Abstract
Objective
Most pediatric emergency department (ED) visits are due to acute abdominal pain. Sonography is a reliable technique for differential diagnosis. The objective of this study was to re-appraise the role of sonography in evaluating acute abdominal pain in children.
Methods
Retrospective chart review of children aged <18 years with acute abdominal pain who visited the emergency department and underwent sonography between December 2004 and June 2006 was conducted. Patients with trauma were excluded.
Findings
775 patients (478 males and 297 females, age 1-17 years; mean age 6±5.8 years) enrolled the study. Among 284 children with suspected appendicitis, 118 were diagnosed with appendicitis using sonography. Of 663 children without appendicitis, majority had gastrointestinal tract infection or non-specific abdominal pain. Other specific diagnoses were established by clinical, laboratory, and radiologic finings in 51 patients (including renal diseases in 20, intussusceptions in 15, gynecologic diseases in six, extra-abdominal disease in 4, and gastrointestinal tract abnormalities in 2). The sensitivity and specificity of sonography was 96.4% and 76.7%, respectively, for diagnosing appendicitis and 100% and 100%, respectively, for intussusception.
Conclusion
Sonography remains a very effective, complementary, non-invasive method for evaluating children with acute abdominal pain, especially those with suspected appendicitis or intussusception.
Keywords: Ultrasound, Abdominal Pain, Emergency, Children
Introduction
Acute abdominal pain is a common clinical problem among children visiting the emergency department (ED). It can be associated with a wide variety of surgical and non-surgical conditions. Although only a small fraction of children presenting with abdominal pain will actually have an organic cause necessitating interventional management, majority of the surgical conditions is acute appendicitis[1–3]. Although medical history and physical examination can help physicians to differentiate among various possible causes, sonography has proven to be a reliable technique for establishing the diagnosis of appendicitis in children[4–6].
The purpose of this study was to re-appraise the role of sonography in children with acute abdominal pain in the ED. The more common and clinically significant causes of abdominal pain in children are also discussed in detail.
Subjects and Methods
This was a retrospective registry-based cohort study of bedside abdominal sonography performed in the ED by the pediatric emergency physician who was board certified in pediatric gastroenterology. We identified from the ED sonographic log, consecutive patients aged <18 years who had acute abdominal pain from December 2004 to June 2006. Patients with trauma were excluded.
All sonographic studies were performed using a commercially available, real-time scanner with a 5-MHz linear transducer (TITAN; Sonosite Inc, Bothell, WA. USA). The sonographic criteria for acute appendicitis included a blind non-compressible tubular structure representing an appendix (long-axis scan), and an echogenic center presenting as a “target sign” on short-axis scan. A shadow-casting fecalith or relatively hypo-echoic pus collection in the lumen of the appendix might also be present[7, 8].
Demographic data obtained included age, sex, clinical presentation, abdominal radiographs, abdominal ultrasound, laboratory tests, and final diagnosis.
The final diagnoses were recorded by reviewing the chart entries made by the pediatric emergency physician after clinical history, laboratory data, and radiologic findings. A final diagnosis of acute appendicitis was based on histologic examination of the excised appendix.
The hospital's institutional review board concurred that this retrospective study was a continuous quality improvement initiative for patient care and did not require informed consent.
Findings
There were 775 ED sonography studies for acute abdominal pain in the pediatric emergency department performed during the 17-month study period. There were 478 males and 297 females, with age range of 1-8 years (mean age, 6±5.8 years). The patients were divided into two groups based on the sonographic findings: the positive group and the negative group. The results are summarized in Table 1.
Table 1.
