Introduction
Because of their similar appearance to melanoma, recurrent and persistent nevi may pose diagnostic difficulties. We present three cases of recurrent nevi and their clinical, dermatoscopic and dermatopathologic findings.
Case 1
A 40-year-old patient presented with a papule on the calf with irregular brown pigmentation (Figure 1). On dermatoscopy the lesion was composed of segmental radial lines and structureless zones. Discrete reticular lines were also seen but they were also present in the surrounding normal skin. The pigmentation did not extend towards the edge of the visible scar. Disregarding the clinical history of a previous surgery of a nevus the differential diagnosis based solely on the dermatoscopic presentation includes recurrent melanoma, basal cell carcinoma and recurrent nevus. Histopathologically one can spot inconspicuous dermal nests of melanocytes on site and heavily pigmented melanocytes at the dermoepidermal junction on the other. The epidermal melanocytes are arranged as single cells of which some can be found in higher levels of the epidermis including the stratum corneum, resembling melanoma in situ. The fact that this area is present above a scar of an otherwise inconspicuous “superficial and deep” congenital nevus, as well as the patient history of a previous shave biopsy, led to the diagnosis of a recurrent nevus.
Figure 1.
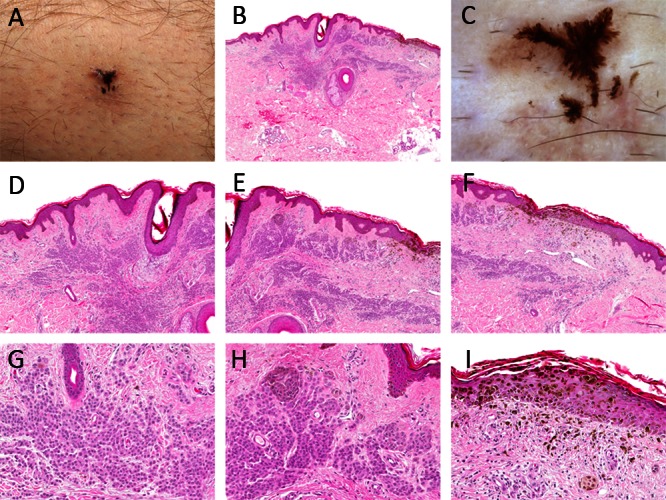
(A & C) Clinical and dermatoscopic picture of an asymmetrically pigmented lesion on the calf. The pigmentation does not extend beyond the area of the visible scar; dermatoscopically one can see segmental radial lines radial and structureless areas. (B & D–H) Dermatopathologic images of the lesion shown in A & C. The lesion is composed of inconspicuous dermal nests of melanocytes and heavily pigmented melanocytes at the dermoepidermal junction overlying scar tissue. [Copyright: ©2013 Tschandl.]
Case 2
A 23-year-old woman presented with a brown macule on the chest (Figure 2). Dermatoscopically there are segmental radial lines, brown clods and structureless zones. The pigmented structures correspond to junctional nests of melanocytes. The scar is visible dermatoscopically at the periphery of the lesion. The pigmentation is not present beyond the scar. The histopathologic findings of unsuspicious nests of melanocytes beneath a scar and junctional nests confined to the area above the scar are in keeping with the presence of a recurrent nevus.
Figure 2.
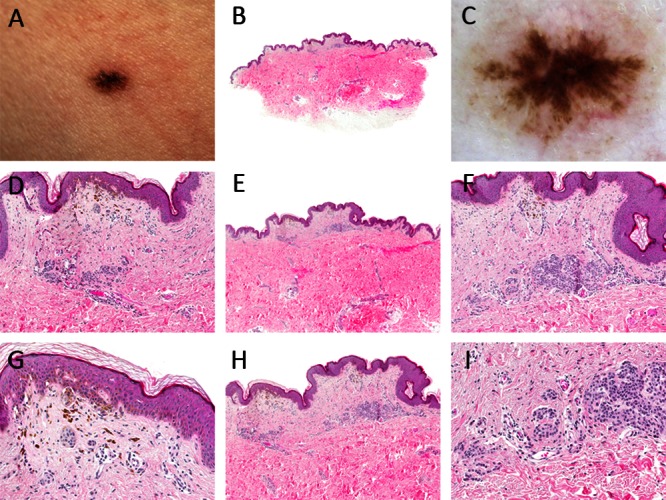
(A & C) Clinical and dermatoscopic picture of a brown macule on the chest. Dermatoscopically radial lines and brown clods are confined to the evident scar. (B & D–H) Dermatopathologic images of the lesion shown in A&C. Nests of melanocytes can be seen in the epidermis as well as beneath a dermal scar. [Copyright: ©2013 Tschandl.]
