Abstract
Background
The aim of this study was to examine prospective predictors of suicide events, defined as suicide attempts or emergency interventions to reduce suicide risk, in 119 adolescents admitted to an in-patient psychiatric unit for suicidal behaviors and followed naturalistically for 6 months.
Method
Structured diagnostic interviews and self-report instruments were administered to adolescent participants and their parent(s) to assess demographic variables, history of suicidal behavior, psychiatric disorders, family environment and personality/temperament.
Results
Baseline variables that significantly predicted time to a suicide event during follow-up were Black race, high suicidal ideation in the past month, post-traumatic stress disorder (PTSD), childhood sexual abuse (CSA), borderline personality disorder (BPD), low scores on positive affectivity, and high scores on aggression. In a multivariate Cox regression analysis, only Black race, CSA, positive affect intensity and high aggression scores remained significant.
Conclusions
Our findings suggest the following for adolescent populations: (1) in a very high-risk population, risk factors for future attempts may be more difficult to ascertain and some established risk factors (e.g. past suicide attempt) may not distinguish as well; and (2) cross-cutting constructs (e.g. affective and behavioral dysregulation) that underlie multiple psychiatric disorders may be stronger predictors of recurrent suicide events than psychiatric diagnoses. Our finding with respect to positive affect intensity is novel and may have practical implications for the assessment and treatment of adolescent suicide attempters.
Keywords: Adolescent, aggression, impulsivity, positive affectivity, suicide
Introduction
Suicidal behavior in adolescents is a serious and pressing public health concern. There have been relatively few naturalistic prospective studies of adolescent suicidality. Community-based studies of adolescents have identified several classes of risk factors, with the most robust set of risk factors being past history of attempts, current suicidal ideation and recent attempt by a friend or family member (Lewinsohn et al. 1994). Other commonly reported risk factors include psychopathology, specifically depression (Lewinsohn et al. 1994), externalizing disorders (Hills et al. 2009), anxiety disorders (Boden et al. 2007) and substance use disorders (SUD; Gould et al. 1998; Wichstrom, 2000; Riala et al. 2007; Bronisch et al. 2008; Nock et al. 2010). Some studies have found that family environment and parenting characteristics (Lewinsohn et al. 1994; Wichstrom, 2000; Mitrou et al. 2010) contribute to suicide risk during adolescence. Many of the risk factors identified by such studies apply to a broad range of the population, and they can lack precision in predicting suicide behaviors in more range-restricted settings, such as clinical environments treating suicidal adolescents.
Risk factors identified in studies involving adolescent clinical (in-patient) samples include depressed mood (Spirito et al. 2003), hopelessness, persistent depression (Brinkman et al. 2000; Aglan et al. 2008), suicidal thoughts, family dysfunction, dysthymia (King et al. 1995), poor social adjustment, mood disorders (Pfeffer et al. 1993), particularly major depressive disorder (MDD), dysthymic disorder and co-morbidity with either conduct and/or SUD (Kovacs et al. 1993), multiple previous suicide attempts, more severe suicidal ideation (Prinstein et al. 2008; King et al. 2010) and more severe functional impairment (King et al. 2010). One of the more comprehensive studies of adolescent suicidality to date suggests that history and number of past attempts, psychiatric disorders and affective dimensions (e.g. trait levels of depression, hopelessness, anxiety and anger) are all associated with future suicide attempt risk in at-risk adolescents (Goldston et al. 1999, 2006, 2009).
The present study builds upon previous studies by examining established risk factors such as past suicide attempts and suicidal behavior, psychopathology and family characteristics, in addition to less examined variables such as personality and temperament. Very few studies of suicidal adolescents have examined the role of affective and behavioral constructs apart from psychiatric diagnoses in suicidal behaviors. For example, studies with adult suicide attempters have found negative affectivity, which refers to a general tendency to experience negative affect beyond normal range experience, to be a more robust prospective predictor of suicidal behavior than psychiatric disorders (Yen et al. 2009). Only one prospective study of adolescent suicide attempters has assessed borderline personality disorder (BPD) and found it to be a significant predictor of recurrent suicidal behavior over 6 months of follow-up (Greenfield et al. 2008). The paucity of such research is probably because of the controversy in applying the BPD diagnosis to adolescents, given the questionable stability of BPD particularly at this age. However, some empirical studies have affirmed the construct validity of the BPD diagnosis in adolescents, albeit with lower diagnostic stability (e.g. Bondurant et al. 2004; Sharp et al. 2012).
The present study sought to examine prospective predictors of suicidal events over 6 months of naturalistic follow-up in a high-risk sample of adolescents hospitalized for suicide risk. Based on the largest treatment study of adolescent suicide attempters to date (the Treatment of Adolescent Suicide Attempters study, TASA; Brent et al. 2009), the outcome variable was suicide events, operationalized as a suicide attempt (including aborted and interrupted attempts) or any emergency intervention (e.g. hospitalization, emergency rescue) to prevent a suicide attempt. Both attempts and emergency interventions are clinically relevant public health concerns, costly (economically and emotionally), and should be targets for reduction. Attempters and those who need emergency intervention do not seem to be characteristically different (Lewinsohn et al. 1996; Kessler et al. 1999); instead the differences are most likely to be circumstantial. Finally, it is the ethical responsibility of research investigators and staff to actively encourage study participants to seek emergency intervention in the event of a suicide crisis in which they otherwise would make an attempt. For relatively low occurrence events such as suicide attempts, exclusion of emergency intervention events in clinical research studies may lead to an artificial deflation of our outcome of interest and an increase in Type II error.
