Abstract
Spontaneous regression in melanomas is not an uncommon phenomenon, as it has been described in 10–35% of primary cutaneous lesions [1]. Regression does not appear to predict a more favorable course, since even fully regressed melanomas may progress into metastatic disease [2]. Several dermoscopic features have been correlated with the regression process, including white scar-like depigmented areas and gray-blue, pepper-like granules, which correspond to dermal scarring, pigment incontinence and presence of melanophages [3,4]. Regression may occur not only in melanomas, but also in melanocytic nevi, which similarly may exhibit white areas and gray-blue granules or areas under dermoscopy [5]. Overall, white areas have been proposed to be associated with the fibrosis type of regression and gray-blue areas to the melanosis type of regression of melanocytic tumors [3]. Lichen planus like keratosis (LPLK) is considered to represent a regressed solar lentigo or seborrheic keratosis. Dermoscopy of LPLK at the late stage of the regression process reveals a diffuse gray-blue granular pattern, similar to that observed in regressed melanocytic lesions [6].
In this context, when evaluating skin lesions that exhibit high degree of regression, interpretation of dermoscopic findings may be problematic, especially when no other dermoscopic clues can be recognized.
Keywords: pigmented lesion, regression, melanoma, lichen planus-like keratosis
Case presentation
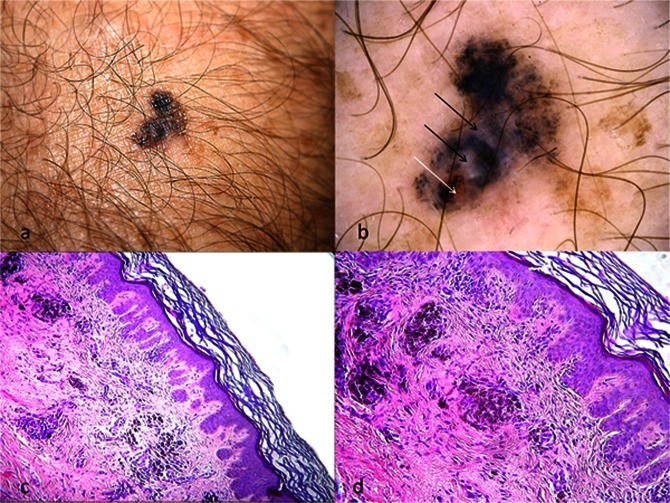
The fully regressed melanoma in Figure 1 was found on the arm of a 50-year-old man, who was recently diagnosed with metastatic melanoma of the ipsilateral axillary lymph nodes (Figure 1A). Dermoscopic examination revealed a diffuse blue-gray granular pattern, scar-like, depigmented areas, and a roundish ulceration in the absence of any specific features of melanoma (Figure 1B). Histopathologic examination showed hyperplasia of the epidermis, prominent scar-like fibrosis of the dermis (corresponding dermoscopically to scar-like depigmented areas), vascular hyperplasia, moderately dense inflammation, pigment incontinence and accumulation of melanophages (observed as blue-gray granularity under dermoscopy) (Figures 1C,D). The latter resulted in a fuzzy appearance of the dermis, obstructing the recognition of residual melanocytes, which were finally highlighted by immunohistochemistry, as slight positivity in S100 and HMB45 stains.
Figure 1.
(A) Clinical image showing a suspicious pigmented lesion on the arm of a 50-year-old man, who was recently diagnosed with metastatic melanoma of the ipsilateral axillary lymph nodes. (B) Diffuse granular pattern in the absence of melanoma-specific criteria in dermoscopy. Scar-like depigmented areas (black arrows) and a roundish ulceration (white arrow) can also be identified. (C, D) Histopathologic images showing prominent dermal fibrosis, increased vascularity and accumulation of melanophages (hematoxylin & eosin [H&E] ×10 magnification (C), H&E ×20 magnification (D)). [Copyright: ©2012 Lallas et al.]
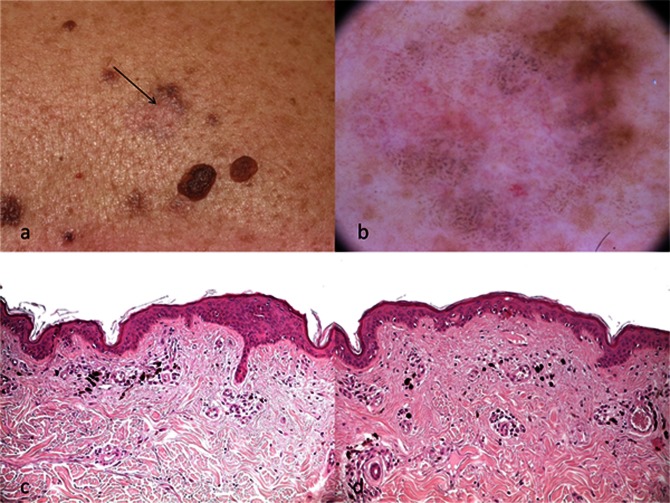
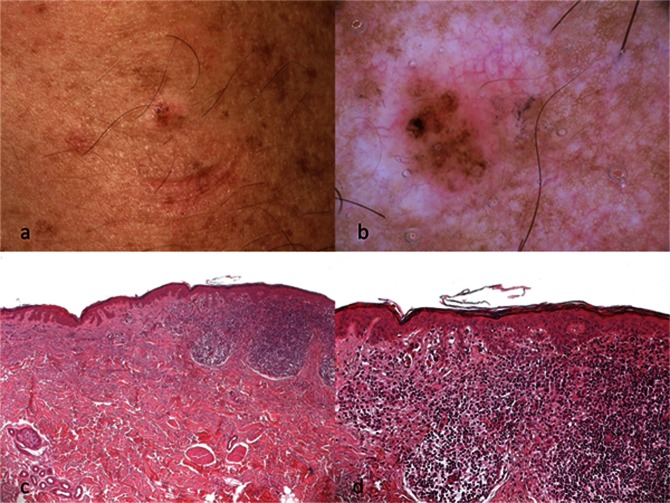
In addition, we present a melanocytic nevus (Figure 2) and a LPLK (Figure 3), both typified by features of diffuse regression, namely blue-gray granules and whitish areas. Similar to the melanoma case, no other dermoscopic clues allowing a confident diagnosis could be identified. Histopathologic features of the nevus were very similar to those observed in the melanoma case, including prominent fibrosis, mild inflammation, telangiectasias and scattered melanophages (Figures 2C,D). On the other hand, the LPLK was histopathologically characterized by mild acanthosis, a band-like lymphocytic infiltrate, focal vacuolar degeneration of the basal cell layer, dermal fibrosis, and abundant melanophages in the upper dermis (Figure 3C,D).