Patient characteristics, final diagnoses and sonographic findings
| Final diagnosis | Sonographic findings | |
|---|---|---|
| Positive (n = 644, 83%) | Negative (n = 131, 17%) | |
| Appendicitis (n = 112, 14.4%) | 108 | 4 |
| GI infection (n = 505, 65.2%) | 495 | 10 |
| Renal disease (n = 20, 2.6%) | ||
| Hydronephrosis | 15 | 0 |
| Urinary tract infection | 2 | 3 |
| Intussusception (n = 15, 1.9%) | 15 | 0 |
| Gynecologic disease (n = 6, 0.7%) | ||
| Ovarian cyst | 4 | 0 |
| Pelvic inflammatory disease | 2 | 0 |
| GI anomalies (n = 2, 0.3%) | ||
| Lymphangioma | 1 | 0 |
| Hernia | 1 | 0 |
| Extra-abdominal disease (n = 4, 0.6%) | 1 | 3 |
| Non specific abdominal pain (abdominal pain of unknown origin) (n = 111, 14.3%) | 0 | 111 |
Appendicitis
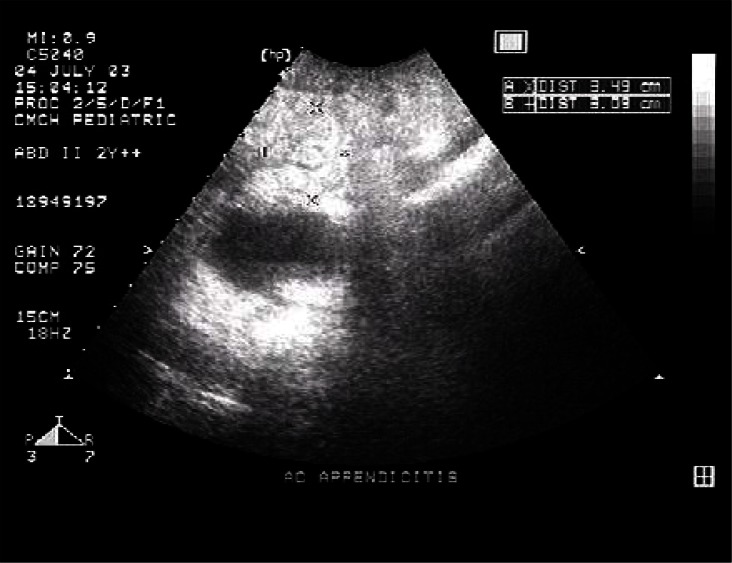
Of the 287 children with suspected appendicitis, 118 had confirmed diagnosis of appendicitis by sonography (Fig. 1). Appendicitis was proven by pathology after surgery in 108 patients. Four patients not initially diagnosed as having appendicitis by ultrasound had appendicitis proven by post-operative histo-pathology. The sensitivity and specificity for diagnosing appendicitis by sonography were 96.4% and 76.7%, respectively. Moreover, 82% of children with appendicitis had at least two of the following associated signs or symptoms: fever, shifting pain, nausea/vomiting, diarrhea, and rebound tenderness.
Fig. 1.
Sonographic image shows the transverse section of an acutely inflamed appendix with an 11-mm outer diameter. Note the surrounding hyperechoic inflamed fatty tissue
Gastrointestinal tract infection
The sonographic findings of patients with gastrointestinal tract infection showed thickening of the bowel walls. Ten of these patients were diagnosed as appendicitis by ultrasound initially and underwent appendectomy. However their post-surgery pathologic examination revealed no inflammation of the excised appendices.
Abdominal pain of unknown origin
There were 111 patients with final clinical diagnoses of abdominal pain of unknown origin. All of them had negative sonography results and all were treated with intravenous hydration and several hours of observation in the ED, and then discharged asymptomatic or with improved abdominal pain.
Renal disease
There were 15 patients with acute abdominal pain who had hydronephrosis proven by sonography. Five children had urinary tract infection based on positive urine culture findings, one had identified focal echogenic areas in the renal parenchyma suggestive of acute focal pyelonephritis, and another one had thickened change of the urinary bladder suggestive of cystitis. The remaining three patients had no specific sonographic findings.
