular outcomes (eg, recovery following coronary artery bypass surgery, cardiovascular mortality, coronary heart disease), cardiophysiological markers (including immune function), immune function only, cancer outcomes, outcomes related to pregnancy, physical symptoms, and pain.36 Optimism, as assessed by the Life Orientation Test used in the current study, was associated with reduced incidence of medical complications following coronary artery bypass surgery and angioplasty as well as reduced progression of atherosclerosis in a number of studies.35
On the other hand, unrealistic optimism, defined in one study as the mistaken belief that one’s chances of experiencing problems are lower than those of other people,37 may be associated with greater health risks.38,39 Unrealistically, optimism has been associated with a wide variety of health events, including risk of heart attack, becoming ill, developing skin cancer, and breast cancer.37 Studies have also demonstrated psychological costs and behavioral health risks associated with unwarranted positivity.40,41 For example, unrealistic optimism has been associated with depression and engaging in harmful alcohol-related or tobacco smoking-related events.37,42,43
Few studies have examined optimism in SCD. One study of adolescents with SCD found that among those with higher levels of optimism, use of opioid medication was more highly correlated with reported pain level than for those with lower levels of optimism.44 This suggests that optimistic patients may be able to better match their medication use according to the pain severity they are experiencing as compared with less optimistic patients.
Little is known about how optimism interacts with perceived discrimination to predict health-related outcomes. One study by Richman et al, examining the interaction between optimism and perceived discrimination, found that among African Americans reporting high perceived discrimination, those who were optimistic showed the highest cardiovascular reactivity and slowest recovery to an anger-recall task.45 Cardiovascular reactivity is defined as the blood pressure and pulse reactivity to a stressor such as an anger-recall task, where participants are asked to describe aloud an event when they were angry at another person.46 Therefore, given the results of Richman et al’s study, we would expect that individuals who experience high levels of discrimination and yet are highly optimistic might have poorer psychological, physiological, and behavioral responses to stress than individuals who are highly optimistic and/or experience little discrimination.
Given the impact of perceived discrimination and optimism on stress responsivity among healthy African Americans, it may be informative to explore the effect of perceived discrimination and optimism on disease outcomes in an SCD population, a group exposed to high levels of stress and among whom small changes in blood pressure can lead to deleterious health outcomes.11 In SCD, cells become stiff and viscous, hindering blood circulation. Hypertension in SCD is therefore hypothesized to contribute to greater pain symptomatology and further medical complications due to rapid circulation of abnormal cells and the resulting endothelial damage. This process is described elsewhere as it applies to normal participants.47
In the current study, we aimed to determine the interactive effects of perceived discrimination and optimism on the health care utilization of persons with SCD. Given previous findings showing an interaction between perceived discrimination and optimism on health,45 we hypothesized that patients with SCD who report higher levels of perceived discrimination and optimism will report more frequent emergency department visits and hospital admissions and longer hospital stays.
METHODS
Sample
Participants in this study were recruited from the patient population of the Sickle Cell Clinic at Duke University Medical Center in Durham, North Carolina. Recruited participants gave written informed consent using forms approved by the institutional review board (IRB) and completed the IRB-approved protocol. Participants were African American patients aged 18 years or older with a confirmed diagnosis of SCD by the attending hematologist based on hemoglobin electrophoresis. All literate patients with SCD were eligible unless they exhibited symptomological (eg, emergency department visit) or scheduling complications (eg, already participating in another conflicting study). Subjects were given $25 upon completion of the study. The present study is based on data obtained from 49 adult participants (71% female; mean age, 37 ± 13). Study coordinators then distributed a printed packet with demographic, psychosocial, and SCD health care utilization questionnaires to be completed by the participant.
Psychosocial Measures
Everyday discrimination
The Everyday Discrimination scale48 assesses the frequency of chronic, routine, and covert experiences of unfair treatment, and measures the construct perceived discrimination. The 11-item measure asks, “In your day-to-day life, how often have any of the following things happened to you?” The respondent then lists how frequently s/he is, for example, “treated with less courtesy than others,” “threatened or harassed,” or “people act as if they think you are not smart.” Questions ask about general experiences of discrimination and are not necessarily specific to discrimination experienced in the health care setting. Response choices ranged from “almost every day” to “never” on a 6-point Likert scale. The Everyday Discrimination scale has demonstrated high levels of internal consistency with Cronbach’s α reliability coefficient of 0.87, item-total correlations that range from 0.50 to 0.70, and split-half reliability48 of 0.83.
