Abstract
Background:
Eccrine poroma is a benign neoplasm that can mimick a malignant neoplasm dermoscopically. The characteristic vascular pattern of this tumor has not been established.
Objective:
To evaluate dermoscopic features of non-pigmented eccrine poroma in Mexican patients.
Method:
We retrospectively studied histologically proven cases of eccrine poroma from three Mexican hospitals analyzed by four dermoscopists.
Results:
Thirteen cases were studied. A polymorphous vascular pattern was found in most cases. Four presented with irregular linear and branched vessels with semi-elliptical, or semicircular endings (“chalice-form” and “cherry-blossoms” vessels). Structureless pink-white areas were the most common other dermoscopic finding.
Conclusions:
“Chalice-form” and “cherry-blossom” vessels have not been reported in other benign or malignant neoplasms and can be a useful clue to the diagnosis of non-pigmented eccrine poroma. Due to the variability of dermoscopic patterns of eccrine poroma further studies are required to establish the specificity of our findings.
Keywords: dermoscopy, eccrine poroma, polymorphous vascular pattern
Background
Eccrine poroma (EP) is a relatively common benign adnexal neoplasm that is of eccrine origin. EP commonly occurs on the soles and lateral aspects of the feet, but it can also be found on other anatomic sites. It appears more frequently in adults. The most common clinical presentation is a firm nodule, from pink to red in color, sometimes slightly pedunculated, measuring up to 2 cm in diameter. Sometimes EP presents as a small papule or as a verrucous plaque. Occasionally EP can be pigmented. Usually it is a solitary tumor. When multiple lesions appear on palms and soles the condition has been termed eccrine poromatosis [1,2].
Dermatopathologically it is a proliferation arising from the lower portion of the epidermis from where it extends into the dermis forming a mass or broad anastomosing bands, composed of epithelial cells with uniform cuboidal appearance with round basophilic nuclei, connected by intercellular bridges. In the majority of cases, small ducts and occasionally cystic spaces are found within the aggregations of tumor cells [3].
Dermoscopy is a non-invasive technique that is useful for the diagnosis of benign and malignant melanocytic and non-melanocytic lesions. In general the presence of a polymorphous vascular pattern is considered to be a useful clue to differentiate between benign and malignant neoplasms. Vascular patterns, including morphology and distribution of vessels, can be useful to make a specific diagnosis, especially in combination with other structures. However, only a few articles describe the dermoscopic features of non-pigmented EP [4–7]. Since the number of published articles is small, specific clues or patterns of non-pigmented EP have not been established.
The aim of this study was to evaluate dermoscopic features of non-pigmented EP in Mexican patients and to compare our findings with those already published.
Material and methods
This is a retrospective study, including histologically verified cases of non-pigmented EP examined by dermoscopy, in three different Mexican hospitals with polarized and nonpolarized dermoscopy (DermLite pro HR and DermLite Hybrid M; 3 Gen, Dana Point, CA, USA). The photographs were taken with a Nikon Coolpix P5100. All cases were analyzed with polarized light with and without immersion; for contact dermoscopy we used common cleansing gel alcohol. All cases were photographed with and without immersion with minimum pressure on the tumor.
Each dermoscopic image was evaluated independently by four dermoscopists for the presence of vascular pattern and additional clues.
Results
We included 13 cases of 6 women and 7 men. The mean age was 53 years (range 35—82). All patients were Mexican with Fitzpatrick’s phototype skin III and IV. None of them had medical histories of importance for the present illness. Only two patients reported pruritus and two reported pain during walking. Eight cases were located on the feet. The remaining cases were located on the arm, thigh, abdomen, back and lateral aspect of the trunk.
Clinically the lesions presented as pink-to-red nodules, as nodules with a keratotic plug, and as a warty, papillated plaque. The average diameter was of 12 mm (range 5–20 mm). The lesions developed to their current size within 1 to 15 years. The clinical differential diagnoses included keratoacanthoma, clear cell acanthoma, larva migrans, amelanotic melanoma and squamous cell carcinoma.