Intussusception
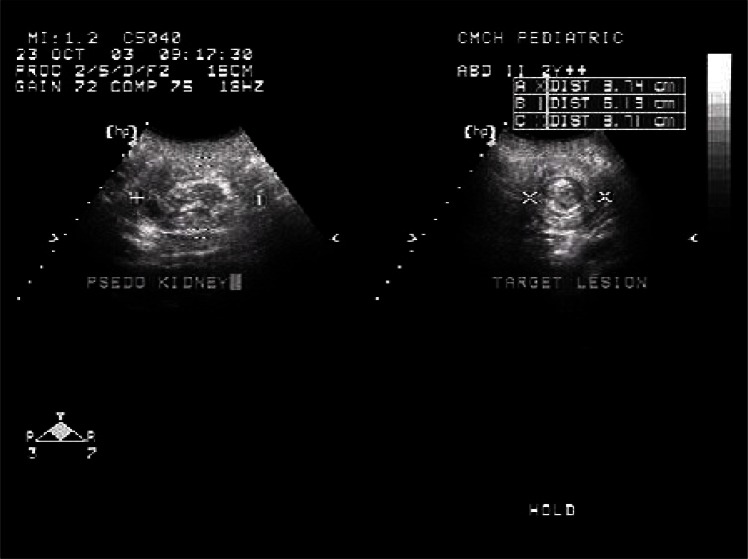
Patients with intussusception were all younger than 3 years. Their sonographic appearance through the mid abdomen showed concentric appearance on a transverse section through an intussusception and the hay fork appearance on a longitudinal section (Fig. 2). Fourteen (86%) suffered from intermittent abdominal pain or irritable crying. One who had vomitus with currant jelly stool underwent surgery because of failed barium reduction. The accuracy of diagnosing intussusception was 100%.
Fig. 2.
Sonographic image of intussusception shows a concentric appearance on a transverse section and the hay fork appearance on a longitudinal section
Gynecologic disease
Of the six children with gynecologic disease, four had ovarian cysts and two had pelvic inflammatory diseases. Sonographic findings of one patient showed prominent endometrium with free peritoneal fluid, which required surgical intervention for suspected ruptured hemorrhagic ovarian cyst. Another five patients were all discharged with observation and medical treatment. There were no specific sonographic findings in patients with pelvic inflammation disease except one who had free fluid in the cul-de-sac.
GI abnormalities
A cystic mass with size of 6.9 × 4.6 cm was noted over the right lower quadrant of the abdomen by sonography in one patient and duplication or omental cyst was considered after abdominal CT. Exploratory laparotomy was performed and cystic duplication was proven by histo-pathology. The sonographic findings of another patient showed features of intestinal obstruction with a zone of transition between dilated and non-dilated bowel, with mild ascites. Abdominal CT revealed encapsulated small bowel loops in the right side of the abdomen and left-sided displacement of the ascending colon. A diagnosis of right para-duodenal hernia was made, which was subsequently proven by surgical exploration.
Extra-abdominal disease
Four patients had final diagnoses of extra-abdominal disease, which was pneumonia in three patients and myocarditis in one. The patient with myocarditis initially presented with abdominal pain. Moderate ascites was documented by abdominal sonography. His blood pressure dropped in the ED and he was admitted to the intensive care unit (ICU) for further care. The diagnosis of myocarditis was made by clinical evidence and echocardiogram. However, there were no specific abdominal sonographic findings in the other three patients with pneumonia.
Discussion
The purpose of this study was to re-appraise the role of sonography for evaluating acute abdominal pain in children visiting the ED. In 775 children with abdominal pain who underwent sonography in the ED, the three most frequent diagnoses were gastrointestinal infection (65%), appendicitis (14%), and non-specific abdominal pain (13%). In the study by Marilyn J et al, the three most frequent diagnoses in 178 children with abdominal pain who underwent sonography were non-specific abdominal pain (30-38%), medical conditions (20-26%), and surgical emergencies (30-38%)[9]. Appendicitis is one of the most worrisome and serious conditions in acute abdominal pain. It is also the most common pediatric surgical emergency and should be ruled out for all children with abdominal pain.