Case 3
The third case is a 22-year-old patient with a brown papule on the back (Figure 3). The most prominent dermatoscopic findings are a pattern of segmental radial lines and a hypopigmented structureless zone (scar). The dermatopathologic image is dominated by heavily pigmented melanophages on one hand and melanocytes at the dermoepidermal junction arranged as single cells and in nests, which are partly confluent. Small nests of monomorphic melanocytes can be spotted beneath the scar.
Figure 3.
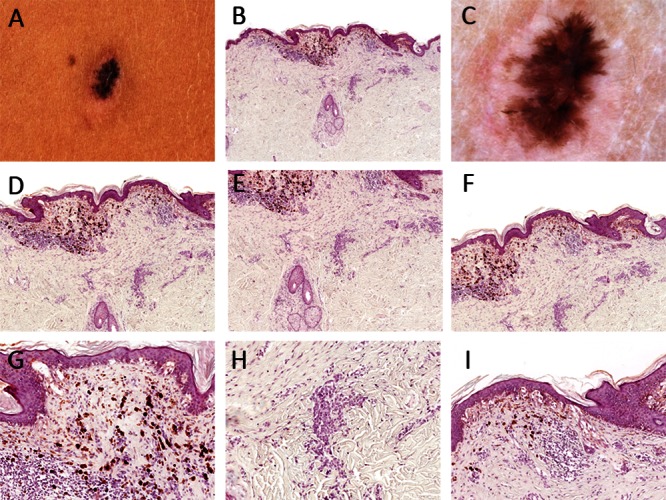
(A & C) Clinical and dermatoscopic picture of a brown papule on the back. Dermatoscopically one can see segmental radial lines within a hypopigmented structureless area (scar). (B & D–H) Dermatopathologic images of the lesion shown in A & C. Melanocytes in the epidermis are arranged as single cells and in confluent nests. Inconspicuous nests of small melanocytes arranged in an adnexocentric fashion can be spotted in the dermis. [Copyright: ©2013 Tschandl.]
Discussion
Recurrent nevi emerge after inadequate or insufficient (superficial shave or partial excision or laser removal [1]) removal of a nevus. The persistent part of the nevus is located in the deeper parts of the dermis and gives rise to the recurrence that is visible clinically and dermatoscopically. Recurrent nevi are usually “superficial and deep congenital nevi,” in rare cases Spitz nevi [2] or Blue nevi [3,4]. Clark nevi or Reed nevi usually do not persist and recur because they do not involve the reticular dermis. In sum, recurrence rates of excised nevi are low, one prospective study found only 3.4% recurrences [5].
Recurrent nevi may resemble melanoma clinically [6], dermatoscopically [7,8], and Histopathologically [9–12]. This problem has been known for many decades [6,13] and the following criteria were established to differentiate recurrent nevi from melanoma:
Presence of a scar. This is evidence of a prior removal and can be seen clinically, dermatoscopically and histologically. In the view of the author though, this feature is not helpful in differentiating recurrent melanoma from recurrent nevi.
Report of a prior excision. Most of the times a histologic diagnosis is available reporting an inconspicuous nevus. If such a report is present this information should always be handed over to the reporting dermatopathologist.
Presence of the prior nevus. This feature is mostly helpful for the dermatopathologist, as sometimes inconspicuous nests of melanocytes are visible below the recurrent nevus.
Monomorphous cytology of melanocytes that constitute the nevus.
Melanocytes in the epidermis are confined to the area of the scar and don’t expand beyond [14].
Melanocytes of nevi become smaller towards descent into the dermis, have a lower proliferation rate, and show less expression of gp100 and tyrosinase with increasing depth [15].
Although recurrent nevi may resemble melanoma clinically and dermatoscopically most lesions can be easily diagnosed by dermatopathology, problematic lesions are rare. In doubtful cases it is mandatory to retrieve the histopathologic slides of the prior excision. However it would be of great practical value to diagnose recurrent nevi with non-invasive techniques. One prospective study [11] focused on the histopathologic correlates of melanotic pigmentation in scars after removal of melanocytic lesions but it remained unclear whether dermatoscopy is helpful in distinguishing recurrent nevi from recurrent melanomas.
Segmental radial lines are present in all three cases of recurrent nevi presented in this series. The possible diagnoses of lesions with a pattern of segmental radial lines are primary melanoma, basal cell carcinoma and recurrent nevi. Usually these three diagnoses can be differentiated easily based on additional clues and the clinical context. It is interesting that recurrent melanoma (in contrast to primary melanoma) is usually not characterized by segmental radial lines.