The dermoscopic features are presented in Table 1. We found no differences with regard to dermoscopic structures seen with polarized light with immersion and polarized light without immersion. Nine cases (70%) showed a polymorphous vascular pattern, including at least two types of vascular structures; four of them (30%) showed irregular linear vessels with a semi-elliptical ending giving the appearance of a chalice (“chalice-form”). In addition to “the chalice-form” vessels, three cases (23%) also showed structures combining thin branching vessels with circular and semicircular tips, very similar to the structure of the cherry blossom tree; and, in addition, one of these displayed a small ulceration (Figures 1, 2, 3). One more case showed “cherry-blossom” vessels in the center of the lesion and milky-red globule/lacuna-like areas surrounded by pink-to-white halo (“frog-egg” aggregations) in the periphery. Four more cases (in total 38%) show these “frog-egg” aggregations (Figure 4) and the rest of the cases combined linear irregular, hairpin vessels in addition to milky–red globules-like areas. In nine cases (70%) a structureless pink-to-white area was found, the most frequently found non-vascular structure.
TABLE 1.
Dermoscopic structures
| Patient | Sex/Age | Anatomic site | Hair pin vessels | Linear irregular vessels | Chalice-form/cherry blossoms | Structureless pink-white areas | Milky-red/lacu na-like areas | Ulceration | Glomerular vessels |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/63 | thigh | - | - | +/+ | − | − | + | − |
| 2 | F/82 | upper arm | + | − | +/− | + | + | − | − |
| 3 | M/49 | foot | − | − | +/+ | + | − | − | − |
| 4 | M/44 | back | − | − | − | + | + | − | − |
| 5 | F/35 | foot | + | + | − | + | − | − | − |
| 6 | M/41 | foot | + | − | +/+ | + | − | + | − |
| 7 | M/36 | foot | + | − | − | + | +* | − | + |
| 8 | M/78 | abdomen | − | − | − | + | + | − | − |
| 9 | F/46 | foot | − | + | − | + | + | + | − |
| 10 | M/63 | foot | − | − | −/+ | − | +* | − | + |
| 11 | M/57 | foot | − | − | − | − | +* | − | − |
| 12 | F/48 | foot | − | − | − | − | +* | − | − |
| 13 | F/46 | trunk | + | + | − | + | +* | − | − |
| Number | 5 | 3 | 4/4 | 9 | 9 | 3 | 2 | ||
| Percentage | 38% | 23% | 30% | 70% | 70% | 23% | 15% | ||
“frog-egg appearance” (38%)
Figure 1.
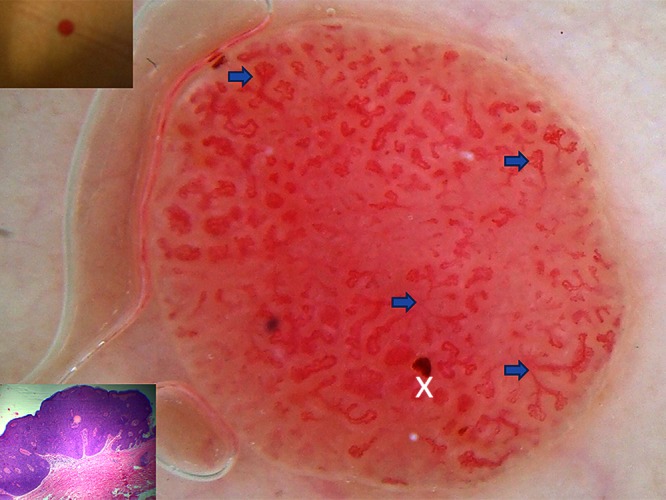
Case 1. Immersion polarized dermoscopy shows the chalice-form and cherry blossom vessels (arrows) and small ulceration (cross). [Copyright: ©2013 Domínguez Espinosa et al.]
Figure 2.