Appendicitis
Acute appendicitis is a difficult disease to diagnose in children. Thus, there should be a high index of suspicion about it in children with acute abdomen pain. Detailed history taking and physical examination are necessary. During the study period, appendicitis was diagnosed in an additional 66 patients not included in the study population, including 55 who underwent surgery without ultrasound and CT imaging studies. Another 11 patients underwent CT scan first without ultrasound. In the present study, five patients underwent both sonography and abdominal CT scan. Two had no appendicitis, one had bowel wall edema, and one had ovarian cyst. The sensitivity and specificity for diagnosing appendicitis by sonography in the present study were 96.4% and 76.7%, respectively, whereas in literature the sensitivity and specificity were 86-100% and 89-98%, respectively[10].
Sonography and CT scan are not always indicated when patients have typical presentations of appendicitis, but sonography can be used as the initial diagnostic tool for patients with suspected appendicitis but without typical presentation because sonography does no harm and has almost no contraindications. The advantage is that sonography is a cost-effective, quick, painless, and non-invasive investigation with no radiation hazards or parental contrast reaction. However, it is not always available and the accuracy of diagnosis is dependent on an experienced sonographer.
Gastrointestinal tract infection
When patients with gastroenteritis present with acute abdominal pain, fever, vomiting, and nausea, they can easily be misdiagnosed as appendicitis. As such, acute gastroenteritis is the most common diagnosis in cases of missed appendicitis[11, 12]. In this situation, ultrasound can be a method to differentiate between these two etiologies of acute abdominal pain. However, ultrasound failed to detect hollow organ perforation in one of the study patients, whose plain abdomen showed free air.
Abdominal pain of unknown origin
Abdominal pain of unknown origin, or non-specific abdominal pain, is the most frequent diagnosis in children with abdominal pain in an emergency department in the study by Reynolds and Jaffe[13]. All of these patients had no specific abdominal sonographic findings and recovered or showed improvement after observation and supportive treatment.
Renal disease
Although fifteen patients with acute abdominal pain had hydronephrosis proven by sonography, it might be coincidental and in some patients who presented with abdominal pain it might be unrelated to hydronephrosis. Ultrasound examination could not detect renal inflammation without the presence of urinary obstruction, calculi, neoplasms, and other focal findings.
Intussusception
Intussusception is another important disease that warrants emergency treatment. When the so-called “target sign” or “pseudo-kidney sign” is present, intussusception is included in the differential diagnoses. Other bowel lesions, including primary and secondary carcinoma, lymphoma, Crohn's disease, inflammation secondary to pancreatitis, infarcted bowel, radiation ileitis, and hematoma should also be considered despite being very rare in children[14–16]. The sensitivity and specificity for diagnosing intussusception by sonography in the present study is 100% and 100%, respectively.
Gynecologic disease
The prevalence of gynecologic disease in children with acute abdominal pain is relatively rare. Most patients have ruptured ectopic pregnancy, ovarian cysts, or pelvic inflammation disease. In the present study, four patients had ovarian cysts and two had pelvic inflammatory disease. Sonography can be used to differentiate these two conditions: ovarian cysts demonstrate a large, complex, cystic mass with septations, while pelvic inflammatory disease has no specific sonographic findings although some may ultrasonographically present with thickening of the tubal wall, incomplete septa within the dilated tube, hyper-echoic mural nodules, free fluid cul-de-sac, hydrosalpinx, or tubo-ovarian abscess. The true value of sonography in acute abdominal pain lies in its ability to detect gynecologic disease and effectively rule out other causes that require surgical intervention.