We hypothesized that a history of suicide attempts would be a robust predictor of subsequent suicide events. We also examined history of deliberate self-harm (both suicidal and non-suicidal), which has also been found to predict future suicidal behavior (Zahl & Hawton, 2004) and suicidal ideation (Lewinsohn et al. 1994). With regard to Axis I psychiatric disorders, depression, disruptive behavior disorders and SUD have been associated with increased risk for suicidal behavior in adolescents (Gould et al. 1998; Spirito & Esposito-Smythers, 2006; Nock et al. 2010) and we anticipated similar findings in the present study. We also examined attention deficit hyperactivity disorder (ADHD) as recent research suggests that young children with ADHD are at risk for suicidal behavior in adolescence (Chronis-Tuscano et al. 2010). Regarding family environment, we hypothesized that lower scores on global family functioning, past history of childhood sexual abuse (CSA) and family history of suicidal behavior would predict subsequent suicidal events. Finally, with regard to personality/ temperament we hypothesized that BPD, trait affective intensity (positive and negative valence) and aggression/behavioral dysregulation would each be robustly associated with subsequent suicide events. Given the diagnostic controversy of BPD in adolescents, we took a conservative approach to analyzing the number of BPD symptoms, excluding the self-injurious behaviors criterion.
Method
Participants
Participants (n = 119) were recruited from an adolescent in-patient psychiatric unit on the basis of having been recently admitted to the unit for elevated suicide risk (e.g. recent suicide attempt, self-injury with suicidal ideation, or suicidal ideation only). Approximately one-third of our baseline sample (n = 33) had made a suicide attempt prior to the index admission. Parental consent and adolescent assent were required to proceed with the intake assessment. Additional information was provided by legal guardians/primary caregivers. This study was approved by the Institutional Review Boards of the university and the respective hospital. Adolescents and parents were each compensated for their time with a payment of US$50, for each of the baseline interviews and for the 6-month follow-up interview.
We obtained some follow-up data from 104 (87.4%) of the sample, with 99 (83.2%) providing 6 months of follow-up data. The present study is based on data from 104 participants who provided some follow-up data.
Assessment
Assessments were conducted during the participants' intake hospitalization stay or shortly thereafter. Whenever applicable, assessments were administered to both adolescent and caregiver. When reports were discrepant, consensus scores were determined during weekly case review meetings using all available information including chart review and information from the treating physician on the adolescent unit. Following the baseline assessments (Time 0), patients were contacted by telephone every 2 months over the subsequent 6 months (26 weeks). During this telephone call, important life events were assessed to assist with recall at the full 6-month interview. Additionally, a brief assessment of the primary predictors and outcomes of interest to this study was reviewed. At the final 6-month follow-up assessment, a more comprehensive assessment of these variables was administered, using measures described in the following sections, resulting in baseline and follow-up (over 6 months) data on variables of interest to the present study.
Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version (K-SADS-PL)
The K-SADS-PL (Kaufman et al. 1997) was used to obtain demographic information, family history, history of CSA, psychiatric diagnoses and past history of suicidal behavior. This semi-structured diagnostic interview provides a reliable and valid assessment of DSM-IV psychopathology in children and adolescents. Inter-rater agreement has been found to be high by the developers (range 93–100%) and in this current sample (κ range 0.61–1.00 for disorders endorsed by at least 15% of the sample). The K-SADS-PL was administered with adolescent and caregiver participants individually. Consensus ratings were used to establish the presence or absence of a diagnosis. The K-SADS-PL also includes a semi-structured suicide module (Kaufman et al. 1997) that was used to assess lifetime and present episodes of suicide attempts along with familial history of suicidal behavior at baseline.
Suicide Ideation Questionnaire (SIQ)
The SIQ (Reynolds, 1985) is a 30-item self-report instrument designed to assess thoughts about suicide experienced by adolescents during the prior month. Excellent internal consistency (α = 0.97) and construct validity for the SIQ have been reported (Reynolds, 1985). Internal consistency was also very high in the present sample (Cronbach's α = 0.97).
Functional Assessment of Self-Mutilation (FASM)
The FASM (Lloyd-Richardson et al. 2007) is a self-report instrument that assesses engagement in non-suicidal self-injury (NSSI) in the past year. The FASM consists of two parts. In the present study, we used responses from the first part of the FASM to determine whether self-injurious behavior was present.
Family Assessment Device (FAD)
The FAD (Epstein et al. 1983) Global Functioning (FAD-GF) subscale score was analyzed for both adolescents and parents. Internal consistency in the present study was strong (α = 0.91 for adolescents, α = 0.88 for caregivers).
Childhood Interview for Borderline Personality Disorder (CI-BPD)
The CI-BPD is the adolescent adaptation of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al. 1996). The DIPD-IV compares favorably to other structured interviews for personality disorders, with excellent inter-rater reliability and test–retest reliability (κ coefficients for BPD = 0.94 and 0.85 respectively) (Zanarini et al. 1987). The CI-BPD was administered at baseline and at the 6-month follow-up. In the present sample, the κ coefficient based on 20 interviews was 0.82.
Affect Intensity Measure (AIM)
The AIM (Larsen & Diener, 1987; Larsen et al. 1987) is a 40-item self-report questionnaire that contains three subscales: negative intensity, positive affectivity, and negative reactivity. Higher scores indicate greater intensity/reactivity. The AIM has strong test–retest reliabilities (0.81 for a 3-month interval and 0.75 for a 2-year interval) and adequate convergent and discriminant validity (Larsen & Diener, 1987; Larsen et al. 1987). The AIM was administered to the adolescent participant at baseline. In the present sample, Cronbach's α was 0.86.
Aggression Questionnaire (AQ)
The AQ (Buss & Perry, 1992) is a widely used measure with 34 items and five scales: physical aggression, verbal aggression, anger, hostility, and indirect aggression. In this study we analyzed parent report of child's behavior as these constructs are observable, externalizing phenomena. In the present sample, Cronbach's α for parent report of the AQ total was 0.95.
Adolescent Longitudinal Interval Follow-Up Evaluation (A-LIFE)
The LIFE (Keller et al. 1987) is a semi-structured interview rating system with demonstrated reliability for assessing the longitudinal course of psychiatric disorders and functioning including suicidal behaviors. It consists of three sections: (1) psychopathology, (2) functioning, including suicidal behavior, and (3) treatment utilization. The latter two are of particular relevance to this study. For suicidal behavior, the numbers of attempts and threats were recorded along with the follow-up week in which they occurred. The treatment utilization section assesses frequency and week of emergency room (ER) visits, in-patient hospitalizations, residential placements, and out-patient treatment sessions. ER visits and in-patient hospitalizations that were related to concerns of suicide risk were counted as a suicide event.