The mean perceived discrimination score of 17.61 (SD, 17.43) for the current sample was relatively lower than in previous samples. In a cross-sectional sample of 330 individuals, authors reported an average score of 2.07 (± 0.81) in 2001 on a 5-point Likert scale, 5-item version of the measure.49 A conversion from this version of the instrument to the version used in this current study would yield an average total score of 22.36. In a more recent sample of 296 older African American adults of which 70% were women, authors reported an average score of 1.82 (± 2.1) on a 4-point Likert scale version of the entire 9-item measure.50 A conversion from this version of the instrument to the version used in this current study would yield an average total score of 24.57. The measure has also been validated as a measure of everyday discrimination in a 5302-member cohort of African Americans and is thought to be appropriate for use in health studies.51
Life Orientation Test
Participants’ trait optimism was assessed using the Revised Life Orientation Test (LOT-R)52 for trait optimism levels. The LOT-R is a 10-item scale with 2 filler items: 4 positively worded items and 4 negatively worded statements. Respondents indicate their levels of agreement with a range from strongly disagree to strongly agree (1–5) on a 5-point scale. Negative scores are reversed and a single sum score is obtained, with higher scores indicative of higher optimism.52 The LOT-R scale has also demonstrated high levels of internal consistency and convergent and divergent validity. In Scheier, Carver, and Bridges’ 1994 study of 4309 participants, psychometric testing reveals a range of scores from 0 to 32, with a mean of 14.33 (SD, 4.28), for the college aged; sample item-scale correlations ranged from 0.43 to 0.63, an internal reliability of 0.88, and a Cronbach’s α52 of .082.
Health care utilization
This measure consists of 5 items, including number of emergency department visits, hospitalizations, and days spent in the hospital, on hospitalizations. These measurements were asked regarding the period within the last 12 months. These questions are adapted from Harrison and colleagues.53
Analysis
All analyses were conducted using SAS v.9, Cary, North Carolina. The current study had power to detect a 0.25 effect size (Cohen’s f2) for β based on p value of .05. All predictor and outcome variables were standardized with a mean of 0 and a standard deviation of 1. Number of emergency department visits and number of hospitalizations variables were positively skewed and were therefore log-transformed to provide a more normal distribution.
Regressions were used to test effect of covariates, age, education (continuous variables), and sex on outcome variables: number of emergency department visits, hospitalizations, and days spent in the hospital. Participants reported education level by reporting years of education completed using a 0 years to ≥21 years scale. A priori hypotheses were tested in multiple regression models with age and sex included as covariates following Richman et al.45 Since education was not related to other dependent or independent variables (all p > .05), it was not used in further analyses. Perceived discrimination, optimism, and their interactions were entered as independent variables in each model predicting health care utilization: number of emergency department visits, number of hospitalizations, and number of days spent in the hospital.
Using hierarchical multiple regression, demographic covariates are entered first, then perceived discrimination and optimism main effects, then 2-way interactions (eg, perceived discrimination × optimism) predicting health care utilization. Interaction plots used maximum and minimum values to represent high and low levels of the primary predictor (ie, perceived discrimination) and maximum and minimum values to represent for high and low levels of the moderator (ie, optimism).
RESULTS
Descriptive Statistics
As shown in Table 1, the sample included 35 women and 14 men, with a mean age of 37 years old. The mean education level was 13.77 years of schooling or approximately an associate’s degree. The mean level of perceived discrimination was 17.61, which is less than approximate means (ie, 24.57, 22.36) derived from previous samples described above.49,50 The mean level of optimism was 16.57, which is greater than means (ie, 14.33) from previous studies described above.52 The mean number of emergency department visits was 6.3; the mean number of hospitalizations was 4.33; and the mean number of days spent in the hospital was 4.68.
Table 1.