GI anomalies
Gastrointestinal abnormalities include developmental obstructive defects of the duodenum and the small intestine, anomalies of rotation and fixation, intestinal duplications, and anomalies of the colon and rectum. In this study, there are two cases of GI anomalies. The sonographic findings showed a cystic mass in one patient and features of intestinal obstruction in the other, which were subsequently proven as duplication cyst and para-duodenal hernia by CT, respectively. Sonography is useful for evaluating many congenital gastrointestinal anomalies, especially hyper-trophic pyloric stenosis and mid-gut malrotation. However, there is no specific sonographic sign for duplication cysts except features of cystic mass, as well as no specific sonographic signs for internal hernia except features of intestinal obstruction. In other words, it may prove impossible to make a precise pre-operative diagnosis for duplication or internal hernia by sonography. Moreover, CT has assumed greater importance because it provides excellent anatomic details for correct diagnosis[17].
Extra-abdominal disease
Except for gastrointestinal, genitourinary, and gynecologic causes, some children with acute abdominal pain have extra-abdominal disease because referred pain results from shared central pathways for afferent neurons from different sites. A classic example is a patient with pneumonia who presents with abdominal pain because the T9 dermatome distribution is shared by the lungs and the abdomen[18]. However, patients with myocarditis may initially present with abdominal pain and vomiting[19]. Hsiao et al report that gastrointestinal symptoms are the most common presentation of myocarditis in children[20]. Thus, abdominal pain may be a manifestation of pneumonia, myocarditis, or other systemic diseases.
Disadvantage of ultrasound
The main disadvantage of ultrasound is the inability of the sound waves to penetrate bone and gas. In short, sonography has less role in patients with pneumoperitoneum while plain abdomen can detect free-air in patients with bowel perforation. The accuracy of ultrasound examination in upper abdominal pain is slightly less than 50% because of its limitations in diagnosing gastrointestinal problems, mild urinary tract infections, and some pathologies above the diaphragm[5–10, 13, 15]. In spite of this, ultrasound has become one of the investigations of choice in patients with upper abdominal pain, after history and clinical examination.
Limitations
This study has some limitations. The most important limitation is that the sonographic results were obtained by a retrospective review of the medical records. Some patients who presented with abdominal pain without undergoing sonography were not included. The small sample size of the study might have affected the sensitivity and specificity of ultrasound for diagnosing appendicitis and intussusception. Follow-up information was insufficient except for those admitted to the wards or those who come back to the out-patient department. Furthermore, the accuracy of diagnosis for pediatric abdominal pain by sonography depended on the performer's experience. Lastly, this study covered only the experience in one hospital. A prospective study in multiple medical centers for sonographic evaluation of abdominal pain in children is required.
Conclusion
Acute abdominal pain is a common complaint in children in the pediatric ED. Aside from history taking and detailed physical examination, sonography is a very effective, complementary, non-invasive method for evaluating children with acute abdominal pain, especially those with unexplained lower abdominal pain or those with suspected appendicitis or intussusception.
Acknowledgment
We gratefully acknowledge the permission for study from authors’ Institutional Review Board. There is no fund given by any agency for the research project.
Conflict of Interest
None.