Analyses
The outcome variable of interest was time to suicide event during the 6-month follow-up interval. A suicide event was defined as a suicide attempt and any emergency intervention taken to prevent a suicidal behavior (e.g. emergency department visit, in-patient hospitalization). Thus, emergency interventions not related to suicide (e.g. homicidal ideation) were not included. All categorical variables were dummy coded (0, 1). A series of univariate Cox proportional hazard regression models were performed for a priori determined predictors. Any predictors significant at an α level of p <0.10 were entered into a multivariate Cox proportional hazards regression analysis.
Results
Of the 119 suicidal adolescent patients enrolled in this study at baseline, 104 provided some follow-up data and 99 provided at least 6 months of follow-up data, resulting in an 83% retention rate. The present analyses used data from 104 participants who provided some follow-up data. Those with and without follow-up data were compared across all predictor variables (Table 1). Those who dropped out were more likely to have bipolar disorder (p = 0.037) and a minority racial status (p = 0.043). No other variables were significantly different.
Table 1. Predictor variables by follow-up status.
| Follow-up sample (n = 104) | |||
|---|---|---|---|
|
|
|||
| Baseline (n = 119) | Suicide event (n = 37) | No suicide event (n = 67) | |
| Demographics | |||
| Age (years), mean (S.D.) | 15.3 (1.4) | 15.2 (1.4) | 15.3 (1.4) |
| Female, n (%) | 80 (67.2) | 23 (62.2) | 44 (65.7) |
| Caucasian, n (%) | 97 (81.5) | 29 (80.6) | 58 (86.6) |
| Black, n (%) | 12 (10.1) | 7 (19.4) | 4 (6.0) |
| Hispanic, n (%) | 21 (17.6) | 7 (19.4) | 10 (15.2) |
| Any minority*, n (%) | 30 (25.2) | 10 (27.8) | 13 (19.4) |
| Suicidal behavior characteristics | |||
| Past history SA, n (%) | 44 (37.0) | 11 (30.6) | 29 (43.9) |
| Any SIB, n (%) | 79 (62.2) | 26 (81.3) | 45 (75.0) |
| SIQ, mean (S.D.) | 92.2 (44.8) | 106.5 (44.2) | 85.5 (42.8) |
| Axis I disorder | |||
| MDE, n (%) | 101 (79.5) | 30 (81.1) | 58 (86.6) |
| Bipolar d/o, n (%) | 13 (10.9) | 2 (5.4) | 7 (10.4) |
| Phobic Anx d/o, n (%) | 50 (39.4) | 14 (37.8) | 32 (47.8) |
| PTSD, n (%) | 29 (22.8) | 14 (37.8) | 13 (19.4) |
| Substance Use d/o, n (%) | 20 (15.7) | 6 (16.2) | 12 (17.9) |
| Disruptive d/o, n (%) | 44 (34.6) | 17 (45.9) | 24 (35.8) |
| ADHD, n (%) | 47 (37.0) | 17 (45.9) | 26 (38.8) |
| Eating d/o, n (%) | 13 (10.9) | 1 (2.7) | 9 (13.4) |
| Family characteristics | |||
| FAD-GF Adolescent, mean (S.D.) | 2.43 (0.63) | 2.44 (0.74) | 2.38 (0.60) |
| FAD-GF Parent, mean (S.D.) | 2.06 (0.44) | 2.04 (0.58) | 2.04 (0.35) |
| CSA, n (%) | 29 (33.3) | 13 (44.8) | 11 (45.8) |
| Family Hx suicidal behavior, n (%) | 62 (52.1) | 17 (31.5) | 37 (68.5) |
| Personality | |||
| BPD, n (%) | 47 (37.0) | 18 (48.6) | 20 (29.9) |
| AIM (Positive), mean (S.D.) | 3.12 (0.82) | 2.77 (0.73) | 3.31 (0.86) |
| AQ Total, mean (S.D.) | 92.49 (28.6) | 103.7 (28.5) | 87.0 (26.4) |
SA, Suicide attempt; SIB, self-injurious behaviors; SIQ, Suicide Ideation Questionnaire; MDE, major depressive episode; Bipolar d/o, bipolar disorder, including bipolar disorder I and bipolar disorder II; Phobic Anx d/o, phobic anxiety disorder, including social phobia, generalized anxiety disorder, panic disorder and agoraphobia; Substance Use d/o, substance use disorders, including alcohol and drug abuse or dependence; Disruptive d/o, disruptive disorders, including conduct disorder and oppositional defiant disorder; Eating d/o, eating disorders, including anorexia nervosa and bulimia nervosa; FAD-GF, Family Assessment Device Global Functioning; CSA, childhood sexual abuse; Hx, history; BPD, borderline personality disorder AIM, Affective Intensity Questionnaire; AQ, Aggression Questionnaire; s.d., standard deviation.
p < 0.05.