Descriptive Statistics and Study Variable Means
| Variable | Mean | Standard Deviation | Max/Min |
|---|---|---|---|
| Sex | 35 females/14 males | ||
| Age | 37 | 13.6 | 20/77 |
| Education | 13.77 | 2.12 | 9/18 |
| Perceived discrimination. | 17.61 | 17.43 | 9/39 |
| Optimism | 16.57 | 4.49 | 7/24 |
| No. of emergency department visits in last year | 6.3 | 16.06 | 0/112.5 |
| No. of hospitalizations in last year | 4.33 | 9.21 | 0/62.5 |
| No. of days in hospital in last year | 4.68 | 4.34 | 0/17.5 |
Significant age differences were found for number of emergency department visits (b = −.28, p = .047) and number of days spent in the hospital (b = −.34, p = .0179), suggesting that older patients had fewer emergency department visits and shorter hospital stays. A trend in sex differences was found for perceived discrimination (b = −.61, p = .052). In the current sample, Cronbach’s α for raw optimism scores was 0.70 and for raw perceived discrimination scores was 0.86.
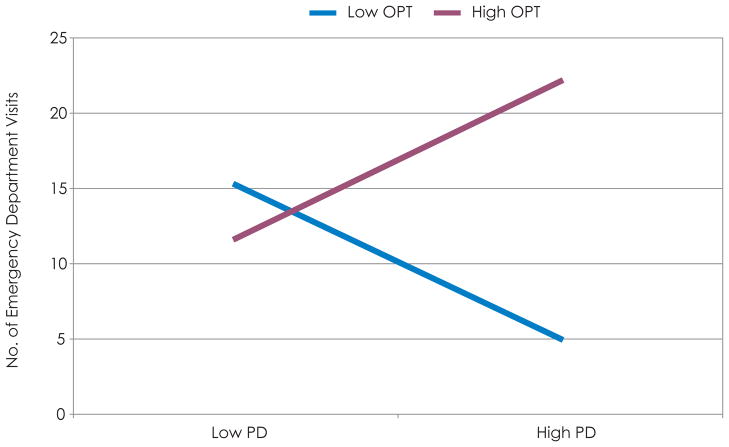
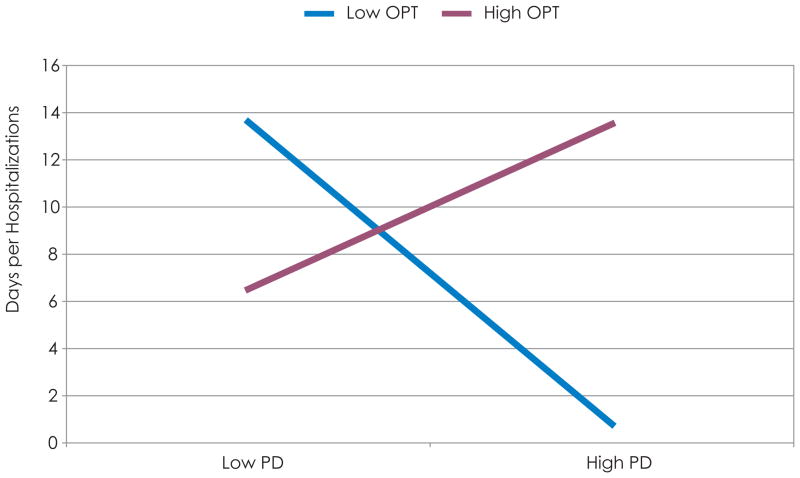
Perceived Discrimination and Optimism Associations With Health Care Utilization
As hypothesized, there was a significant perceived discrimination × optimism interaction effect on SCD-related health care utilization: number of emergency department visits (b = .29, p = .052), number of hospitalizations (b = .36, p = .019), and number of days spent in the hospital (b = .30, p = .045), as seen in Tables 2 to 4. The effect of this interaction was similar across all 3 outcomes. As shown in Figure 1, as perceived discrimination increases, there is an increase in the number of emergency department visits among those with high optimism and a decrease among those with low optimism. The nature of the interaction for number of hospitalizations is illustrated in Figure 2. As perceived discrimination increases, there is an increase in the number of hospitalizations among those with high optimism and a decrease among those with low optimism. As shown in Figure 3, as perceived discrimination increases, there is an increase in the number of days spent in the hospital among those with high optimism and a decrease among those with low optimism.
Table 2.
