Abstract
We present a case of an early invasive melanoma (Breslow thickness 0.25 mm), 1.6 mm in diameter on the arm of a 38-year-old woman. She was under surveillance due to having multiple (>100) nevi, and the melanoma was assessed as a new lesion by the examining doctor. Clinically the lesion was hyper-pigmented compared with surrounding nevi and dermatoscopically it had a clue of pseudopods/lines radial, but they were arranged in an arguably symmetrical circumferential pattern around a structureless blue-gray center. Generally melanomas are expected to be dermatoscopically asymmetrical, but we believe that this case illustrates the fact that small melanomas may be recognized by clues such as pseudopods/lines radial and dermatoscopic gray even when they have not yet developed unequivocal asymmetry.
Keywords: melanoma, small melanoma, dermatoscopy, dermoscopy, dermatopathology
Introduction
The diagnosis of melanomas smaller than 4 mm presents difficulties because the clinical and dermatoscopic features of small melanomas have been reported infrequently.
Case report
A 38-year-old Australian-born woman of Italian descent, with Fitzpatrick type 4 skin, presented for a routine yearly skin examination. She was examined with a Heine Delta 20 dermatoscope (Heine, Optotechnic GmbH, Herrsching, Germany) and had been having total body photography with a Molemax Dermdoc video monitoring system (Derma Medical Systems, Austria). In previous years some pigmented lesions (PSLs) had been observed to change with symmetrical growth of peripheral clods. These were deemed to be maturing nevi and had not been excised. One pigmented skin lesion had been excised in 2007 and was reported by the pathologist to be an irritated dysplastic nevus.
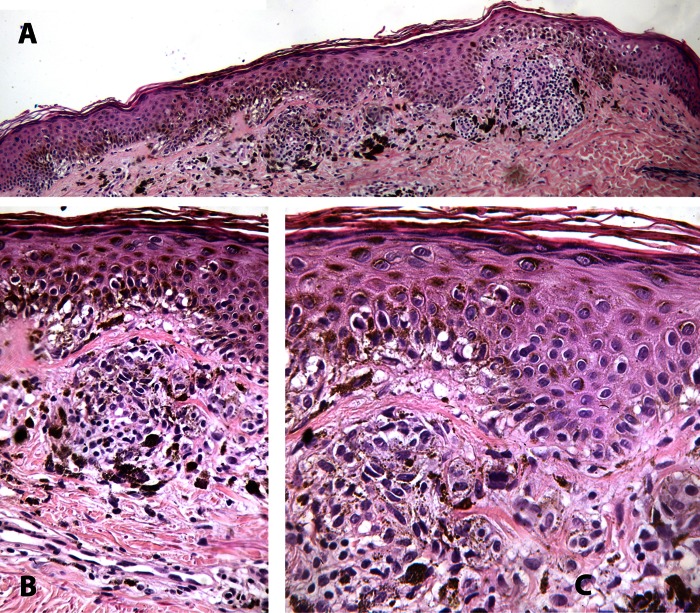
At this visit in May 2012, a new lesion was detected on the left arm (Figure 1A). Clinically it was noted to be darker than surrounding PSLs and dermatoscopically pseudopods and radial lines were arranged circumferentially around a structureless blue-gray center (Figure 1B); the radial lines were arguably symmetrically distributed, appearing in all quadrants of the perimeter while being less clearly defined and sparser in one quadrant. This lesion was new at mature age (evolving), which raised suspicion for malignancy despite the lesion’s small size and equivocal symmetry [1]. The lesion was subjected to excision biopsy and dermatopathologic assessment (Figure 2 composite) showed a small, but asymmetric, nested and single cell proliferation of atypical melanocytes along the dermoepidermal junction with scattered single cell intraepithelial upward spread. There was limited extension into the papillary dermis to a depth of 0.25 mm. Superficial dermal melanosis and inflammation were present along with mild fibroplasia, suggesting a component of regression to a depth of 0.35 mm. In spite of the dermatoscopic appearance of lines radial circumferential, there were no spitzoid features dermatopathologically. The diagnosis of early level 2 malignant melanoma of superficial spreading type was rendered. Physical examination revealed no evidence of lymphatic or systemic metastasis and the patient will have routine clinical and dermatoscopic surveillance in accordance with current guidelines [2].
Figure 1.