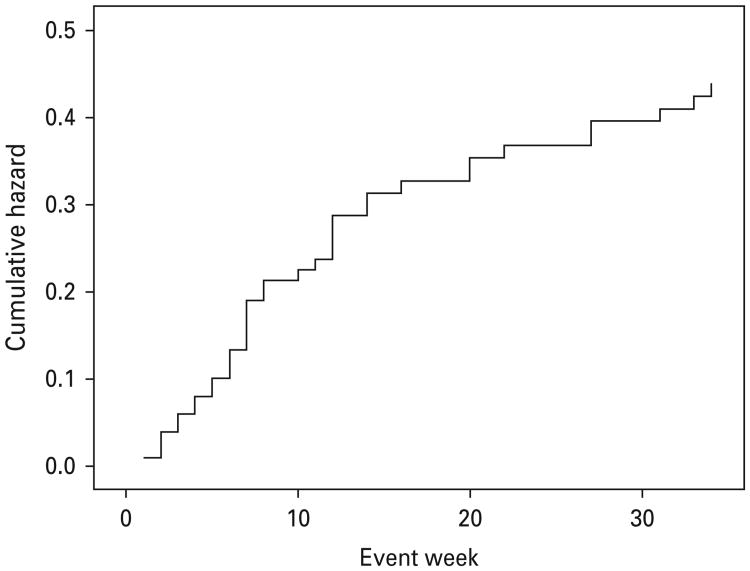
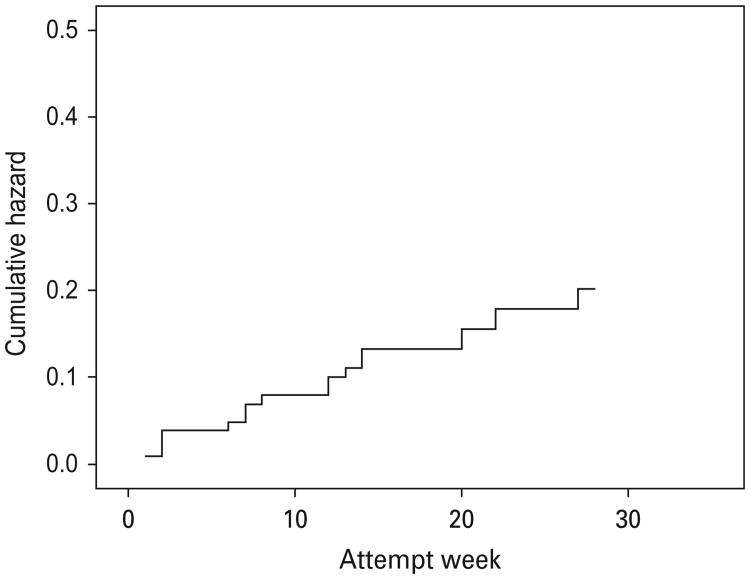
During the follow-up period, 19 (18%) participants made a suicide attempt. In addition, 27 (26%) participants were admitted to the emergency department, 24 (23%) of whom were admitted for suicide-related reasons. Twenty-nine (28%) were readmitted to an in-patient psychiatric unit due to suicide risk. A total of 37 (36%) participants met the criteria for a suicide event during follow-up, with 11 reporting both an attempt and an emergency intervention. The median number of weeks to the first suicide event was 8 (Fig. 1) and the median number of weeks to the first suicide attempt was 12 (Fig. 2). The results using the suicide event outcome and suicide attempt outcome were in the same direction; all subsequent results are based on time to suicide event outcome.
Fig. 1.
Cumulative hazard for suicide events.
Fig. 2.
Cumulative hazard for suicide attempts.
Table 2 depicts demographic characteristics by suicide event status. Mean age and gender were not different in those with and without suicide events. Because of the large number of participants who reported multiple racial and ethnic categories, we analyzed race and ethnicity by creating dichotomous grouping for: (1) White versus non-White; (2) Hispanic versus non-Hispanic; (3) Black versus non-Black; and (4) Any minority versus No minority status (i.e. non-Hispanic Caucasian). Black race significantly predicted time to a suicide event during follow-up [Wald χ2 = 6.40, hazard ratio (HR) 2.91, p = 0.011]; this variable was included as a covariate in the multivariate model.
Table 2. Univariate Cox proportional hazards regression analyses by suicide event group.
| B (s.e.) | Wald χ2 | HR | 95% CI | |
|---|---|---|---|---|
| Age | −0.03 (0.12) | 0.06 | 0.97 | 0.77–1.23 |
| Female | −0.13 (0.34) | 0.13 | 0.88 | 0.45–1.71 |
| Caucasian | −0.35 (0.42) | 0.69 | 0.71 | 0.31–1.61 |
| Black* | 1.07 (0.42) | 6.40 | 2.91 | 1.27–6.67 |
| Hispanic | 0.30 (0.42) | 0.51 | 1.35 | 0.59–3.08 |
| Any minority | 0.42 (0.37) | 1.30 | 1.53 | 0.74–3.17 |
| Past history SA | 0.47 (0.36) | 1.67 | 1.60 | 0.79–3.25 |
| Any SIB | 0.21 (0.45) | 0.22 | 1.23 | 0.51–2.99 |
| SIQ* | 0.01 (0.01) | 4.81 | 1.01 | 1.00–1.02 |
| MDE | −0.25 (0.42) | 0.36 | 0.78 | 0.34–1.77 |
| Phobic Anx d/o | −0.36 (0.34) | 1.13 | 0.70 | 0.36–1.36 |
| PTSD* | 0.71 (0.34) | 4.31 | 2.02 | 1.04–3.94 |
| Substance Use d/o | −0.16 (0.45) | 0.13 | 0.85 | 0.36–2.04 |
| Disruptive d/o | 0.31 (0.33) | 0.90 | 1.37 | 0.72–2.61 |
| ADHD | 0.16 (0.33) | 0.23 | 1.17 | 0.61–2.24 |
| FAD-GF Adolescent | 0.14 (0.28) | 0.26 | 1.16 | 0.66–2.01 |
| FAD-GF Parent | −0.01 (0.45) | 0.01 | 1.00 | 0.41–2.41 |
| CSA** | 1.04 (0.37) | 7.70 | 2.83 | 1.36–5.89 |
| Fam Hx suicidal behav | 0.37 (0.41) | 0.82 | 1.45 | 0.65–3.25 |
| BPD*** | 0.56 (0.33) | 2.89 | 1.75 | 0.97–5.11 |
| AIM (Positive)** | −0.60 (0.21) | 8.43 | 0.55 | 0.37–0.82 |
| AQ Total** | 0.02 (0.01) | 6.17 | 1.02 | 1.01–1.03 |
HR, Hazard ratio; CI, confidence interval; SA, suicide attempt; SIB, self-injurious behaviors; SIQ, Suicide Ideation Questionnaire; MDE, major depressive episode; Phobic Anx d/o, phobic anxiety disorder, including social phobia, generalized anxiety disorder, panic disorder and agoraphobia; PTSD, post-traumatic stress disorder; Substance Use d/o, substance use disorders, including alcohol and drug abuse or dependence; Disruptive d/o, disruptive disorders, including conduct disorder and oppositional defiant disorder; ADHD, attention deficit hyperactivity disorder; FAD-GF, Family Assessment Device Global Functioning; CSA, childhood sexual abuse; Fam Hx suicidal behav, family history of suicidal behavior; BPD, borderline personality disorder; AIM, Affective Intensity Questionnaire; AQ, Aggression Questionnaire; s.e., standard error; s.d., standard deviation.
p<0.05,
p<0.01,
p<0.10.