Figure 2.
(A) Clinical image showing a fully regressed melanocytic nevus (arrow). (B) Dermoscopy reveals diffuse blue-gray granules, white areas and some telangiectatic vessels. Remnants of pigmented network can be observed at the upper right part of the lesion. (C, D) Scattered melanophages, prominent fibrosis and telangiectasias can be seen on histopathology, corresponding to the above-mentioned dermoscopic features (H&E ×20 magnification). [Copyright: ©2012 Lallas et al.]
Figure 3:
(A, B) Clinical and dermoscopic aspect of a lichen planus-like keratosis exhibiting blue-gray granules, white areas and telangiectasias. No areas reminiscent of a solar lentigo or a seborrheic keratosis could be observed. (C, D) Histopathologically, the lesion is characterized by a band-like lymphocytic infiltrate, dermal fibrosis and abundant melanophages in the upper dermis (H&E ×10 magnification (C), H&E ×20 magnification (D)). [Copyright: ©2012 Lallas et al.]
Conclusions
Zalaudek et al proposed that the management of melanocytic lesions exhibiting dermoscopic features of regression may be facilitated by the use of an algorithm based on the degree and combination of regression features [3]. In particular, the authors suggest that risk of melanoma is higher for lesions showing either moderate or high degree of regression features along with the presence of combined blue and white areas.
The dermoscopic diagnosis of a LPLK may be assisted by the identification of areas reminiscent of a solar lentigo or a seborrheic keratosis within the lesion [7]. However, at the end-stage of the regression process, when such features have disappeared and the lesion is characterized only by the presence of blue-gray granules, LPLK may strikingly mimic regressive melanoma [6].
In the three lesions reported here, the presence of prominent regression features did not allow a confident differential diagnosis. Under this scenario, an otherwise benign lesion, as a melanocytic nevus, or even a LPLK, may be virtually indistinguishable on clinical and dermoscopic examination from a melanoma and vice versa. In such cases, even histopathologic examination may fail to establish a definite diagnosis. Thus, in lesions exhibiting high degree of regression under dermoscopy, complete excision and careful clinicopathologic evaluation is mandatory to reach a reliable final diagnosis.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
References
- 1.Blessing K, McLaren KM. Histological regression in primary cutaneous melanoma: recognition, prevalence and significance. Histopathology. 1992;20(4):315–22. doi: 10.1111/j.1365-2559.1992.tb00988.x. [DOI] [PubMed] [Google Scholar]
- 2.Bories N, Dalle S, Debarbieux S, Balme B, Ronger-Savié S, Thomas L. Dermoscopy of fully regressed cutaneous melanoma. Br J Dermatol. 2008;158(6):1224–9. doi: 10.1111/j.1365-2133.2008.08501.x. [DOI] [PubMed] [Google Scholar]
- 3.Zalaudek I, Argenziano G, Ferrara G, et al. Clinically equivocal melanocytic skin lesions with features of regression: a dermoscopic-pathological study. Br J Dermatol. 2004;150(1):64–71. doi: 10.1111/j.1365-2133.2004.05657.x. [DOI] [PubMed] [Google Scholar]
- 4.Massi D, De Giorgi V, Carli P, Santucci M. Diagnostic significance of the blue hue in dermoscopy of melanocytic lesions: a dermoscopic–pathologic study. Am J Dermatopathol. 2001;23(5):463–9. doi: 10.1097/00000372-200110000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Menzies SW, Gutenev A, Avramidis M, Baltrac A, McCarthy WH. Short-term digital surface microscopic monitoring of atypical or changing melanocytic lesions. Arch Dermatol. 2001;137(12):1583–9. doi: 10.1001/archderm.137.12.1583. [DOI] [PubMed] [Google Scholar]
- 6.Raptoulis G, Spencer R, Einstein B, Oliviero M, Braun R, Rabinovitz H. Lichen planus-like keratosis of the face: a simulator of melanoma in situ. Dermatol Surg. 2007;33(7):854–6. doi: 10.1111/j.1524-4725.2007.33183.x. [DOI] [PubMed] [Google Scholar]
- 7.Oliviero M, Rabinovitz H. Lichen planus-like keratosis. In: Malvehy J, Puig S, editors. Principles of Dermoscopy. Barcelona, Spain: 2002. pp. 145–54. Self-Published. [Google Scholar]