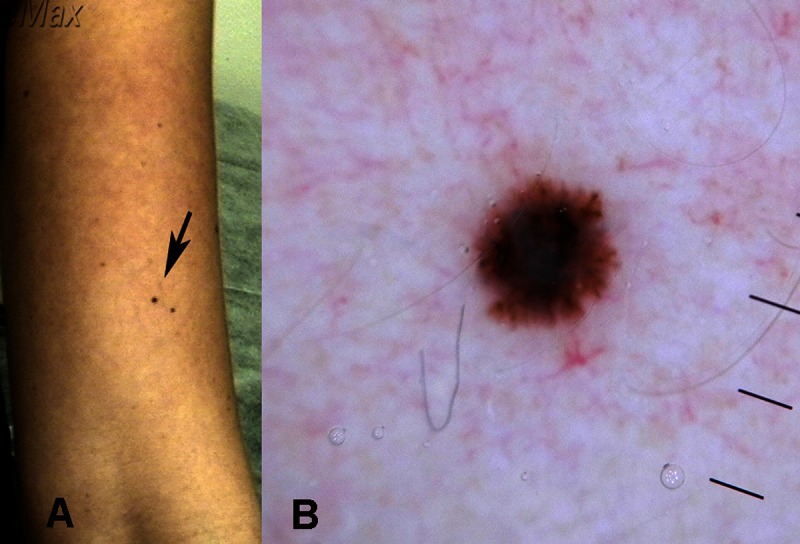
(A) Clinical image and (B) dermatoscopic image of a new pigmented skin lesion on the arm of a 38-year-old woman. Radial lines/pseudopods are arranged circumferentially around a structureless blue-gray centre. Although radial lines/pseudopods are present in all quadrants of the periphery they are less numerous in the upper-left quadrant. Asymmetry is assessed as equivocal. [Copyright: ©2013 Pellizzari et al.]
Figure 2.
(A) Low power and (B, C) high power dermatopathologic images of the lesion shown in Figure 1. [Copyright: ©2013 Pellizzari et al.]
Discussion
A proportion of melanomas have been found not to fit the D criterion of the ABCD acronym, where D stands for a diameter of 6 mm or greater. Such small melanomas have a reported frequency of 11.4–38.2% of all melanomas [3–6]. One review in particular, published in 2004, found that small melanomas include less than 1 to 38% of all invasive melanomas [1] and it recommended that the ABCD acronym be modified to ABCDE with “E” to stand for “evolving.”
Previously the dermatoscopic features of an in-situ melanoma with a diameter of 1.6 mm were reported [7]. Published dermatoscopy images revealed that even at this minute size there was unequivocal asymmetry of structure and the presence of the dermatoscopic clue to melanoma of gray dots. It satisfied the criteria for malignancy of the 3-point checklist [8], the Menzies method [9] and Chaos and Clues [10]. Teng et al reported the dermatoscopic features of an in-situ melanoma with a diameter of 2 mm [11]. A published dermatoscopy image revealed unequivocal asymmetry of both color and structure with some lines radial segmental and blue-gray structures.
In the case that we report, the lesion was noted to be hyperpigmented compared to surrounding PSLs. One previous study reported that intensity of dark pigmentation was the defining clinical characteristic in each of 13 (including 5 invasive) small melanomas (<4 mm diameter) in a series of 95 melanomas [5], although this may in fact be due to selection bias as minute dark melanomas are more likely to be noticed and assessed in comparison to small pale melanomas which may be present but not detected. The case reported here, unlike the two previously reported smallest in-situ melanomas [7,11] did not exhibit unequivocal dermatoscopic asymmetry, and this is significant because dermatoscopic asymmetry is a generally accepted criterion for all of the published clinical and dermatoscopic algorithms. However in one study of consecutive pigmented skin lesions with a maximum diameter of 6mm (range 3–6 mm) excised in a specialized university dermatology department over four years, 34 out of a total of 103 melanocytic lesions were melanomas [12], and of those 34 melanomas only 11 (32.4%) were asymmetrical. This supports the need to assess small PSLs without the required algorithmic criterion of asymmetry.
In one pilot study of 28 diagnosed melanomas less than or equal to 4 mm in diameter, there were only 14 (50%) that were unanimously diagnosed as melanomas by each of three dermatopathologists [13]. The dermatopathologic criteria of these were evaluated. The criteria regarded as most significant included pagetoid spread (n=9/14), irregular nesting (n=9/14), predominance of individual junctional melanocytes (n=6/14) and cytological atypia (n=13/14). The very small melanoma we present in this case report exhibited all of these features as well as poor maturation in the invasive portion with pigmentation and nesting to the base of the lesion.