Interaction Between Perceived Discrimination and Optimisma Predicts Number of Emergency Department Admissionsb
| Parameter | Estimate | Standard Error | Confidence Interval | t Value | Pr > |t| |
|---|---|---|---|---|---|
| Intercept | −0.22 | 0.26 | −0.74 to 0.31 | −0.83 | 0.411 |
| Age | −0.32 | 0.14 | −0.60 to −.04 | −2.30 | 0.026 |
| Sex | 0.44 | 0.32 | −0.21 to 1.10 | 1.36 | 0.181 |
| Perceived discrimination | 0.34 | 0.16 | −0.02 to 0.67 | 2.12 | 0.040 |
| Optimism | −0.04 | 0.15 | −0.34 to 0.27 | −0.24 | 0.810 |
| Perceived discrimination × optimism | 0.29 | 0.15 | −0.003 to 0.59 | 1.99 | 0.052 |
All variables are standardized.
Log-transformed variable.
Table 4.
An Interaction Between Perceived Discrimination and Optimisma Predicts Length of Hospitalization
| Parameter | Estimate | Standard Error | Confidence Interval | t Value | Pr > |t| |
|---|---|---|---|---|---|
| Intercept | 0.04 | 0.25 | −.47 to 0.56 | 0.17 | 0.869 |
| Age | −.36 | 0.14 | −.64 to −.09 | −2.67 | 0.011 |
| Sex | 0.08 | 0.32 | −.56 to 0.72 | 0.25 | 0.807 |
| Perceived discrimination | −.09 | 0.16 | −.41 to 0.22 | −0.60 | 0.553 |
| Optimism | −.09 | 0.15 | −.39 to 0.22 | −0.56 | 0.578 |
| Perceived discrimination × optimism | 0.30 | 0.14 | 0.01 to 0.59 | 2.07 | 0.045 |
All variables are standardized.
Figure 1.
Perceived Discrimination × Optimism Interaction Is Associated With Number of Emergency Department Visits
Abbreviations: ED, emergency department; OPT, optimism; PD, perceived discrimination.
Figure 2.

Perceived Discrimination × Optimism Interaction Is Associated With Number of Hospitalizations
Abbreviations: ED, emergency department; OPT, optimism; PD, perceived discrimination.
Figure 3.
Perceived Discrimination × Optimism Interaction Is Associated With Days per Hospitalization
Abbreviations: ED, emergency department; OPT, optimism; PD, perceived discrimination.
Controlling for covariates sex and age, the main effects of perceived discrimination on number of emergency department visits (b = .22, p = .142), number of hospitalizations (b = .02, p = .871), and number of days spent in the hospital (b = −.21, p = .153) were all nonsignificant. Controlling for covariates, the main effects of optimism on number of emergency department visits (b = −.05, p = .737), number of hospitalizations (b = .06, p = .695), and number of days spent in the hospital (b = .05, p = .714) were also all nonsignificant.
DISCUSSION
Consistent with our primary hypothesis, our study showed significantly greater health care utilization as indexed by more frequent emergency department visits and hospitalizations among patients with SCD who reported higher perceived discrimination (perceived discrimination) and trait optimism, whereas among patients who reported low optimism, increasing perceived discrimination was associated with a decrease in health care utilization. For length of hospital stay, low optimism was still protective but only in the presence of high discrimination, as the high perceived discrimination and low optimism group reported fewer days per hospitalization.
Patients reporting higher perceived discrimination and optimism may be exhibiting unrealistic levels of optimism, and, ultimately, a greater need for medical assistance to cope with SCD crises. As described above, this style of coping may be associated with adverse health consequences.38,39
We also found that older patients with SCD in the sample reported significantly fewer number of emergency department visits and number of days spent in the hospital. Very little work has compared functioning in older and younger patients, although one study also found that older patients with SCD reported significantly fewer number of emergency department visits than younger patients.54 This study also reported that older patients utilized greater outpatient services. Together, these data suggest that older patients may have different patterns of health care utilization than younger ones. It is possible that survival bias accounts for this discrepancy; older patients with SCD may be hardy survivors who are able to cope more effectively with their disease. These findings may also reflect a treatment preference that changes with age or that has changed over time along with health care structure and availability—creating a culture that encourages younger adults to seek care in an emergency department rather than an outpatient clinic. Possible societal and/or individual moderating variables that change over time or with age should be explored in future prospective studies.