History of suicidal and self-injurious behaviors and suicide ideation at baseline were examined as univariate predictors of a suicide event over follow-up (Table 2). Approximately two-thirds of the sample had a history of suicide attempts. A majority of the sample reported a history of self-injurious behaviors (with or without intent to die). Neither a history of suicide attempts nor self-injurious behaviors predicted a suicide event during follow-up. Severity of suicidal ideation at baseline using the SIQ was a significant prospective predictor of time to suicide event (Wald χ2 = 4.81, HR 1.01, p=0.028).
Post-traumatic stress disorder (PTSD) was the only Axis I disorder that significantly predicted time to suicide event (Wald χ2 = 4.31, HR 2.02, p = 0.038). Positive incidents of any bipolar disorder [I, II, not otherwise specified (NOS)] and any eating disorder (anorexia nervosa, bulimia nervosa, eating disorder NOS) were too few to analyze.
Family functioning and family history of suicidal behaviors did not significantly predict suicide events. However, CSA was a strong significant predictor of time to suicide event (Wald χ2 = 7.71, HR 2.83, p=0.005).
BPD diagnosis, although not significant (Wald χ2 = 2.89, HR 1.75; p = 0.089), met the threshold for inclusion in the multivariate model. After removing the self-injurious behaviors criterion to mitigate the possibility that the item reflected a suicide attempt, the sum of the remaining eight BPD criteria operationalized continuously was a significant predictor of time to suicide event (Wald χ2 = 6.44, HR 1.22, p = 0.01) (the inclusion of all nine BPD criteria yielded consistent findings). In keeping with other studies, categorical BPD diagnosis was entered as a covariate in the multivariate model.
Only the positive affect subscale of the AIM was significant in predicting time to suicide event, with lower positive affect associated with higher risk (Wald χ2=8.43, HR 0.55, p=0.004). Subsequent multivariate models included only this AIM subscale. This finding prompted us to consider whether this was better accounted for by depression. Using MDD diagnosis, number of MDD symptoms and the anhedonia criterion as covariates, low positive affectivity remained significant in each of these multivariate models, with the effect size relatively unchanged.
Because the AQ subscales were highly correlated with one another (range 0.419–0.916), only the AQ total was analyzed in the multivariate models for parsimony. It was a significant predictor of time to suicide event (Wald χ2 = 6.17, HR 1.02, p = 0.013).
All univariate predictors with significance level <0.10 (Black race, SIQ baseline score, CSA, PTSD diagnosis, BPD diagnosis, positive affectivity and AQ total) were entered simultaneously into a multivariate Cox proportional hazards regression model. We did not include as covariates the two variables (bipolar disorder and minority race) that differed between those with and without follow-up data because of the overlap between minority race and Black race and because the sample size of those with bipolar disorder (nine in the sample, two with subsequent suicide events and seven without) was too limited for analysis. As shown in Table 3, the results from the multivariate Cox regression model indicate that the only variables that remained significant are Black race, CSA, positive affectivity and aggression.
Table 3. Multivariate analyses with all significant univariate predictors.
| B (s.e.) | Wald χ2 | HR | 95% CI | |
|---|---|---|---|---|
| Black* | 1.12 (0.54) | 4.30 | 3.08 | 1.06–8.90 |
| SIQ | 0.01 (0.01) | 1.01 | 1.01 | 1.00–1.02 |
| PTSD | −0.51 (0.49) | 1.08 | 0.60 | 0.23–1.56 |
| CSA*** | 1.51 (0.48) | 10.10 | 4.52 | 1.78–11.47 |
| BPD | 0.47 (0.45) | 1.09 | 1.60 | 0.66–3.86 |
| AIM Positive* | −0.61 (0.28) | 4.87 | 0.55 | 0.32–0.94 |
| AQ Total** | 0.03 (0.01) | 9.64 | 1.03 | 1.01–1.05 |
HR, Hazard ratio; CI, confidence interval; SIQ, Suicide Ideation Questionnaire; PTSD, post-traumatic stress disorder; CSA, childhood sexual abuse; BPD, borderline personality disorder; AIM, Affective Intensity Questionnaire; AQ, Aggression Questionnaire; s.e., standard error.
p<0.05,
p<0.01,
p<0.001.
Discussion
High rates of repeat suicide attempts (19%) and suicide events (37%) over 6 months of follow-up were observed in our sample of in-patient suicidal adolescents. These rates were consistent with, and in some cases higher than, those from studies of clinical high-risk adolescent samples (King et al. 1995; Goldston et al. 1999; Prinstein et al. 2008; Brent et al. 2009). Collectively, these studies demonstrate the pernicious course of suicidal behavior in high-risk adolescents. Our outcome of suicide events includes both suicide attempts and emergency interventions to intercede an attempt. Some of these events may thus reflect a positive outcome of seeking help. Nevertheless, these outcomes indicate that the period of suicidal concern continues beyond discharge from an in-patient unit. The mean of 8 weeks to the first suicide event demonstrates that the risk of repeated suicide attempts is particularly high during the months following discharge from a psychiatric in-patient unit.