Conclusion
The melanoma reported here had the same diameter, of 1.6 mm, as the previously smallest reported melanoma with dermatoscopic images, but it differed in that it was invasive. As has been previously reported with small melanomas, it was darker than surrounding nevi but this may be due to selection bias. We regard it as very significant that this melanoma did not have unequivocal asymmetry, although it did have recognized clues to malignancy, including the presence of gray color and radial lines/pseudopods, albeit arranged in a circumferential pattern. We believe that very small pigmented lesions which have any recognized clues to melanoma should be assessed for biopsy whether or not unequivocal asymmetry is present.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Abbasi NR, Shaw HM, Rigel DS, et al. Early diagnosis of cu-taneous melanoma: revisiting the ABCD criteria. JAMA. 2004;292(22):2771–6. doi: 10.1001/jama.292.22.2771. [DOI] [PubMed] [Google Scholar]
- 2.Australian Cancer Network Melanoma Guidelines Revision Working Party . Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. The Cancer Council Australia and Australian Cancer Network, Sydney and New Zealand Guidelines Group; Wellington: 2008. p. xxxii. [Google Scholar]
- 3.Fernandez EM, Helm KF. The diameter of melanomas. Dermatol Surg. 2004;30(9):1219–22. doi: 10.1111/j.1524-4725.2004.30379.x. [DOI] [PubMed] [Google Scholar]
- 4.Abbasi NR, Yancovitz M, Gutkowicz-Krusin D, et al. Utility of lesion diameter in the clinical diagnosis of cutaneous melanoma. Arch Dermatol. 2008;144(4):469–74. doi: 10.1001/archderm.144.4.469. [DOI] [PubMed] [Google Scholar]
- 5.Goldsmith SM, Solomon AR. A series of melanomas smaller than 4 mm and implications for the ABCDE rule. J Eur Acad Dermatol Venereol. 2007;21(7):929–34. doi: 10.1111/j.1468-3083.2006.02115.x. [DOI] [PubMed] [Google Scholar]
- 6.Helsing P, Loeb M. Small diameter melanoma: a follow-up of the Norwegian Melanoma Project. Br J Dermatol. 2004;151(5):1081–3. doi: 10.1111/j.1365-2133.2004.06248.x. [DOI] [PubMed] [Google Scholar]
- 7.Rosendahl C, Cameron A, Bulinska A, Williamson R, Kittler H. Dermatoscopy of a minute melanoma. Australas J Dermatol. 2011;52(1):76–8. doi: 10.1111/j.1440-0960.2010.00725.x. [DOI] [PubMed] [Google Scholar]
- 8.Argenziano G, Soyer HP, Chimenti S, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. 2003;48(5):679–93. doi: 10.1067/mjd.2003.281. [DOI] [PubMed] [Google Scholar]
- 9.Menzies SW, Ingvar C, Crotty KA, McCarthy WH. Frequency and morphologic characteristics of invasive melanomas lacking specific surface microscopic features. Arch Dermatol. 1996;132(10):1178–82. [PubMed] [Google Scholar]
- 10.Rosendahl C, Cameron A, McColl I, Wilkinson D. Dermatoscopy in routine practice—‘chaos and clues’. Aust Fam Physician. 2012;41(7):482–7. [PubMed] [Google Scholar]
- 11.Teng PP, Hofmann-Wellenhof R, Campbell TM, Soyer HP. Dermoscopic presentation of a 2-mm melanoma in situ. Australas J Dermatol. 2010;51(2):152–3. doi: 10.1111/j.1440-0960.2009.00620.x. [DOI] [PubMed] [Google Scholar]
- 12.de Giorgi V, Savarese I, Rossari S, et al. Features of small mela-nocytic lesions: does small mean benign? A clinical-dermoscopic study. Melanoma Res. 2012;22(3):252–6. doi: 10.1097/CMR.0b013e3283527430. [DOI] [PubMed] [Google Scholar]
- 13.Ferrara G, Tomasini C, Argenziano G, Zalaudek I, Stefanato CM. Small-diameter melanoma: toward a conceptual and practical reappraisal. J Cutan Pathol. 2012;39(7):721–3. doi: 10.1111/j.1600-0560.2012.01884.x. [DOI] [PubMed] [Google Scholar]