We found a nonsignificant trend for men to report more discrimination than women. This finding is difficult to interpret both because it was only marginally significant and because of the small number of men in our sample. However, this trend does reflect similar findings in national studies that men across races are nearly twice as likely as women to report frequent day-to-day discrimination.55
There are several limitations of the current study that must be acknowledged. First of all, these findings are based on retrospective self-reports for both predictor (eg, perceived discrimination, optimism) and outcome (eg, number of emergency department visits, number of hospitalizations, and number of days spent in the hospital) variables. To confirm that high perceived discrimination is indeed causing a more adverse clinical course in patients with SCD who have high levels of optimism, it will be necessary to conduct a prospective study showing that the perceived discrimination × optimism interaction predicts subsequent number of emergency department visits, number of hospitalizations and number of days spent in the hospital in a larger sample of patients with SCD who are followed over a period of time.
While our indicators of health care utilization approximate the current knowledge regarding progressive SCD severity, these measures may not necessarily represent a valid construct of SCD severity given the potential for confounders in self-reported report data. Moreover, patients who, for example, visit the emergency department regularly or undergo regular hospitalizations may not necessarily be those who are in the greatest need of these services. However, with a paucity of literature on SCD disease progression and a lack of a standard indicator of disease severity, we are limited in our measures. Fortunately, our measures were adapted from previous literature and created alongside SCD physicians who witness and track clinically the real-life difficulties facing patients with SCD.9,53 Since no standard disease indicators exist as they do for other conditions (eg, hypertension, diabetes, or heart disease), the measures of health care utilization may more effectively capture a patient’s SCD-related disability than more objective measures (eg, measure of tissue damage).
In conclusion, the present study’s findings suggest that patients with SCD who have greater optimism but who also report higher levels of perceived discrimination may be susceptible to a more adverse clinical course and greater utilization of medical services. We believe that the current findings require replication in a larger prospective study. Further, to help decrease the cost of patient health care utilization, more studies examining behavioral interventions in the sickle cell population are needed—specifically those targeting psychological factors such as optimism and perceived discrimination.
Table 3.
| Parameter | Estimate | Standard Error | Confidence Interval | t Value | Pr > |t| |
|---|---|---|---|---|---|
| Intercept | −0.16 | 0.26 | −0.69 to 0.37 | −0.59 | 0.557 |
| Age | −0.30 | 0.14 | −0.58 to −.02 | −2.13 | 0.039 |
| Sex | 0.39 | 0.33 | −0.27 to 1.05 | 1.19 | 0.242 |
| Perceived discrimination | 0.19 | 0.16 | −0.13 to 0.52 | 1.19 | 0.240 |
| Optimism | −0.01 | 0.16 | −0.32 to 0.31 | −0.04 | 0.970 |
| Perceived discrimination × optimism | 0.36 | 0.15 | 0.06 to 0.66 | 2.45 | 0.019 |
All variables are standardized.
Log-transformed variable.
Acknowledgments
Funding/Support: This research was supported by the National Heart, Lung, and Blood Institute grant P01-HL036587 and by the Duke Behavioral Medicine Research Center.