Black race significantly predicted time to suicide event during follow-up. This was unexpected because historically, Caucasian youth and adults have higher rates of suicide deaths and suicidal behavior compared to their Black and Hispanic counterparts (Sorenson & Golding, 1988; Garlow et al. 2005). However, more recent reports suggest that the gap is closing, with increased rates of suicidal behavior in Black Americans (Balis & Postolache, 2008). However, to the best of our knowledge, no study has reported higher rates among Black youth compared to Caucasian youth. Our sample size of Black participants was small, thereby limiting inferences to the larger population.
Contrary to expectations and other documented findings, a history of a previous suicide attempt did not significantly predict time to suicide event during follow-up in our sample. In the present study two-thirds of the sample had a past suicide attempt; thus it can be argued that there was not enough variability to detect a lower frequency event. It may be that a past history of suicide attempts is a more useful and reliable predictor of subsequent suicide attempts in less acute settings such as in community, school or primary care samples. Indeed, most (but not all) studies that have identified past history of suicide attempts as a significant predictor of future attempts have been conducted on community as opposed to clinical samples (Borges et al. 2008; Nrugham et al. 2008). Although some studies of acute in-patient or ER samples have also found that past history of suicide attempts significantly predicted subsequent suicide attempts (Greenfield et al. 2008), several other studies report number of past attempts (King et al. 2010), severity of depressed mood (Goldston et al. 1999) or suicidal ideation (Prinstein et al. 2008) as being more salient in an acute sample. In our study, severity of suicidal ideation over the past month as assessed by the SIQ was significant, although only at the univariate level. Thus, it may be that chronicity and/or severity of suicidal ideation is a better predictor in high-risk samples where the majority may have a suicide attempt history. Our lack of finding regarding past history of suicide attempts highlights a problem faced by numerous acute care providers: that it is particularly challenging to identify patients at high risk for recurrent suicidal behavior in an acute setting.
Aside from PTSD, Axis I disorders at baseline did not predict time to suicide event over follow-up. The significance of PTSD seemed to be better accounted for by a history of CSA, which remained significant in the multivariate model. In the present sample 44% of those meeting criteria for PTSD also reported CSA. Other studies that have examined suicidal adolescents have yielded more robust associations between psychiatric disorders, particularly MDD, and prospective suicidal behavior. However, the present sample had a particularly high prevalence of MDD, with more than 80% of the sample endorsing a current depressive episode. It is possible that depression may predict suicidal ideation but not suicide plans or attempts among those with ideation (Nock et al. 2010). A more qualitative evaluation of depression such as severity or chronicity of depressive symptoms may be a more useful predictor of future suicidal behavior. Unfortunately, these data were not available in the present sample.
Our results indicate that family environment, as assessed by the FAD-GF, and family history of suicidal behavior did not significantly predict time to suicide events. CSA was significant in predicting time to suicide event in both univariate and multivariate models. In studies of adults, CSA has been demonstrated to be a very robust predictor of suicidal behavior, remaining significant even after controlling for multiple psychiatric disorders including BPD and PTSD (Yen et al. 2004). The adverse short- and long-term consequences of CSA underscore the need for the assessment of childhood abuse and also public health awareness of its ramifications, such as increased suicide risk.
Among our hypothesized sets of predictors, variables associated with personality/temperament were generally stronger predictors of time to suicide events than other types of predictors. Few studies have examined BPD in adolescents despite the strong associations between BPD symptoms and suicidal behaviors in adults. In the present study, to elucidate the association between BPD symptoms and suicidality, a conservative analytic approach was taken in which BPD symptoms was calculated as a continuous variable without the self-injurious behavior criterion and was found to be significant in predicting time to suicide event in univariate analyses but not in multivariate analyses. This finding suggests that the evaluation of BPD characteristics in high-risk adolescents, although controversial and not without caveats, may still be warranted.
Two personality/temperament dimensions were robust in predicting suicide events: low positive affectivity and aggression. Both are addressed in the National Institute of Mental Health (NIMH) Research Domain Criteria (Sanislow et al. 2010) as underlying (cross-cutting) constructs that can be examined through multiple levels of analyses ranging from the molecular level to observed behavior. The positive affect valence and negative affect valence are conceptualized as broader domains or ‘systems’ and aggression is conceptualized as a construct within the negative valence system.
Low positive affect intensity was a stronger predictor of time to suicidal events than negative affect intensity, despite the commonly accepted belief that suicidal ideation and behaviors arise from negative emotions. It is likely that both act on suicidal behaviors; perhaps high negative affectivity is ubiquitous and non-discriminating in this high-risk sample. Nevertheless, our findings suggest the need to also focus on positive affect along with the traditional risk factors that prototypically involve negative affect and depressive symptomatology. Our results regarding low positive affectivity as a prospective predictor of time to suicidal events are novel; to the best of our knowledge, no other prospective study has examined low positive affectivity as a risk factor for suicidal behavior in adults or adolescents. One study reported positive future thinking to be a more important predictor of suicidal ideation than global attitudes of hopelessness in suicidal adult in-patients (O'Connor et al. 2008). That study, in addition to our own results, supports a framework of conceptualizing opposite valence constructs as being distinct and uniquely relevant.
Not surprisingly, aggression predicted time to subsequent suicidal events in this high-risk group of adolescents. Although both impulsivity and aggression have been widely linked to suicidal behaviors, some have speculated that aggression has a stronger association with suicidal behaviors than impulsivity (Brent et al. 1994; Perroud et al. 2011). However, most of these studies have examined adult samples. Notably, emerging research suggests that aggression and impulsivity are likely to be more prominent forces for adolescents than adults (Parellada et al. 2008). In a prospective study of children of parents with a history of mood disorder and suicidal behaviors, self-reported impulsive-aggression in offspring predicted earlier time to and greater hazard of a suicidal event (Melhem et al. 2007). Conversely, in another prospective study of 270 acutely suicidal adolescents, aggression was not directly related to suicide attempts concurrently or prospectively. However, in those who reported more aggression, those with internalizing symptoms were more likely to make a suicide attempt (Kerr et al. 2007). Our study sample, with 80% reporting a recent major depressive episode, is indeed a highly co-morbid sample with high rates of both internalizing and externalizing disorders. Thus, our study findings suggest that aggression, particularly when co-morbid with internalizing disorder, significantly increases suicide event risk in adolescents.