Using confocal microscopy Longo et al. [14] demonstrated that in recurrent nevi the pigmentation remained within the boundaries of the scar. This finding might be an important clue to differentiate recurrent melanoma form recurrent nevi but additional studies are needed to confirm this observation.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
References
- 1.Al-Hadithy N, Al-Nakib K, Quaba A. Outcomes of 52 patients with congenital melanocytic naevi treated with UltraPulse Carbon Dioxide and Frequency Doubled Q-Switched Nd-Yag laser. J Plast Reconstr Aesthet Surg. 2012;65(8):1019–28. doi: 10.1016/j.bjps.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Harvell JD, Bastian BC, LeBoit PE. Persistent (recurrent) Spitz nevi: a histopathologic, immunohistochemical, and molecular pathologic study of 22 cases. Am J Surg Pathol. 2002;26:654–61. doi: 10.1097/00000478-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Muñoz C, Quintero A, Sánchez JL, Ruiz-Santiago H. Persistent blue nevus simulating melanoma. J Am Acad Dermatol. 2004;50:S118–20. doi: 10.1016/j.jaad.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 4.Harvell JD, White WL. Persistent and recurrent blue nevi. Am J Dermatopathol. 1999;21(6):506–17. doi: 10.1097/00000372-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Goodson AG, Florell SR, Boucher KM, Grossman D. Low rates of clinical recurrence after biopsy of benign to moderately dysplastic melanocytic nevi. J Am Acad Dermatol. 2010;62(4):591–6. doi: 10.1016/j.jaad.2009.06.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kornberg R, Ackerman AB. Pseudomelanoma: recurrent melanocytic nevus following partial surgical removal. Arch Dermatol. 1975;111(12):1588–90. doi: 10.1001/archderm.111.12.1588. [DOI] [PubMed] [Google Scholar]
- 7.Yoshida Y, Yamada N, Adachi K, Tanaka M, Yamamoto O. Traumatized recurrent melanocytic naevus with typical starburst pattern on dermoscopy. Acta Derm Venereol. 2008;88(4):408–9. doi: 10.2340/00015555-0468. [DOI] [PubMed] [Google Scholar]
- 8.Marghoob AA, Kopf AW. Persistent nevus: an exception to the ABCD rule of dermoscopy. J Am Acad Dermatol. 1997;36:474–5. doi: 10.1016/s0190-9622(97)80230-7. [DOI] [PubMed] [Google Scholar]
- 9.King R, Hayzen BA, Page RN, Googe PB, Zeagler D, Mihm MC., Jr Recurrent nevus phenomenon: a clinicopathologic study of 357 cases and histologic comparison with melanoma with regression. Mod Pathol. 2009;22(5):611–7. doi: 10.1038/modpathol.2009.22. [DOI] [PubMed] [Google Scholar]
- 10.Sommer LL, Barcia SM, Clarke LE, Helm KF. Persistent mela-nocytic nevi: a review and analysis of 205 cases. J Cutan Pathol. 2011;38(6):503–7. doi: 10.1111/j.1600-0560.2011.01692.x. [DOI] [PubMed] [Google Scholar]
- 11.Botella-Estrada R, Nagore E, Sopena J, et al. Clinical, dermoscopy and histological correlation study of melanotic pigmentations in excision scars of melanocytic tumours. Br J Dermatol. 2006;154(3):478–84. doi: 10.1111/j.1365-2133.2005.07105.x. [DOI] [PubMed] [Google Scholar]
- 12.LeBoit PE. Persistent nevus, with “no” previous biopsy. Am J Dermatopathol. 2004;26(4):347–8. doi: 10.1097/00000372-200408000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Park HK, Leonard DD, Arrington JH, 3rd, Lund HZ. Recurrent melanocytic nevi: clinical and histologic review of 175 cases. J Am Acad Dermatol. 1987;17:285–92. doi: 10.1016/s0190-9622(87)70204-7. [DOI] [PubMed] [Google Scholar]
- 14.Longo C, Moscarella E, Pepe P, et al. Confocal microscopy of recurrent naevi and recurrent melanomas: a retrospective morphological study. Br J Dermatol. 2011;165(1):61–8. doi: 10.1111/j.1365-2133.2011.10310.x. [DOI] [PubMed] [Google Scholar]
- 15.Hoang MP, Prieto VG, Burchette JL, Shea CR. Recurrent melanocytic nevus: a histologic and immunohistochemical evaluation. J Cutan Pathol. 2001;28(8):400–6. doi: 10.1034/j.1600-0560.2001.028008400.x. [DOI] [PubMed] [Google Scholar]