References
- 1.Brousseau DC, Panepinto JA, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: National and state estimates. Am J Hematol. 2010;85(1):77–78. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 2.Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330(23):1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 3.Brousseau DC, Mukonje T, Brandow AM, Nimmer M, Panepinto JA. Dissatisfaction with hospital care for children with sickle cell disease not due only to race and chronic disease. Pediatr Blood Cancer. 2009;53(2):174–178. doi: 10.1002/pbc.22039. [DOI] [PubMed] [Google Scholar]
- 4.Zennadi R, Moeller BJ, Whalen EJ, et al. Epinephrine-induced activation of LW-mediated sickle cell adhesion and vaso-occlusion in vivo. Blood. 2007;110(7):2708–2717. doi: 10.1182/blood-2006-11-056101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnog JB, Duits AJ, Muskiet FA, ten Cate H, Rojer RA, Brandjes DP. Sickle cell disease; a general overview. Neth J Med. 2004;62(10):364–374. [PubMed] [Google Scholar]
- 6.Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84(6):323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- 7.Woods K, Karrison T, Koshy M, Patel A, Friedmann P, Cassel C. Hospital utilization patterns and costs for adult sickle cell patients in Illinois. Public Health Rep. 1997;112(1):44–51. [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson TL, Jonassaint JC, Ansah D, et al. Sickle cell education: Working to promote prevention. Paper presented at: 27th Annual Meeting of the National Sickle Cell Disease Program; 2004; Orlando, FL. [Google Scholar]
- 9.Edwards CL, Scales MT, Loughlin C, et al. A brief review of the pathophysiology, associated pain, and psychosocial issues in sickle cell disease. Int J Beh Med. 2005;12(3):171–179. doi: 10.1207/s15327558ijbm1203_6. [DOI] [PubMed] [Google Scholar]
- 10.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson CS. Arterial blood pressure and hyperviscosity in sickle cell disease. Hematol Oncol Clin North Am. 2005;19(5):827–837. vi. doi: 10.1016/j.hoc.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Waldrop RD, Mandry C. Health professional perceptions of opioid dependence among patients with pain. Am J Emerg Med. 1995;13(5):529–531. doi: 10.1016/0735-6757(95)90163-9. [DOI] [PubMed] [Google Scholar]
- 13.Maxwell K, Streetly A, Bevan D. Experiences of hospital care and treatment seeking for pain from sickle cell disease: qualitative study. BMJ. 1999;318(7198):1585–1590. doi: 10.1136/bmj.318.7198.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Markel H. The stigma of disease: implications of genetic screening. Am J Med. 1992;93(2):209–215. doi: 10.1016/0002-9343(92)90052-d. [DOI] [PubMed] [Google Scholar]
- 15.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162(21):2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 17.Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans’ views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001;52(5):797–808. doi: 10.1016/s0277-9536(00)00178-7. [DOI] [PubMed] [Google Scholar]
- 18.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87(11):1773–1778. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nickerson KJ, Helms JE, Terrell F. Cultural Mistrust, Opinions About Mental-Illness, and Black-Students Attitudes toward Seeking Psychological Help from White Counselors. J Couns Psychol. 1994;41(3):378–385. [Google Scholar]
- 20.Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19(2):101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dressler WW. Lifestyle, stress, and blood pressure in a southern black community. Psychosom Med. 1990;52(2):182–198. doi: 10.1097/00006842-199003000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.James SA, LaCroix Az, Kleinbaum DG, Strogatz DS. John Henryism and blood pressure differences among black men. II. The role of occupational stressors. J Behav Med. 1984;7(3):259–275. doi: 10.1007/BF00845359. [DOI] [PubMed] [Google Scholar]
- 24.Steffen PR, McNeilly M, Anderson N, Sherwood A. Effects of perceived racism and anger inhibition on ambulatory blood pressure in African Americans. Psychosom Med. 2003;65(5):746–750. doi: 10.1097/01.psy.0000079380.95903.78. [DOI] [PubMed] [Google Scholar]
- 25.Gump BB, Matthews KA, Raikkonen K. Modeling relationships among socioeconomic status, hostility, cardiovascular reactivity, and left ventricular mass in African American and White children. Health Psychol. 1999;18(2):140–150. doi: 10.1037//0278-6133.18.2.140. [DOI] [PubMed] [Google Scholar]
- 26.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- 28.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. Am J Epidemiol. 2008;167(5):624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- 29.Peters RM. Racism and hypertension among African Americans. West J Nurs Res. 2004;26(6):612–631. doi: 10.1177/0193945904265816. [DOI] [PubMed] [Google Scholar]