This study has some limitations to consider. The retention rate for this 6-month follow-up study was adequate (83% at 6 months) but may have affected findings despite the lack of differences on key predictor variables. Our methodology relies solely on self- and other-report; there were no behavioral assessments to validate and better understand our results with regard to positive affect intensity and aggression. Finally, there may be limitations to generalizability in that this is a very acutely severe sample. Our sample was recruited from a single in-patient setting. Two-thirds of our participants had a past history of suicide attempts and nearly 80% had engaged in self-injuring behaviors. However, our ability to distinguish prospective predictors for suicide events during follow-up in the context of an acutely severe sample lends strength to these findings and has particular relevance to the acute settings in which many of these patients are treated.
In summary, the present study was a naturalistic 6-month follow-up observation of 104 suicidal adolescents who were admitted to an in-patient psychiatric unit due to suicide risk. In a multivariate model, only Black race, low positive affect intensity, aggression and CSA remained significant predictors. These results have direct implications for treatment and assessment. Increased awareness of the closing gap between Caucasian and Black youth with respect to suicidal events should improve the accuracy of suicide risk assessment. The assessment of CSA is a high priority in this population. Our findings with regard to positive affect intensity and aggression are concordant with the recent emphasis on dimensional constructs that cut across multiple psychiatric disorders, and suggest that these constructs be targeted in assessment and in intervention programs for suicidal adolescents.
Acknowledgments
This study was supported by NIMH grant K23 MH69904 to Dr S. Yen. We thank our clinical collaborators (Drs D. Picotte, J. Solomon, S. Shephard and G. Tarnoff) and the research staff (H. Pelletier, J. Lipschitz, S. Samways and C. Melvin) for their assistance in this study.
Footnotes
Declaration of Interest: None.
References
- Aglan A, Kerfoot M, Pickles A. Pathways from adolescent deliberate self-poisoning to early adult outcomes: a six-year follow-up. Journal of Child Psychology and Psychiatry. 2008;49:508–515. doi: 10.1111/j.1469-7610.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- Balis T, Postolache TT. Ethnic differences in adolescent suicide in the United States. International Journal of Child Health and Human Development. 2008;1:281–296. [PMC free article] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: findings from a longitudinal study. Psychological Medicine. 2007;37:431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Bondurant H, Greenfield B, Tse SM. Construct validity of the adolescent borderline personality disorder: a review. Canadian Child and Adolescent Psychiatry Review. 2004;13:53–57. [PMC free article] [PubMed] [Google Scholar]
- Borges GJ, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: a 10-year follow-up study using the National Comorbidity Surveys. Journal of Affective Disorders. 2008;105:25–33. doi: 10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Greenhill LL, Compton S, Emslie G, Wells K, Walkup JT, Vitiello B, Bukstein O, Stanley B, Posner K, Kennard BD, Cwik MF, Wagner A, Coffey B, March JS, Riddle M, Goldstein T, Curry J, Barnett S, Capasso L, Zelazney J, Hughes J, Shen S, Gugga SS, Tunder JB. The Treatment of Adolescent Suicide Attempters study (TASA): predictors of suicidal events in an open treatment trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, Rather C. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1080–1086. doi: 10.1097/00004583-199410000-00003. [DOI] [PubMed] [Google Scholar]
- Brinkman-Sull DC, Overholser JC, Silverman E. Risk of future suicide attempts in adolescent psychiatric inpatients at 18-month follow-up. Suicide and Life-Threatening Behavior. 2000;30:327–340. [PubMed] [Google Scholar]
- Bronisch T, Hofler M, Lieb R. Smoking predicts suicidality: findings from a prospective community study. Journal of Affective Disorders. 2008;108:135–145. doi: 10.1016/j.jad.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. Journal of Personality and Social Psychology. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Garlow SJ, Purselle D, Heninger MD. Ethnic differences in patterns of suicide across the life cycle. American Journal of Psychiatry. 2005;162:319–323. doi: 10.1176/appi.ajp.162.2.319. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Reboussin BA, Mayfield A, Frazier PH, Treadway SL. Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: developmental changes. Journal of Consulting and Clinical Psychology. 2009;77:281–290. doi: 10.1037/a0014732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin DM, Frazier PH, Kelley AE. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:660–671. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Reboussin BA, Daniel SS. Predictors of suicide attempts: state and trait components. Journal of Abnormal Psychology. 2006;115:842–849. doi: 10.1037/0021-843X.115.4.842. [DOI] [PubMed] [Google Scholar]
- Gould MS, King R, Greenwald MA, Fisher P, Schwab-Stone M, Kramer R, Flisher AJ, Goodman S, Canino G, Shaffer D. Psychopathology associated with suicidal ideation and attempts among children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:915–923. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- Greenfield B, Henry M, Weiss M, Tse SM, Guile JM, Dougherty JM, Dougherty G, Zhang X, Fombonne E, Lis E, Lapalme-Remis S, Harnden B. Previously suicidal adolescents: predictors of six-month outcome. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2008;17:197–201. [PMC free article] [PubMed] [Google Scholar]