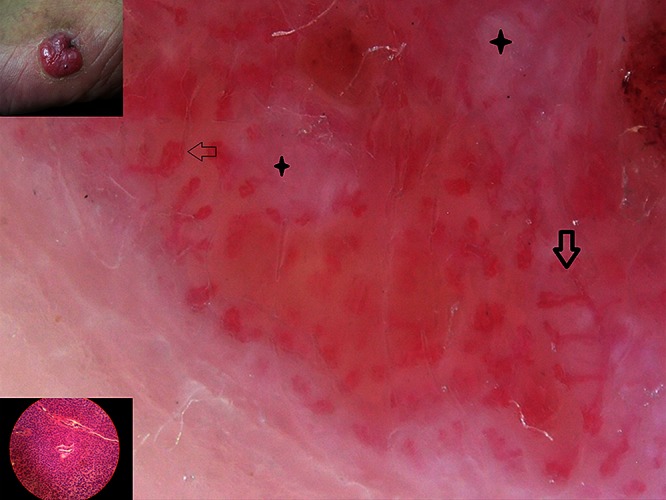
Case 3. Polarized dermoscopy without immersion showing cherry-blossom, chalice-form vessels (arrows), and structureless pink-white areas (cross). [Copyright: ©2013 Domínguez Espinosa et al.]
Figure 3.
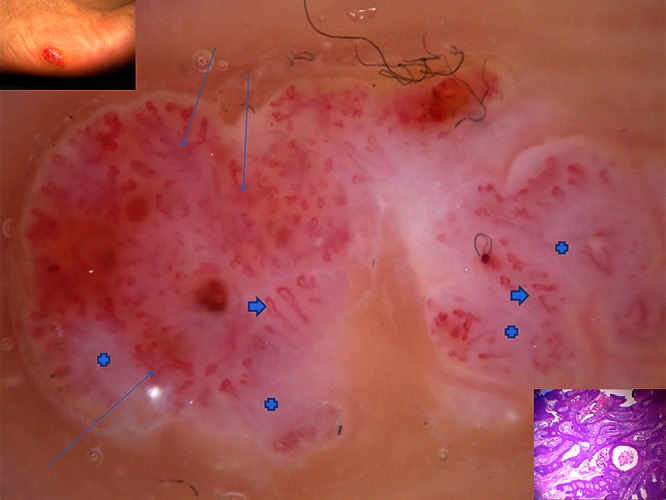
Case 6. Immersion polarized dermoscopy. Cherry-blossom, chalice-form (thin arrows) hairpin vessels (thick arrows), structureless pink-to-white areas (cross). [Copyright: ©2013 Domínguez Espinosa et al.]
Figure 4.
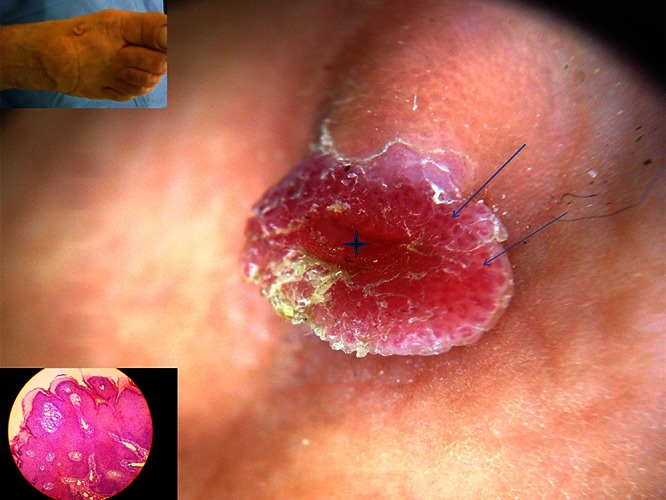
Case 11. Polarized dermoscopy without immersion. Frog-egg aggregations (arrows) and central lacuna-like area (cross). [Copyright: ©2013 Domínguez Espinosa et al.]
The dermatopathologic findings were typical for eccrine poroma. All lesions were formed of cuboidal basophilic cells arranged in anastomosing broad bands with small ductal spaces in contact with the epidermis and extending onto the dermis. Some cases show pseudocystic spaces with mucous stroma. The capillaries were dilated and filled with erythrocytes. Since all the samples were cut vertically, we could not carry out any other histological analysis of the vascular morphology.
Discussion
Eccrine poroma can mimic malignant tumors, including amelanotic melanoma, which emphasizes the importance of characterizing the dermoscopic patterns of non-melanocytic lesions.