- 30.Booth-kewley S, Vickers RR., Jr Associations between major domains of personality and health behavior. J Pers. 1994;62(3):281–298. doi: 10.1111/j.1467-6494.1994.tb00298.x. [DOI] [PubMed] [Google Scholar]
- 31.Cooper ML, Agocha VB, Sheldon MS. A motivational perspective on risky behaviors: the role of personality and affect regulatory processes. J Pers. 2000;68(6):1059–1088. doi: 10.1111/1467-6494.00126. [DOI] [PubMed] [Google Scholar]
- 32.Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire. Sevenoaks, kent: Hodder and Stoughton; 1975. [Google Scholar]
- 33.Lazarus RS. Stress and emotion: A new synthesis. New York, NY: Springer Pub Co; 1999. [Google Scholar]
- 34.Rosenman RH. Personality, behaviour patterns and heart disease. In: Cooper CL, editor. Handbook of Stress, Medicine and Health. New York, NY: CRC Press; 1996. [Google Scholar]
- 35.Smith TW, Mackenzie J. Personality and risk of physical illness. Annu Rev Clin Psychol. 2006;2:435–467. doi: 10.1146/annurev.clinpsy.2.022305.095257. [DOI] [PubMed] [Google Scholar]
- 36.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37(3):239–256. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dillard AJ, Midboe AM, Klein WM. The dark side of optimism: unrealistic optimism about problems with alcohol predicts subsequent negative event experiences. Pers Soc Psychol Bull. 2009;35(11):1540–1550. doi: 10.1177/0146167209343124. [DOI] [PubMed] [Google Scholar]
- 38.Breakwell GM. Risk communication: factors affecting impact. Br Med Bull. 2000;56(1):110–120. doi: 10.1258/0007142001902824. [DOI] [PubMed] [Google Scholar]
- 39.Weinstein ND. Optimistic biases about personal risks. Science. 1989;246(4935):1232–1233. doi: 10.1126/science.2686031. [DOI] [PubMed] [Google Scholar]
- 40.Diener E, Colvin CR, Pavot WG, Allman A. The psychic costs of intense positive affect. J Pers Soc Psychol. 1991;61(3):492–503. [PubMed] [Google Scholar]
- 41.Raats MM, Sparks P. Unrealistic optimism about diet-related risks: implications for interventions. Proc Nutr Soc. 1995;54(3):737–745. doi: 10.1079/pns19950073. [DOI] [PubMed] [Google Scholar]
- 42.Dunning D, Story AL. Depression, realism, and the overconfidence effect: are the sadder wiser when predicting future actions and events? J Pers Soc Psychol. 1991;61(4):521–532. doi: 10.1037//0022-3514.61.4.521. [DOI] [PubMed] [Google Scholar]
- 43.Dillard AJ, McCaul KD, Klein WM. Unrealistic optimism in smokers: implications for smoking myth endorsement and self-protective motivation. J Health Commun. 2006;11(suppl 1):93–102. doi: 10.1080/10810730600637343. [DOI] [PubMed] [Google Scholar]
- 44.Pence L, Valrie CR, Gil KM, Redding-Lallinger R, Daeschner C. Optimism predicting daily pain medication use in adolescents with sickle cell disease. J Pain Symptom Manage. 2007;33(3):302–309. doi: 10.1016/j.jpainsymman.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 45.Richman LS, Bennett GG, Pek J, Siegler I, Williams RB., Jr Discrimination, dispositions, and cardiovascular responses to stress. Health Psychol. 2007;26(6):675–683. doi: 10.1037/0278-6133.26.6.675. [DOI] [PubMed] [Google Scholar]
- 46.Brummett BH, Boyle SH, Kuhn CM, Siegler IC, Williams RB. Positive affect is associated with cardiovascular reactivity, norepinephrine level, and morning rise in salivary cortisol. Psychophysiology. 2009;46(4):862–869. doi: 10.1111/j.1469-8986.2009.00829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Williams RB. Blood pressure reactivity to psychological stress: a new risk factor for coronary disease? Hypertension. 2006;47(3):329–330. doi: 10.1161/01.HYP.0000200688.37802.01. [DOI] [PubMed] [Google Scholar]
- 48.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 49.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96(7):1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24(3):438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sims M, Wyatt SB, Gutierrez ML, Taylor HA, Williams DR. Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethn Dis. 2009;19(1):56–64. [PMC free article] [PubMed] [Google Scholar]
- 52.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 53.Harrison MO, Edwards CL, Koenig HG, Bosworth HB, Decastro L, Wood M. Religiosity/Spirituality and Pain in Patients With Sickle Cell Disease. J Nerv Ment Dis. 2005;193(4):250–257. doi: 10.1097/01.nmd.0000158375.73779.50. [DOI] [PubMed] [Google Scholar]
- 54.Sanders KA, Labott SM, Molokie R, Shelby SR, Desimone J. Pain, coping and health care utilization in younger and older adults with sickle cell disease. J Health Psychol. 2010;15(1):131–137. doi: 10.1177/1359105309345554. [DOI] [PubMed] [Google Scholar]
- 55.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–230. [PubMed] [Google Scholar]