- Hills AL, Afifi TO, Cox BJ, Bienvenu OJ, Sareen J. Externalizing psychopathology and risk for suicide attempt: cross-sectional and longitudinal findings from the Baltimore Epidemiologic Catchment Area Study. Journal of Nervous and Mental Disease. 2009;197:293–297. doi: 10.1097/NMD.0b013e3181a206e0. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version (K-SADS-PL) : initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Follow-up Evaluation. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kerr DC, Washburn JJ, Feingold A, Kramer AC, Ivey AZ, King CA. Sequelae of aggression in acutely suicidal adolescents. Journal of Abnormal Child Psychology. 2007;35:817–830. doi: 10.1007/s10802-007-9132-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- King CA, Kerr DC, Passarelli MN, Foster CE, Merchant CR. One-year follow-up of suicidal adolescents : parental history of mental health problems and time to post-hospitalization attempt. Journal of Youth and Adolescence. 2010;39:219–232. doi: 10.1007/s10964-009-9480-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Segal H, Kaminski K, Naylor MW, Ghaziuddin N, Radpour L. A prospective study of adolescent suicidal behavior following hospitalization. Suicide and Life-Threatening Behavior. 1995;25:327–338. [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Gatsonis C. Suicidal behaviors and childhood-onset depressive disorders: a longitudinal investigation. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:8–20. doi: 10.1097/00004583-199301000-00003. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: a review. Journal of Research in Personality. 1987;21:1–39. [Google Scholar]
- Larsen RJ, Diener E, Cropanzano RS. Cognitive operations associated with individual differences in affect intensity. Journal of Personality and Social Psychology. 1987;53:767–774. doi: 10.1037//0022-3514.53.4.767. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology. 1994;62:297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3:25–46. [Google Scholar]
- Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychological Medicine. 2007;37:1183–1192. doi: 10.1017/S003329170700027X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Brent DA, Ziegler M, Iyengar S, Kolko D, Oquendo M, Birmaher B, Burke A, Zelazny J, Stanley B, Mann JJ. Familial pathways to early-onset suicidal behavior: familial and individual antecedents of suicidal behavior. American Journal of Psychiatry. 2007;164:1364–1370. doi: 10.1176/appi.ajp.2007.06091522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrou F, Gaudie J, Lawrence D, Silburn SR, Stanley FJ, Zubrick SR. Antecedents of hospital admission for deliberate self-harm from a 14-year follow-up study using data-linkage. BMC Psychiatry. 2010;10:1–11. doi: 10.1186/1471-244X-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nrugham L, Larsson B, Sund AM. Predictors of suicidal acts across adolescence: influences of familial, peer and individual factors. Journal of Affective Disorders. 2008;109:35–45. doi: 10.1016/j.jad.2007.11.001. [DOI] [PubMed] [Google Scholar]
- O'Connor RC, Fraser L, Whyte M, MacHale S, Masterton G. A comparison of specific positive future expectancies and global hopelessness as predictors of suicidal ideation in a prospective study of repeat self-harmers. Journal of Affective Disorders. 2008;110:207–214. doi: 10.1016/j.jad.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Parellada M, Saiz P, Moreno D, Vidal J, Llorente C, Álvarez M, García-Portilla P, Ruiz-Sancho A, Arango C, Bobes J. Is attempted suicide different in adolescent and adults? Psychiatry Research. 2008;157:131–137. doi: 10.1016/j.psychres.2007.02.012. [DOI] [PubMed] [Google Scholar]
- Perroud N, Baud P, Mouthon D, Courtet P, Malafosse A. Impulsivity, aggression and suicidal behavior in unipolar and bipolar disorders. Journal of Affective Disorders. 2011;134:112–118. doi: 10.1016/j.jad.2011.05.048. [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Klerman GL, Hurt SW, Kakuma T, Peskin JR, Siefker CA. Suicidal children grow up: rates and psychosocial risk factors for suicide attempts during follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:106–113. doi: 10.1097/00004583-199301000-00016. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds WM. Suicide Ideation Questionnaire. Psychological Assessment Resources; Odessa, FL: 1985. [Google Scholar]
- Riala K, Alaraisanen A, Taanila A, Hakko H, Timonen M, Rasanen P. Regular daily smoking among 14-year-old adolescents increases the subsequent risk for suicide: the Northern Finland 1966 Birth Cohort Study. Journal of Clinical Psychiatry. 2007;68:775–780. doi: 10.4088/jcp.v68n0518. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Pine DP, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Wang RK, Cuthbert BN. Developing constructs for psychopathology research: research domain criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Sharp C, Ha C, Michonski J, Venta A, Carbone C. Borderline personality disorder in adolescents: evidence in support of the Childhood Interview for DSM-IV Borderline Personality Disorder in a sample of adolescent inpatients. Comprehensive Psychiatry. 2012;53:765–774. doi: 10.1016/j.comppsych.2011.12.003. [DOI] [PubMed] [Google Scholar]
- Sorenson SB, Golding JM. Suicide ideation and attempts in Hispanics and non-Hispanic whites : demographic and psychiatric disorder issues. Suicide and Life-Threatening Behavior. 1988;18:205–218. doi: 10.1111/j.1943-278x.1988.tb00157.x. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annual Review of Clinical Psychology. 2006;2:237–266. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- Spirito A, Valeri S, Boergers J, Donaldson D. Predictors of continued suicidal behavior in adolescents following a suicide attempt. Journal of Clinical Child and Adolescent Psychology. 2003;32:284–289. doi: 10.1207/S15374424JCCP3202_14. [DOI] [PubMed] [Google Scholar]
- Wichstrom L. Predictors of adolescent suicide attempters: a naturally representative longitudinal study of Norwegian adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:603–610. doi: 10.1097/00004583-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, McGlashan TH, Zanarini MC, Morey LC. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Skodol AE, Grilo CM, Stout RL, Morey LC, Zanarini MC, McGlashan TH, Daversa MT, Gunderson JG. Personality traits as prospective predictors of suicide attempts. Acta Psychiatrica Scandinavica. 2009;120:222–229. doi: 10.1111/j.1600-0447.2009.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahl DL, Hawton K. Repetition of deliberate self-harm and subsequent suicide risk: long-term follow-up study of 11,583 patients. British Journal of Psychiatry. 2004;185:70–75. doi: 10.1192/bjp.185.1.70. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The diagnostic interview for personality disorders: interrater and test-retest reliability. Comprehensive Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorder. Laboratory for the Study of Adult Development, McLean Hospital; Belmont, MA: 1996. [Google Scholar]