References
- 1.Reynolds SL, Jaffe DM. Diagnosing abdominal pain in a pediatric emergency department. Pediatr Emerg Care. 1992;8(3):126–8. doi: 10.1097/00006565-199206000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Siegel MJ, Carel C, Surratt S. Ultrasonography of acute abdominal pain in children. JAMA. 1991;266(14):1987–9. [PubMed] [Google Scholar]
- 3.Mason JD. The evaluation of acute abdominal pain in children. Emerg Med Clin North Am. 1996;14(3):629–43. doi: 10.1016/s0733-8627(05)70271-6. [DOI] [PubMed] [Google Scholar]
- 4.Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158(2):355–60. doi: 10.1148/radiology.158.2.2934762. [DOI] [PubMed] [Google Scholar]
- 5.Parulekar SG. Ultrasonographic findings in diseases of the appendix. J Ultrasound Med. 1983;2(2):59–64. doi: 10.7863/jum.1983.2.2.59. [DOI] [PubMed] [Google Scholar]
- 6.Rubin SZ, Martin DJ. Ultrasonography in the management of possible appendicitis in childhood. J Pediatr Surg. 1990;25(7):737–40. doi: 10.1016/s0022-3468(05)80008-9. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Yousef MM, Bleichen JJ, Maher JW, et al. A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med. 1987;317(11):666–9. doi: 10.1056/NEJM198709103171103. [DOI] [PubMed] [Google Scholar]
- 8.Rious M. Sonographic detection of the normal and abnormal appendix. AJR Am J Roentgenol. 1992;158(4):773–8. doi: 10.2214/ajr.158.4.1546592. [DOI] [PubMed] [Google Scholar]
- 9.Siegel MJ, Carel C, Surratt S. Ultrasonography of acute abdominal pain in children. JAMA. 1991;266(14):1987–9. [PubMed] [Google Scholar]
- 10.Carrico CW, Fenton LZ, Taylor GA, et al. Impact of sonography on the diagnosis and treatment of acute lower abdominal pain in children and young adults. AJR Am J Roentgenol. 1999;172(2):513–6. doi: 10.2214/ajr.172.2.9930815. [DOI] [PubMed] [Google Scholar]
- 11.Humes DJ, Simpos J. Acute appendicitis. BMJ. 2006;333(7567):530–4. doi: 10.1136/bmj.38940.664363.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor GA, Callahan MJ, Rodriguez D, et al. Clinical guidelines, computed tomography scan, and negative appendectomies: a case series. Am J Emerg Med. 2006;24(1):68–72. doi: 10.1016/j.ajem.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds SL, Jaffe DM. Diagnosing abdominal pain in a pediatric emergency department. Pediatr Emerg Care. 1992;8(3):126–8. doi: 10.1097/00006565-199206000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Montali G, Groce F, DePra L, et al. Intussuception of the bowel: a new sonographic pattern. Br J Radiol. 1983;56(669):621–3. doi: 10.1259/0007-1285-56-669-621. [DOI] [PubMed] [Google Scholar]
- 15.Fleischer AC, Muhlataler CA, James AE. Sonographic assessment of the bowel wall. AJR Am J Roentgenol. 1981;136(5):887–91. doi: 10.2214/ajr.136.5.887. [DOI] [PubMed] [Google Scholar]
- 16.Morgan CL, Trought WS, Oddson TA, et al. Ultrasound patterns of disorders affecting the gastrointestinal tract. Radiology. 1980;135(1):129–35. doi: 10.1148/radiology.135.1.7360950. [DOI] [PubMed] [Google Scholar]
- 17.Gupta AK, Guglani B. Imaging of congenital anomalies of the gastrointestinal tract. Indian J Pediatr. 2005;72(5):403–14. doi: 10.1007/BF02731737. [DOI] [PubMed] [Google Scholar]
- 18.Ravichandran D, Burge DM. Pneumonia presenting with acute abdominal pain in children. Br J Surg. 1996;83(12):1707–8. doi: 10.1002/bjs.1800831214. [DOI] [PubMed] [Google Scholar]
- 19.Chang YJ, Chao HC, Hsia SH, et al. Myocarditis presenting as gastritis in children. Pediatr Emerg Care. 2006;22(6):439–40. doi: 10.1097/01.pec.0000221346.64991.e7. [DOI] [PubMed] [Google Scholar]
- 20.Hsiao HJ, Hsia SH, Wu CT. Clinical presentation of pediatric myocarditis in Taiwan. Pediatr Neonatol. 2011;52(3):135–9. doi: 10.1016/j.pedneo.2011.03.005. [DOI] [PubMed] [Google Scholar]