Altamura et al were the first to publish dermoscopic characteristics of a case of non-pigmented EP. Since then 22 additional cases have been reported. All reported cases had a polymorphous vascular pattern [4,6–9]. This pattern is characterized by the presence of irregular vessels that vary in size and shape and by the combination of different types of vessels. The vascular pattern of cases reported by Aydingoz [8] was described as “floral and leaf-like.” We propose to call these vessels “chalice-form” and “cherry-blossom vessels” because of their similarity with a chalice and because the branches resemble the flowers of cherry trees. We consider these terms easy to remember. These vascular patterns seem to combine hairpin and branched vessels and have not been reported as part of the vascular pattern of melanoma or other malignant tumors [5,10]. Therefore, the presence of this vascular pattern could be a helpful clue in differentiating EP from other benign or malignant non-pigmented neoplasms. However, given the small number of cases in our study, it would be premature to consider these vessels specific for eccrine poroma.
Although in other studies glomerular, arborizing and linear irregular vessels were dominant, we barely found them in our series. Structureless pink-to-white areas, a dominant characteristic of non-pigmented EP in of our series, were also found in most cases in the study of Ferrari et al [6]. The well-circumscribed milky-red lacunas separated by white-pink bands, the “frog-egg” appearance, which were seen in five (38%) of our patients, were also found in 90% of cases studied by Minagawa et al [9].
Conclusion
The “chalice-form” and “cherry-blossom” vessels are a good clue for the diagnosis of non-pigmented EP, although, for unknown reasons, the pattern of non-pigmented EP is not uniform, and further studies are required to establish the specificity of our findings.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Taylor S, Perone J, Kaddu S. Appendage tumors and hamartomas of the skin. In: Wolff K, editor. Fitzpatrick’s Dermatology in General Medicine. 7th ed. USA: McGraw Hill; 2008. pp. 1069–87. [Google Scholar]
- 2.Calonje E. Tumours of the skin appendages. In: Burns T, editor. Rook’s Textbook of Dermatology. 8th ed. Oxford, UK: Wiley-Blackwell; 2010. pp. 53.1–53.44. [Google Scholar]
- 3.Elder D, Elenitsas R, Bernett J, et al. Tumors with eccrine differentiation. In: Elder D, editor. Lever’s Histopathology of the Skin. 9th ed. Philadelphia, USA: Lippincot Williams & Wilkins; 2005. pp. 898–910. [Google Scholar]
- 4.Avilés-Izquierdo JA, Velázquez-Tarjuelo D, Lecona-Echevarria M, Lázaro-Ochaita P. [Dermoscopic features of eccrine poroma.] Article in Spanish. Actas Dermosifilogr. 2009;100(2):133–6. [PubMed] [Google Scholar]
- 5.Blum A, Metzler G, Juergen B. Polymorphous vascular patterns in dermoscopy as a sign of malignant skin tumors. A case of an amelanotic melanoma and a porocarcinoma. Dermatology. 2005;210(1):58–9. doi: 10.1159/000081486. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari A, Buccini P, Silipo V, et al. Eccrine poroma: a clinical-dermoscopic study of seven cases. Acta Derm Venereol. 2009;89(2):160–4. doi: 10.2340/00015555-0608. [DOI] [PubMed] [Google Scholar]
- 7.Nicolino R, Zalaudek I, Ferrara G, et al. Dermoscopy of eccrine poroma. Dermatology. 2007;215(2):160–3. doi: 10.1159/000104270. [DOI] [PubMed] [Google Scholar]
- 8.Aydingoz IE. New dermoscopic vascular patterns in a case of eccine poroma. J Eur Acad Dermatol Venereol. 2009;23(6):725–6. doi: 10.1111/j.1468-3083.2009.03182.x. [DOI] [PubMed] [Google Scholar]
- 9.Minagawa A, Koga H, Takahashi M, Sano K, Okuyama R. Dermoscopic features of nonpigmented eccrine poromas in association with their histopathological features. Br J Dermatol. 2010;163(6):1264–68. doi: 10.1111/j.1365-2133.2010.10017.x. [DOI] [PubMed] [Google Scholar]
- 10.Suzaki R, Shioda T, Konohana I, Ishizaki S, Sawada M, Tanaka M. Dermoscopic features of eccrine porocarcinoma arising from hidroacanthoma simplex. Dermatol Res Pract. 2010:192371. doi: 10.1155/2010/192371. [DOI] [PMC free article] [PubMed] [Google Scholar]


